Abstract
Aims
To report the outcomes of using a modified Bick’s procedure (MBP) combined with a monopedicle myocutaneous flap (MMCF) or full-thickness skin grafting (FTSG) to correct lower eyelid cicatricial ectropion.
Patients and methods
A retrospective case-note review of patients undergoing cicatricial ectropion repair between 2012 and 2016 was undertaken. Patient demographics, clinical features, the type of surgery, and outcomes were analysed.
Results
Twenty-four eyelids of 21 treated patients (17 males; 81%) with lower eyelid cicatricial ectropion were identified. They presented at an average age of 79.8 years (median 78; range 58–92). The commonest symptom was epiphora (15 eyelids; 63%), 12 patients (50%) experienced intermittent irritation, and 2(8%) had mucoid discharge. The aetiology included actinic cicatricial ectropion with midface descent (n = 19, 79%), previous tumour resection (n = 3, 13%), trauma (n = 1) and other previous eyelid surgery (n = 1). At a mean follow-up period of 15.3 months (median 6; range 6–52), 22 eyelids (92%) had anatomical success with good cosmesis and two eyelids (8%) had mild residual punctal ectropion. Twenty-one patients (87%) experienced functional success. Comparing the outcomes of MBP + FTSG versus MBP + MMCF, there was no statically significant difference in terms of anatomical (p = 0.48) and functional (p = 1.0) success rates. No cases of failure or recurrence were noted during the follow-up period.
Conclusions
Anterior lamellar deficit ectropion occurs in the absence of overt scarring. It is crucial to fully address both the horizontal laxity and the anterior lamellar deficit associated with such ectropion to minimise the risks of early failure and recurrence. MBP combined with FTSG or MMCF is a safe and effective treatment for such ‘cicatricial ectropion’ and has a low early recurrence rate.
Similar content being viewed by others
Introduction
Acquired ectropion is traditionally classified as involutional, cicatricial, paralytic or mechanical (ranked in order of frequency of occurrence) [1]. The latter two are self-explanatory. Paralytic ectropion affects the lower lid and occurs because the orbicularis muscle lid lacks the muscular tone to hold it against the globe, allowing gravity to pull the lid downwards. True mechanical ectropion is rare and occurs if excessive lower lid loading, by a tumour or cyst, is sustained and sufficient to overcome the orbicularis tone.
The distinction between involutional and cicatricial ectropion is less clear cut. In pure cicatricial ectropion anterior lamellar shortening by scar tissue applies sustained traction to which eventually stretches the lid margin (tissue expansion) and pulls it away from the globe. In effect this is another form of ‘mechanical ectropion’. Underlying causes include mechanical, thermal and chemical trauma, dermatological disease, eyelid tumour surgery or cosmetic procedures [1,2,3,4,5,6,7,8,9]. Often, relative skin shortage is due to tight actinic skin [2, 4, 5, 7, 9]. Frequently overlooked is the contribution of involutional mid face descent which may be a consequence of age induced ‘facial deflation’ [10] or facial ligament stretching and failure. This can be exacerbated by frequent eye rubbing. A better catch all term might be “anterior lamellar deficit ectropion”. However, for shorthand this continuum is usually termed “cicatricial”, even in the absence of a cicatricial process.
The surgical management of such “cicatricial ectropion” involves three steps:
-
1.
Release of the radial lid margin traction forces.
-
2.
Shortening of the lengthened lid margin to bring it back snugly against the globe.
-
3.
Correction of the revealed anterior lamellar deficit.
Various eyelid shortening procedures have been proposed for correction of horizontal eyelid laxity associated with cicatricial ectropion, including pentagon excision/wedge resection, lateral tarsal strip, lateral canthopexy or lateral eyelid-block excision with canthoplasty, with an anatomical recurrence or persistent ectropion rate up to 43% [2,3,4,5,6,7,8,9]. The high recurrence rates are most likely the combination of a failure to recognise and adequately correct the anterior lamellar deficit and to the particular lid margin tightening technique used. Some are longer lasting than others.
