Abstract
Objectives
To review the 3-year follow-up results of subthreshold micropulse yellow laser (SMYL) delivered by a short-duration multiple-session method for treatment of chronic central serous chorioretinopathy (CSC).
Methods
A total of 27 eyes from 27 patients with chronic CSC available for 3 years of follow-up were enrolled in this retrospective and interventional study. Patients were treated with 577-nm SMYL photocoagulation at a 15% duty cycle over multiple sessions, with low power ranging from 200 to 400 mW that was increased in 100 mW increments according to resolution of subretinal fluid at monthly follow-up. Laser titration was not performed. A treatment duration of 20 ms rather than the conventional duration (100–300 ms) was applied over the area of retinal pigment epithelium leakage and all areas of serous retinal detachment, including the fovea.
Results
The mean follow-up period was 3.7 ± 0.8 years (range, 3–6 years). A total of 22 out of 27 eyes (81.5%) including six cases of recurrence during the follow-up period exhibited complete resolution of subretinal detachment at final follow-up, whereas only five eyes (15.5%) had either a partial or null response to SMYL treatment. The baseline best-corrected visual acuity was 0.26 ± 0.24 logarithm of the minimum angle of resolution (logMAR), which was improved to 0.08 ± 0.15 logMAR at 1-year (p = 0.005) and 3-year (p = 0.01) follow-up. The central macular thickness at baseline was 389.6 ± 103.4 μm, which was changed to 197.2 ± 40.0 μm (p < 0.001) at 1-year follow-up, 196.4 ± 40.2 μm (p < 0.001) at 3-year follow-up.
Conclusion
Short-duration multiple-session SMYL therapy may be effective for long-term treatment of chronic CSC.
Similar content being viewed by others
Introduction
Central serous chorioretinopathy (CSC) was first described in 1866 by Albrecht von Graefe, who named it “relapsing central luetic retinitis” [1]. CSC was appropriately renamed by Gass in 1967 [2]. CSC is characterized by neurosensory detachment with or without concomitant pigment epithelial detachment [3] and remains an idiopathic disorder with systemic associations and a multifactorial etiology. Many cases of CSC resolve spontaneously without treatment after a period of observation [4]; however, some patients with chronic neurosensory retinal detachment or frequent recurrence may develop atrophy of the retinal pigment epithelium (RPE) and neurosensory retinal atrophic changes, resulting in permanent loss of visual function, including visual acuity (VA), color vision, and contrast sensitivity [5,6,7,8]. In these cases, treatment options include focal laser treatment, photodynamic therapy, and intravitreal injection of anti-vascular endothelial growth factor (VEGF) [9].
Conventional lasers can cause thermal burns in the retina and can put patients at risk of developing scotoma, long-term focal scar expansion, choroidal neovascularization (CNV), and potential new sites of leakage [10]. On the other hand, photodynamic therapy (PDT) has shown promising results in the treatment of chronic CSC, but is associated with several side effects including choroidal ischemia, tearing or atrophy of the RPE, and iatrogenic CNV [11,12,13,14,15]. Likewise, the evidence supporting intravitreal anti-VEGF agents for the management of CSC is poor [16,17,18,19], except in cases where secondary CNV is present.
Non-damaging retinal laser therapy, also called subthreshold laser therapy, does not cause collateral tissue damage. Instead, this promising new technology raises the temperature of the RPE to just below the threshold for protein denaturation, thereby limiting transmission of thermal energy to the neurosensory retina and preventing formation of a visible burn. Mechanistically, subthreshold laser treatment is thought to stimulate a metabolic effect whereby the retinal tissue produces mediators with anti-angiogenic and anti-edema effects, such as pigment epithelium-derived factor, β-actin, and thrombospondin 1. Subthreshold laser therapy is also hypothesized to improve RPE function by stimulating the upregulation of heat-shock proteins [20, 21]. Advantages of subthreshold laser therapy include the ability to apply treatment near the fovea as well as the ability to treat the same area multiple times.
