Abstract
Given the early use of triplet and quadruplet regimens, most patients with multiple myeloma (MM) will be exposed and/or refractory to PIs, IMiDs, and anti-CD38 mAbs after first- or second-line treatment. Effective treatment for this group of triple class exposed/refractory (TCE/R) patients is crucial. Here we present a post-hoc subgroup analysis of TCE/R patients treated on the ALGONQUIN study of belantamab mafodotin plus pomalidomide-dexamethasone (belamaf-Pd) for relapsed MM. Of the 99 patients treated on the ALGONQUIN study, 69 were TCE and 56 were TCR and were included in this analysis. Patients had a median of three prior lines of therapy. The ORR was 86.4% in TCE patients and 84.9% in TCR patients, with ≥ very good partial response rates of 64% and 68% respectively. The median progression free survival was 18.3 months in TCE patients and 19.6 months in TCR patients, with overall survival not yet reached and 34.4 months, respectively for TCE and TCR patients. No new safety signals were identified. The most common Grade ≥ 3 AEs were keratopathy (48%), decreased visual acuity (42%), neutropenia (36%), thrombocytopenia (27%), and infection (25%). In this subgroup analysis of the ALGONQUIN study, patients with TCE/TCR disease treated with belamaf-Pd achieved high clinical response rates with durable remissions, comparable to other novel therapeutics in this space.
Similar content being viewed by others
Introduction
Multiple myeloma (MM) is a malignancy of terminally differentiated plasma cells. The treatment of MM has evolved rapidly over the last two decades, with the advent of novel therapeutics leading to significant increases in patient survival [1, 2]. Despite substantial improvement in patient outcomes, MM remains incurable in most patients and disease relapse is expected [3]. The mainstays of treatment for newly diagnosed and relapsed patients include various combinations of proteosome inhibitors (PIs; [bortezomib, carfilzomib, ixazomib]), immunomodulatory drugs (IMiDs; [lenalidomide, pomalidomide, thalidomide]), anti-CD38 monoclonal antibodies (mAbs; [daratumuab, isatuximab]), as well autologous stem cell transplantation (ASCT) in select fit patients based on Phase 3 trials [4,5,6,7,8,9,10,11].
Ultimately, patients become triple class refractory (TCR; refractory to a PI, IMiD, and anti-CD38 mAb) or, increasingly, penta-drug refractory (refractory to bortezomib, carfilzomib, lenalidomide, pomalidomide, and daratumumab). With the upfront use of triplets and now quadruplets including a PI, IMiD, anti-CD38 mAb, and dexaemethasone in first line [12,13,14], this is occurring after first- or second-line treatment in many jurisdictions. Once patients are refractory to treatment, outcomes with current widely available therapeutics are almost universally poor, with median progression free survival (mPFS) and median overall survival (mOS) ranging from 3.9–4.4 months and 10.5–11.1 months, respectively [15, 16]. Therefore, new agents exploiting novel targets are required. B cell maturation antigen (BCMA) is a cell surface protein universally expressed on plasma cells and has become a therapeutic target for patients with MM using various platforms including BCMA targeted antibody-drug conjugates (ADCs), bispecific antibodies (bispecifics), and chimeric antigen receptor T cells (Car-Ts) [17,18,19,20,21].
Belantamab mafodotin (belamaf) is a first in class afucosylated humanized anti-BCMA IgG1 mAb conjugated to microtubule disrupting monomethyl auristatin F (MMAF). It binds to FcγRIIIa on plasma cells resulting in activation and recruitment of immune effector cells and enhanced antibody-dependent cell-mediated cytotoxicity (ADCC) [17]. Belamaf has single agent activity as demonstrated in the DREAMM-1 First In Human trial, in which patients with heavily pre-treated relapsed/refractory MM (RRMM) enrolled in Part 2 of the study had an overall response rate (ORR) of 60% (95% confidence interval [CI]: 42.1–76.1); 46.2% (95% CI: 19.2–74.9) in patients who had previously had > five prior therapies and 68.2% (95% CI: 45.1–86.1) in those with ≤ five prior lines [22]. Notably, single agent belamaf had an ORR of 38.5% (95% CI: 13.9–68.4) in patients refractory to an IMiD, a PI and were daratumumab exposed [23]. At median follow up of 12.5 months, the mPFS was 12 months (95% CI: 3.1–not estimable), 6.2 months in those that were triple class exposed (TCE) [23]. The single agent clinical activity was subsequently confirmed in the Phase 2, DREAMM-2 trial, where all patients were TCR. For the patients that received single agent belamaf (2.5 mg/kg every three weeks) the ORR was 31% (97.5% CI: 20.8–42.6) and the median duration of response (mDOR) was 11 months [4]. Finally, the DREAMM-3 Phase 3 study compared single agent belamaf to pomalidomide and dexamethasone (Pd). Although the study did not meet its primary endpoint of PFS superiority over Pd (11.2 vs 7.0 months; HR 1.03; 95% CI: 0.72–1.47), the study reaffirmed the clinical activity of belamaf in heavily pre-treated patients.
