Abstract
The purpose of this study is to systematically review the reported data of normal optical coherence tomography (OCT) results in the paediatric population. A systematic literature search was performed using the PubMed, Embase, and Web of Science databases, using the keywords “optical coherence tomography”; “normative data” or “healthy eyes”; “children” or “paediatric population”. Studies with at least 50 participants were included, irrespective of the OCT equipment employed. We excluded the OCT angiography studies or the studies investigating the choroidal thickness. Seventy-four studies were included in the final analysis and information on study design, number of participants, demographic characteristics, type of OCT equipment, OCT parameters and results was collected. Due to the high variability of OCT instruments and parameters used, a meta-analysis was not feasible. We report the normative values for the peripapillary retinal nerve fibre layer thickness and the macular retinal thickness for each ETDRS quadrant, as provided by the studies included in the present analysis. We also report the influence of ethnicity, age, gender, eye laterality, ISNT rule, spherical equivalent, and axial length on OCT results.
摘要
本研究旨在系统性回顾小儿群体中正常者相干光断层扫描(OCT)的结果。通过使用“相干光断层扫描”、“常模数据”或“健康眼”、“儿童”或“小儿群体”等关键词, 在PubMed、Embase和Web of Science等数据库中进行系统性文献检索。不管应用哪种OCT设备, 研究至少包括50名受试者。我们将有关OCTA或脉络膜厚度的研究排除在外。最终纳入了74项研究, 收集研究设计、参与人数、人口学特征、OCT设备类型、OCT参数和结果等信息。由于不同研究中OCT仪器和参数高度变异, meta分析不具备可行性。根据纳入的研究, 我们报道了每个ETDRS象限的视乳头周围视网膜神经纤维层厚度和黄斑视网膜厚度的常模值, 以及种族、年龄、性别、眼偏侧性、ISNT原则、等效球镜和眼轴长度对OCT数值的影响。
Similar content being viewed by others
Introduction
Optical coherence tomography (OCT) is a non-invasive and non-contact imaging technique, which found its applicability in various ocular conditions affecting either the anterior segment of the eye or the optic nerve and the retina. Due to the high speed of scanning, the OCT assessment can also be performed in patients who present certain difficulties in collaboration, including children. Despite of the challenges of OCT use in the paediatric population (e.g., height and position of the headrest, size of the machine, image artifacts produced by small movements, etc.), there are numerous papers reporting the OCT evaluation in children with optic nerve swelling, glaucoma, retinal dystrophies, and other [1], with high repeatability and reproducibility indices for the OCT use in this young population [2].
Several OCT instruments produced by different manufacturers are available, but the equipment has an incorporated age-matched normative database only for adults. This is the reason why the quantitative interpretation of results obtained in children is difficult.
Some authors suggested to use the follow-up method, which consists in setting the first examination as a reference, and all the other examinations would be compared to the first [3]. However, the sequential analysis of a growing eye during larger periods of time could be potentially influenced by the changing values of the examined parameters given by the growth itself.
Other researchers examined the OCT features in normal children and many papers showing these results have already been published. In order to help the clinicians to find the relevant study for their practice, the purpose of our paper is to review the literature on the normative data for OCT parameters in the paediatric population.
Methods
A systematic literature review was conducted using the PubMed, Embase, and Web of Science databases. The search was performed independently by both authors according to the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [4]. We restricted the search to articles published in English and the following MeSH terms (Medical Subject Headings) were used: “optical coherence tomography”, “normative database” OR “healthy eyes”, “children” OR “paediatric population”. We did not use any restriction for the publication date.
The inclusion criteria were: original studies conducted on human participants aged <18, no ocular disease other than refractive errors, use of posterior pole OCT, and at least 50 participants enroled in the study.
We excluded review articles and the papers in which adult participants were also included or the patients had a systemic disease which can induce retinal or optic nerve alterations (e.g., diabetes). We did not include in the present review the research on OCT angiography or the studies which had the objective to evaluate the thickness of the choroid. Inconsistency in statistical report was another reason for exclusion. We also excluded the studies which investigated solely the reproducibility of the OCT examination in children.
All the records were screened for relevancy based on title and abstract, and the relevant articles were included in the full-text evaluation. The above-mentioned inclusion and exclusion criteria were the only criteria used to determine the eligibility of each study. The differences between the lists of eligible studies were discussed by the two authors. We also performed a manual search of the list of references of the included articles in order to identify additional published studies not indexed in the three databases.
We did not use the type of OCT equipment as an indicator for the selection of articles, and we have no conflict of interest for this research. The date of our last search was June 17, 2020.
In order to perform the quality assessment for the included studies, we employed the Joanna Briggs Institute Critical appraisal tool for case series [5]. From each study included into evaluation, we collected information on study design, number of participants, demographic characteristics, type of OCT equipment, and OCT parameters.
Results
The review process
The PubMed database search provided 581 records, Embase provided 562 records, and Web of Science 274 records. After screening and full-text assessment, 74 articles were included into the analysis (Fig. 1).
Records identified through searching of 3 databases were screened based on title and abstract; after duplicates were removed, the full-text version of 103 articles was assessed for eligibility. Four additional papers were found by searching the lists of references of the eligible articles. After the exclusion of 33 articles which did not meet the inclusion criteria, 74 studies were included in the present review.
In Table 1, we provide the results of the quality assessment of the studies included in our systematic review. The Joanna Briggs Institute checklist [5] contains 10 items assessing the selection bias (item 1), performance bias (items 2 and 3), design bias (items 4, 5, and 10), and reporting bias (items 6–9). All these items are found in Table 1. For item 2, we considered the standardised ophthalmological examination which had concluded that the selected eyes were normal, whereas for item 3 we assessed the OCT scanning protocol of the included eyes. Regarding the reporting of the demographics of the participants in the study (item 6), we took into consideration age, gender, and ethnicity. For item 7, we evaluated the reporting of the ophthalmological evaluation results, and for item 8 we assessed the reporting of OCT results.
