Abstract
Background
Colorectal cancer is associated with lifestyle characteristics such as diet, physical inactivity, obesity, and smoking, but these are not incorporated in screening recommendations. Moreover, the joint association of these factors with various colorectal polyps is not established.
Methods
A case–control study, among consecutive subjects aged 40–70 years, undergoing colonoscopy. Cases with colorectal polyps were compared with controls. Detailed information was gathered regarding polyp histology and anatomic location, demographics, medical history, anthropometrics, and lifestyle. The healthy lifestyle index was estimated as the sum of: non-smoking, maintaining a healthy weight, healthy diet, and physical activity.
Results
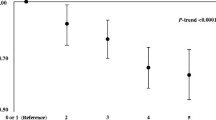
A total of 788 participants were included (cases n = 403, controls n = 385). The healthy lifestyle index had a negative association with colorectal polyps (OR = 0.72, 95% CI 0.62–0.85, P < 0.001), both adenomas and serrated polyps (OR = 0.75, 0.64–0.89, and OR = 0.59, 0.44–0.79, respectively), and both proximal and distal adenomas (OR = 0.77, 0.62–0.95, and OR = 0.73, 0.59–0.90, respectively). Adherence to ≥ 2 healthy lifestyle components was strongly related with colorectal polyps (OR = 0.50, 0.34–0.75, P = 0.001). Abstinence from smoking, and a healthy diet were the factors most strongly associated with lower odds of colorectal polyps (OR = 0.58, 0.42–0.79, and OR = 0.61, 0.44–0.85, respectively).
Conclusions
Adherence to a healthy lifestyle (≥2 healthy lifestyle components) is inversely associated with colorectal polyps, especially serrated and distal polyps, with no dose–response association. Components most strongly associated with lower odds of colorectal polyps were maintaining a healthy diet and abstinence from smoking. Lifestyle-related characteristics may assist in risk stratification and are potential goals for colorectal neoplasia prevention.



Similar content being viewed by others
References
Smith RA, Andrews K, Brooks D, DeSantis CE, Fedewa SA, Lortet-Tieulent J, et al. Cancer screening in the United States, 2016: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin. 2016;66:95–114.
Park S-Y, Boushey CJ, Wilkens LR, Haiman CA, Le Marchand L. High-quality diets associate with reduced risk of colorectal cancer: analyses of diet quality indexes in the multiethnic cohort. Gastroenterology. 2017;153:386–394.e2.
Mehta RS, Song M, Nishihara R, Drew DA, Wu K, Qian ZR et al. Dietary patterns and risk of colorectal cancer: analysis by tumor location and molecular subtypes. Gastroenterology 2017;152:1944-1953.e1.
Mehta M, Shike M. Diet and physical activity in the prevention of colorectal cancer. J Natl Compr Canc Netw. 2014;12:1721–6.
Robsahm TE, Aagnes B, Hjartåker A, Langseth H, Bray FI, Larsen IK. Body mass index, physical activity, and colorectal cancer by anatomical subsites: a systematic review and meta-analysis of cohort studies. Eur J Cancer Prev. 2013;22:492–505.
Riondino S, Roselli M, Palmirotta R, Della-Morte D, Ferroni P, Guadagni F. Obesity and colorectal cancer: role of adipokines in tumor initiation and progression. World J Gastroenterol. 2014;20:5177–90.
Ortega LS, Bradbury KE, Cross AJ, Morris JS, Gunter MJ, Murphy N. A prospective investigation of body size, body fat composition and colorectal cancer risk in the UK biobank. Sci Rep. 2017;7:17807.
Ordóñez-Mena JM, Schöttker B, Mons U, Jenab M, Freisling H, Bueno-de-Mesquita B, et al. Quantification of the smoking-associated cancer risk with rate advancement periods: meta-analysis of individual participant data from cohorts of the CHANCES consortium. BMC Med. 2016;14:62.
Lee PN, Thornton AJ, Hamling JS. Epidemiological evidence on environmental tobacco smoke and cancers other than lung or breast. Regul Toxicol Pharm. 2016;80:134–63.
Kaminski MF, Polkowski M, Kraszewska E, Rupinski M, Butruk E, Regula J. A score to estimate the likelihood of detecting advanced colorectal neoplasia at colonoscopy. Gut. 2014;63:1112–9.
Corte C, Zhang L, Chen J, Westbury S, Shaw J, Yeoh KG, et al. Validation of the Asia Pacific Colorectal Screening (APCS) score in a Western population: an alternative screening tool. J Gastroenterol Hepatol. 2016;31:370–5.
IJspeert JEG, Bossuyt PM, Kuipers EJ, Stegeman I, de Wijkerslooth TR, Stoop EM, et al. Smoking status informs about the risk of advanced serrated polyps in a screening population. Endosc Int Open. 2016;4:E73–8.
Schroy PC, Wong JB, O’Brien MJ, Chen CA, Griffith JL. A risk prediction index for advanced colorectal neoplasia at screening colonoscopy. Am J Gastroenterol. 2015;110:1062–71.
