Abstract
Introduction Dentists prescribe a significant proportion of all antibiotics, while antimicrobial stewardship aims to minimise antibiotic-prescribing to reduce the risk of developing antibiotic-resistance and adverse drug reactions.
Aims To evaluate NHS antibiotic-prescribing practices of dentists in England between 2010-2017.
Methods NHS Digital 2010-2017 data for England were analysed to quantify dental and general primary-care oral antibiotic prescribing.
Results Dental prescribing accounted for 10.8% of all oral antibiotic prescribing, 18.4% of amoxicillin and 57.0% of metronidazole prescribing in primary care. Amoxicillin accounted for 64.8% of all oral antibiotic prescribing by dentists, followed by metronidazole (28.0%), erythromycin (4.4%), phenoxymethylpenicillin (0.9%), clindamycin (0.6%), co-amoxiclav (0.5%), cephalosporins (0.4%) and tetracyclines (0.3%). Prescriptions by dentists declined during the study period for all antibiotics except for co-amoxiclav. This increase is of concern given the need to restrict co-amoxiclav use to infections where there is no alternative. Dental prescribing of clindamycin, which accounted for 43.9% of primary care prescribing in 2010, accounted for only 14.6% in 2017. Overall oral antibiotic prescribing by dentists fell 24.4% as compared to 14.8% in all of primary care.
Conclusions These data suggest dentists have reduced antibiotic prescribing, possibly more than in other areas of primary-care. Nonetheless, opportunities remain for further reduction.
Similar content being viewed by others
Key points
Identifies antibiotics most commonly prescribed by dentists.
Reports on the changes in antibiotic prescribing by dentists between 2010-2017 and also on the cost of this prescribing.
Compares the frequency with which dentists prescribe specific antibiotics with the prescribing of the same antibiotics by general medical practitioners.
Demonstrates that dentists, possibly more than doctors, have complied with the antibiotic stewardship message to reduce non-essential antibiotic prescribing.
Introduction
Antibiotics play an invaluable role in both the treatment and prevention of life-threatening infections. An inability to treat infections, however, is the price we may pay if more antibiotics become ineffective due to antimicrobial resistant bacteria. Prescribing guidelines and antimicrobial stewardship initiatives highlight the need to minimise unnecessary prescribing of antibiotics and to ensure that antibiotics are prescribed at the right dose, for the right duration and with the optimal spectrum of antimicrobial activity to kill pathogens, while minimising the risk of encouraging bacterial drug resistance.1 Since dental oral antibiotic prescribing accounts for a significant proportion of all antibiotic prescribing, it is important to monitor dental oral antibiotic prescribing trends and to evaluate them in the context of changes in the overall prescribing of oral antibiotics in primary care.
The aim of this study was to evaluate NHS oral antibiotic prescribing practices of dentists in England during the period 2010-2017.
Methods
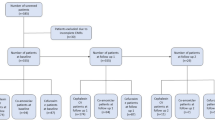
Prescription cost analysis data held by NHS Digital (https://digital.nhs.uk/data-and-information/publications/statistical/prescription-cost-analysis) was abstracted to obtain all oral antibiotics prescribed in the primary care setting in England between 2010-2017. Prescriptions were submitted by physicians, nurse practitioners, and other healthcare providers, including dentists. A further abstraction was performed that restricted the data to oral antibiotics prescribed by dentists working in NHS primary care. Hospital and private prescribing of antibiotics was not covered.
These data also provide the net ingredient cost (NIC) for all prescriptions. This is the basic cost of a drug used in primary care. This is the list price cost excluding value added tax (VAT), that is, the price listed in the national Drug Tariff or in standard price lists, but it is not necessarily the price the NHS paid. It does not include contract prices or discounts, dispensing costs, fees or prescription charge income, so the amount the NHS paid will be different. None-the-less, it provides an estimate of the comparative cost of prescribing different medicines and is widely used to estimate and compare prescribing costs.