The promising single agent activity in heavily pre-treated patients has supported the development of belamaf-combination regimens. The Canadian Myeloma Research Group ALGONQUIN trial is a two-part study evaluating belamaf in combination with Pd for patients that are lenalidomide refractory and PI exposed. We have recently reported outcomes of the dose and schedule optimization of the combination. We identified 2.5 mg/kg as the maximally tolerated dose (MTD) combined with standard dosing of Pd and a recommended part 2 dose (RP2D) and schedule of belamaf 2.5 mg/kg administered every eight weeks (Q8W) [24]. For the intent to treat population, the ORR was 87.7% and the PFS was 21.8 months. Herein, we report a post- hoc subgroup analysis of patients treated on the ALGONQUIN study who were TCE and/or TCR.
Methods
Study design and participants
The ALGONQUIN study is a multicenter, open-label, single arm, 2-Part study (ClinicalTrials.gov Identifier: NCT03715478) evaluating the combination of belamaf +Pd conducted at nine Canadian academic centres. Part 1 was a dose-exploration phase using a standard 3 + 3 dose escalation design to determine the MTD patients enrolled at belamaf doses of 1.92, 2.5, and 3.4 mg/kg combined with standard dose Pd; up to 12 patients could be enrolled in each dose cohort and the option of additional dosing cohorts to better inform the RP2D was included in the protocol. Part 2 consisted of an expansion cohort of 26 patients to further evaluate safety and efficacy of the RP2D established in Part 1 and an additional cohort of 12 patients (cohort 2b) treated at the RP2D but exploring an alternative dose modification schedule for corneal adverse events (AEs).
We enrolled patients with RRMM aged ≥18 with Eastern Cooperative Oncology Group (ECOG) performance status of 0–2 and adequate bone marrow, cardiac and renal function who had progressive disease after ≥ one treatment line including a PI and lenalidomide (combined or in separate lines). Patients were excluded if they had unstable comorbidities or laboratory abnormalities that may affect their safety, ability to provide consent, compliance with study procedures, or if they had concurrent or prior corneal epithelial disease except for mild punctate keratopathy.
Data were collected by the sponsor with all authors having full access to data interpretation, manuscript preparation, revision, and final approval.
Procedures
In the dose escalation cohort, patients received intravenous belamaf at the following doses: 1.92 mg/kg every four weeks (Q4W) (cohort 1); 2.5 mg/kg Q4W (cohort 1a), 2.5 mg/kg Q4W split 50% on days one and eight (cohort 1b), 2.5 mg/kg loading dose cycle 1 day 1 then 1.92 mg/kg Q4W thereafter (cohort 1c), 3.4 mg/kg Q4W split 50% on days one and eight (cohort 2), 2.5 mg/kg Q8W (cohort 3a), 2.5 mg/mg every 12 weeks (Q12W) (cohort 3b). Based on the Part 1 results, patients treated in the Part 2a and 2b dose expansion portion received belamaf 2.5 mg/kg Q8W. For both Part 1 and Part 2 pomalidomide was administered using the standard dose of 4 mg daily for 21 of 28 days with dexamethasone 40 mg (20 mg if >75 years) weekly. Patients were required to undergo ophthalmology assessments prior to each dose of belamaf and use preservative free lubricating eye drops. Treatment was continued until disease progression, prohibitive toxicity, intolerance, or withdrawal of consent. Protocol-defined dose modifications (omissions, delays, reductions) were made independently for each drug as clinically indicated based on the grade of the toxicity.