The records in Table 1 are sorted by OCT technology, alphabetically by OCT manufacturer, and then chronologically by the publication date; this order is respected throughout the “Results” section.
Collected data
In Table 2 are found the demographic and clinical features of the papers included in the present review. Twenty-two studies were conducted using the time domain OCT technology, whereas 52 studies employed spectral domain OCT devices. Twenty-four studies were population based, whereas the other were hospital based. The vast majority of the studies included children older than 3 and the OCT evaluation was performed at a table-mounted instrument; four papers used a handheld OCT device to examine neonates or very young children [6,7,8,9].
Table 3 comprises the values of the predefined peripapillary retinal nerve fibre layer (RNFL) thicknesses, as reported by the included studies. Other papers used additional optic disc parameters or employed custom-made scanning protocols (see Table 2 to identify such studies).
In Table 4 are included the values of the average and sectorial thicknesses of the macula. The ETDRS (Early Treatment Diabetic Retinopathy Study Research Group 1991) circular grid [10] scanning protocol was the most frequently used. Some studies also evaluated segmented retinal layers’ thickness (results not included in Table 4).
Due to the high variability of both the OCT instruments and methodologies of the studies, a statistical analysis of the data was not feasible.
Discussion
Comments on our methodology
We included both hospital-based and population-based studies. Although population-based studies are preferable for the topic of our paper, the majority of studies are hospital based and valuable information would have been lost if we excluded this type of studies. Moreover, the inclusion and exclusion criteria for all the studies were thoroughly verified.
We chose arbitrarily the minimum number of participants included in the selected papers (i.e., 50 participants): although higher number of records is required for a database to be considered normative, there are several limitative factors for such a study to be conducted (e.g., collaboration of children, parent or tutor consent, experience of technicians, and others).
Risk of bias within the studies
Table 1 demonstrates that the highest risk of bias of the included studies is related to the consecutive inclusion of participants, and complete inclusion of participants, respectively.
Risk of bias across the studies
We observed a high variability of inclusion criteria and/or ophthalmological tests performed across the studies (i.e., selection bias)—e.g., visual acuity presented different ranges between studies, cycloplegia was performed only in some studies before the refraction measurement, and only a part of the studies also included the assessment of the intraocular pressure. Moreover, some investigators examined and/or included into analysis only one eye of each participant.
Influence of ethnicity on OCT parameters
The influence of race or ethnicity on the OCT parameters was reported by the following authors:
-
(1)
Huynh et al. [11]: Central and inner macular thickness is higher in white children compared with East Asians, and the thickness of the outer temporal macular region is higher in Middle Eastern children compared with whites.
-
(2)
Huynh et al. [12]: Both the average and sectorial RNFL thicknesses are higher in white participants compared with East Asians.
-
(3)
Huynh et al. [13]: East Asians had larger optic discs, but smaller neural rim areas than European white children.
-
(4)
El-Dairi et al. [14]: The inner macular thickness, foveal thickness and total macular volume were greater in white children compared with black children, whereas the thicknesses of average RNFL and superior quadrant of RNFL were higher in black than in white children.
-
(5)
Tariq et al. [15]: East Asians demonstrated the strongest relationship between axial length and retinal OCT parameters; Caucasians had smaller correlations with axial length for retinal OCT parameters, except for foveal minimum and central macular thickness; Middle Eastern children presented strong negative correlation of axial length with outer macular thickness and macular volume; South Asians had a positive correlation between the thickness of the temporal sector of RNFL and axial length.
-
(6)
Samarawickrama et al. [16]: The RNFL thickness and optic cup size were higher in East Asian children compared with European Caucasians.
-
(7)
Allingham et al. [6]: Black infants had larger vertical cup diameter than whites, and Hispanic infants had larger vertical disc diameter than whites.
-
(8)
Rothman et al. [7]: Superior-temporal sector of RNFL presented greater thickness in blacks and Hispanics than in whites.
-
(9)
Yanni et al. [17]: No significant effect of race or ethnicity on central macular or average RNFL thicknesses was found.
-
(10)
Rotruck et al. [18]: There was no relationship between RNFL thickness and race.
The other papers included in this analysis did not evaluate the possible association between ethnicity or race and the OCT parameters.
Studies conducted on adult participants reported ethnic differences in the structures of the eye that are commonly imaged [19]. These results are difficult to compare with the reports from the paediatric studies because of differences in sampling and imaging techniques.
Influence of age on OCT parameters
Several papers reported no significant association between age and RNFL thickness [9, 17, 18, 20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35] or macular thickness [34, 36,37,38,39,40,41,42,43,44] in the paediatric population.
However, Salchow et al. [45], Lee et al. [46] and Ali et al. [44] found a statistically significant effect of age on RNFL thickness, Hong et al. [47] reported that ocular magnification—corrected average RNFL thickness was positively correlated with age, whereas Goh et al. [48] demonstrated a negative correlation between superior sector RNFL thickness and age, and Chen et al. [49] reported that for the children aged >11 almost all RNFL parameters decrease with age.
For the macular area, there was a high variability of studied parameters and some studies found a correlation between age and the thickness of some of the ETDRS sectors either for total retinal thickness or segmented retinal layers’ thickness [11, 17, 18, 25, 27, 28, 31, 42, 44, 50,51,52,53,54,55], but these results were inconstant.