In this study, we report the outcomes of “cicatricial ectropion” correction using a modified Bick’s procedure (MBP) [11] to address the horizontal eyelid laxity and skin transfer, either as a free skin graft or as a myocutaneous flap.
Methods
A retrospective case note review of patients undergoing “cicatricial eyelid ectropion” surgery between 2012 and 2016 was undertaken.
Primary outcome measures were anatomical and functional success. Anatomical success was defined as complete restoration of the normal eyelid or punctal position. Functional success was defined as resolution or improvement of the presenting symptomatic complaint. Early and late postoperative complications rate recorded during the follow-up period were noted. Data were also collected on patient demographics, the aetiology of their cicatricial ectropion, previous eyelid or lacrimal surgery, and on any adjunctive procedures. The minimum follow-up period was 6 months.
In the absence of obvious scarring the test used to determine whether a significant anterior lamellar deficit existed was to look for the presence of lower lid movement coupled to gentle digital lower cheek manipulation, while the patient is looking up.
The surgical technique consisted of:
-
1.
An infraciliary incision made ~4–5 mm below the lid margin and extending past the medial and lateral canthi (unless the scar was very localised) with subcutaneous and/or orbital septum cicatrix-lysis as required.
-
2.
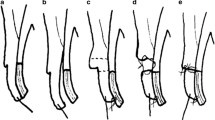
Correction of the horizontal eyelid laxity by means of MBP [11], which is a full thickness lateral lid margin resection (the amount gauged by overlapping the lid and canthus) followed by a direct repair of the cut tarsal plate edge to the cut end of the lateral canthal tendon (easily confirmed by its strong resistance to pull). (Fig. 1 and 2)
Fig. 1: Schematic illustration of the modified Bick’s procedure combined with a skin graft. a Following placement of 4/0 polypropylene lower lid traction suture, a skin and orbicularis incision is performed 4–5 mm below the lash line. b Keeping the lid margin under upward tension deeper dissection is carried out to release any restricting attachments or scars, especially if to the orbital septum. A downward angled, full thickness, lid margin incision is made at the junction of the lateral canthus and lower eyelid (leaving the main body of the lateral canthal tendon (LCT) intact). c The cut LCT is pulled medially and the cut lid margin overlapped laterally under moderate tension, to mark the excess lid margin. d The excess margin is excised as a full thickness triangle. e The tarsal plate stump is reattached to the lateral canthal tendon by 1 or 2 double armed 6/0 or 5/0 absorbable sutures, followed by reformation of the lateral canthal angle with a 7/0 absorbable suture. f The lid margin is placed on upward traction to size the skin defect thus allowing for graft shrinkage. The defect is repaired using a full thickness skin graft or local flap.
Fig. 2: Schematic illustration of the modified Bick’s procedure combined with a skin pedicle flap. a Following placement of 4/0 polypropylene lower lid traction suture, a skin and orbicularis incision is performed 4–5 mm below the lash line & extending 7 mm lateral to the lateral canthus. b Keeping the lid margin under upward tension deeper dissection is carried out to release any restricting attachments or scars, especially if to the orbital septum. c downward angled, full thickness, lid margin incision is made at the junction of the lateral canthus and lower eyelid (leaving the main body of the lateral canthal tendon (LCT) intact). d The cut LCT is pulled medially and the cut lid margin overlapped laterally under moderate tension, to mark the excess lid margin. The excess margin is excised as a full thickness triangle. e The tarsal plate stump is reattached to the lateral canthal tendon by 1 or 2 double armed 6/0 or 5/0 absorbable sutures, followed by reformation of the lateral canthal angle with a 7/0 absorbable horizontal mattress suture. f The lid margin is placed on upward traction to size the skin defect thus allowing for graft shrinkage. g An upper lid skin and orbicularis lateral pedicle flap is marked and raised. Note that points A and B are vertically aligned. h The defect is repaired by transposing the upper lid flap and its pedicle into the lower lid, effectively moving point C vertically upwards from B to A.
-
3.