Application of subthreshold micropulse laser (SML) in the setting of CSC has been previously described [9, 21,22,23,24,25,26]. According to previous studies, the laser duty cycle is typically set between 5 and 15%, representing an “on” time of 0.15–0.30 ms during each 2-ms treatment period. These 2-ms periods are repeated for the duration of the burst exposure, which typically lasts between 100 and 300 ms. Titration is usually employed with this approach to establish proper laser power [26].
In the present study, we evaluated the effects of 577 nm subthreshold micropulse yellow laser (SMYL) for the treatment of chronic CSC at a 3-year follow-up. The settings for SMYL photocoagulation consisted of a 15% duty cycle, multiple sessions, low power from 200 to 400 mW increased by 100 mW depending on the resolution of the subretinal fluid (SRF) at monthly follow-up, and a 20 ms treatment duration, which differed from that of the conventional duration of 100–300 ms. Our motivation for using lower energy SMYL was to achieve truly sub-visible treatment in order to avoid RPE damage without the use of a test burn. To the best of our knowledge, this is the study to report the longest follow-up results of SML for the treatment of chronic CSC.
Materials and methods
We performed a retrospective and interventional study of 27 eyes from 27 patients who received SMYL photocoagulation for chronic or chronic recurrent CSC at Nune Eye Hospital (Daegu, Republic of Korea) between July 2011 and October 2017. This study adhered to the ethical standards in the Declaration of Helsinki. It was approved by Nune Eye Hospital Institutional Review Board. Informed consent was obtained from all individual participants included in the study. The inclusion criteria for this study were as follows: (1) patients with symptomatic CSC lasting 3 months or longer, (2) patients with recurrent CSC and a history of chronic CSC, (3) patients who received SMYL treatment for CSC, and (4) patients with at least 3 years of follow-up data. The exclusion criteria consisted of (1) a history of other macular disease such as age-related macular degeneration, retinal vascular occlusion, diabetic retinopathy, or epiretinal membrane, (2) patients who had received anti-VEGF treatment or conventional thermal laser in the past 6 months before SMYL treatment, (3) patients with a history of PDT or intraocular surgery, (4) and patients who were not followed for at least 3 years after undergoing SMYL therapy.
All patients underwent ophthalmic examinations, including anterior segment examination and dilated biomicroscopic fundus examination. Best-corrected visual acuity (BCVA) was measured using the Snellen visual acuity (VA) chart. BCVA was converted to logarithm of the minimum angle of resolution (logMAR) units for statistical analysis. Color fundus photography and fluorescein angiography (Spectralis HRA; Heidelberg Engineering, Heidelberg, Germany) were performed prior to initiating SMYL treatment. Central macular thickness (CMT) was measured using spectral-domain optical coherence tomography (SD-OCT) (Spectralis OCT; Heidelberg Engineering) before SMYL treatment and at every follow-up visit.
SMYL treatment was performed by a single retina specialist (HS Park) with the 577-nm yellow laser system (Supra Scan, Quantel Medical, Cedex, France). Laser application was performed with a Mainster macular contact lens (Ocular Instruments, Mentor, OH, USA, laser spot magnification ×1.05). All patients were treated using a multiple-session format with the following SMYL settings: 100-µm spot diameter, 20-ms duration, 15% duty cycle, and low power ranging from 200 to 400 mW that was incrementally increased by 100 mW depending on the resolution of the SRF at monthly follow-up visits. SMYL photocoagulation was applied in 3 × 3 pattern mode (0.5 widths) over the area of RPE leakage and all area of serous retinal detachment, including the fovea.
BCVA, CMT measured by SD-OCT, and treatment responses were evaluated at every follow-up. If the SRF was not completely resolved within 1 month of SMYL treatment, additional photocoagulation was delivered monthly until the SRF was completely resolved. Patients with recurrent CSC received SMYL photocoagulation after complete resolution of SRF by initial SMYL treatment during the follow-up period. If SRF was not completely resolved (either no response or partial response) after multiple sessions of SMYL photocoagulation, other treatment options such as PDT and anti-VEGF were utilized. Treatment failure (no response) was defined as the SRF was reduced by <50% or increased comparing the preceding treatment result, even though the laser energy was increased from 200 to 400 every month. Partial response was defined as the SRF was reduced by more than 50%, but not completely resolved comparing the preceding treatment result.
