Abstract
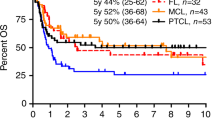
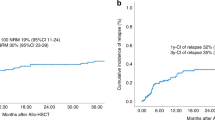
Autologous hematopoietic stem cell transplantation (ASCT) is a well-established treatment strategy in HIV-related lymphoma patients (HIV+ Ly). Nevertheless, current evidence is mainly based on reports from specialized centers, multicentre heterogeneous studies, noncomparative analyses, or registry data-based comparisons. Likewise, the risk of infections reported so far for this population, seems to be similar to that of HIV- patients, and it does not seem to impact on mortality. We report a single-center retrospective comparative analysis of AHCT procedural results, infectious complications and survival in HIV+ Ly matched with a non-HIV comparative cohort. Thirty-three HIV+ patients and 45 matched controls, who underwent ASCT between 2000 and 2016, were included. Transplant-related toxicity, event-free survival, relapse rate, and overall survival were similar in both groups. Engraftment was delayed in HIV+ Ly (neutrophils: 15 vs 12 days (p = 0.0001), and platelets 39 vs 16 days (p = 0.00001)). Bacterial infections during the pre-engraftment period were more frequent in HIV+ Ly (RR 2.24, p = 0.017), as well as viral infections in the postengraftment period (RR 3.22, p = 0.004). CMV reactivation was more frequent in HIV+ Ly (39% vs 15% p = 0.007). In conclusion, ASCT is viable and effective in HIV+ Ly, but it is associated with a higher risk of infection.







Similar content being viewed by others
References
Hogg R, Lima V, Sterne JA, Grabar S, Battegay M, Bonarek M, et al. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;372:293–9.
Marcus JL, Chao CR, Leyden WA, Xu L, Quesenberry CP, Klein DB, et al. Narrowing the gap in life expectancy between HIV-infected and HIV-uninfected individuals with access to care. J Acquir Immune Defic Syndr. 2016;73:39–46.
Powles T, Robinson D, Stebbing J, Shamash J, Nelson M, Gazzard B, et al. Highly active antiretroviral therapy and the incidence of non-AIDS-defining cancers in people with HIV infection. J Clin Oncol J Am Soc Clin Oncol 2009;27:884–90.
Goedert JJ, Bower M. Impact of highly effective antiretroviral therapy on the risk for Hodgkin lymphoma among people with human immunodeficiency virus infection. Curr Opin Oncol. 2012;24:531–6.
Morlat P, Roussillon C, Henard S, Salmon D, Bonnet F, Cacoub P, et al. Causes of death among HIV-infected patients in France in 2010 (national survey): trends since 2000. AIDS. 2014;28:1181–91.
Coghill AE, Shiels MS, Suneja G, Engels EA. Elevated cancer-specific mortality among HIV-infected patients in the United States. J Clin Oncol. 2015;33:2376–83.
Balsalobre P, Díez-Martín JL, Re A, Michieli M, Ribera JM, Canals C, et al. Autologous stem-cell transplantation in patients with HIV-related lymphoma. J Clin Oncol J Am Soc Clin Oncol. 2009;27:2192–8.
Salgado M, Kwon M, Gálvez C, Badiola J, Nijhuis M, Bandera A, et al. Mechanisms that contribute to a profound reduction of the HIV-1 reservoir after allogeneic stem cell transplant. Ann Intern Med. 2018;169:674.
Zaia JA, Forman SJ. Transplantation in HIV-infected subjects: is cure possible? Hematol Am Soc Hematol Educ Program. 2013;2013:389–93.
Kwon M, Bailén R, Balsalobre P, Jurado M, Bermudez A, Badiola J, et al. Allogeneic stem-cell transplantation in HIV-1-infected patients with high-risk hematological disorders. AIDS. 2019;33:1441–7.
Gabarre J, Leblond V, Sutton L, Azar N, Jouan M, Boccaccio C, et al. Autologous bone marrow transplantation in relapsed HIV-related non-Hodgkin’s lymphoma. Bone Marrow Transplant. 1996;18:1195–7.
Krishnan A, Zaia J, Forman SJ. Should HIV-positive patients with lymphoma be offered stem cell transplants? Bone Marrow Transplant. 2003;32:741–8.
Molina A, Krishnan AY, Nademanee A, Zabner R, Sniecinski I, Zaia J, et al. High dose therapy and autologous stem cell transplantation for human immunodeficiency virus-associated non-Hodgkin lymphoma in the era of highly active antiretroviral therapy. Cancer. 2000;89:680–9.
Díez-Martín JL, Balsalobre P, Re A, Michieli M, Ribera JM, Canals C, et al. Comparable survival between HIV+ and HIV− non-Hodgkin and Hodgkin lymphoma patients undergoing autologous peripheral blood stem cell transplantation. Blood. 2009;113:6011–4.
Simonelli C, Zanussi S, Pratesi C, Rupolo M, Talamini R, Caffau C, et al. Immune recovery after autologous stem cell transplantation is not different for HIV-infected versus HIV-uninfected patients with relapsed or refractory lymphoma. Clin Infect Dis Publ Infect Dis Soc Am. 2010;50:1672–9.
