Abstract
Purpose To review current practice regarding oral surgery input for patients awaiting cardiac valvular surgery and who are at risk of infective endocarditis (IE) in the context of the COVID-19 pandemic, and to stimulate debate around the indications for pre-operative oral surgery assessment. It also opens the way to developing a new research-based approach which is patient-centred, safe, effective and efficient.
Methods A desk-top based patient review was undertaken between 27 March 2020 and 1 July 2022 to record the outcome of patients undergoing cardiac valvular surgery in Northern Ireland, following the revision of the referral guidelines for oral surgery intervention. Data were collected for all cardiac referrals to the oral surgery on-call service in the Royal Victoria Hospital, Belfast. Complications were recorded at two weeks, two months, and six months post-surgery, using Northern Ireland Electronic Care Records.
Results In total, 67 cardiac patients were identified between 27 March 2020 and 1 July 2022: 65.7% of patients were male and had an average age of 68, while the female patients had an average age of 61. The mean interval of date of cardiology referral to surgery date was 9.7 working days, with 36% of patients referred within five days of the planned surgery date. Moreover, 39% had valvular surgery in combination with another type of cardiac surgery. No complications linked to dental aetiology were noted.
Conclusions This paper raises questions about the advisability of oral surgery input before cardiac surgery for anything other than pain relief, management of acute dental sepsis, or IE whose source has been identified as an oral commensal. The COVID-19 pandemic has presented an opportunity to review current practice and open the way to developing a new approach which is patient-centred, safe, effective and efficient.
Key points
-
This paper discusses the controversial topic of dental treatment before cardiac valvular surgery and reviews patients' post-valve surgery.
-
Patients included in this paper have not received dental input.
-
Results show no complications of a dental aetiology.
Similar content being viewed by others
Introduction
Infective endocarditis (IE), inflammation of the endocardium, is a relatively rare disease, with an estimated incidence of 3-10 cases per 100,000 person-years in most population-based studies.1,2,3Despite diagnostic and treatment advances, prognosis remains poor, with hospital mortality at 22%, rising to 40% at five years.1,2,3,4 Morbidity rates are also high: 50% of patients require operative treatment in the acute phase of the disease, often with ongoing detriment to the quality of life.5,6
Cardiovalvular surgery (CVS involving valve replacement) increases patients' risk of developing postoperative IE. CVS cases complicated by IE are also increasing.7 The links between oral health and cardiovascular disease have long been established.8 Importantly, the presence of chronic periodontitis increases the risk of IE, especially in patients with heart defects.8,9 Community-associated IE is often linked to oral bacteria, leading to cardiologists requesting the elimination of dental infections before CVS.10 American and European cardiology guidelines currently recommend dental examination before cardiac surgery, with the European Society of Cardiology advising the elimination of dental sepsis sources two weeks before procedures.11,12 However, there is currently no standardised guidance on the acceptable standard of oral health required for these patients, and if dental interventions that can be conducted in a limited preoperative time frame actually improve long-term surgical outcomes. Furthermore, the guidance does not specify who should carry out a dental assessment preoperatively and what would constitute a valid dental assessment. Notably, the cost-benefit and risk-benefit of dental interventions before cardiac surgery have not been well defined.13
The removal of dental infection appears to be more important in patients undergoing heart transplants due to the need for postoperative immunosuppressants.13 These patients regularly present with poor dentition, including periodontitis and apical pathology, and often have poor surgical outcomes.14 However, there is still conflicting guidance about the level of oral assessment, type of dental treatment required, and the treatment timing before CVS.13
In January 2020, the World Health Organisation, following the recommendations of the emergency committee, declared the COVID-19 outbreak a public health emergency of international concern, with a pandemic declared in March 2020.15 This outbreak created an unusual disruption and placed an exceptional strain on the NHS system.16 This pressure to adapt was felt across all specialities, forcing drastic changes to be implemented.17 Prior to the pandemic, the demand for dental services had already increased due to the adoption of percutaneous cardio-valvular procedures where turnaround time was reduced.17
The oral surgery department in the School of Dentistry in the Royal Victoria Hospital, Belfast, historically assessed and treated sources of dentoalveolar infection for in-patients before cardiac valve replacement to reduce the risk of IE. However, due to the constraints placed on the provision of this service by the pandemic, with patient and staff face-to-face contacts minimised (except for emergency treatment and assessment cases), the oral surgery department outlined an interim arrangement for cardiac patients during the COVID-19 pandemic. Following managerial approval and communication to cardiology colleagues, the changes were implemented, with patient assessment limited to those exhibiting signs or symptoms of acute infection, including IE of likely dental origin as confirmed by blood cultures. Cardiology colleagues were reminded that post-surgical discharge should include explicit instruction for the patient to resume and maintain dental treatment with their general dental practitioner.