We analyzed the changes in mean BCVA and CMT from baseline to final follow-up. The number of recurring CSC cases after initial treatment and the incidence of adverse events were counted. Sample size was calculated by using a power 80% and a two-sided level of significance of 5%, and adjusted by t-distribution. Data are presented as mean ± standard deviation. The normal distribution of variables will be verified by the Kolgomorov–Smirnov test for continuous variables. Post-treatment values were compared with the baseline values using repeated-measures ANOVA (analysis of variance). To check for sphericity, the variances of the differences between all combinations of groups of within-subjects factors will be analyzed with the Mauchly test. Post hoc analyses of significant group × time interaction effects will be carried out using the Tukey's multiple comparison procedure to examine pairwise comparisons of the groups’ means for all outcome measures and across the seven data collection times. A p value of 0.05 will be used for statistical significance. Statistical analysis was performed using SPSS ver. 21.0 (SPSS Inc., Chicago, IL, USA).
Results
A total of 27 eyes from 27 patients met the inclusion criteria for our study and were treated with 577-nm SMYL. The mean patient age at the time of diagnosis was 45.1 ± 8.6 years (range, 30–62 years). A total of 24 patients were male (88.9%) and 3 patients were female (11.2%). Five patients had a history of anti-VEGF treatment at least 6 months before SMYL photocoagulation. The mean follow-up period was 3.7 ± 0.8 years (range, 3–6 years). Baseline characteristics of patients of this study were shown in Table 1. The mean number of treatment sessions was 2.5 ± 1.5 (range, 1–7), which included both initial treatment and repeat treatment due to recurrence.
A total of 22 out of 27 eyes (81.5%) showed complete resolution of SRF at the final follow-up, which included six cases of recurrence during the follow-up period. Conversely, there were five eyes (15.5%) that showed either no response or partial response to SMYL treatment. Complete resolution after initial SMYL treatment was achieved in 16 of 27 eyes (59.3%), with no evidence of recurrence at the final follow-up (Fig. 1). The mean number of treatment sessions in patients who achieved complete resolution after initial treatment was 2.2 ± 1.2 (range, 1–4). Four cases in this group received four times SMYL in initial treatment period with laser power from 200 to 400 mW, and the third and fourth treatments were performed with 400 mW. Six (22.2%) eyes exhibited recurrence of SRF after evidence of complete resolution during follow-up, and all six responded to repeat SMYL photocoagulation therapy. In the recurrence group (n = 6), the number of SMYL sessions for re-treatment was one in three eyes and two in the other three eyes. And four of six eyes in recurrent cases during follow-up were retreated with 400 mW power till the SRF resolved. The mean period of SRF resolution after SMYL treatment in complete resolution group (n = 22) was 2.7 ± 1.6 months. Four eyes had no response to SMYL treatment, while one eye had a partial response. Among patients who did not respond to SMYL therapy, three eyes underwent PDT, while two eyes received anti-VEGF injection.
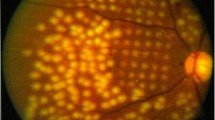
Late-phase fluorescein angiography (a), near-infrared image (b), and SD-OCT images (c) of a chronic CSC patient at baseline. The superimposed circle (b) represents the approximate area of SMYL spot application at the time of treatment. At 6 months after SMYL treatment, late-phase fluorescein angiography (d) shows a decrease of leakage compared with baseline (a). No definite RPE damage due to laser was noted (e). Complete resolution of subretinal fluid was achieved (f). Good anatomical results on SD-OCT imaging were noted (h) during the 3-year follow-up after SMYL treatment, with the absence of laser-induced retinal damage (g)
In the complete resolution group (n = 22), BCVA was 0.26 ± 0.24 (range, 0–0.7 logMAR) at baseline, which was improved to 0.13 ± 0.19 (range, 0–0.8 logMAR) at 6 months (p = 0.055), 0.08 ± 0.15 (range, 0–0.5 logMAR) at 1 year (p = 0.005), 0.08 ± 0.15 (range, 0–0.5 logMAR) at 3 years (p = 0.01), and 0.08 ± 0.14 (range, 0–0.5 logMAR) at the final follow-up (p = 0.008) (Table 2 and Fig. 2). CMT at baseline was 389.6 ± 103.4 μm (range, 226–609 μm), which decreased to 208.4 ± 49.4 μm (range, 127–324 μm) (p < 0.001) at 6 months, 197.2 ± 40.0 μm (range, 131–302 μm) (p < 0.001) at 1 year, 196.4 ± 40.2 μm (range, 120–278 μm) (p < 0.001) at 3 years, and 193.5 ± 40.0 μm (range, 118–278 μm) (p < 0.001) at the final follow-up (Table 2 and Fig. 3).