Based on the relatively small number of prescriptions for individual cephalosporins or tetracyclines, all cephalosporin and tetracycline prescriptions were respectively grouped. Aminoglycosides were excluded since their oral absorption is minimal to none and they accounted for only 0.002% of overall oral antibiotic prescribing and zero dental prescribing. Similarly, fosfomycin was not included due to its limited use. Linezolid and tidezolid were not included in the analysis since these agents are only prescribed by secondary care. Fluoroquinolone data were included in the overall analysis of oral antibiotic use, although there was no dental prescribing of fluoroquinolones. Further details regarding oral fluoroquinolone use were the focus of a prior publication.2 Oral antibiotics (isoniazid, rifampin, ethambutol, para-aminosalicylic acid, pyrazinamide, clofazimine, bedaquiline, rifabutin, rifapentine, dapsone, ethionamide, cycloserine, prothionamide, and delamanid) used primarily to treat mycobacterial infections were also excluded.
The numbers of active dentists, patients treated, and courses of dental treatment provided in England annually were obtained from NHS Digital, Dental Statistics (https://digital.nhs.uk/data-and-information/publications/statistical/nhs-dental-statistics). The number of practising dentists included those working wholly within the NHS and those working privately, but with some NHS activity. NHS digital recorded the number of adult patients treated by counting the number seen at least once in the last 24 months, while for children it counted the number seen in the last 12 months. These figures were produced quarterly. To estimate the number of patients who had dental treatment during each year of the study, June figures for each year were examined. The number of adults was halved to obtain an estimate of the number of adults who underwent treatment in the preceding 12 months and this was added to the figure for children seen in the previous 12 months. The number of active general medical practitioners was obtained from the British Medical Association (https://www.bma.org.uk/-/media/files/pdfs/news%20views%20analysis/press%20briefings/general-practice.pdf?la=en).
Data on other prescriber numbers, for example nurse practitioners, were not available. It was assumed, therefore, that all non-dental primary care prescribing of antibiotics was by general medical practitioners, or done under their authority.
The size of the English population between 2010-2017 (mean 54,137,125) was obtained from the Office for National Statistics (https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration).
Because all data reported herein were obtained from national data resources and completely anonymised, ethics approval was not required.
Results
Dental oral antibiotic prescribing trends
Between 2010 and 2017, there were 266,652,987 NHS prescriptions for oral antibiotics issued in the primary care setting in England by physicians, nurse practitioners, and other healthcare providers, including dentists, at a cost of £1,065,982,500. On average, this amounted to 33,331,623 prescriptions (616 prescriptions per thousand of the English population) each year at an annual cost of £133,247,813. Of these, dentists issued 28,825,698 prescriptions (Table 1), 10.8% of the total, at a cost of £49,708,614 between 2010-2017. On average, this amounted to 3,603,212 prescriptions (67 prescriptions per thousand of the English population) at £6,213,577 per annum (pa) over that period.
The mean number of actively practising dentists in England between 2010-2017 was 23,624 (Table 2) and each dentist issued, on average, 153 antibiotic prescriptions each year at a mean annual cost of £264. This compares to 41,985 general medical practitioners who, on average, issued 794 antibiotic prescriptions per year at a mean annual cost of £3,174. Between 2010-2017, 147.7 million patients received 316.5 million courses of dental treatment (Table 2). On average, therefore, one antibiotic prescription was issued for every 5.1 patients treated or for every 11 courses of dental treatment.
Between 2010-2017, dentists issued 18,667,126 amoxicillin prescriptions (Table 1) (mean 2,333,391 pa), accounting for 64.8% of all antibiotics prescribed by dentists and 18.4% of all primary care amoxicillin prescriptions (Table 3). As a class, 19,070,587 penicillin prescriptions were issued (mean 2,383,823 pa), accounting for 66.1% of dental antibiotic prescriptions and 11.2% of all primary care penicillin prescriptions. Metronidazole was the next most frequently prescribed antibiotic (8,082,568; mean 1,010,321 pa), accounting for 28.0% of all dental antibiotic prescribing (Table 1) but more than half (57%) of all metronidazole prescribing in primary care (Table 3). For comparison, all other primary care prescribing of metronidazole, ie prescribing by doctors, nurse practitioners etc but not by dentists, amounted to just 6,086,852 prescriptions between 2010-2017 (mean 760,857 pa). The next most frequently prescribed dental antibiotics were macrolides (1,301,900; mean 162,737 pa; 4.5% of dental antibiotics), of which erythromycin accounted for the vast majority (96.5%), clindamycin (167,426; mean 20,928 pa; 0.6% of dental antibiotics), cephalosporins (121,234; 15,154 pa; 0.4% of dental antibiotics) and tetracyclines (81,983; 10,248 pa; 0.3% of dental antibiotics).