The need for an aged-matched normative database in adults is given by the presence of the so-called “age-related loss” for several parameters. For example, a linear decrease of average RNFL thickness was reported and the results suggest that the reduction of RNFL is pronounced after the age of 50, and the RNFL quadrants are not equally affected [56].
The majority of the studies included in our qualitative analysis showed no association between age and OCT parameters, while the results of the papers which did report a correlation are variable. Until further evidence is available, we find reasonable to consider that in the paediatric population there is no effect of age on RNFL thickness.
However, the macular thickness may vary with age: histologic studies show that most of the morphological development of the human macula takes place in the first 5 years of life and research performed with handheld OCT devices for this age range show a progressive macular thickening, with a logarithmic increase of the photoreceptor layer and a decrease in the ganglion cell and inner nuclear layers [18, 57]. The majority of the studies included in our evaluation did not include children under the age of 5, and to the best of our knowledge, there is no paper with participants covering the entire range 0–18 years of age.
Rotruck et al. [18] reported the RNFL thickness for the 0–5 years old range and the OCT examination was performed with a portable Spectralis device. The results are similar with those reported by Yanni et al. [17] for children aged between 5 and 15, using a Spectralis table-mounted OCT device (see Table 3). This finding suggests that the peripapillary RNFL thickness does not vary in parallel with the changing morphology of the macula.
Handheld OCT devices
Portable OCT devices are a good alternative to the table-mounted instruments for the examination of young, anxious or autistic children, even though unsteady hands of the examiner or the excessive motion of the child may influence the quality of the acquired images. However, the examination can also be performed under general anaesthesia [1]. Four out of the five studies included in our review which employed a handheld device used nonstandard OCT parameters (Table 2).
Influence of gender on OCT parameters
For the RNFL thickness, 18 studies found no significant difference between boys and girls [2, 17, 18, 20, 22,23,24,25, 27,28,29, 32, 44, 45, 50, 58,59,60].
Huynh et al. [12] found greater values of average RNFL, inferior sector RNFL, and 6, 12, and 9 o’clock RNFL sectors in boys, while Chen et al. [49] reported similar results for the inferior and temporal RNFL sectors. However, Zhu et al. [33] found girls to have higher thicknesses for the same inferior and temporal RNFL sectors.
For the macular OCT assessment, no correlation with gender was found by Eriksson et al. [36], Galdos et al. [52], Molnar et al. [38], Sushil et al. [39], Nigam et al. [40], and Yanni et al. [17]. A greater number of studies reported higher values in boys for different macular parameters: Huynh et al. [11]—inferior macular quadrant, Zhang et al. [37]—foveal minimum, central macula, inner ring, temporal outer quadrant, Barrio-Barrio et al. [25]—central macula, Katiyar et al. [51]—central macula and inner ETDRS ring, Al-Haddad et al. [27]—central macula, Chen et al. [61]—central macula, Queiros et al. [28]—central macula and inner ring, Guragac et al. [29]—fovea, Read et al. [41]—total macular thickness, Passani et al. [54]—inner macula volumes, Yabas Kiziloglu et al. [34]—central macula, inner ring, inferior outer quadrant, Ali et al. [44]—macular volume, central macular thickness, inferior quadrants, and temporal outer quadrant. There were no studies reporting greater values of macular OCT parameters in girls.
Based on the reported results, we draw the conclusion that RNFL thickness is not influenced by gender in the paediatric population, although the central macular OCT parameters tend to be higher in boys. These results are in agreement with the findings in the adult population [62,63,64,65,66].
Influence of eye laterality on OCT parameters
The average RNFL thickness presented no significant differences between the right and left eye in the studies of Ahn et al. [20], Salchow et al. [45], Leung et al. [21], Larsson et al. [22], Rao et al. [26], Al-Haddad et al. [67], Rotruck et al. [18], Chen et al. [49], and Ali et al. [44].
However, greater values in the right eye were reported as follows: Queiros et al. [28] and Pawar et al. [59]—temporal RNFL quadrant, and Dave et al. [68]—temporal superior, nasal superior, and temporal RNFL sectors.
Other results show higher values of RNFL parameters in the left eye: Qian et al. [69]—for the thicknesses of superior and nasal RNFL sectors, Queiros et al. [28]—superior RNFL quadrant, and Pawar et al. [59]—superior RNFL quadrant.
Few studies assessed the differences between the maculae of the right and the left eye or between the dominant and nondominant eye, and the results showed no statistically significant differences [28, 38, 40].
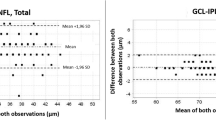
Altemir et al. [70] recommended that the interocular differences in average RNFL thickness should not exceed 13 µm, and the differences in the macular thickness should not measure more than 23 µm.
The average RNFL thickness and the macular thickness did not show differences between the right and the left eye, but the temporal sector of RNFL was thicker in the right eye, whereas the superior sector of RNFL was thicker in the left eye. These findings imply that in future research either eye can be randomly chosen if the average RNFL or macular thicknesses are studied, but for the sectorial RNFL thicknesses the difference between the right and the left eye should be considered.
Influence of the ISNT rule on OCT parameters
The order of decreasing thicknesses of the RNFL quadrants (i.e., I = inferior, S = superior, N = nasal, T = temporal) was reported as follows:
-
(1)
I > S > N > T: Salchow et al. [45], Elia et al. [24], Al-Haddad et al. [27], Queiros et al. [28], Pawar et al. [59], Larsson et al. [2], Gama et al. [71], Rotruck et al. [18], Bhoiwala et al. [72], and Ali et al. [44].