In all cases, no definite adverse effects or visible laser burns were identified on comparison of fundus photographs obtained before and after the procedure or on comparison of SD-OCT and near-infrared images.
Discussion
Acute CSC is believed to be self-limiting, and treatment is not always necessary. However, chronic CSC can result in permanent visual loss. Specifically, SRF in CSC can lead to loss of VA as a result of RPE damage. Thus, treatment may be indicated to achieve a faster recovery as well as to minimize the risk of further macular damage [3, 4].
A number of treatment modalities for CSC have been reported [4, 26]. Retinal photocoagulation is a good treatment option capable of resolving SRF in CSC; however, continuous-wave laser photocoagulation can result in scotoma formation, CNV, enlargement of the laser spot, and reduction of contrast sensitivity. In addition, retinal photocoagulation cannot be applied to subfoveal or juxtafoveal areas. Interestingly, several studies have failed to identify a difference in final VA or recurrence rates between treated and untreated eyes in long-term follow-up [5, 27, 28].
Since Bandello et al. [29] reported the first pilot study investigating SML for CSC in 2003, a number of studies have reported the results of SML in CSC [28]. Despite the differences in laser wavelength and parameters in these studies, the overall treatment response at the last reported follow-up was 79.6%, with a 63.6% rate of complete resolution of SRF. In controlled studies, SML has been shown to be either comparable or superior to PDT treatment (half dose or half fluence) and superior to untreated controls [28]. In addition, the majority of studies on SML have shown no definite adverse events after treatment [28].
In the present study, we utilized 577-nm SMYL, which provides a peak of absorption consistent with oxyhemoglobin, excellent lesion visibility, low intraocular light scattering and pain, and negligible xanthophyll absorption [30, 31]. The SMYL settings in our study consisted of a 100-µm spot diameter, 20-ms duration delivered over multiple sessions, 15% duty cycle, and low power ranging from 200 to 400 mW that was increased by 100 mW increments based on the status of SRF resolution at monthly follow-up. These settings differed from those of recently published studies, which were also inconsistent. The major differences between our study and previous work are treatment duration, power, and not utilizing laser titration. Specifically, several recent studies utilized a duty cycle between 5 and 15%, a duration between 100 and 300 ms, and power often >500 mW, even when titration was performed to avoid retinal damage [28, 32]. When 27 patients in this study were treated by SMYL photocoagulation for the first time (between 2011 and 2014), 15% duty cycle was the most popular parameter in the most studies of SML for CSC [28]. To explain the reason for treatment in 20 ms duration, you need to refer our past research in 2013 ARVO annual meeting [33]. Although it is already known that SMYL does not damage the retina, repetitive treatment of low energy setting such as 20-ms duration, 100 mW, 100-µm spot diameter, and 15% duty cycle could result in irreversible histologic change despite no changes on FA/ICGA and SD-OCT in rabbit model [33]. Because the laser treatment is performed on the macula, we had tried to minimize the damage that might occur even by using lower energy. And, we also reported the efficacy and safety of this parameter setting for treating CSC in 2015 [34]. With respect to titration, one case report described the consequences of overtreatment with SML, which included certain retinal damage and a retinal shock response in the form of SRF despite following a careful titration procedure [35]. In our study, the purpose of using a short duration and low power setting was to reduce the possibility of retinal damage while also avoiding the need for laser titration. To compensate for the inherent under-treatment associated with this approach, we utilized multiple sessions and increased laser power by 100 mW increments, never exceeding 400 mW.