Dental prescribing of oral antibiotics peaked at 3,935,698 prescriptions pa in 2011 (Table 1, Fig. 1) and then fell year on year to 2,977,430 in 2017 (a 24.4% fall). Among the penicillins (Fig. 2), amoxicillin prescribing followed a similar trend, peaking in 2011 and then falling 22.5% between 2011 and 2017. In contrast, ampicillin prescribing fell to zero in 2014 and ceased thereafter while phenoxymethylpenicillin prescribing progressively fell from 61,675 prescriptions pa in 2010 to just 12,837 in 2017 (a 79.1% fall). Prescribing of the combined agent co-amoxiclav (containing amoxicillin and the beta-lactamase inhibitor clavulanic acid), however, increased rapidly between 2010 and 2014 by 130%, from 8,540 prescriptions in 2010 to 19,620 in 2014. Following this, there was a smaller (20.6%) year on year fall to 15,578 prescriptions pa in 2017 for this drug. Finally, there was no flucloxacillin prescribing by dentists.
Cephalosporin prescribing fell steadily from 23,478 prescriptions in 2010 to 6,220 in 2017 (Table 1, Fig. 1), with a decline of 73.5%. Tetracycline prescribing also decreased steadily from 14,563 prescriptions in 2010 to 6,016 in 2017, representing a 58.7% fall.
Overall, there was a decline in macrolide prescribing between 2010 and 2017 (Table 1, Fig. 1) which was primarily due to a progressive decline in erythromycin prescribing from 184,311 prescriptions in 2010 to 107,047 in 2017 (Table 1, Fig. 3), a 41.9% fall. This was offset to some degree by a rapid increase in prescribing of both azithromycin and clarithromycin (Table 1, Fig. 3). Azithromycin prescribing increased from 301 prescriptions in 2010 to 2,236 in 2017, which was a 643% increase. Moreover, clarithromycin prescribing increased from 199 prescriptions in 2010 to 7,654 in 2017, which was a 3,746% increase.
There was a progressive decline (54.6%) in clindamycin prescribing from 31,364 prescriptions in 2010 to 14,253 in 2017 (Table 1, Fig. 1). Metronidazole prescribing peaked in 2012 at 1,096,742 prescriptions before falling by 22.8% to 846,207 in 2017 (Table 1, Fig. 1).
Amoxicillin was the most frequently prescribed antibiotic accounting for 64.8% of all antibiotic prescriptions by dentists (Fig. 4). This was followed by metronidazole (28.0%), erythromycin (4.4%), phenoxymethylpenicillin (0.9%), clindamycin (0.6%), co-amoxiclav (0.5%), cephalosporins (0.4%) and tetracyclines (0.3%). All other oral antibiotics combined accounted for only 0.1% of all dental prescribing.
Dental prescribing compared to overall primary care prescribing
The steady decline in clindamycin prescribing by dentists occurred while primary care prescribing of clindamycin overall increased (37%) from 71,395 prescriptions in 2010 to 97,905 in 2017. Dental prescribing of clindamycin, however, as a percentage of overall clindamycin prescribing, fell from 43.9% in 2010 to 14.6% in 2017 (Fig. 5). Trends in dental prescribing of other antibiotics largely paralleled those in primary care as a whole. Although overall antibiotic prescribing by dentists fell slightly more quickly. Thus, overall primary care oral antibiotic prescribing accounted for by dentists fell from 11.2% in 2010 to 10% in 2017 (Fig. 5).
