Abstract
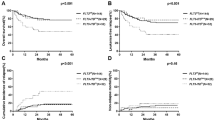
Given the controversies in the prognostic value of KIT mutations and optimal thresholds and time points of MRD monitoring for AML with CBFB-MYH11, we retrospectively evaluated 88 patients who underwent allogeneic hematopoietic stem cell transplantation (Allo-HSCT, n = 60) or autologous HSCT (Auto-HSCT, n = 28). The D816V KIT mutation was significantly associated with post-transplant relapse, contrasting with other types of mutations in KIT. Pre- and post-transplant (3 months after transplant) CBFB-MYH11 MRD assessments were useful in predicting post-transplant relapse and poor survival. The optimal threshold was determined as a 2 log reduction at both time points. In multivariate analysis, the D816V KIT mutation and CBFB-MYH11 MRD assessments were independently associated with post-transplant relapse and survival. Stratification by D816V KIT and pre-transplant CBFB-MYH11 MRD status further distinguished the risk of relapse and survival. Auto-HSCT was superior to Allo-HSCT in MRD negative patients without D816V KIT, while Allo-HSCT trended to be superior to Auto-HSCT in patients with MRD positivity or the D816V KIT mutation. In conclusion, this study demonstrated the differentiated prognostic value of the D816V KIT mutation in AML with CBFB-MYH11 and clarified optimal time points and thresholds for CBFB-MYH11 MRD monitoring in the setting of HSCT.



Similar content being viewed by others
References
Dohner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Buchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–47.
Jourdan E, Boissel N, Chevret S, Delabesse E, Renneville A, Cornillet P, et al. Prospective evaluation of gene mutations and minimal residual disease in patients with core binding factor acute myeloid leukemia. Blood. 2013;121:2213–23.
Marcucci G, Mrozek K, Ruppert AS, Maharry K, Kolitz JE, Moore JO, et al. Prognostic factors and outcome of core binding factor acute myeloid leukemia patients with t(8;21) differ from those of patients with inv(16): a Cancer and Leukemia Group B study. J Clin Oncol. 2005;23:5705–17.
Schlenk RF, Benner A, Krauter J, Buchner T, Sauerland C, Ehninger G, et al. Individual patient data-based meta-analysis of patients aged 16 to 60 years with core binding factor acute myeloid leukemia: a survey of the German Acute Myeloid Leukemia Intergroup. J Clin Oncol. 2004;22:3741–50.
Mosna F, Papayannidis C, Martinelli G, Di Bona E, Bonalumi A, Tecchio C, et al. Complex karyotype, older age, and reduced first-line dose intensity determine poor survival in core binding factor acute myeloid leukemia patients with long-term follow-up. Am J Hematol. 2015;90:515–23.
Ishikawa Y, Kawashima N, Atsuta Y, Sugiura I, Sawa M, Dobashi N, et al. Prospective evaluation of prognostic impact of KIT mutations on acute myeloid leukemia with RUNX1-RUNX1T1 and CBFB-MYH11. Blood Adv. 2020;4:66–75.
Duployez N, Marceau-Renaut A, Boissel N, Petit A, Bucci M, Geffroy S, et al. Comprehensive mutational profiling of core binding factor acute myeloid leukemia. Blood. 2016;127:2451–9.
Opatz S, Bamopoulos SA, Metzeler KH, Herold T, Ksienzyk B, Braundl K, et al. The clinical mutatome of core binding factor leukemia. Leukemia. 2020;34:1553–62.
Yin JA, O’Brien MA, Hills RK, Daly SB, Wheatley K, Burnett AK. Minimal residual disease monitoring by quantitative RT-PCR in core binding factor AML allows risk stratification and predicts relapse: results of the United Kingdom MRC AML-15 trial. Blood. 2012;120:2826–35.
Chen W, Xie H, Wang H, Chen L, Sun Y, Chen Z, et al. Prognostic significance of KIT mutations in core-binding factor acute myeloid leukemia: a systematic review and meta-analysis. PLoS One. 2016;11:e0146614.
Cho BS, Min GJ, Park SS, Park S, Jeon YW, Shin SH, et al. Prognostic impacts of D816V KIT mutation and peri-transplant RUNX1-RUNX1T1 MRD monitoring on acute myeloid leukemia with RUNX1-RUNX1T1. Cancers. 2021;13:336.
Schuurhuis GJ, Heuser M, Freeman S, Bene MC, Buccisano F, Cloos J, et al. Minimal/measurable residual disease in AML: a consensus document from the European LeukemiaNet MRD Working Party. Blood. 2018;131:1275–91.
Tang FF, Xu LP, Zhang XH, Chen H, Chen YH, Han W, et al. Monitoring of post-transplant CBFB-MYH11 as minimal residual disease, rather than KIT mutations, can predict relapse after allogeneic haematopoietic cell transplantation in adults with inv(16) acute myeloid leukaemia. Br J Haematol. 2018;180:448–51.
Xiaosu Z, Leqing C, Yazhen Q, Yu W, Xiaohui Z, Lanping X, et al. Classifying AML patients with inv(16) into high-risk and low-risk relapsed patients based on peritransplantation minimal residual disease determined by CBFbeta/MYH11 gene expression. Ann Hematol. 2019;98:73–81.
Duan W, Liu X, Jia J, Wang J, Gong L, Jiang Q, et al. The loss or absence of minimal residual disease of <0.1% at any time after two cycles of consolidation chemotherapy in CBFB-MYH11-positive acute myeloid leukaemia indicates poor prognosis. Br J Haematol. 2021;192:265–71.