The re-treatment period in the study till the complete resolution of SRF was also different from other studies. Most prefer to wait for 3 months before repeating laser treatment. However, we disagree to wait for the 3 months before repeating. The persistent presence of the SRF associated with a progressive deterioration of the RPE functions may be a cause of vision loss secondary to progressive retinal damage [36]. In the beginning, treatment should be considered after 3 months without resolution of acute CSC or in chronic CSC. And then one needs to try more active treatment to resolve SRF depending on response of initial treatment. All patients in the study included SRF with recurrent CSC and a history of chronic CSC or symptomatic CSC lasting 3 months or longer. Even if SRF is completely resolved by re-treatment after 3 months waiting, RPE or outer retina could be damaged during the period.
To the best of our knowledge, our study represents the longest follow-up duration to date with respect to efficacy and safety of 577-nm SMYL treatment for chronic CSC. The results of previous reports have been based on a relatively short follow-up period (approximately 1 year or less), although it is important to note that patients with chronic CSC require long-term observation. In our study, 16/27 eyes (53.3%) exhibited complete resolution of SRF with no recurrence after initial treatment, while six recurrences (22.2%) after initial SMYL treatment exhibited complete resolution at the last follow-up after repeat SMYL treatment. Overall, the rate of complete resolution of SRF at the final (at least 3 years) follow-up in our study was 81.5%, compared to 63.6% at the last mentioned follow-up described in other studies [28]. In spite of the short duration and low laser power, we noted a relatively higher success rate in resolution of SRF and found that SMYL had a good effect on recurrent cases even after initial failure of SMYL treatment. In addition, BCVA was significantly improved in the complete resolution group (n = 22).
A total of five eyes (15.5%) showed no or partial response to SMYL treatment, indicating that SMYL may not be successful in all cases of CSC reccurrence. It is possible that SMYL only impacts RPE dysfunction without influencing hyperdynamic choroidal circulation. Consistent with this possibility, choroidal hyper-permeability has been proposed as a primary cause of CSC. Under-treatment with SMYL may be another plausible explanation for the treatment failures observed in our study. Specifically, the laser energy used in our study may not have been sufficient to upregulate RPE heat-shock proteins in some patients, and the duration or power of SMYL may need to be adjusted in order to achieve proper energy levels in select patients. There is currently no consensus among physicians regarding the settings for SML. Our study may be a good reference for establishing laser parameter guidelines in chronic CSC patients, especially Asian CSC patients.
This study had several limitations, including its design as a small-sized retrospective study with an irregular follow-up period and lack of a control group. Therefore, our data should be interpreted with caution.
The majority of recent studies on SML therapy have reported good outcomes in CSC; however, laser parameters have differed significantly between studies, and the follow-up times have been relatively short. With respect to treatment power, several authors have utilized the titration method to establish an appropriate laser power for each patient. However, setting the proper area for initial titration remains problematic, and physicians should choose either the area of SRF or normal retina. The possibility of incurring retinal damage is another problem associated with the titration method. While the damage may be not serious, it can occur. A final question with respect to titration is the percent reduction of threshold laser power that can be selected to achieve a proper effect. In conclusion, fixed parameters for SML therapy, especially short-duration treatment delivered over multiple sessions, with incremental elevation of laser power starting from a low baseline to achieve SRF resolution, may be a good option for effective and safe treatment of chronic and recurrent CSC over the long term. Prospective, randomized, large-scale, controlled trials will be required to establish the optimum settings of SML for the treatment of CSC.
Summary
What was known before
• SMYL is an effective and safe method in the treatment of chronic CSC. However, proper laser setting for treatment is not well defined.
What this study adds
• Short-duration multiple-session method without titration can be a good reference for treating chronic CSC, and this study shows the longest follow-up results.
References
Von Graefe A, Abhandlungen K. Notizen und casaistische Mitheilungen vermischten Inhalts: VI. Ueber zentrale ecidivirende retinitis. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1866;12:211–5.
Gass JD. Pathogenesis of disciform detachment of the neuroepithelium. Am J Ophthalmol. 1967;63 Suppl:1–139.