This period of enforced altered service provision afforded the oral surgery team an opportunity to observe subsequent cardiac outcomes for these patients during the COVID-19 pandemic.
Methods
All cardiac referrals to the oral surgery on-call service in Royal Victoria Hospital were reviewed between 27 March 2020 and 1 July 2022.
The initial data collected included:
-
Date of referral
-
Staff member taking the referral
-
Patient identifiers including age, sex and catchment area
-
Referral source
-
Reason for referral and date of planned procedure.
The data were pseudo-anonymised and recorded in a secure Microsoft Excel file. Data analysis and summative statistical analysis were performed on Microsoft Excel 16.43. Further data were collected by one investigator using the Northern Ireland Electronic Care Record System at the following postoperative time points: two weeks, two months and six months.
This additional data included:
-
Surgical outcomes outlined in the notes, including all complications recorded
-
Treatment date and type
-
Discharge arrangements and instructions
-
Review dates and clinical details of attendance at out-patient appointments
-
Review of any 'out of hours' hospital attendance or in-patient admission.
The inclusion criteria encompassed all patients referred to the service for pre-cardiac surgery dental input, where oral surgery input was not required due to the absence of acute dental pathology as per the new departmental guidance. Excluded cases were those patients with acute dental pain, infection, or established IE with a possible dental cause.
Results
In total, 18 referrals from the cardiology department were received by the oral surgery department during the initial data collection period between 27 March 2020 and 1 June 2020. Four patients were excluded as they were not awaiting valvular surgery. Three of the remaining 14 patients, initially referred by cardiology, had signs of IE (with supportive blood cultures), or acute dental symptoms requiring assessment and input.
None of the remaining initial 11 patients observed subsequently developed endocarditis or had complications felt to be attributable to dental causes.
This initial data collection and analysis prompted formal approval by management and communication to the cardiology team, as previously detailed.
Further data collection was carried out between 2 June 2020 and 1 July 2022, with a further 56 patients awaiting valvular surgery referred to the oral surgery department. Longitudinal data are therefore available for a total of 67 patients.
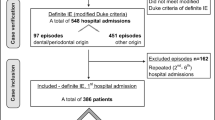
Data analysis revealed 65.7% of patients were male with an average age of 68 years. The average age of the female patients was 61 years. The mean interval from date of cardiology referral to planned cardiac surgery date was 9.7 working days, with 36% of patients referred within five days of planned surgery (see Fig. 1).
Patients referred by cardiology for assessment pre-valvular surgery were noted to have undergone various procedures, with 39% of patients having valvular surgery in combination with another type of cardiac surgery (see Fig. 2).
All postoperative complications were recorded at the previously noted interval of two weeks, two months and six months. Two-week postoperative data are available for all the 67 recorded patients (see Table 1), two-month review data are available for 66 patients, and six-month data for 53 of the 67 patients. There were no complications relating to dental aetiology noted at any of the defined recovery periods.
Discussion
There is conflicting evidence in the literature regarding the necessity for dental assessment and treatment before cardiac surgery.
A national study in the USA between 2004-2010 found a strong association between gingivitis and periodontitis and increased postoperative bacterial infections. However, it is not clear from the paper whether this refers to bacterial IE and prolonged hospitalisation in patients undergoing heart valve surgery.18 Furthermore, evidence suggests that patients who require cardiac valve replacement or heart transplantation often have poor dental health, and removing odontogenic infective sources is advocated to reduce infection risk.19
In contrast, there is also evidence from the literature suggesting there is no difference in postoperative valvular infection rates between patients who had pre-cardiac surgery dental assessment and those without. In a study of 74 patients undergoing cardiac transplantation, 43 had dental foci eliminated, with 31 having no preoperative dental treatment: there was no difference in infection rate, rejection rate or mortality between the groups.20 This is further supported by two subsequent studies on the same cohort of patients undergoing heart valve surgery, where there was no reduction in postoperative infections or improved survival following dental screening and treatment 3-6 months before surgery.21,22
A systematic review published in 2019 by Lockhart et al. looked at determining the potential effect of dental treatment before cardiac valve surgery on patient outcomes. The results suggest uncertainty about whether dental intervention for patients undergoing cardiac surgery resulted in a different health outcome and therefore the influence of dental treatment before CVS on morbidity and mortality remains unclear.23
Treatment of patients at high risk of dental caries and periodontal disease is a longitudinal process and not limited to any single episode or 'treatment burst'. These patients require long-term supportive care, including regular assessments and likely supportive periodontal treatment before, as well as after, cardiac surgery.