-
(2)
S > I > N > T: Huynh et al. [12], Pawar et al. [23], Rao et al. [26], and Yanni et al. [17].
-
(3)
S > I > T > N: Ahn et al. [20], Leung et al. [21], Larsson et al. [22], Qian et al. [69], Chen et al. [49], and Zhu et al. [33].
-
(4)
I > S > T > N: Turk et al. [30], Perez-Garcia et al. [31], Tsai et al. [73], and Kang et al. [60].
Dave et al. [74] also reported the prevalence of the rule in their participants: I > S > N > T (23.8%); I > S > T (52.4%); S > I (45.2%); T > N (50%).
The ISNT rule was first described on optic disc photographs for the neuroretinal rim thicknesses [75], and it was reported that the eyes of patients with glaucoma do not follow this rule. Later OCT studies also investigated the ISNT rule for the sectorial RNFL thicknesses, mostly in adults [74].
As shown, the results reported by studies conducted on paediatric participants demonstrate high variability, so the disobedience of the ISNT rule cannot be interpreted as abnormal.
Influence of spherical equivalent and ocular axial length on OCT parameters
A positive correlation between spherical equivalent of refractive error and average RNFL thickness was observed in several studies: Salchow et al. [45], Huynh et al. [12], Jun and Lee [76], Qian et al. [69], Tas et al. [58], Pawar et al. [23], Barrio-Barrio et al. [25], Rao et al. [26], Al-Haddad et al. [27], Queiros et al. [28], Bueno-Gimeno et al. [77], Lee et al. [46], Eslami et al. [32], Tsai et al. [73], Chen et al. [49], Zhu et al. [33], Kang et al. [60], and Ayala and Ntoula [35]. A few papers found no correlation between spherical equivalent and average RNFL thickness: Goh et al. [48], Larsson et al. [2], Gama et al. [71], and Ali et al. [44].
No significant effect of refractive error on optic nerve head parameters was found, as reported by Samarawickrama et al. [78], Patel et al. [8], Bueno-Gimeno et al. [77], Larsson et al. [2], and Ali et al. [44].
For the macular region, a positive correlation between spherical equivalent and various regional OCT parameters was observed [25, 29, 34, 37, 42,43,44, 48, 52, 54, 77, 79, 80]. On the other hand, Queiros et al. [28] and Sultan et al. [80] found a negative correlation with central macular thickness, whereas Molnar et al. [38] and Gama et al. [71] found no correlation at all with the investigated macular parameters.
The majority of papers investigating the possible association between ocular axial length and average RNFL thickness observed a negative correlation: Huynh et al. [12], Jun and Lee [76], Leung et al. [21], Tas et al. [58], Rao et al. [26], Oner et al. [81], Bueno-Gimeno et al. [77], Lee et al. [46], Aykut et al. [82], Chen et al. [49], Zhu et al. [33], Kang et al. [60], and Ali et al. [44]. Two studies found no correlation with average RNFL thickness [9, 48].
For the macular OCT parameters, three types of results were obtained:
-
(1)
Positive correlation: Huynh et al. [11] and Bueno-Gimeno et al. [77]—for central macular thickness; Goh et al. [48]—for the ganglion cell—inner plexiform layer thickness; Ali et al. [44]—for the thickness of the temporal outer sector.
-
(2)
Negative correlation: Luo et al. [79]—for total macular volume, and outer and inner macular volume; Galdos et al. [52] and Totan et al. [53]—for the ganglion cell—inner plexiform layer thickness; Guragac et al. [29] and Bueno-Gimeno et al. [77]—for the average macular thickness and volume; Yabas Kiziloglu et al. [34]—for the thicknesses of the temporal, inferior and nasal outer macular sectors; Ali et al. [44]—for the thicknesses of the superior and inferior inner sectors.
-
(3)
No correlation: Lim et al. [9]—for the ganglion cell complex volume; Barrio-Barrio et al. [25]—total macular thickness; Lee et al. [43]—for the ganglion cell—inner plexiform layer thickness; Ali et al. [44]—for the macular volume, average macular volume, central macular thickness.
A positive correlation between spherical equivalent of refractive error and RNFL thickness was observed by the majority of papers, whereas the measurements of optic nerve head parameters (e.g., optic disc size, and cup/disc ratio) did not correlate with the spherical equivalent. Inconsistent results were reported for the macular parameters, and also for the relation between OCT results and ocular axial length.
Ocular magnification effect was incriminated to affect these results: the distance between the instrument and the examined tissue can vary from eye to eye and thus influence the measurements. However, the magnification effect may exert influence only on the lateral measurements, i.e. the measurements made parallel to the retinal plane, which eventually affect the calculation of area or volume [83, 84]. The axial measurements (e.g., macular thickness evaluation) should not be influenced by this optical effect [84]. For the RNFL assessment, the thickness measurement itself is not affected by the ocular magnification, but the distance between the scanning circle and the optic nerve head can vary: all the OCT devices use a predefined diameter of the scanning circle, so the RNFL thickness values can indirectly be influenced by this effect.
The great variability of the results reported in the evaluated papers is given by the various methodologies employed: some authors included adjustments for ocular magnification (e.g., Bueno-Gimeno et al. [77], and Read et al. [41]), whereas other authors did not (e.g., Bhoiwala et al. [72] and Sultan et al. [80]). Moreover, there is debate between those who used a correction for ocular magnification on which formula is better to be used [49].
However, the presentation of differences between OCT instruments and the review of physical principles behind the ocular magnification effect are beyond the scope of this paper. What is relevant from the clinician’s point of view is that the ocular magnification effect can influence the lateral measurements in the child’s growing eye and the issue is not yet fully addressed by the OCT manufacturers.
