Abstract
Background/objectives
Maternal diet is critical to fetal development. This study aimed to explore the association between maternal dietary diversity during pregnancy and congenital heart defects (CHD) in Chinese population.
Methods
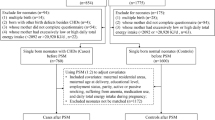
A hospital-based case-control study was conducted including 474 cases and 948 controls in Northwest China. We recruited eligible women waiting for delivery in the hospital and gathered their diets during the whole pregnancy by a validated food frequency questionnaire. According to the FAO Minimum Dietary Diversity for Women (MDD-W) guideline, the participants were categorized into “inadequate dietary diversity score (DDS)” (DDS < 5) and “adequate DDS” (DDS ≥ 5) groups. The association between dietary diversity and CHD was estimated using the mixed logistic regression models.
Results
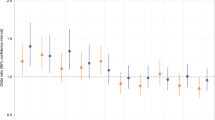
Case mothers had a lower DDS during pregnancy than the controls (P < 0.001). The proportions of women consuming all the ten defined food groups were lower in the inadequate DDS group than in the adequate DDS group among both cases and controls (all P < 0.001). The prevalence of inadequate micronutrient intake was higher in the inadequate DDS group than in the adequate DDS group among both cases and controls (all P < 0.05). Women in the adequate DDS group had reduced risks of having fetuses with total CHD (OR = 0.62, 95% CI = 0.45–0.84) and ventricular septal defects (OR = 0.58, 95% CI = 0.38–0.88).
Conclusions
Adequate DDS during pregnancy might be associated with a lower risk of CHD in offspring. Efforts to promote dietary diversity during pregnancy need to be strengthened to reduce the prevalence of CHD in Chinese population.



Similar content being viewed by others
References
Liu Y, Chen S, Zuhlke L, Black GC, Choy MK, Li N, et al. Global birth prevalence of congenital heart defects 1970-2017: updated systematic review and meta-analysis of 260 studies. Int J Epidemiol. 2019;48:455–63.
Donofrio MT, Moon-Grady AJ, Hornberger LK, Copel JA, Sklansky MS, Abuhamad A, et al. Diagnosis and treatment of fetal cardiac disease: a scientific statement from the American Heart Association. Circulation. 2014;129:2183–242.
Zhao QM, Liu F, Wu L, Ma XJ, Niu C, Huang GY. Prevalence of congenital heart disease at live birth in China. J Pediatr. 2019;204:53–8.
Mao B, Qiu J, Zhao N, Shao Y, Dai W, He X, et al. Maternal folic acid supplementation and dietary folate intake and congenital heart defects. PLoS ONE. 2017;12:e0187996.
Smedts HP, Rakhshandehroo M, Verkleij-Hagoort AC, de Vries JH, Ottenkamp J, Steegers EA, et al. Maternal intake of fat, riboflavin and nicotinamide and the risk of having offspring with congenital heart defects. Eur J Nutr. 2008;47:357–65.
Yang J, Kang Y, Cheng Y, Zeng L, Shen Y, Shi G, et al. Iron intake and iron status during pregnancy and risk of congenital heart defects: a case-control study. Int J Cardiol. 2020;301:74–9.
Yang J, Dang S, Cheng Y, Qiu H, Mi B, Jiang Y, et al. Dietary intakes and dietary patterns among pregnant women in Northwest China. Public Health Nutr. 2017;20:282–93.
Liu D, Cheng Y, Dang S, Wang D, Zhao Y, Li C, et al. Maternal adherence to micronutrient supplementation before and during pregnancy in Northwest China: a large-scale population-based cross-sectional survey. BMJ Open. 2019;9:e028843.
Chakona G, Shackleton C. Minimum dietary diversity scores for women indicate micronutrient adequacy and food insecurity status in South African towns. Nutrients. 2017;9:812.
FAO and FHI 360. Minimum dietary dieversity for women: a guide for measurement. Rome: FAO; 2016.
Yang J, Kang Y, Cheng Y, Zeng L, Yan H, Dang S. Maternal dietary patterns during pregnancy and congenital heart defects: a case-control study. Int J Environ Res Public Health. 2019;16:2957.
Crozier SR, Robinson SM, Godfrey KM, Cooper C, Inskip HM. Women’s dietary patterns change little from before to during pregnancy. J Nutr. 2009;139:1956–63.
Cheng Y, Yan H, Dibley MJ, Shen Y, Li Q, Zeng L. Validity and reproducibility of a semi-quantitative food frequency questionnaire for use among pregnant women in rural China. Asia Pac J Clin Nutr. 2008;17:166–77.
Yang J, Cheng Y, Pei L, Jiang Y, Lei F, Zeng L, et al. Maternal iron intake during pregnancy and birth outcomes: a cross-sectional study in Northwest China. Br J Nutr. 2017;117:862–71.
Institute of Nutrition and Food Safety, China Center for Disease Control. China Food Composition Book 2. Beijing: Peking University Medical Press; 2005.
Institute of Nutrition and Food Safety, China Center for Disease Control. China Food Composition Book 1. 2nd ed. Beijing: Peking University Medical Press; 2009.
Chinese Nutrition Society. Chinese Dietary Guideline. Beijing: People’s Medical Publishing House; 2016.