Discussion
Dental antibiotic prescribing accounts for a sizable (10.8%) proportion of all NHS oral antibiotic prescribing in primary care in England. This proportion has increased slightly from the 9-10% recorded in the 1990s.3,4 However, it is higher than the 8.2% figure in 2017 that was recently cited by the report of the English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR).5 This figure is also higher than the 3% of all antibiotic prescribing reported for dentists in Australia,6 but lower than the 11.8% and 13.2%, respectively, that have been reported for Canada7 and the USA.8
Within dentistry, antibiotics are used for two general purposes, either to treat dental infections or prophylactically to prevent infections. During the period covered by our study (2010-2017), however, there were no UK guidelines recommending the prophylactic use of antibiotics within dentistry. NICE clinical guideline 64 recommending against the use of antibiotic prophylaxis to prevent infective endocarditis came into effect in 2008 and by January 2010, antibiotic prophylaxis prescribing in the UK had dropped dramatically.9,10 The Scottish Dental Clinical Effectiveness Programme implementation advice recommending that antibiotic prophylaxis should be considered for certain individuals for example, those with prosthetic and repaired heart valves, previous history of infective endocarditis and certain congenital heart conditions, did not come into effect until August 2018.11 Therefore, during the period of the study, all antibiotic prescribing should have been for treatment of dental infections although a low level of antibiotic prophylaxis prescribing by dentists did occur during this period.9 In contrast, dental prescribing in other countries during this period included prescribing of antibiotic prophylaxis for those at high-risk of infective endocarditis and, in the case of the US, for many patients with prosthetic joints.
Over the period of the study (2010-2017), after peaking in 2012, there was a 14.8% fall in overall antibiotic prescribing in primary care,12 possibly reflecting, in part, antimicrobial stewardship efforts. After peaking in 2011, the fall in dental antibiotic prescribing was even greater (24.4%), despite an upward trend in the number of dentists (Table 2). These figures are closely similar to those recently reported in the 2018 ESPAUR report.5 They reported a 13.2% fall in antibiotic prescribing in primary care between 2012 and 2017 and a 24.8% fall in dental antibiotic prescribing between 2013-2017. This decline could suggest that dentists have responded positively to the antimicrobial stewardship message to reduce unnecessary antibiotic prescribing to avoid development of antibiotic resistant organisms or it could be due to other factors, or a combination of factors. The fall was the result of declines in prescribing of seven of the eight most commonly prescribed antibiotics by dentists as follows, respectively:
- 1.
Amoxicillin (22.5%)
- 2.
Metronidazole (22.8%)
- 3.
Erythromycin (41.9%)
- 4.
Phenoxymethylpenicillin (79.1%)
- 5.
Clindamycin (54.6%)
- 6.
Cephalosporins (73.5%)
- 7.
Tetracyclines (58.7%).
The exception was co-amoxiclav; prescribing increased 82.4% between 2010 and 2017. It is possible, although not confirmed, that the decline in clindamycin prescribing could have been a response to antimicrobial stewardship messages highlighting the potential of clindamycin to cause Clostridioides (previously known as Clostridium) difficile infections that can be complicated by recurrent infection and/or life-threatening complications.13,14,15,16
In 2010, dental prescribing of clindamycin accounted for 43.9% of all oral clindamycin prescriptions in primary care but by 2017, this had fallen to just 14.6% (Table 3). This dramatic fall is explained by the fact that dental clindamycin prescribing fell over this period while it was increasing in primary care as a whole. If an antimicrobial stewardship programme resulted in the decline in clindamycin use, then this suggests the message may have been better responded to by dentists than by GPs. None-the-less, clindamycin remained the fifth most frequently prescribed dental antibiotic and warrants additional stewardship attention as recent publications have highlighted the high adverse reaction risks associated with clindamycin use such as the risk of C. difficile infection with its associated complications, including death. These risks are unparalleled among the antibiotics prescribed by dentists.13,17,18 The low and falling level of clindamycin prescribing by dentists in the UK contrasts greatly with that in the US where clindamycin is the main alternative to amoxicillin, is the second most frequently prescribed dental antibiotic and accounts for 15% of all dental antibiotic prescriptions.8