Devin JL, Hill MM, Mourtzakis M, Quadrilatero J, Jenkins DG, Skinner TL. Acute high intensity interval exercise reduces colon cancer cell growth. J Physiol (Lond). 2019;597:2177–84.
Roy P, Chowdhury S, Roy HK. Exercise-induced myokines as emerging therapeutic agents in colorectal cancer prevention and treatment. Future Oncol. 2018;14:309–12.
Martinez-Useros J, Garcia-Foncillas. J obesity and colorectal cancer: molecular features of adipose tissue. J Transl Med 2016;14:21.
Hu H, Cai Y, Huang J, Zhang J, Deng Y. Visceral adipose tissue and the risk of colorectal adenomas: a meta-analysis of observational studies. Eur J Cancer Prev. 2015;24:462–9.
Castelló A, Amiano P, Fernández de Larrea N, Martín V, Alonso MH, Castaño-Vinyals G et al. Low adherence to the western and high adherence to the mediterranean dietary patterns could prevent colorectal cancer. Eur J Nutr. 2018;58:1495–1505.
Yao Y, Suo T, Andersson R, Cao Y, Wang C, Lu J, et al. Dietary fibre for the prevention of recurrent colorectal adenomas and carcinomas. Cochrane Database Syst Rev. 2017;1:CD003430.
Turner ND, Lloyd SK. Association between red meat consumption and colon cancer: a systematic review of experimental results. Exp Biol Med (Maywood). 2017;242:813–39.
Demeyer D, Mertens B, De Smet S, Ulens M. Mechanisms linking colorectal cancer to the consumption of (Processed) red meat: areview. Crit Rev Food Sci Nutr. 2016;56:2747–66.
Song M, Garrett WS, Chan AT. Nutrients, foods, and colorectal cancer prevention. Gastroenterology. 2015;148:1244–60.e16.
Cottet V, Bonithon-Kopp C, Kronborg O, Santos L, Andreatta R, Boutron-Ruault M-C, et al. Dietary patterns and the risk of colorectal adenoma recurrence in a European intervention trial. Eur J Cancer Prev. 2005;14:21–9.
Abe SK, Inoue M, Sawada N, Iwasaki M, Ishihara J, Sasazuki S, et al. Rice, bread, noodle and cereal intake and colorectal cancer in Japanese men and women: the Japan Public Health Center-based prospective Study (JPHC Study). Br J Cancer. 2014;110:1316–21.
Bernstein AM, Song M, Zhang X, Pan A, Wang M, Fuchs CS, et al. Processed and unprocessed red meat and risk of colorectal cancer: analysis by tumor location and modification by time. PLoS ONE. 2015;10:e0135959.
Martínez F, Fernández-Martos C, Quintana MJ, Castells A, Llombart A, Ińiguez F, et al. APC and KRAS mutations in distal colorectal polyps are related to smoking habits in men: results of a cross-sectional study. Clin Transl Oncol. 2011;13:664–71.
He X, Wu K, Ogino S, Giovannucci EL, Chan AT, Song M. Association between risk factors for colorectal cancer and risk of serrated polyps and conventional adenomas. Gastroenterology. 2018;155:355–73.e18.
Davenport JR, Su T, Zhao Z, Coleman HG, Smalley WE, Ness RM, et al. Modifiable lifestyle factors associated with risk of sessile serrated polyps, conventional adenomas and hyperplastic polyps. Gut. 2018;67:456–65.
Gianfredi V, Salvatori T, Villarini M, Moretti M, Nucci D, Realdon S. Is dietary fibre truly protective against colon cancer? A systematic review and meta-analysis. Int J Food Sci Nutr. 2018;69:904–15.
Stintzing S, Tejpar S, Gibbs P, Thiebach L, Lenz H-J. Understanding the role of primary tumour localisation in colorectal cancer treatment and outcomes. Eur J Cancer. 2017;84:69–80.
Lucini D, Zanuso S, Blair S, Pagani M. A simple healthy lifestyle index as a proxy of wellness: a proof of concept. Acta Diabetol. 2015;52:81–9.
Lv J, Yu C, Guo Y, Bian Z, Yang L, Chen Y, et al. Adherence to healthy lifestyle and cardiovascular diseases in the chinese population. J Am Coll Cardiol. 2017;69:1116–25.
Orenstein L, Chetrit A, Dankner R. Healthy lifestyle pattern is protective against 30-yr cancer incidence in men and women: a cohort study. Nutr Cancer. 2016;68:410–9.
Aleksandrova K, Pischon T, Jenab M, Bueno-de-Mesquita HB, Fedirko V, Norat T, et al. Combined impact of healthy lifestyle factors on colorectal cancer: a large European cohort study. BMC Med. 2014;12:168.
Tilg H, Moschen AR. Mechanisms behind the link between obesity and gastrointestinal cancers. Best Pract Res Clin Gastroenterol. 2014;28:599–610.