Liu DT, Fok AC, Chan W, Lai TY, Lam DS. Central serous chorioretinopathy. In: Ryan SJ, Schachat AP, Sadda SR, editors). Retina. 5th ed. London: Elsevier; 2013. p. 1291–1303.
Wang M, Munch IC, Hasler PW, Prunte C, Larsen M. Central serous chorioretinopathy. Acta Ophthalmol. 2008;86:126–45.
Ficker L, Vafidis G, While A, Leaver P. Long-term follow-up of a prospective trial of argon laser photocoagulation in the treatment of central serous retinopathy. Br J Ophthalmol. 1988;72:829–34.
Bujarborua D. Long-term follow-up of idiopathic central serous chorioretinopathy without laser. Acta Ophthalmol Scand. 2001;79:417–21.
Baran NV, Gurlu VP, Esgin H. Long-term macular function in eyes with central serous chorioretinopathy. Clin Exp Ophthalmol. 2005;33:369–72.
Folk JC, Thompson HS, Han DP, Brown CK. Visual function abnormalities in central serous retinopathy. Arch Ophthalmol. 1984;102:1299–302.
Malik KJ, Sampat KM, Mansouri A, Steiner JN, Glaser BM. Low-intensity/high-density subthreshold micropulse diode laser for chronic central serous chorioretinopathy. Retina. 2014;35:532–6.
Little HL. Complications of argon laser retinal photocoagulation: a five-year study. Int Ophthalmol Clin. 1976;16:145–59.
Cardillo Piccolino F, Eandi CM, Ventre L, Rigault de la Longrais RC, Grignolo FM. Photodynamic therapy for chronic central serous chorioretinopathy. Retina. 2003;23:752–63.
Taban M, Boyer DS, Thomas EL, Taban M. Chronic central serous chorioretinopathy: photodynamic therapy. Am J Ophthalmol. 2004;137:1073–80.
Koytak A, Erol K, Coskun E, Asik N, Ozturk H, Ozerturk Y. Fluorescein angiography-guided photodynamic therapy with halfdose verteporfin for chronic central serous chorioretinopathy. Retina. 2010;30:1698–703.
Reibaldi M, Cardascia N, Longo A, Furino C, Avitabile T, Faro S, et al. Standard-fluence versus low-fluence photodynamic therapy in chronic central serous chorioretinopathy: a nonrandomized clinical trial. Am J Ophthalmol. 2010;149:307–15.
Kim SW, Oh J, Oh IK, Huh K. Retinal pigment epithelial tear after half fluence PDT for serous pigment epithelial detachment in central serous chorioretinopathy. Ophthalmic Surg Lasers Imaging. 2009;40:300–3.
Kim JW, Ryu SJ, Shin MC. The effect of intravitreal bevacizumab in patients with acute central serous chorioretinopathy. Korean J Ophthalmol. 2010;24:155–8.
Kim M, Lee SC, Lee SJ. Intravitreal ranibizumab for acute central serous chorioretinopathy. Ophthalmologica. 2013;229:152–7.
Tekin K, Sekeroglu MA, Cankaya AB, Teke MYm Doguizi S, Yilmazbas P. Intravitreal bevacizumab and ranibizumab in the treatment of acute central serous chorioretinopathy: a single center retrospective study. Semin Ophthalmol. 2018;33:265–70.
Pitcher JD 3rd, Witkin AJ, DeCroos FC, Ho AC. A prospective pilot study of intravitreal aflibercept for the treatment of chronic central serous chorioretinopathy: the CONTAIN study. Br J Ophthalmol. 2015;99:848–52.
Lavinsky D, Wang J, Huie P, Dalal R, Lee SJ, Lee DY, et al. Nondamaging retinal laser therapy: rationale and applications to the macula. Invest Ophthalmol Vis Sci. 2016;57:2488–2500.
Gupta B, Elagouz M, McHugh D, Chong V, Sivaprasad S. Micropulse diode laser photocoagulation for central serous chorioretinopathy. Clin Exp Ophthalmol. 2009;37:801–5.