Although amoxicillin and phenoxymethylpenicillin prescribing have fallen, this was, to some extent, compensated for by a rapid 130% rise in co-amoxiclav prescribing between 2010 and 2014 and a further 21% increase between 2014 and 2017. Co-amoxiclav is a broad-spectrum antibiotic with activity against beta-lactamase-producing bacteria and therefore plays an important role in most hospital formularies for treating antibiotic-resistant and life-threatening infections. The large increase in its use in primary-care, without microbiological sensitivity testing, is therefore very concerning since its use should be reserved for situations where amoxicillin or phenoxymethylpenicillin ± metronidazole are ineffective. There are several potential reasons for the increasing popularity of co-amoxiclav. These include an increased prevalence of beta-lactamase producing bacteria isolated from the mouth,19,20,21 the effectiveness of co-amoxiclav in treating acute dentoalveolar infections,19,22,23 and the convenient twice daily dosing regimen of co-amoxiclav compared to the three times daily regimen for amoxicillin and four times daily regimen for phenoxymethylpenicillin. However, amoxicillin and phenoxymethylpenicillin ± metronidazole remain highly effective in treating acute dentoalveolar infections and co-amoxiclav should be reserved for infections where other penicillins, particularly amoxicillin, lack efficacy due to the presence of beta-lactamase producing bacteria. Moreover, co-amoxiclav may have a significantly worse adverse event profile than does amoxicillin alone.13
In dental abscesses and dentoalveolar infections related to the periodontium for example, pericoronitis, lateral periodontal abscess and acute necrotising ulcerative gingivitis (ANUG), strictly anaerobic Gram-positive cocci and Gram-negative bacilli predominate,24,25,26,27 and are pathogenic.28 This, and metronidazole's activity against anaerobes, make it a good choice for treating dental infections,24,26,29,30,31,32,33,34 particularly when patients are warned about the likelihood of unpleasant side effects if taken with alcohol. This probably accounts, in part, for the relatively small reduction in metronidazole use over the study period. Interestingly, although metronidazole is the second antibiotic of choice for dentists in the UK,35 much of Europe,36 Africa,37 Middle East,38 Indian Subcontinent39, 40 and Australasia,6, 41 in the USA clindamycin is the second most-prescribed antibiotic and metronidazole does not appear among the seven most frequently prescribed antibiotics by dentists.8
Although prescribing of erythromycin, the third most common antibiotic prescribed by dentists in England, fell by nearly 42%, this was to some extent compensated for by increased prescribing of two other azalide/macrolides, azithromycin and clarithromycin. There was a large increase in both of these over the period of study (respectively a 643% and 3,746% increase) no doubt reflecting their significant advantages over erythromycin as an alternative to amoxicillin for patients allergic to penicillins. Erythromycin requires four times daily dosage and often causes nausea, vomiting and diarrhoea. In comparison, azithromycin and clarithromycin exhibit better tissue penetration and efficacy,42,43 particularly in periodontal tissues,44 and require only once daily and twice daily dosing, respectively.
While antibiotic prescribing in dentistry has fallen, there is still scope for further reductions and a more optimal use of antibiotics within dentistry. For example, a recent study of Welsh dental antibiotic prescribing found that only 19% of antibiotics were prescribed in situations where their use was indicated by clinical guidelines45 including those published in the British National Formulary,46 by the Scottish Dental Clinical Effectiveness Programme47 and the Faculty of General Dental Practice.48 These guidelines highlight that antibiotics should not be prescribed for unexplained pyrexia, cervical lymphadenopathy or facial swelling. In addition, samples should be obtained for bacterial culture, particularly for severe infections, where laboratory support is available. The guidelines also emphasise that antibiotics should only be prescribed for treatment of identifiable oral infections for example, acute periapical or periodontal abscess, cellulitis, severe pericoronitis, localised osteitis, acute necrotising gingivitis and destructive forms of periodontal disease. Moreover, most of these infections should be managed in the first instance with early drainage and/or removal of the nidus of infection (for example, a necrotic pulp) rather than with antibiotics alone. They also point out that antibiotics are more appropriately used where there is evidence that infection is spreading, and may be required if surgical treatment has to be delayed in immunocompromised patients or those with conditions such as diabetes mellitus or Paget's disease. Certain rarer infections, such as bacterial sialadenitis, osteomyelitis, actinomycosis and Ludwig's angina, however, should prompt urgent specialist care and possibly parenteral antibiotic treatment.