Kant AK, Schatzkin A, Harris TB, Ziegler RG, Block G. Dietary diversity and subsequent mortality in the first national health and nutrition examination survey epidemiologic follow-up study. Am J Clin Nutr. 1993;57:434–40.
Tian X, Wu M, Zang J, Zhu Y, Wang H. Dietary diversity and adiposity in Chinese men and women: an analysis of four waves of cross-sectional survey data. Eur J Clin Nutr. 2017;71:506–11.
Willett W. Nutritional epidemiology. 3rd ed. New York: Oxford University Press; 2013.
Feng Y, Cai J, Tong X, Chen R, Zhu Y, Xu B, et al. Non-inheritable risk factors during pregnancy for congenital heart defects in offspring: a matched case-control study. Int J Cardiol. 2018;264:45–52.
Pei L, Kang Y, Zhao Y, Yan H. Prevalence and risk factors of congenital heart defects among live births: a population-based cross-sectional survey in Shaanxi province, Northwestern China. BMC Pediatr. 2017;17:18.
Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. 1989;129:125–37.
Kennedy E. Dietary diversity, diet quality, and body weight regulation. Nutr Rev. 2004;62:S78–81.
Obermann-Borst SA, Vujkovic M, de Vries JH, Wildhagen MF, Looman CW, de Jonge R, et al. A maternal dietary pattern characterised by fish and seafood in association with the risk of congenital heart defects in the offspring. BJOG. 2011;118:1205–15.
Sotres-Alvarez D, Siega-Riz AM, Herring AH, Carmichael SL, Feldkamp ML, Hobbs CA, et al. Maternal dietary patterns are associated with risk of neural tube and congenital heart defects. Am J Epidemiol. 2013;177:1279–88.
Kornatowski BM, Comstock SS. Dietary diversity is inversely correlated with pre-pregnancy body mass index among women in a Michigan pregnancy cohort. PeerJ. 2018;6:e5526.
Yeneabat T, Adugna H, Asmamaw T, Wubetu M, Admas M, Hailu G, et al. Maternal dietary diversity and micronutrient adequacy during pregnancy and related factors in East Gojjam Zone, Northwest Ethiopia, 2016. BMC Pregnancy Childbirth. 2019;19:173.
Cheng Y, Dibley MJ, Zhang X, Zeng L, Yan H. Assessment of dietary intake among pregnant women in a rural area of western China. BMC Public Health. 2009;9:222.
Cano-Ibanez N, Martinez-Galiano JM, Amezcua-Prieto C, Olmedo-Requena R, Bueno-Cavanillas A, Delgado-Rodriguez M. Maternal dietary diversity and risk of small for gestational age newborn: findings from a case-control study. Clin Nutr. 2019. https://doi.org/10.1016/j.clnu.2019.08.019. E-pub ahead of print.
Rammohan A, Goli S, Singh D, Ganguly D, Singh U. Maternal dietary diversity and odds of low birth weight: empirical findings from India. Women Health. 2019;59:375–90.
Wu G, Bazer FW, Cudd TA, Meininger CJ, Spencer TE. Maternal nutrition and fetal development. J Nutr. 2004;134:2169–72.
Narmaki E, Siassi F, Fariba K, Qorbani M, Shiraseb F, Ataie-Jafari A, et al. Dietary diversity as a proxy measure of blood antioxidant status in women. Nutrition. 2015;31:722–6.
Fisher SA, Burggren WW. Role of hypoxia in the evolution and development of the cardiovascular system. Antioxid Redox Signal. 2007;9:1339–52.
Bosco JL, Tseng M, Spector LG, Olshan AF, Bunin GR. Reproducibility of reported nutrient intake and supplement use during a past pregnancy: a report from the Children’s Oncology Group. Paediatr Perinat Epidemiol. 2010;24:93–101.
Bunin GR, Gyllstrom ME, Brown JE, Kahn EB, Kushi LH. Recall of diet during a past pregnancy. Am J Epidemiol. 2001;154:1136–42.
Acknowledgements
The authors are grateful to all medical staff involved in the study for recruiting the participants. The authors are also grateful to all mothers and infants who participated in the study and all investigators who contributed to data collection.
Funding
This research was supported by the National Natural Science Foundation of China (81230016), the Shaanxi Health and Family Planning Commission (Sxwsjswzfcght2016-013), the National Key R&D Program of China (2017YFC0907200, 2017YFC0907201), the China Postdoctoral Science Foundation (2019M663751), and the China Scholarship Council (201906285048).
Author information
Authors and Affiliations
Contributions
JY, SD, and HY designed the study; JY analysed and interpreted the data and wrote the paper; JY, YC, and LZ contributed to data analysis and data interpretation; JY, SD, and HY provided critical revision of the paper; SD and HY had primary responsibility for the final content. All the authors read and approved the final version of the paper.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Yang, J., Cheng, Y., Zeng, L. et al. Maternal dietary diversity during pregnancy and congenital heart defects: a case-control study. Eur J Clin Nutr 75, 355–363 (2021). https://doi.org/10.1038/s41430-020-0617-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-0617-4
- Springer Nature Limited
This article is cited by
-
Dietary protein intake during pregnancy and birth weight among Chinese pregnant women with low intake of protein
Nutrition & Metabolism (2022)