Correction of the residual anterior lamellar deficit, following margin repair. A paper template of the defect is made while the reconstructed lid margin is held in gentle upward traction by a meibomian orifice line traction suture (Fig. 3). The template is used to mark the donor skin area. Either a free full-thickness skin graft (FTSG) (Fig. 1) or an upper to lower lid transpositional flap [3]–inlaid monopedicle myocutaneous flap (MMCF)—(Fig. 2) harvested from the upper lid is used when available. Otherwise a free graft is taken from the inner brachial area.
Fig. 3: Meibomian Orifice Line Tarsal Traction Suture Placement. a The lid margin is grasped flat. A 4/0 Polypropylene suture on a half circle round bodied (non-cutting) needle is inserted into the meibomian orifice line. b The suture is advanced, following the curve of its needle, within the tarsal plate plane. It should again exit through the meibomian orifice line. It allows painless, lasting, lid margin traction.
Post-operatively, the eyelid margin is kept on upward traction using the previously placed 4/0 polypropylene meibomian orifice line suture taped to the forehead with adhesive tape, and a pressure dressing is applied for at least 5 days. The traction suture is removed at the first dressing. From 2 weeks postoperatively patients are instructed to gently massage the operated lid upwards for three minutes twice daily with a thin smear of hydrocortisone 1% skin ointment and to continue doing this for 2 months. The upward massage is an attempt to counteract the natural, healing contracture that occurs in grafts and flaps.
Statistical analysis was performed to compare the treatment outcomes of MBP + FTSG versus MBP + MMCF. Categorical variables were compared with the Fisher’s exact test, and an α-risk of 0.05 was considered significant. The study had local ethics approval (CA_2016–17–148) and adhered to the tenets of the Declaration of Helsinki.
Results
Twenty-four eyelids of 21 patients (17 males; 81%) treated for lower eyelid cicatricial ectropion were identified. Mean age at presentation was 79.8 years (median 78; range 58–92). The commonest symptom was epiphora (15 eyelids; 63%) that was bilateral in 3 patients (12%), although 12 cases (50%) had intermittent irritation, and 2 (8%) had mucoid discharge (Table 1).
Tight actinic facial skin associated mid-face descent was the most common underlying cause of the anterior lamellar deficit (19 eyelids, 79%) and three cases (13%) had undergone previous periorbital tumour resection surgery (2 basal cell carcinoma, and 1 squamous cell carcinoma). (Table 1) Six patients (25%) had had previous oculoplastics surgery including tumour surgery (3), eyelid laceration (1), pentagon excision (1) and endoscopic dacryocystorhinostomy (1).
MBP was performed in all cases to address the horizontal laxity, with a mean eyelid margin resection of 9.83 mm (median 10 mm; range 5–16 mm). The anterior lamellar deficit was treated with FTSG (11 eyelids, 46%) or MMCF (13 eyelids, 56%). Posterior medial canthal thermoplasty [12] (n = 2) for repair of a lax medial canthal tendon and lower lid retractor plication (n = 1) were performed as adjunctive procedures to stabilise three eyelids. (Table 1)
After a mean follow-up period of 15.3 months (median 6; range 6–52), 22 eyelids (92%) achieved a restoration of normal eyelid margin anatomy with good cosmesis, two eyelids (8) had mild residual punctal ectropion, and 21/24 (87%) had patient reported functional success. Comparing the outcomes of MBP + FTSG versus MBP + MMCF, there was no statistically significant difference in terms of anatomical (p = 0.48) or functional (p = 1.0) success rates. (Table 2) No cases of failure or recurrence were noted during the follow-up period.
Complications were minor with no long-term implications. (Table 2) None of the patients had postoperative lateral canthal wound dehiscence, graft or flap necrosis, unallowed for graft contracture, graft hypertrophy, granuloma formation or infection.
Discussion
Repair of lower eyelid ectropion should address all the contributing anatomical factors. The benefits of skin grafting or myocutaneous flaps are well recognised for treating the vertically shortened anterior lamella [3,4,5,6,7,8,9]. However, ectropion is generally associated with horizontal ‘lid-globe disparity’ (eyelid laxity) [1, 7, 8, 11, 13] and failure to address this factor effectively will lead to sub-optimal outcomes.