Gorin NC, Labopin M, Frassoni F, Milpied N, Attal M, Blaise D, et al. Identical outcome after autologous or allogeneic genoidentical hematopoietic stem-cell transplantation in first remission of acute myelocytic leukemia carrying inversion 16 or t(8;21): a retrospective study from the European Cooperative Group for Blood and Marrow Transplantation. J Clin Oncol. 2008;26:3183–8.
Nakasone H, Izutsu K, Wakita S, Yamaguchi H, Muramatsu-Kida M, Usuki K. Autologous stem cell transplantation with PCR-negative graft would be associated with a favorable outcome in core-binding factor acute myeloid leukemia. Biol Blood Marrow Transpl. 2008;14:1262–9.
Kuwatsuka Y, Miyamura K, Suzuki R, Kasai M, Maruta A, Ogawa H, et al. Hematopoietic stem cell transplantation for core binding factor acute myeloid leukemia: t(8;21) and inv(16) represent different clinical outcomes. Blood. 2009;113:2096–103.
Shin HJ, Min WS, Min YH, Cheong JW, Lee JH, Kim IH, et al. Different prognostic effects of core-binding factor positive AML with Korean AML registry data. Ann Hematol. 2019;98:1135–47.
Yoon JH, Kim HJ, Kim JW, Jeon YW, Shin SH, Lee SE, et al. Identification of molecular and cytogenetic risk factors for unfavorable core-binding factor-positive adult AML with post-remission treatment outcome analysis including transplantation. Bone Marrow Transpl. 2014;49:1466–74.
Yoon JH, Kim HJ, Park SS, Jeon YW, Lee SE, Cho BS, et al. Clinical outcome of autologous hematopoietic cell transplantation in adult patients with acute myeloid leukemia: who may benefit from autologous hematopoietic cell transplantation? Biol Blood Marrow Transpl. 2017;23:588–97.
Jang W, Yoon JH, Park J, Lee GD, Kim J, Kwon A, et al. Significance of KIT exon 17 mutation depends on mutant level rather than positivity in core-binding factor acute myeloid leukemia. Blood Cancer J. 2016;6:e387.
Boissel N, Leroy H, Brethon B, Philippe N, de Botton S, Auvrignon A, et al. Incidence and prognostic impact of c-Kit, FLT3, and Ras gene mutations in core binding factor acute myeloid leukemia (CBF-AML). Leukemia. 2006;20:965–70.
Yu G, Yin C, Wu F, Jiang L, Zheng Z, Xu D, et al. Gene mutation profile and risk stratification in AML1ETOpositive acute myeloid leukemia based on nextgeneration sequencing. Oncol Rep. 2019;42:2333–44.
Kim HJ, Ahn HK, Jung CW, Moon JH, Park CH, Lee KO, et al. KIT D816 mutation associates with adverse outcomes in core binding factor acute myeloid leukemia, especially in the subgroup with RUNX1/RUNX1T1 rearrangement. Ann Hematol. 2013;92:163–71.
Tarlock K, Alonzo TA, Wang YC, Gerbing RB, Ries R, Loken MR, et al. Functional properties of KIT mutations are associated with differential clinical outcomes and response to targeted therapeutics in CBF acute myeloid leukemia. Clin Cancer Res. 2019;25:5038–48.
Qin YZ, Xu LP, Chen H, Jiang Q, Wang Y, Jiang H, et al. Allogeneic stem cell transplant may improve the outcome of adult patients with inv(16) acute myeloid leukemia in first complete remission with poor molecular responses to chemotherapy. Leuk Lymphoma. 2015;56:3116–23.
Wang Y, Wu DP, Liu QF, Qin YZ, Wang JB, Xu LP, et al. In adults with t(8;21)AML, posttransplant RUNX1/RUNX1T1-based MRD monitoring, rather than c-KIT mutations, allows further risk stratification. Blood. 2014;124:1880–6.
Faber ZJ, Chen X, Gedman AL, Boggs K, Cheng J, Ma J, et al. The genomic landscape of core-binding factor acute myeloid leukemias. Nat Genet. 2016;48:1551–56.
Sula M, Bacher U, Oppliger Leibundgut E, Mansouri Taleghani B, Novak U, Pabst T. Excellent outcome after consolidation with autologous transplantation in patients with core binding factor acute myeloid leukemia. Bone Marrow Transpl. 2020;55:1690–93.
Hansrivijit P, Gale RP, Barrett J, Ciurea SO. Cellular therapy for acute myeloid Leukemia - current status and future prospects. Blood Rev. 2019;37:100578.
Greiner J, Gotz M, Bunjes D, Hofmann S, Wais V. Immunological and clinical impact of manipulated and unmanipulated DLI after allogeneic stem cell transplantation of AML patients. J Clin Med. 2019;9:39.
Paschka P, Schlenk RF, Weber D, Benner A, Bullinger L, Heuser M, et al. Adding dasatinib to intensive treatment in core-binding factor acute myeloid leukemia-results of the AMLSG 11-08 trial. Leukemia. 2018;32:1621–30.
Acknowledgements
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Education (NRF-2018R1D1A1B07043395) and a grant from the National R & D Program for Cancer Control, Ministry for Health and Welfare, Republic of Korea (HA17C0042).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Cho, BS., Min, GJ., Park, SS. et al. Prognostic values of D816V KIT mutation and peri-transplant CBFB-MYH11 MRD monitoring on acute myeloid leukemia with CBFB-MYH11. Bone Marrow Transplant 56, 2682–2689 (2021). https://doi.org/10.1038/s41409-021-01384-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-021-01384-w
- Springer Nature Limited