Failure of a patient with infection to respond within 48 hours of surgical drainage and antibiotic initiation, should prompt reconsideration of the appropriateness of the antibiotic regimen with any change being based on bacterial culture and antibiotic susceptibility testing results. It is notable that the Welsh study found that 65.5% of antibiotics were prescribed by dentists in the absence of evidence of spreading infection, and 70.6% without operative intervention.45
Other studies support these observations and suggest that factors, such as dentists' concern about their ability to perform surgical procedures or to obtain local anaesthesia in the presence of infection plus the pressure of balancing the demands of a busy routine patient list with the addition of unscheduled emergency patients, often pressures dentists into prescribing antibiotics against guidance or best practice.49,50,51
Limitations
Although the NHS Digital Prescription Cost Analysis data that were analysed included the number of prescriptions issued in NHS primary dental care in England, it did not provide information on the reason the antibiotic was prescribed or on the appropriateness or effectiveness of the prescription. Nor did it provide information on the dose or duration of the course of antibiotic prescribed. This is important since the inappropriate prescribing of an antibiotic, or the prescribing of an antibiotic at too low a dose or for too long, are among the most important factors responsible for the selection of antibiotic resistant bacteria.1 Further studies are needed to better understand how much of the decline in dental antibiotic prescribing that we observed was related to antimicrobial stewardship efforts and/or other factors. Our data also did not cover hospital, that is, secondary care, or private primary-care prescriptions for antibiotics for which no centrally recorded data are available. We are unable, therefore, to quantify the impact of private prescribing by doctors or dentists on primary care prescribing of antibiotics in England.
Conclusions
This study highlights a number of significant changes in prescribing of oral antibiotics by dentists between 2010 and 2017. Likely as a result of antimicrobial stewardship messages, there were significant reductions in prescribing of the five antibiotics most frequently prescribed by dentists. Most notably, dental prescribing of clindamycin, which has a poor adverse drug reaction profile, including C. difficile infection, fell, while prescribing of clindamycin increased in the remainder of primary care. These results support the notion that dentists have complied with the antimicrobial stewardship message and antibiotic prescribing guidelines, with a steady downward progression in the prescribing of most commonly prescribed oral antibiotics. Nonetheless, further progress can be made, and Public Health England have produced a Dental Antimicrobial Stewardship Toolkit to help primary care practitioners promote the appropriate use of antibiotics in dentistry; available at: https://www.gov.uk/guidance/dental-antimicrobial-stewardship-toolkit#the-toolkit.
References
National Institute for Health and Care Excellence (NICE). Antimicrobial stewardship: systems and processes for effective antimicrobial medicine use 2015. Nice Guideline 15 [NG]. Available online at https://www.nice.org.uk/guidance/NG15/chapter/1-Recommendations#recommendationsforprescribers (accessed 12 November 2019).
Baddour L M, Dayer M J, Thornhill M H. Fluoroquinolone use and associated adverse drug events in England. J Infect 2019; 78: 249-259.
Longman L P, Martin M V. The use of antibiotics in the prevention of post-operative infection: a re-appraisal. Br Dent J 1991; 170: 257-262.
Martin M V, Longman L P, Hill J B, Hardy P. Acute dentoalveolar infections: an investigation of the duration of antibiotic therapy. Br Dent J 1997; 183: 135-137.
Public Health England. English surveillance programme for antimicrobial utilisation and resistance (ESPAUR). London: Public Health England, 2018.
Teoh L, Stewart K, Marino R J, McCullough M J. Part 1. Current prescribing trends of antibiotics by dentists in Australia from 2013 to 2016. Aust Dent J 2018; DOI: 10.1111/adj.12622.
Marra F, George D, Chong M, Sutherland S, Patrick D M. Antibiotic prescribing by dentists has increased: Why? J Am Dent Assoc 2016; 147: 320-327.
Durkin M J, Hsueh K, Sallah Y H et al. An evaluation of dental antibiotic prescribing practices in the United States. J Am Dent Assoc 2017; 148: 878-886.
Dayer M J, Jones S, Prendergast B, Baddour L M, Lockhart P B, Thornhill M H. Incidence of infective endocarditis in England, 2000-2013: a secular trend, interrupted time-series analysis. Lancet 2015; 385: 1219-1228.
Thornhill M H, Dayer M J, Forde J M et al. Impact of the NICE guideline recommending cessation of antibiotic prophylaxis for prevention of infective endocarditis: before and after study. BMJ 2011; 342: d2392.
SDCEP. Antibiotic prophylaxis against infective endocarditis 2018. (Updated 23rd August 2018.) Available online at http://www.sdcep.org.uk/published-guidance/antibiotic-prophylaxis/ (accessed 12 November 2019).