While the type of anterior lamella repair does not appear to greatly influence the outcome [2], the ectropion recurrence rate has been shown to be significantly lower among the eyelids that had concurrent horizontal tightening in addition to skin transfer [5]. Our results support this finding.
Several studies have combined lateral tarsal strip or lateral canthopexy with different myocutaneous flaps or skin grafting–with the reported failure or recurrence rate ranging between 6.5 and 44% [4,5,6,7,8,9]. However, aetiological factors or additional concurrent procedures may have also influenced these outcomes. (Table 3) Although lateral canthopexy is a relatively simple technique, it merely tightens the lateral canthal supporting structures without shortening the eyelid margin, and is therefore, only suitable for milder degrees of eyelid laxity.
A recent study combining lateral eyelid-block excision with canthoplasty and FTSG reported an overall recurrence rate of 29% after 3 months of follow-up [8]. Another group used a fairly similar eyelid shortening technique combined with lower lid retractor plication, and found 43% anatomical recurrence, and 11% reoperation rate at 48 months follow-up [9].
In our study combination of MBP and FTSG or MMCF was associated with anatomical success in 92%, while 8% had mild under correction with a zero recurrence rate (at minimum 6 months follow up). Our functional improvement of 87% of the cases is similar to previously reported series which range between 70 and 90% [4, 6, 9]. Likewise, the modality of skin transfer–FTSG versus MMCF–did not significantly affect the objective and subjective outcomes (Table 2). The choice of skin repair is dependent on the availability of local tissue. Theoretically a pedicle graft brings its own blood supply and provides additional lateral lift. In practice however the periocular blood supply is usually so good that avascular graft necrosis should not occur. The benefit of any putative additional lift remains to be proven.
The eyelid margin was found to be significantly lengthened in the majority of our cases. This is likely due to a combination of factors including involutional changes, chronic tractional force exerted by the cicatrix or tight skin, and midface descent generating an additional gravitational vector on the lid margin [10]. On average, approximately 1 cm of eyelid margin resection was required to stabilise the eyelid margin. The amount was gauged by overlapping the lid with the lateral canthus after the lateral canthal incision until the margin became tight. This was to compensate for the anticipated postoperative relaxation (tissue expansion) that invariably occurs. Although it is difficult to independently quantify the contribution of the eyelid shortening, the effective treatment of horizontal laxity significantly improves eyelid stability and so by inference the recurrence rate. Our results support this concept. However, unless the causative factor (anterior lamellar deficit), which brought about the lid margin lengthening in the first place, is not adequately addressed early recurrence should be expected.
Bick’s lateral shortening [13] involves a full-thickness triangular excision at the lateral canthus, which unlike LTS, spares the lateral canthal anatomy including main body of the lateral canthal tendon. This allows direct re-attachment of the shortened eyelid margin. Unpublished laboratory work on the mechanical properties of pig canthal tendon and tarsal plate showed that tendon does not stretch under load, but tarsal plate does. This is of particular relevance for the late failure of tarsal strip tightening surgery [14]. Bick’s procedure has been criticised for its complexity, lateral canthal rounding and dehiscence [15]. However, in our experience – a retrospective comparative study of 641 procedures [11]–a MBP was associated with excellent anatomic and functional success and lower aforementioned complication rates compared with the lateral tarsal strip. MBP is a simple procedure which also allows a more natural anatomic union of the tarsal plate to the lateral canthal supporting structures [11].
The weaknesses of this report include its small numbers, retrospective nature and non-comparative design. However, its findings do support our longstanding clinical experience.
In summary, in cicatricial ectropion it is crucial to look for and to effectively address both the horizontal laxity caused by the traction from chronic anterior lamellar deficit, as well as to correct the deficit itself. Addressing only one factor risks early failure and recurrence. Occult relative anterior lamellar deficit in the absence of overt scarring may be a contributing factor in some involutional ectropions. The Modified Bick’s Procedure (MBP) is a safe and effective treatment for addressing horizontal eyelid laxity when combined with FTSG or MMCF anterior lamellar augmentation. It has a low recurrence rate.
Summary
What was known before
-
Relative eyelid skin shortage due to tight actinic skin or midface descent is often termed as cicatricial ectropion.