Limitations of our review
We did not take into consideration the studies assessing the choroid thickness, the OCT angiography studies, or the papers in which anterior segment OCT was employed. We chose to include only the posterior pole OCT examinations because these are the most frequently used in the clinical practice.
The minimum number of participants enroled in the studies to be included in this analysis was arbitrarily chosen. To the best of our knowledge, there is no consensus regarding the minimum number of participants (or eyes) enroled for the study of the normal range values of the OCT parameters. However, the total number of participants for each study included in this review can be found in Table 2.
Conclusions
The general conclusions of our analysis on the normal OCT results in the paediatric population are:
-
(1)
Average RNFL thickness is not influenced by age, gender, or eye laterality.
-
(2)
Macular thickness should be considered separately for children aged <5 and children aged >5.
-
(3)
Central macular thickness has a tendency towards higher values in boys.
-
(4)
Temporal RNFL sector is thicker in the right eye.
-
(5)
Superior RNFL sector is thicker in the left eye.
-
(6)
Macular thickness is not significantly different between the right and the left eye.
-
(7)
The ISNT rule is not necessarily valid.
-
(8)
RNFL thickness increases as the spherical equivalent of refractive error increases.
-
(9)
The optic nerve head OCT parameters are not influenced by the refractive error.
-
(10)
Ocular axial length can have an effect on the ocular magnification, and thus influence the lateral OCT measurements.
-
(11)
Handheld OCT devices are a good alternative for young or uncooperative children.
References
Maccora KA, Sheth S, Ruddle JB. Optical coherence tomography in paediatric clinical practice. Clin Exp Optom. 2019;102:300–8.
Larsson E, Molnar A, Holmstrom G. Repeatability, reproducibility and interocular difference in the assessment of optic nerve OCT in children—a Swedish population-based study. BMC Ophthalmol. 2018;18:270.
Fard MA, Fakhree S, Eshraghi B. Correlation of optical coherence tomography parameters with clinical and radiological progression in patients with symptomatic optic pathway gliomas. Graefes Arch Clin Exp Ophthalmol. 2013;251:2429–36.
Moher D, Liberati A, Tetzlaff J, Altman DG—The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses. PLoS Med. 2009;6:e1000097. https://doi.org/10.1371/journal.pmed1000097.
Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R et al. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z, editors. Joanna Briggs Institute Reviewer’s Manual. The Joanna Briggs Institute; 2017. https://reviewersmanual.joannabriggs.org/.
Allingham MJ, Cabrera MT, O’Connell RV, Maldonado RS, Tran-Viet D, Toth CA, et al. Racial variation in optic nerve head parameters quantified in healthy newborns by handheld spectral domain optical coherence tomography. J AAPOS. 2013;17:501–6.
Rothman AL, Sevilla MB, Freedman SF, Tong AY, Tai V, Tran-Viet D, et al. Assessment of retinal nerve fiber layer thickness in healthy, full-term neonates. Am J Ophthalmol. 2015;159:803–11.
Patel A, Purohit R, Lee H, Sheth V, Maconachie G, Papageorgiou E, et al. Optic nerve head development in healthy infants and children using handheld spectral-domain optical coherence tomography. Ophthalmology. 2016;123:2147–57.
Lim ME, Jiramongkolchai K, Xu L, Freedman SF, Tai V, Toth CA, et al. Handheld optical coherence tomography normative inner retinal layer measurements for children <5 years of age. Am J Ophthalmol. 2019;207:232–9.
Early Treatment Diabetic Retinopathy Study Research Group. Grading diabetic retinopathy from stereoscopic color fundus photographs—an extension of the modified Airlie House classification. ETDRS report number 10. Ophthalmology. 1991;98:786–806.
Huynh SC, Wang XY, Rochtchina E, Mitchell P. Distribution of macular thickness by optical coherence tomography: findings from a population-based study of 6-year-old children. Investig Ophthalmol Vis Sci. 2006;47:2351–7.
Huynh SC, Wang XY, Rochtchina E, Mitchell P. Peripapillary retinal nerve fiber layer thickness in a population of 6-year-old children. Ophthalmology. 2006;113:1583–92.
Huynh SC, Wang XY, Rochtchina E, Crowston JG, Mitchell P. Distribution of optic disc parameters measured by OCT: findings from a population-based study of 6-year-old Australian children. Investig Ophthalmol Vis Sci. 2006;47:3276–85.
El-Dairi MA, Asrani SG, Enyedi LB, Freedman SF. Optical coherence tomography in the eyes of normal children. Arch Ophthalmol. 2009;127:50–8.
Tariq YM, Samarawickrama C, Pai A, Burlutsky G, Mitchell P. Impact of ethnicity on the correlation of retinal parameters with axial length. Investig Ophthalmol Vis Sci. 2010;51:4977–82.
Samarawickrama C, Wang JJ, Huynh SC, Pai A, Burlutsky G, Rose KA, et al. Ethnic differences in optic nerve head and retinal nerve fiber layer thickness parameters in children. Br J Ophthalmol. 2010;94:871–6.
Yanni SE, Wang J, Cheng CS, Locke KI, Wen Y, Birch DG, et al. Normative reference ranges for the retinal nerve fiber layer, macula, and retinal layer thicknesses in children. Am J Ophthalmol. 2013;155:354–60.
Rotruck JC, House RJ, Freedman SF, Kelly MP, Enyedi LB, Prakalapakorn SG, et al. Optical coherence tomography normative peripapillary retinal nerve fiber layer and macular data in children ages 0-5 years. Am J Ophthalmol. 2019;208:323–30.
Bourne RRA. Ethnicity and ocular imaging. Eye. 2011;25:297–300.
