Abstract
Background
Up to 40% of vulvar cancer patients present with local recurrence within 10 years of follow-up. An inguinofemoral lymphadenectomy (IFL) is indicated if not performed at primary treatment. The incidence and risk factors for lymph node metastases (LNM) at first local recurrence, however, are unclear. Our aim was to determine the incidence of LNM at first local recurrence, in relation to previous groin treatment and clinicopathological factors.
Methods
A multicenter cohort study including vulvar cancer patients with a first macroinvasive local recurrence after primary surgical treatment between 2000 and 2015 was conducted in the Netherlands. Groin status at local recurrence was defined as positive (N+), negative (N−) or unknown (N?) and based on histology, imaging and follow-up. Patient-, tumour- and treatment characteristics of primary and recurrent disease were analysed.
Results
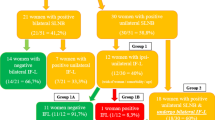
Overall, 16.3% (66/404) had a N+ groin status at first local recurrence, 66.4% (268/404) N− and 17.3% (70/404) N? groin status. The incidence of a N+ groin status was comparable after previous SLN and IFL, 11.5% and 13.8%, respectively. A N+ groin status was related to tumour size (25 vs.12 mm; P < 0.001), depth of invasion (5 vs. 3 mm; P < 0.001) and poorly differentiated tumours (22.9 vs. 11.9%; P = 0.050) at local recurrence.
Conclusions
The incidence of LNM at first local recurrence in vulvar cancer patients was 16.3%, and independent of previous type of groin surgery. In accordance with primary diagnosis, tumour size, depth of invasion, and tumour grade were significantly associated with a positive groin status.






Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this published article (and its supplementary information files).
References
Institute NC SEER cancer statistics factsheets: vulvar cancer. 2020. https://seer.cancer.gov/statfacts/html/vulva.html.
Schuurman M, van den Einden L, Massuger L, Kiemeney L, van der Aa M, de Hullu J. Trends in incidence and survival of Dutch women with vulvar squamous cell carcinoma. Eur J Cancer. 2013;49:3872–80.
Pleunis N, Schuurman MS, Van Rossum MM, Bulten J, Massuger LF, De Hullu JA, et al. Rare vulvar malignancies; incidence, treatment and survival in the Netherlands. Gynecol Oncol. 2016;142:440–5.
van der Steen S, de Nieuwenhof HP, Massuger L, Bulten J, de Hullu JA. New FIGO staging system of vulvar cancer indeed provides a better reflection of prognosis. Gynecol Oncol. 2010;119:520–5.
Oonk MH, Hemel BMV, Hollema H, Hullu JAD, Ansink AC, Vergote I, et al. Size of sentinel-node metastasis and chances of non-sentinel-node involvement and survival in early stage vulvar cancer: results from GROINSS-V, a multicentre observational study. Lancet Oncol. 2010;11:646–52.
Zhou J, Shan G. The prognostic role of FIGO stage in patients with vulvar cancer: a systematic review and meta-analysis. Curr Med Res Opin. 2016;32:1121–30.
De Hullu JA, Hollema H, Lolkema S, Boezen M, Boonstra H, Burger MP, et al. Vulvar carcinoma. The price of less radical surgery. Cancer. 2002;95:2331–8.
Van der Zee AG, Oonk MH, De Hullu JA, Ansink AC, Vergote I, Verheijen RH, et al. Sentinel node dissection is safe in the treatment of early-stage vulvar cancer. J Clin Oncol. 2008;26:884–9.
Hacker NF, Leuchter RS, Berek JS, Castaldo TW, Lagasse LD. Radical vulvectomy and bilateral inguinal lymphadenectomy through separate groin incisions. Obstet Gynecol. 1981;58:574–9.
Oonk M, Planchamp F, Baldwin P, Bidzinski M, Brännström M, Landoni F, et al. European Society of Gynaecological Oncology Guidelines for the management of patients with vulvar cancer. Int J Gynecol Cancer. 2017;27:832–7.
Gaarenstroom KN, Kenter GG, Trimbos JB, Agous I, Amant F, Peters AA, et al. Postoperative complications after vulvectomy and inguinofemoral lymphadenectomy using separate groin incisions. Int J Gynecol Cancer. 2003;13:522–7.
Leermakers ME, Pleunis N, Boll D, Hermans RH, Ezendam NP, Pijnenborg JM. High incidence of erysipelas after surgical treatment for vulvar carcinoma: an observational study. Int J Gynecol Cancer. 2016;26:582–7.
Woolderink JM, de Bock GH, de Hullu JA, Davy MJ, van der Zee AG, Mourits MJ. Patterns and frequency of recurrences of squamous cell carcinoma of the vulva. Gynecol Oncol. 2006;103:293–9.
Te Grootenhuis NC, van der Zee AG, van Doorn HC, van der Velden J, Vergote I, Zanagnolo V, et al. Sentinel nodes in vulvar cancer: long-term follow-up of the GROningen INternational Study on Sentinel nodes in Vulvar cancer (GROINSS-V) I. Gynecol Oncol. 2016;140:8–14.
Pouwer AW, Arts HJ, van der Velden J, de Hullu JA. Limiting the morbidity of inguinofemoral lymphadenectomy in vulvar cancer patients; a review. Expert Rev Anticancer Ther. 2017;17:615–24.
van Doorn HC, Oonk MHM, Fons G, Gaarenstroom KN, de Hullu J, van Rosmalen J, et al. Sentinel lymph node procedure in patients with recurrent vulvar squamous cell carcinoma: a proposed protocol for a multicentre observational study. BMC Cancer. 2022;22:445.