-
Horizontal eyelid laxity may associate cicatricial lower eyelid ectropion.
-
MBP is an effective and safe treatment for involutional ectropion.
What this study adds
-
The category of “Anterior lamellar deficit ectropion” which encompasses both true cicatricial ectropion and involutional mid face ptosis ectropion.
-
Occult relative anterior lamellar deficit in the absence of overt scarring may be a contributing factor in some involutional ectropions.
-
In cicatricial ectropion it is crucial to look for and to effectively address both the horizontal laxity, as well as to correct the deficit itself.
-
Evidence to support the use of MBP with anterior lamellar skin transfer in ‘anterior lamellar deficit ectropion’ surgery.
Change history
18 June 2020
The original HTML version of this Article was updated shortly after publication in order to correct typos in the acronym for “lateral canthal tendon” (the acronym was misstated as “LTC” but has been updated to “LCT”).
References
Collin JRO. A Manual of Systematic Eyelid Surgery. 3rd ed. Edinburgh: Butterworth-Heinemann, Elsevier Limited, 2006:57-59.
Marshall JA, Valenzuela AA, Strutton GM, Sullivan TJ. Anterior lamella actinic changes as a factor in involutional eyelid malposition. Ophthalmic Plast Reconstr Surg. 2006;22:192–4.
Hurwitz JJ, Lichter M, Rodgers J. Cicatricial ectropion due to essential skin shrinkage: treatment with rotational upper-lid pedicle flaps. Can J Ophthalmol. 1983;18:269–73.
O’Donnell BA. Eyelid retractor surgery as an adjunct to cicatricial ectropion repair. Clin Exp Ophthalmol. 2000;28:293–7.
Manku K, Leong JK, Ghabrial R. Cicatricial ectropion: repair with myocutaneous flaps and canthopexy. Clin Exp Ophthalmol. 2006;34:677–81.
Kim HJ, Hayek B, Nasser Q, Esmaeli B. Viability of full-thickness skin grafts used for correction of cicatricial ectropion of lower eyelid in previously irradiated field in the periocular region. Head Neck. 2013;35:103–8.
Choi CJ, Bauza A, Yoon MK, Sobel RK, Freitag SK. Full-thickness skin graft as an independent or adjunctive technique for repair of cicatricial lower eyelid ectropion secondary to actinic skin changes. Ophthalmic Plast Reconstr Surg. 2015;31:474–7.
Mol I, Paridaens D. Efficacy of lateral eyelid-block excision with canthoplasty and full-thickness skin grafting in lower eyelid cicatricial ectropion. Acta Ophthalmol. 2019;97:e657–e661.
McKelvie J, Papchenko T, Carroll S, Ng SG. Cicatricial ectropion surgery: a prospective study of long-term symptom control, patient satisfaction and anatomical success. Clin Exp Ophthalmol. 2018;46:1002–7.
Chung JE, Yen MT. Midface lifting as an adjunct procedure in ectropion repair. Ann Plast Surg. 2007;59:635–40.
Vahdani K, Ford R, Garrott H, Thaller VT. Lateral tarsal strip versus Bick’s procedure in correction of eyelid malposition. Eye (Lond). 2018;32:1117–22.
Vahdani K, Thaller VT. Posterior medial canthal thermoplasty. Ophthalmic Plast Reconstr Surg. 2017;33:221–4.
Bick MW. Surgical management of orbital tarsal disparity. Arch Ophthalmol. 1966;75:386–9.
Blanc J-P, Thaller VT. Mechanical properties of pig canthal tendon and tarsal plate. Paper presented at Annual Meeting of the European Society of Ophthalmic Plastic and Reconstructive Surgery; 2005; Crete. (Unpublished)
Hurwitz JJ, Mishkin SK, Rodgers KJ. Modifications of Bick’s procedure for treatment of eyelid laxity.”. Can J Ophthalmol. 1987;22:262–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vahdani, K., Thaller, V.T. Anterior lamellar deficit ectropion management. Eye 35, 929–935 (2021). https://doi.org/10.1038/s41433-020-0998-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0998-6
- Springer Nature Limited