Ahn HC, Son HW, Kim JS, Lee JH. Quantitative analysis of retinal nerve fiber layer thickness of normal children and adolescents. Korean J Ophthalmol. 2005;19:195–200.
Leung MMP, Huang RYC, Lam AKC. Retinal nerve fiber layer thickness in normal Hong Kong Chinese children measured with optical coherence tomography. J Glaucoma. 2010;19:95–9.
Larsson E, Eriksson U, Alm A. Retinal nerve fibre layer thickness in full-term children assessed with Heidelberg retinal tomography and optical coherence tomography: normal values and interocular asymmetry. Acta Ophthalmol. 2011;89:151–8.
Pawar N, Maheshwari D, Ravindran M, Ramakrishnan R. Retinal nerve fiber layer thickness in normal Indian pediatric population measured with optical coherence tomography. Indian J Ophthalmol. 2014;62:412–8.
Elia N, Pueyo V, Altemir I, Oros D, Pablo LE. Normal reference ranges of optical coherence tomography parameters in childhood. Br J Ophthalmol. 2012;96:665–70.
Barrio-Barrio J, Noval S, Galdos M, Ruiz-Canela M, Bonet E, Capote M, et al. Multicenter Spanish study of spectral-domain optical coherence tomography in normal children. Acta Ophthalmol. 2013;91:e56–63.
Rao A, Sahoo B, Kumar M, Varshney G, Kumar R. Retinal nerve fiber layer thickness in children <18 years by spectral-domain optical coherence tomography. Semin Ophthalmol. 2013;28:97–102.
Al-Haddad C, Barikian A, Jaroudi M, Massoud V, Tamim H, Noureddin B. Spectral domain optical coherence tomography in children: normative data and biometric correlations. BMC Ophthalmol. 2014;14:53.
Queiros T, Freitas C, Guimaraes S. Normative database of optical coherence tomography parameters in childhood. Acta Med Port. 2015;28:148–57.
Guragac FB, Totan Y, Guler E, Tenlik A, Ertugrul IG. Normative spectral domain optical coherence tomography data in healthy Turkish children. Semin Ophthalmol. 2017;32:216–22.
Turk A, Ceylan OM, Arici C, Keskin S, Erdurman C, Durukan AH, et al. Evaluation of the nerve fiber layer and macula in the eyes of healthy children using spectral-domain optical coherence tomography. Am J Ophthalmol. 2012;153:552–9.
Perez-Garcia D, Ibanez-Alperte J, Remon L, Cristobal JA, Sanchez-Cano A, Pinilla I. Study of spectral-domain optical coherence tomography in children: normal values and influence of age, sex, and refractive status. Eur J Ophthalmol. 2016;26:135–41.
Eslami Y, Vahedian Z, Moghimi S, Bazvand F, Salari H, Shahabinejad M, et al. Peripapillary retinal nerve fiber layer thickness in normal Iranian children measured with optical coherence tomography. J Ophthalmic Vis Res. 2018;13:453–7.
Zhu BD, Li SM, Li H, Liu LR, Wang Y, Yang Z, et al. Retinal nerve fiber layer thickness in a population of 12-year-old children in central China measured by iVue-100 spectral-domain optical coherence tomography: The Anyang Childhood Eye Study. Investig Ophthalmol Vis Sci. 2013;54:8104–11.
Yabas Kiziloglu O, Toygar O, Toygar B, Hacimustafaoglu AM. Retinal nerve fiber layer and macula thickness with spectral domain optical coherence tomography in children: normal values, repeatability and the influence of demographic and ocular parameters. Turkiye Klinikleri J Ophthalmol. 2018;27:28–34.
Ayala M, Ntoula E. Retinal fibre layer thickness measurement in normal paediatric population in Sweden using optical coherence tomography. J Ophthalmol. 2016;2016:4160568.
Eriksson U, Holmstrom G, Alm A, Larsson E. A population-based study of macular thickness in full-term children assessed with Stratus OCT: normative data and repeatability. Acta Ophthalmol. 2009;87:741–5.
Zhang Z, He X, Zhu J, Jiang K, Zheng W, Ke B. Macular measurements using optical coherence tomography in healthy Chinese school age children. Investig Ophthalmol Vis Sci. 2011;52:6377–83.
Molnar A, Holmstrom G, Larsson E. Macular thickness assessed with spectral domain OCT in a population-based study of children: normative data, repeatability and reproducibility and comparison with time domain OCT. Acta Ophthalmol. 2015;93:470–5.
Sushil O, Vaibhav J, Reena S, Brijesh S, Dipendra S. OCT normative database of macula in the paediatric population. Indian J Clin Exp Ophthalmol. 2015;1:238–44.
Nigam B, Garg P, Ahmad L, Mullick R. OCT based macular thickness in a normal Indian pediatric population. J Ophthalmic Vis Res. 2018;13:144–8.
Read SA, Alonso-Caneiro D, Vincent SJ. Longitudinal changes in macular retinal layer thickness in pediatric populations: myopic vs non-myopic eyes. PLoS ONE. 2017;12:e0180462.
Munoz-Gallego A, De la Cruz J, Rodriguez-Salgado M, Torres-Pena JL, Lucas-Viejo B, Ortueta-Olartecoechea A, et al. Assessment of macular ganglion cell complex using optical coherence tomography: Impact of a paediatric reference database in clinical practice. Clin Exp Ophthalmol. 2018;47:490–7.
Lee YP, Ju YS, Choi DG. Ganglion cell-inner plexiform layer thickness by swept-source optical coherence tomography in healthy Korean children: normative data and biometric correlations. Sci Rep. 2018;8:10605.