While a one-off 'treatment burst' for these patients in a hospital setting before cardiac surgery may help mitigate one source of infection, such as acute dental abscesses, it may also give rise to false expectations of confidence, both to the cardiac surgeon and the patient, as it will not eliminate the risk and certainly will not help address the other underlying causes of dental disease, such as caries and chronic periodontal disease, in the time frame normally available for dental input.
Advocates for pre-cardiac surgery dental assessment and treatment point to the need to avoid treating these patients after cardiac surgery, where they are at risk of prolonged bleeding due to anticoagulant therapy and, of course, the catastrophic impact of IE involving new valves. In the case of heart transplant patients, a concern also arises around the potentially higher risk of infections due to immunosuppressive therapies themselves.
In contrast, it is possible to argue that, postoperatively, and with appropriate adjunctive support, one would reasonably expect these patients to have improved cardiovascular fitness as a result of their surgical intervention and be more tolerant of the necessary protracted dental remediation and maintenance required to render them fully dentally fit.
Considering the higher risk of developing IE after bacteraemia occurs, dental treatment should be carried out a minimum of two weeks before surgery to ensure adequate healing and optimise dental health.24 Some authors advocate undertaking dental treatment between 1-3 months before surgery to reduce the risk of recurrence of infection and ensure dental health is maintained.25,26 Clearly, while this ideal situation might apply for elective cardiac procedures, it will not help with emergency admissions where there will be time constraints for these patients admitted in an emergency setting, and where it is very likely that patients will either progress directly to cardiac surgery without dental intervention or, at best, will only have the extraction of teeth whose prognosis is considered an immediate cause of concern.
In contrast, some authors have advocated concomitant surgery. In a case-control of 21 patients, Lockart et al. (2009) performed extractions simultaneously with cardiac valvular surgery under the coverage of antibiotic prophylaxis with no surgical complications.8
Conclusion
This paper raises the question of the advisability of oral surgery input before cardiac surgery for anything other than pain relief, acute dental abscesses/sepsis management, or IE confirmed to be caused by oral commensals.
The numbers involved in this review are necessarily small given the population size of Northern Ireland, which is around 1.9 million. Nonetheless, the study findings do serve to open a debate around the area of the oral surgeon's (and dentist's) role in the preoperative assessment of the cardiac patient awaiting valvular surgery. The current COVID-19 pandemic has presented an opportunity to review the logic and efficacy of our current practice relating to pre-cardiac dental assessment and treatment, and opens the way to developing a new approach which is patient-centred, safe, effective and efficient.
References
Dios P D. Infective endocarditis prophylaxis. Oral Dis 2014; 20: 325-328.
Berlin J A, Abrutyn E, Strom B L et al. Incidence of infective endocarditis in the Delaware Valley, 1988-1990. Am J Cardiol 1995; 76: 933-936.
McDonald J R. Acute infective endocarditis. Infect Dis Clin North Am 2009; 23: 643-664.
Selton-Suty C, Célard M, Le Moing V et al. Preeminence of Staphylococcus aureus in infective endocarditis: a 1-year population-based survey. Clin Infect Dis 2012; 54: 1230-1239.
Moreillon P, Que Y-A. Infective endocarditis. Lancet 2004; 363: 139-149.
Verhagen D W, Hermanides J, Korevaar J C et al. Health-related quality of life and posttraumatic stress disorder among survivors of left-sided native valve endocarditis. Clin Infect Dis 2009; 48: 1559-1565.
Lockhart P B, Brennan M T, Sasser H C, Fox P C, Paster B J, Bahrani-Mougeot F K. Bacteraemia associated with toothbrushing and dental extraction. Circulation 2008; 117: 3118-3125.
Mougeot F K, Saunders S E, Brennan M T, Lockhart P B. Associations between bacteraemia from oral sources and distant-site infections: tooth brushing versus single tooth extraction. Oral Surg Oral Med Oral Pathol Oral Radiol 2015; 119: 430-435.
Souza A F, Rocha A L, Castro W H et al. Dental management for patients undergoing heart valve surgery. J Card Surg 2017; 32: 627-632.