Baddour L M, Dayer M J, Thornhill M H. Adverse drug reactions due to oral antibiotics in the community setting - England. Infectious Diseases 2019; 51: 866-869.
Thornhill M H, Dayer M J, Durkin M J, Lockhart P B, Baddour L M. Risk of adverse reactions to oral antibiotics prescribed by dentists. J Dent Res 2019; 98: 1081-1087.
Bartlett J G, Chang T W, Gurwith M, Gorbach S L, Onderdonk A B. Antibiotic-associated pseudomembranous colitis due to toxin-producing clostridia. N Engl J Med 1978; 298: 531-534.
Lusk R H, Fekety F R Jr., Silva J Jr. et al. Gastrointestinal side effects of clindamycin and ampicillin therapy. The Journal of infectious diseases. 1977; 135 Suppl: S111-119.
Thornhill M H, Dayer M J, Prendergast B, Baddour L M, Jones S, Lockhart P B. Incidence and nature of adverse reactions to antibiotics used as endocarditis prophylaxis. J Antimicrob Chemother 2015; 70: 2382-2388.
Brown K A, Khanafer N, Daneman N, Fisman D N. Meta-analysis of antibiotics and the risk of community-associated Clostridium difficile infection. Antimicrob Agents Chemother 2013; 57: 2326-2332.
Beacher N, Sweeney M P, Bagg J. Dentists, antibiotics and Clostridium difficile-associated disease. Br Dent J 2015; 219: 275-279.
Eick S, Pfister W, Straube E. Antimicrobial susceptibility of anaerobic and capnophilic bacteria isolated from odontogenic abscesses and rapidly progressive periodontitis. Int J Antimicrob Agents 1999; 12: 41-46.
Handal T, Olsen I. Antimicrobial resistance with focus on oral beta-lactamases. Eur J Oral Sci 2000; 108: 163-174.
Handal T, Olsen I, Walker C B, Caugant D A. Beta-lactamase production and antimicrobial susceptibility of subgingival bacteria from refractory periodontitis. Oral Microbiol Immunol 2004; 19: 303-308.
Baumgartner J C, Xia T. Antibiotic susceptibility of bacteria associated with endodontic abscesses. J Endod 2003; 29: 44-47.
Lewis M A, Carmichael F, MacFarlane T W, Milligan S G. A randomised trial of co-amoxiclav (Augmentin) versus penicillin V in the treatment of acute dentoalveolar abscess. Br Dent J 1993; 175: 169-174.
Ellison S J. The role of phenoxymethylpenicillin, amoxicillin, metronidazole and clindamycin in the management of acute dentoalveolar abscessesa review. Br Dent J 2009; 206: 357-362.
Lewis M A, MacFarlane T W, McGowan D A. Quantitative bacteriology of acute dento-alveolar abscesses. J Med Microbiol 1986; 21: 101-104.
Lewis M A, MacFarlane T W, McGowan D A. A microbiological and clinical review of the acute dentoalveolar abscess. Br J Oral Maxillofac Surg 1990; 28: 359-366.
Stefanopoulos P K, Kolokotronis A E. The clinical significance of anaerobic bacteria in acute orofacial odontogenic infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004; 98: 398-408.
Lewis M A, MacFarlane T W, McGowan D A, MacDonald D G. Assessment of the pathogenicity of bacterial species isolated from acute dentoalveolar abscesses. J Med Microbiol 1988; 27: 109-116.
Hood F J. The place of metronidazole in the treatment of acute oro-facial infection. J Antimicrob Chemother 1978; 4 Suppl C: 71-73.
Kuriyama T, Williams D W, Yanagisawa M et al. Antimicrobial susceptibility of 800 anaerobic isolates from patients with dentoalveolar infection to 13 oral antibiotics. Oral Microbiol Immunol 2007; 22: 285-288.
Lewis M A, MacFarlane T W, McGowan D A. Antibiotic susceptibilities of bacteria isolated from acute dentoalveolar abscesses. J Antimicrob Chemother 1989; 23: 69-77.
Sandor G K, Low D E, Judd P L, Davidson R J. Antimicrobial treatment options in the management of odontogenic infections. J Can Dent Assoc 1998; 64: 508-514.