Ali AN, Farag RK, El Wahab TAA, Ghanem AA, Hababeh M. Macular and retinal nerve fiber layer analysis by optical coherence tomography in normal children. ARC J Ophthalmol. 2018;3:17–28.
Salchow DJ, Oleynikov YS, Chiang MF, Kennedy-Salchow SE, Langton K, Tsai JC, et al. Retinal nerve fiber layer thickness in normal children measured with optical coherence tomography. Ophthalmology. 2006;113:786–91.
Lee JWY, Yau GSK, Woo TTY, Yick DWF, Tam VTY, Lai JSM. Retinal nerve fiber layer thickness in myopic, emmetropic, and hyperopic children. Medicine. 2015;94:e699.
Hong SW, Ahn YJ, Kang NY. Relationship between age and retinal nerve fiber layer thickness in normal children. Semin Ophthalmol. 2017;32:655–60.
Goh JP, Koh V, Chan YH, Ngo C. Macular ganglion cell and retinal nerve fiber layer thickness in children with refractive errors—an optical coherence tomography study. J Glaucoma. 2017;26:619–25.
Chen L, Huang J, Zou H, Xue W, Ma Y, He X, et al. Retinal nerve fiber layer thickness in normal Chinese students aged 6 to 17 years. Investig Ophthalmol Vis Sci. 2013;54:7990–7.
Huynh SC, Wang XY, Burlutsky G, Rochtchina E, Stapleton F, Mitchell P. Retinal and optic disc findings in adolescence: a population-based OCT study. Investig Ophthalmol Vis Sci. 2008;49:4328–35.
Katiyar V, Mugdha K, Bangwal S, Gupta SK. Normative macular Cirrus spectral domain optical coherence tomography data in Indian pediatric population. Egypt Retin J. 2013;1:50–55.
Galdos M, Barrio-Barrio J, Noval S, Ruiz-Canela M, Bonet E, Capote M, et al. Multicenter macular ganglion cell analysis: normative paediatric reference range. Acta Ophthalmol. 2014;92:e326–7.
Totan Y, Guragac FB, Guler E. Evaluation of the retinal ganglion cell layer thickness in healthy Turkish children. J Glaucoma. 2015;24:e103–8.
Passani A, Sframeli AT, Posarelli C, Lisi D, Guidi G, Casini G, et al. Macular spectral-domain optical coherence tomography values and correlations in healthy children. Int Ophthalmol. 2019;39:2449–57.
Read SA, Collins MJ, Vincent SJ, Alonso-Caneiro D. Macular retinal layer thickness in childhood. Retina. 2015;35:1223–33.
Parikh RS, Parikh SR, Sekhar GC, Prabakaran S, Babu JG, Thomas R. Normal age-related decay of retinal nerve fiber layer thickness. Ophthalmology. 2007;114:921–6.
Alabduljalil T, Westall CA, Reginald A, Farsiu S, Chiu SJ, Arshavsky A, et al. Demonstration of anatomical development of the human macula within the first 5 years of life using handheld OCT. Int Ophthalmol. 2019;39:1533–42.
Tas M, Oner V, Turkcu FM, Alakus MF, Simsek A, Iscan Y, et al. Peripapillary retinal nerve fiber layer thickness in hyperopic children. Optom Vis Sci. 2012;89:1009–13.
Pawar N, Maheshwari D, Ravindran M, Ramakrishnan R. Interocular symmetry of retinal nerve fiber layer and optic nerve head parameters measured by Cirrus high-definition optical coherence tomography in a normal pediatric population. Indian J Ophthalmol. 2017;65:955–62.
Kang MT, Li SM, Li H, Li L, Li SY, Zhu BD, et al. Peripapillary retinal nerve fiber layer thickness and its association with refractive error in Chinese children: the Anyang Childhood Eye Study. Clin Exp Ophthalmol. 2016;44:701–9.
Chen S, Wang B, Dong N, Ren X, Zhang T, Xiao L. Macular measurements using spectral-domain optical coherence tomography in Chinese myopic children. Investig Ophthalmol Vis Sci. 2014;55:7410–6.
Wong AC, Chan CW, Hui SP. Relationship of gender, body mass index, and axial length with central retinal thickness using optical coherence tomography. Eye. 2005;19:292–7.
Wexler A, Sand T, Elsas TB. Macular thickness measurements in healthy Norwegian volunteers: an optical coherence tomography study. BMC Ophthalmol. 2010;10:13.
Sole Gonzalez L, Abreu Gonzalez R, Alonso Plasencia M, Abreu, Reyes P. Normal macular thickness and volume using spectral domain optical coherence tomography in a reference population. Arch Soc Esp Oftalmol. 2013;88:352–8.
Cubuk M, Sahinoglu-Keskek N, Keskek SO. Retinal nerve fiber layer thickness in a healthy Turkish population measured by optical coherence tomography. Ann Saudi Med. 2016;36:409–13.
Cubuk M, Kasim B, Kocluk Y, Sukgen EA. Effects of age and gender on macular thickness in healthy subjects using spectral optical coherence tomography/scanning laser ophthalmoscopy. Int Ophthalmol. 2018;38:127–31.
Al-Haddad C, Antonios R, Tamim H, Noureddin B. Interocular symmetry in retinal and optic nerve parameters in children as measured by spectral domain optical coherence tomography. Br J Ophthalmol. 2014;98:502–6.
Dave P, Jethani J, Shah J. Asymmetry of retinal nerve fiber layer and posterior pole asymmetry analysis parameters of spectral domain optical coherence tomography in children. Semin Ophthalmol. 2017;32:443–8.