Alemán JO, Eusebi LH, Ricciardiello L, Patidar K, Sanyal AJ, Holt PR. Mechanisms of obesity-induced gastrointestinal neoplasia. Gastroenterology. 2014;146:357–73.
Levesque C. Therapeutic lifestyle changes for diabetes mellitus. Nurs Clin North Am. 2017;52:679–92.
Luo S, Li J-Y, Zhao L-N, Yu T, Zhong W, Xia Z-S, et al. Diabetes mellitus increases the risk of colorectal neoplasia: an updated meta-analysis. Clin Res Hepatol Gastroenterol. 2016;40:110–23.
ICD-10-CM. Chapters List. https://icd.codes/icd10cm (Accessed 11 Apr 2018).
Kaluski DN, Goldsmith R, Arie OM, Mayer C, Green M. The first Israeli national health and nutrition survey (MABAT) as a policy maker. Public Health Rev. 2000;28:23–6.
Fox CS, Golden SH, Anderson C, Bray GA, Burke LE, de Boer IH, et al. Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: a scientific statement from the american heart association and the american diabetes association. Diabetes Care. 2015;38:1777–803.
Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Horn LV, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the american heart association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613.
Khera AV, Emdin CA, Drake I, Natarajan P, Bick AG, Cook NR, et al. Genetic risk, adherence to a healthy lifestyle, and coronary disease. N Engl J Med. 2016;375:2349–58.
Medina-Remón A, Kirwan R, Lamuela-Raventós RM, Estruch R. Dietary patterns and the risk of obesity, type 2 diabetes mellitus, cardiovascular diseases, asthma, and neurodegenerative diseases. Crit Rev Food Sci Nutr. 2018;58:262–96.
Tabung FK, Steck SE, Burch JB, Chen C-F, Zhang H, Hurley TG, et al. A healthy lifestyle index is associated with reduced risk of colorectal adenomatous polyps among non-users of non-steroidal anti-inflammatory drugs. J Prim Prev. 2015;36:21–31.
Erben Vanessa, Carr PrudenceR, Holleczek Bernd, Stegmaier Christa, Hoffmeister Michael, Brenner Hermann. Strong associations of a healthy lifestyle with all stages of colorectal carcinogenesis: results from a large cohort of participants of screening c…—PubMed—NCBI. Int J Cancer. 2019;144:2135–43.
Huang JLW, Wang YH, Jiang JY, Yu CP, Wu YL, Chen P, et al. The association between distal findings and proximal colorectal neoplasia: a systematic review and meta-analysis. Am J Gastroenterol. 2017;112:1234–45.
Lindblom A. Different mechanisms in the tumorigenesis of proximal and distal colon cancers. Curr Opin Oncol. 2001;13:63–9.
Missiaglia E, Jacobs B, D’Ario G, Di Narzo AF, Soneson C, Budinska E, et al. Distal and proximal colon cancers differ in terms of molecular, pathological, and clinical features. Ann Oncol. 2014;25:1995–2001.
Peterse EFP, Meester RGS, Siegel RL, Chen JC, Dwyer A, Ahnen DJ, et al. The impact of the rising colorectal cancer incidence in young adults on the optimal age to start screening: microsimulation analysis I to inform the American Cancer Society colorectal cancer screening guideline. Cancer. 2018;124:2964–73.
Fliss-Isakov N, Zelber-Sagi S, Webb M, Halpern Z, Kariv R. Smoking habits are strongly associated with colorectal polyps in a population-based case-control study. J Clin Gastroenterol. 2018;52:805–11.
Limsui D, Vierkant RA, Tillmans LS, Wang AH, Weisenberger DJ, Laird PW, et al. Cigarette smoking and colorectal cancer risk by molecularly defined subtypes. J Natl Cancer Inst. 2010;102:1012–22.
Ognjanovic S, Yamamoto J, Maskarinec G, Le Marchand L. NAT2, meat consumption and colorectal cancer incidence: an ecological study among 27 countries. Cancer Causes Control. 2006;17:1175–82.
Nimptsch K, Pischon T. Body fatness, related biomarkers and cancer risk: an epidemiological perspective. Horm Mol Biol Clin Invest. 2015;22:39–51.
Author information
Authors and Affiliations
Contributions
Fliss-Isakov N. conceived the study; designed the study; collected the data; and preformed statistical analysis, interpreted the results, and wrote the manuscript. Kariv R. conceived the study; designed the study; interpreted the results; and wrote the manuscript. Zaslavsky O. critically reviewed the manuscript. Webb M. performed medical data collection. Ivancovsky-Wajcman D. performed the data collection. Margalit D. performed the data collection. Shibolet O. critically reviewed the manuscript. Zelber-Sagi S. conceived the study; designed the study; interpreted the results; and wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fliss-Isakov, N., Kariv, R., Webb, M. et al. A healthy lifestyle pattern has a protective association with colorectal polyps. Eur J Clin Nutr 74, 328–337 (2020). https://doi.org/10.1038/s41430-019-0481-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-019-0481-2
- Springer Nature Limited