Barker G R, Qualtrough A J. An investigation into antibiotic prescribing at a dental teaching hospital. Br Dent J 1987; 162: 303-306.
Olson A K, Edington E M, Kulid J C, Weller R N. Update on antibiotics for the endodontic practice. Compendium 1990; 11: 328-332.
Palmer N O, Martin M V, Pealing R, Ireland R S. An analysis of antibiotic prescriptions from general dental practitioners in England. J Antimicrob Chemother 2000; 46: 1033-1035.
Al-Haroni M, Skaug N. Incidence of antibiotic prescribing in dental practice in Norway and its contribution to national consumption. J Antimicrob Chemother 2007; 59: 1161-1166.
Fadare J O, Oshikoya K A, Obimakinde O S et al. Patterns of drugs prescribed for dental outpatients in Nigeria: findings and implications. Acta Odontol Scand 2017; 75: 496-506.
Dar-Odeh N S, Abu-Hammad O A, Khraisat A S, El Maaytah M A, Shehabi A. An analysis of therapeutic, adult antibiotic prescriptions issued by dental practitioners in Jordan. Chemotherapy 2008; 54: 17-22.
Konde S, Jairam L S, Peethambar P, Noojady S R, Kumar N C. Antibiotic overusage and resistance: A cross-sectional survey among paediatric dentists. J Indian Soc Paedod Prev Dent 2016; 34: 145-151.
Tanwir F, Marrone G, Tariq A, Lundborg C S. Diagnosis and prescribing pattern of antibiotics and painkillers among dentists. Oral Health Prev Dent 2015; 13: 75-83.
Ford P J, Saladine C, Zhang K, Hollingworth S A. Prescribing patterns of dental practitioners in Australia from 2001 to 2012. Antimicrobials. Aust Dent J 2017; 62: 52-57.
Schentag J J, Ballow C H. Tissue-directed pharmacokinetics. Am J Med 1991; 91: 5S-11S.
Williams J D, Sefton A M. Comparison of macrolide antibiotics. J Antimicrob Chemother 1993; 31 Suppl C: 11-26.
Malizia T, Tejada M R, Ghelardi E et al. Periodontal tissue disposition of azithromycin. J Periodontol 1997; 68: 1206-1209.
Cope A L, Francis N A, Wood F, Chestnutt I G. Antibiotic prescribing in UK general dental practice: a cross-sectional study. Community Dent Oral Epidemiol 2016; 44: 145-153.
British Medical Association & Royal Pharmaceutical Society. BNF - The British National Formulary: BMJ Group and Pharmaceutical Press, 2019.
Scottish Dental Clinical Effectiveness Programme. Drug Prescribing for Dentistry 2016. Available online at http://www.sdcep.org.uk/published-guidance/drug-prescribing/ (accessed 12 November 2019).
Faculty of General Dental Practice. Antimicrobial prescribing for GDPs. London: Royal College of Surgeons of England Faculty of General Dental Practice, 2016.
Cope A L, Chestnutt I G. Inappropriate prescribing of antibiotics in primary dental care: reasons and resolutions. Prim Dent J 2014; 3: 33-37.
Cope A L, Wood F, Francis N A, Chestnutt I G. General dental practitioners' perceptions of antimicrobial use and resistance: a qualitative interview study. Br Dent J 2014; 217: E9.
Thompson W, Tonkin-Crine S, Pavitt S H et al. Factors associated with antibiotic prescribing for adults with acute conditions: an umbrella review across primary care and a systematic review focusing on primary dental care. J Antimicrob Chemother 2019; 74: 2139-2152.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thornhill, M., Dayer, M., Durkin, M. et al. Oral antibiotic prescribing by NHS dentists in England 2010-2017. Br Dent J 227, 1044–1050 (2019). https://doi.org/10.1038/s41415-019-1002-3
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-1002-3
- Springer Nature Limited
This article is cited by
-
AAA: a rock and a hard place
British Dental Journal (2021)
-
Can antibiotic prescribing recover its downward trajectory during 2021?
BDJ In Practice (2021)
-
Biofilm viability checker: An open-source tool for automated biofilm viability analysis from confocal microscopy images
npj Biofilms and Microbiomes (2021)
-
How did COVID-19 impact on dental antibiotic prescribing across England?
British Dental Journal (2020)