DeSimone D C, Tleyjeh I M, Correa de Sa D D et al. Temporal trends in infective endocarditis epidemiology from 2007 to 2013 in Olmsted County MN. Am Heart J 2015; 170: 830-836.
Habib G, Lancellotti P, Antunes M J et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 2015; 36: 3075-3128.
Wilson W, Taubert K A, Gewitz M et al. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anaesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation 2007; 116: 1736-1754.
De Souza A F, Rocha A L, Castro W H et al. Dental care before cardiac valve surgery: Is it important to prevent infective endocarditis? Int J Cardiol Heart Vasc 2016; 12: 57-62.
Lockhart P B, Brennan M T, Cook W H et al. Concomitant surgical treatment of dental and valvular heart diseases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: 71-76.
Sackett D L, Rosenberg W M, Gray J A, Haynes R B, Richardson W S. Evidence based medicine: what it is and what it isn't. BMJ 1996; 312: 71-72.
Commonwealth Fund. The Impact of the COVID-19 Pandemic on Outpatient Visits: Changing Patterns of Care in the Newest COVID-19 Hotspots. 2020. Available at https://www.commonwealthfund.org/publications/2020/aug/impact-covid-19-pandemic-outpatient-visits-changing-patterns-care-newest (accessed April 2023).
McCabe R, Schmit N, Christen P et al. Adapting hospital capacity to meet changing demands during the COVID-19 pandemic. BMC Med 2020; 18: 329.
Allareddy V, Elangovan S, Rampa S, Shin K, Nalliah R P, Allareddy V. Presence of gingivitis and periodontitis significantly increases hospital charges in patients undergoing heart valve surgery. J Mass Dent Soc 2015; 63: 10-16.
Cotti E, Arrica M, Di Lenarda A et al. The perioperative dental screening and management of patients undergoing cardiothoracic, vascular surgery and other cardiovascular invasive procedures: A systematic review. Eur J Prev Cardiol 2017; 24: 409-425.
Meyer U, Weingart D, Deng M C, Scheld H H, Joos U. Heart transplants - assessment of dental procedures. Clin Oral Investig 1999; 3: 79-83.
Hakeberg M, Dernevik L, Gatzinsky P, Eklöf C, Kennergren C, Jontell M. The significance of oral health and dental treatment for the postoperative outcome of heart valve surgery. Scand Cardiovasc J 1999; 33: 5-8.
Bratel J, Kennergren C, Dernevik L, Hakeberg M. Treatment of oral infections before heart valve surgery does not improve long-term survival. Swed Dent J 2011; 35: 49-55.
Lockhart P B, DeLong H R, Lipman R D et al. Effect of dental treatment before cardiac valve surgery: Systematic review and meta-analysis. J Am Dent Assoc 2019; 150: 739-747.
Starkebaum M, Durack D, Beeson P. The 'incubation period' of subacute bacterial endocarditis. Yale J Biol Med 1977; 50: 49-58.
Yasny J S, Silvay G. The value of optimizing dentition before cardiac surgery. J Cardiothoracic Vasc Anaesth 2007; 21: 587-591.
Yasny J S, Herlich A. Perioperative dental evaluation. Mt Sinai J Med 2012; 79: 34-45.
Author information
Authors and Affiliations
Contributions
John Marley was responsible for the concept of the audit and inputted into the design and writing of the manuscript. Victoria Stewart was responsible for the data collection and inputted into the design and writing of the manuscript. Rebekah Milligan contributed to data collection. Marwa Ramadan and Nusaybah Elsherif were responsible for the literature review and contributed to the drafting of the paper. Marwa Ramadan also contributed to the data collection. Amanda Beresford contributed to the concept of the audit and inputted to the review of the paper.
Corresponding author
Ethics declarations
The authors have no conflicts of interest to declare.
This was a retrospective audit of patient outcomes arising from an enforced change in clinic practice due to the COVID-19 pandemic; therefore, ethical approval and consent was not required.
Rights and permissions
About this article
Cite this article
Ramadan, M., Stewart, V., Elsherif, N. et al. Infective endocarditis and oral surgery input before cardiac surgery: time to prick the paradigm of pre-cardiac surgery assessments?. Br Dent J 234, 678–681 (2023). https://doi.org/10.1038/s41415-023-5796-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-023-5796-7
- Springer Nature Limited
This article is cited by
-
Dental screening: pre-cardiac surgery
British Dental Journal (2023)