Nikolić O, Sousa FAE, Cunha TM, Nikolić MB, Otero-García MM, Gui B, et al. Vulvar cancer staging: guidelines of the European Society of Urogenital Radiology (ESUR). Insights Imaging. 2021;12:131.
Land RHJ, Moskovic E, King M, Sohaib SA, Trott P, et al. Routine computerized tomography scanning, groin ultrasound with or without fine needle aspiration cytology in the surgical management of primary squamous cell carcinoma of the vulva. Int J Gynecol Cancer. 2006;16:312–7.
Woelber L, Eulenburg C, Kosse J, Neuser P, Heiss C, Hantschmann P, et al. Predicting the course of disease in recurrent vulvar cancer—a subset analysis of the AGO-CaRE-1 study. Gynecol Oncol. 2019;154:571–6.
Nooij LS, van der Slot MA, Dekkers OM, Stijnen T, Gaarenstroom KN, Creutzberg CL, et al. Tumour-free margins in vulvar squamous cell carcinoma: Does distance really matter? Eur J Cancer. 2016;65:139–49.
Yap JK, Fox R, Leonard S, Ganesan R, Kehoe ST, Dawson CW, et al. Adjacent lichen sclerosis predicts local recurrence and second field tumour in women with vulvar squamous cell carcinoma. Gynecol Oncol. 2016;142:420–6.
Tantipalakorn C, Robertson G, Marsden DE, Gebski V, Hacker NF. Outcome and patterns of recurrence for International Federation of Gynecology and Obstetrics (FIGO) stages I and II squamous cell vulvar cancer. Obstet Gynecol. 2009;113:895–901.
Te Grootenhuis NC, Pouwer AW, de Bock GH, Hollema H, Bulten J, van der Zee AGJ, et al. Prognostic factors for local recurrence of squamous cell carcinoma of the vulva: a systematic review. Gynecol Oncol. 2018;148:622–31.
(WOG) WOG. National Guideline vulvar carcinoma. 2018. https://www.oncoline.nl/vulvacarcinoom2011.
Maaskant-Braat AJ, Voogd AC, Roumen RM, Nieuwenhuijzen GA. Repeat sentinel node biopsy in patients with locally recurrent breast cancer: a systematic review and meta-analysis of the literature. Breast Cancer Res Treat. 2013;138:13–20.
Beasley GM, Speicher P, Sharma K, Seigler H, Salama A, Mosca P, et al. Efficacy of repeat sentinel lymph node biopsy in patients who develop recurrent melanoma. J Am Coll Surg. 2014;218:686–92.
van Doorn HC, van Beekhuizen HJ, Gaarenstroom KN, van der Velden J, van der Zee AG, Oonk MH, et al. Repeat sentinel lymph node procedure in patients with recurrent vulvar squamous cell carcinoma is feasible. Gynecol Oncol. 2016;140:415–9.
Oonk MHM, Slomovitz B, Baldwin PJW, van Doorn HC, van der Velden J, de Hullu JA, et al. Radiotherapy versus inguinofemoral lymphadenectomy as treatment for vulvar cancer patients with micrometastases in the sentinel node: results of GROINSS-V II. J Clin Oncol. 2021;39:3623–32.
Pounds R, O'Neill D, Subba K, Garg A, Scerif M, Leong E, et al. The role of preoperative computerized tomography (CT) scan of the pelvis and groin in the management of clinically early staged vulva squamous cell carcinoma. Gynecol Oncol. 2020;157:444–9.
Pleunis N, Pouwer A, van Heertum A, te Grootenhuis N, Massuger L, Tjiong M, et al. EP1180 Incidence and prognostic factors for inguinofemoral lymph node metastasis in patients with a first local recurrence of vulvar squamous cell carcinoma. Int J Gynecol Cancer. 2019;29:A609.
Acknowledgements
Published conference abstracts: in an earlier stage of the study, the abstract was presented at the European Society of Gynecological Oncology (ESGO) meeting in 2019 [30]. Additional contributions: Martijn Mensink, Anouk van Heertum and Anne Hompesch are medical (Master of Science) students and were involved in the data collection process as part of their thesis.
Funding
The author(s) received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
Conceptualisation: JdH, HP, NP and AFP. Data curation: NP, AFP, MO, HvD, MT, JvdV, HZ, MvP, EvD and BS. Formal Analysis: NP, JdH and HP. Methodology: NP, AFP, JdH and HP. Supervision: JdH and HP. Writing—original draft: NP. Writing—review and editing: NP, AFP, MO, HvD, MT, JvdV, HZ, MvP, EvD, BS and CV.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the medical ethics committee at the Radboud University Medical Center (case file number 2017–3475) and all local ethics committees. All required data had been previously registered during medical treatment and records were anonymized. The study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41416_2023_2373_MOESM2_ESM.docx
Supplement 2; Exploration of reasons for refraining from surgical treatment in patients with N+ groin status at local recurrence on basis of positive imaging (n = 10)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pleunis, N., Pouwer, AF.W., Oonk, M.H.M. et al. Incidence of inguinofemoral lymph node metastases at the first local recurrence of vulvar cancer: a Dutch nationwide study. Br J Cancer 129, 956–964 (2023). https://doi.org/10.1038/s41416-023-02373-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-023-02373-0
- Springer Nature Limited