Qian J, Wang W, Zhang X, Wang F, Jiang Y, Wang W, et al. Optical coherence tomography measurements of retinal nerve fiber layer thickness in Chinese children and teenagers. J Glaucoma. 2011;20:509–13.
Altemir I, Oros D, Elia N, Polo V, Larrosa JM, Pueyo V. Retinal asymmetry in children measured with optical coherence tomography. Am J Ophthalmol. 2013;156:1238–43.
Gama R, Santos JC, Costa RS, Costa DC, Eiro N. Optical coherence tomography analysis of the inner retinal layers in children. Can J Ophthalmol. 2018;53:614–20.
Bhoiwala DL, Simon JW, Raghu P, Krishnamoorthy M, Todani A, Gandham SB, et al. Optic nerve morphology in normal children. J AAPOS. 2015;19:531–4.
Tsai DC, Huang N, Hwu JJ, Jueng RN, Chou P. Estimating retinal nerve fiber layer thickness in normal schoolchildren with spectral-domain optical coherence tomography. Jpn J Ophthalmol. 2012;56:362–70.
Dave P, Jethani J, Shah J. Applicability of the ISNT and IST rules on retinal nerve fiber layer measurement on spectral-domain optical coherence tomography in normal Indian children. Graefes Arch Clin Exp Ophthalmol. 2015;253:1795–9.
Jonas JB, Gusek GC, Naumann GOH. Optic disc, cup and neuroretinal rim size, configuration, and correlations in normal eyes. Investig Ophthalmol Vis Sci. 1998;29:1151–8.
Jun JH, Lee SY. The effects of optic disc factors on retinal nerve fiber layer thickness measurement in children. Korean J Ophthalmol. 2008;22:115–22.
Bueno-Gimeno I, Espana-Gregori E, Gene-Sampedro A, Ondategui-Parra JC, Zapata-Rodriguez CJ. Variations of OCT measurements corrected for the magnification effect according to axial length and refractive error in children. J Innov Opt Health Sci. 2018;1:185001.
Samarawickrama C, Wang XY, Huynh SC, Burlutsky G, Stapleton F, Mitchell P. Effects of refraction and axial length on childhood optic disk parameters measured by optical coherence tomography. Am J Ophthalmol. 2007;144:459–61.
Luo HD, Gazzard G, Fong A, Aung T, Hoh ST, Loon SC, et al. Myopia, axial length, and OCT characteristics of the macula in Singaporean children. Investig Ophthalmol Vis Sci. 2006;47:2773–81.
Sultan M, Hamza SA, Shah MA, Khan MN, Saeed N. Comparison of macular thickness between highly myopic and normal children aged 5 to 8 years using optical coherence tomography. J Postgrad Med Inst. 2018;32:76–9.
Oner V, Ozgur G, Turkyilmaz K, Sekeryapan B, Durmus M. Effect of axial length on retinal nerve fiber layer thickness in children. Eur J Ophthalmol. 2014;24:265–72.
Aykut V, Oner V, Tas M, Iscan Y, Agachan A. Influence of axial length on peripapillary retinal nerve fiber layer thickness in children: a study by RTVue spectral-domain optical coherence tomography. Curr Eye Res. 2013;38:1241–7.
Ctori I, Gruppetta S, Huntjens B. The effects of ocular magnification on Spectralis spectral domain optical coherence tomography scan length. Graefe Arch Clin Exp Ophthalmol. 2015;253:733–8.
Salmon AE, Sajdak BS, Atry F, Carroll J. Axial scaling is independent of ocular magnification in OCT images. Investig Ophthalmol Vis Sci. 2018;59:3037–40.
Samarawickrama C, Wang JJ, Huynh SC, Wang XY, Burlutsky G, Stapleton F, et al. Macular thickness, retinal thickness, and optic disk parameters in dominant compared with nondominant eyes. J AAPOS. 2009;13:142–7.
Tariq YM, Pai A, Li H, Afsari S, Gole GA, Burlutsky G, et al. Association of birth parameters with OCT measured macular and retinal nerve fiber layer thickness. Investig Ophthalmol Vis Sci. 2011;52:1709–15.
Yau GSK, Lee JWY, Woo TTY, Wong RLM, Wong IYH. Central macular thickness in children with myopia, emmetropia, and hyperopia: an optical coherence tomography study. Biomed Res Int. 2015;2015:847694.
Lee JWY, Yau GSK, Woo TTY, Lai JSM. The association between macular thickness and peripapillary retinal nerve fiber layer thickness in Chinese children. Medicine. 2015;94:e567.
Grundy SJ, Tshering L, Wanjala SW, Diamond MB, Audi MS, Prasad S, et al. Retinal parameters as compared with head circumference, height, weight, and body mass index in children in Kenya and Bhutan. Am J Trop Med Hyg. 2018;99:482–8.
Yabas Kiziloglu O, Toygar O, Toygar B, Hacimustafaoglu AM. Optic nerve head parameters measured with spectral-domain optical coherence tomography in healthy Turkish children: normal values, repeatability, and interocular symmetry. Neuro-Ophthalmology. 2018;42:83–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Banc, A., Ungureanu, M.I. Normative data for optical coherence tomography in children: a systematic review. Eye 35, 714–738 (2021). https://doi.org/10.1038/s41433-020-01177-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01177-3
- Springer Nature Limited
This article is cited by
-
Fairness and generalizability of OCT normative databases: a comparative analysis
International Journal of Retina and Vitreous (2023)
-
Reference database of total retinal vessel surface area derived from volume-rendered optical coherence tomography angiography
Scientific Reports (2022)
-
Visual perception and macular integrity in non-classical CLN2 disease
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)