Alvarnas JC, Le Rademacher J, Wang Y, Little RF, Akpek G, Ayala E, et al. Autologous hematopoietic cell transplantation for HIV-related lymphoma: results of the BMT CTN 0803/AMC 071 trial. Blood. 2016;128:1050–8.
Reid E, Suneja G, Ambinder RF, Ard K, Baiocchi R, Barta SK, et al. Cancer in people living with HIV, version 1.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2018;16:986–1017.
Uldrick TS, Ison G, Rudek MA, Noy A, Schwartz K, Bruinooge S, et al. Modernizing clinical trial eligibility criteria: recommendations of the American Society of clinical oncology-friends of cancer research HIV Working Group. J Clin Oncol J Am Soc Clin Oncol 2017;35:3774–80.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9.
Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol J Am Soc Clin Oncol. 2014;32:3059–68.
Caro-Murillo AM, Gil Luciano A, Navarro Rubio G, Leal Noval M, Blanco Ramos JR.Cohorte de la Red de Investigación en Sida (CoRIS HIV infection in different age groups: potential implications for prevention. CoRIS Cohort, Spain, 2004–2008. Med Clin. 2010;134:521–7.
Caro-Murillo AM, Gutiérrez F, Manuel Ramos J, Sobrino P, Miró JM, López-Cortés LF. et al. HIV infection in immigrants in Spain: epidemiological characteristics and clinical presentation in the CoRIS Cohort (2004–2006). Enferm Infecc Microbiol Clin. 2009;27:380–8.
Cingolani A, Cozzi Lepri A, Teofili L, Galli L, Mazzotta V, Baldin GM, et al. Survival and predictors of death in people with HIV-associated lymphoma compared to those with a diagnosis of lymphoma in general population. PLoS ONE. 2017;12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5663375/.
Carbone A, Volpi CC, Gualeni AV, Gloghini A. Epstein-Barr virus associated lymphomas in people with HIV. Curr Opin HIV AIDS. 2017;12:39–46.
Moraes Filho AV, de, Carvalho C, de JS, Carneiro CC, Vale CR, do, Lima DC, et al. Genotoxic and cytotoxic effects of antiretroviral combinations in mice bone marrow. PloS ONE 2016;11:e0165706.
Wickramasinghe SN, Beatty C, Shiels S, Tomlinson DR, Harris JR. Ultrastructure of the bone marrow in HIV infection: evidence of dyshaemopoiesis and stromal cell damage. Clin Lab Haematol. 1992;14:213–29.
Kovacic JC, Macdonald P, Freund J, Rasko JEJ, Allan R, Fernandes VB, et al. Profound thrombocytopenia related to G-CSF. Am J Hematol. 2007;82:229–30.
Holtzer CD, Stanley HD, Jacobson MA. Severe reversible thrombocytopenia caused by recombinant human granulocyte colony-stimulating factor in an AIDS patient receiving chronic ganciclovir therapy. AIDS. 1997;11:1403–5.
Spector SA, Wong R, Hsia K, Pilcher M, Stempien MJ. Plasma cytomegalovirus (CMV) DNA load predicts CMV disease and survival in AIDS patients. J Clin Investig. 1998;101:497–502.
Wohl DA, Zeng D, Stewart P, Glomb N, Alcorn T, Jones S, et al. Cytomegalovirus viremia, mortality, and end-organ disease among patients with AIDS receiving potent antiretroviral therapies. J Acquir Immune Defic Syndr. 2005;38:538–44.
Bigliano P, Calcagno A, Lucchini A, Audagnotto S, Montrucchio C, Marinaro L, et al. The outcome of HIV-positive late presenters according to detectable CMV DNA and anti-CMV treatment. Antivir Ther. 2018;23:451–6.
Krishnan A, Palmer JM, Zaia JA, Tsai N-C, Alvarnas J, Forman SJ. HIV status does not affect the outcome of autologous stem cell transplantation (ASCT) for non-Hodgkin lymphoma (NHL). Biol Blood Marrow Transplant. 2010;16:1302–8.
Acknowledgements
The authors greatly acknowledge the members of the Infectious Diseases and Microbiology Department of Hospital Gregorio Marañón for their essential contribution to HIV-infected patients’ diagnosis, treatment optimization, and follow-up. I am grateful to Dr Gayoso for his dedication and support in my training in transplant and lymphoma field. I want to give special thanks to Dr Juan Churruca for his important contribution to the development of this study and I want to particularly thank to JLDM and MK for giving me the opportunity to carry out this study.
Author information
Authors and Affiliations
Contributions
MB, PB, JLDM, and MK, were responsible for the study design. MB, ND, RB, and DS were involved in data collection and statistical analysis, MB and MK wrote the paper and all authors contributed to the revision of the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics
The study was conducted in accordance with the Declaration of Helsinki. The institutional review board approved the study and written informed consent was obtained from all participants regarding data collection and analysis for publication.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bastos-Oreiro, M., Balsalobre, P., Miralles, P. et al. Autologous stem cell transplantation for lymphoma in HIV+ patients: higher rate of infections compared with non-HIV lymphoma. Bone Marrow Transplant 55, 1716–1725 (2020). https://doi.org/10.1038/s41409-020-0846-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-0846-0
- Springer Nature Limited