Koss MJ, Beger I, Koch FH. Subthreshold diode laser micropulse photocoagulation versus intravitreal injections of bevacizumab in the treatment of central serous chorioretinopathy. Eye (Lond). 2012;26:307–14.
Chen SN, Hwang JF, Tseng LF, Lin CJ. Subthreshold diode micropulse photocoagulation for the treatment of chronic central serous chorioretinopathy with juxtafoveal leakage. Ophthalmology. 2008;115:2229–34.
Lanzetta P, Furlan F, Morgante L, Veritti D, Bandello F. Nonvisible subthreshold micropulse diode laser (810 nm) treatment of central serous chorioretinopathy. A pilot study. Eur J Ophthalmol. 2008;18:934–40.
Ricci F, Missiroli F, Regine F, Grossi M, Dorin G. Indocyanine green enhanced subthreshold diode-laser micropulse photocoagulation treatment of chronic central serous chorioretinopathy. Graefes Arch Clin Exp Ophthalmol. 2009;247:597–607.
Goldhagen BE, Goldhardt R. Diagnosed a patients with central serous chorioretinopathy? Now what?: management of central serous chorioretinopathy. Curr Ophthalmol Rep. 2017;5:141–8.
Gemenetzi M, De Salvo G, Lotery AJ. Central serous chorioretinopathy: an update on pathogenesis and treatment. Eye (Lond). 2010;24:1743–56.
Scholz P, Altay L, Fuser S. A review of subthreshold micropulse laser for treatment of macular disorders. Adv Ther. 2017;34:1528–55.
Bandello F, Lanzetta P, Furlan F, Polito A. Non visible subthreshold micorpulse diode laser treatment of idiopathic central serous chorioretinopathy. A pilot study. Invest Ophthalmol Vis Sci. 2003;44:4858.
Mainster MA. Wavelength selection in macular photocoagulation. Tissue optics, thermal effects, and laser systems. Ophthalmology. 1986;93:952–8.
Mainster MA. Decreasing retinal photocoagulation damage: principles and techniques. Semin Ophthalmol. 1999;14:200–9.
Luttrull JK. Low-intensity/high density subthreshold diode micropulse laser for central serous chorioretinopathy. Reina. 2016;36:1658–63.
Lee DK, Kang HS, Lee SJ, You YS, Kim SY, Kwon OW. Effects of repeated subthreshold micropulse laser photocoagulation in rabbit eyes. Invest Ophthalmol Vis Sci. 2013;54:4137.
Kim JY, Park HS, Kim SY. Short-term efficacy of subthreshold micropulse yellow laser (577-nm) photocoagulation for chronic central serous chorioretinopathy. Graefes Arch Clin Exp Ophthalmol. 2015;253:2129–35.
Gawecki M. Increase in central retinal edema after subthreshold diode micropulse laser treatment of chronic central serous chorioretinopathy. Case Rep Ophthalmol Med. 2015;2015:813414.
Wang M, Munch IC, Hasler PW, Prunte C, Larsen M. Central serous chorioretinopathy. Acta Ophthalmol. 2008;86:126–45.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kim, Y.J., Kim, S.Y., Ha, S. et al. Short-duration multiple-session subthreshold micropulse yellow laser (577 nm) for chronic central serous chorioretinopathy: results at 3 years. Eye 33, 819–825 (2019). https://doi.org/10.1038/s41433-018-0309-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-018-0309-7
- Springer Nature Limited
This article is cited by
-
Half-dose photodynamic therapy versus 577 nm subthreshold pulse laser therapy in treatment-naive patients with central serous chorioretinopathy
BMC Ophthalmology (2024)
-
Subthreshold laser compared to oral spironolactone for the treatment of chronic central serous chorioretinopathy: a retrospective study
International Ophthalmology (2024)
-
Development of the selective micropulse individual retinal therapy depends on age and type on the Fitzpatrick scale
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Yellow Subthreshold Micropulse Laser in Retinal Diseases: An In-Depth Analysis and Review of the Literature
Ophthalmology and Therapy (2023)
-
Short-term comparison between navigated subthreshold microsecond pulse laser and oral eplerenone for chronic central serous chorioretinopathy
Scientific Reports (2022)