Assessments
In all patients, clinical assessments, laboratory tests for hematology and biochemistry and disease assessments were done on day 1 of each cycle. Clinical activity was assessed according to the International Myeloma Working Group Uniform Response Criteria for Multiple Myeloma [25]. The National Cancer Institute Common Terminology for Adverse Events (CTCAE version 5.0) were used to grade severity of AEs. Visual acuity was assessed by the Snellen method and corneal epithelial changes were graded by prespecified keratopathy and visual acuity (KVA) scale [26].
Study endpoints/outcomes
The primary endpoints of the trial were to determine the MTD and RP2D of belamaf in combination with Pd in Part 1, as well as the ORR (PR or better) in response evaluable patients treated at the RP2D in Part 1 (cohort 3a) and Part 2 (cohort 2a). Secondary endpoints included determining the PFS, OS, DOR, and safety in the intention to treat population as previously described [24]. In this post-hoc subgroup analysis, we evaluated the ORR, PFS, DOR, OS, and AEs in patients who were TCE (exposed to a PI, lenalidomide, and an anti-CD38 mAb) and/or TCR (refractory to a PI, lenalidomide, and anti-CD38 mAb) defined as disease that is non-responsive to therapy or progression during or within 60 days of drug administration.
Statistical analysis
No formal statistical power calculations were performed to determine the sample sizes for the Part 1 of the trial or for this subgroup analysis. All analyses of outcomes from Part 1 of the study were descriptive, with results reported by dose and schedule, as relevant. For the RP2D cohort a sample size of 35 was obtained to detect a response rate of 0.60 against 0.30 as the historical response rate [2, 3], a one-side binomial proportional test was performed, type I error rate was set at 0.05 and the power was set at 97%. Also, a 10% drop rate was considered. Efficacy counts (rates) were calculated for ORR in the dose escalation and all patients treated at the RP2D that had two consecutive response assessments. Data are summarized by all treated patients, dose group, and RP2D-dosed patients. Median PFS, DOR, and OS (with 95% CI) were analyzed using the Kaplan-Meier method. Number of patients at risk and event-free rates (with 95% CI) at specific months were displayed within the survival curves. SAS 9.4 (SAS Institute Inc.) was used as a statistical tool for all analyses.
Results
Patient disposition and baseline characteristics
Baseline characteristics are presented in Table 1. Between 04 January 2019 and 14 September 2022, 99 patients were enrolled and received at least one dose of belamaf. Of these, 69 patients were identified as TCE or TCR and are the focus of this analysis, of whom 41 were treated at the RP2D. Fifty-six of the 69 (81.2%) were TCR across all cohorts. The median age of this cohort was 67 years (36–85) and 47.8% (33/69) were female. Twenty three percent (16/69) of patients were International Staging System (ISS) Stage III and 22% (15/69) had high risk cytogenetics [del(17p) and/or translocation t(4:14) and/or translocation t(14,16)]. Median number of prior therapies was 3 (range 1–5). In this subgroup analysis, 100% of patients were exposed to lenalidomide, a PI, and anti-CD38 mAb (100% TCE), with 98.6% (68/69) of patients refractory to lenalidomide, 82.6% (57/69) refractory to a PI, and 100% refractory to anti-CD38, resulting in 81.2% (56/69) TCR patients.
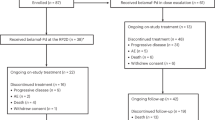
At the data cutoff of 30 June 2023, 56 (57%) of 99 patients enrolled had progressed or died; 31 (45%) of 69 TCE, 14 (34%) of 41 TCE treated at the RP2D and 27 (48%) of 56 patients that were TCR and treated across all cohorts (Fig. 1).
Efficacy
The clinical efficacy data for this subgroup of patients is shown in Table 2 and by dosing cohort for Part 1 patients in Supplementary Table 1. The combination of belamaf-Pd demonstrated deep and durable responses in patients that are TCE/R. The ORR and very good partial response (VGPR) rate or better were 86.4% (57/66) and 63.6% (42/66) for the overall cohort, respectively, and 88.6% (31/35) and 62.8% (22/35) for patients treated across various dose cohorts in Part 1, respectively. Specifically, for all TCE patients, (16/66) 24.2% achieved a complete response (CR) or stringent CR (sCR), 39.4% (26/66) achieved VGPR, and 22.7% (15/66) achieved a confirmed PR. For the 57 responders, the median time to first response of PR or better was 61 days (range, 56–82) with responses being durable with a median DOR of 22·1 months (95% CI, 18.3–not yet reached [NYR]). At a median follow up of 12.2 months (range, 0.9–34.4), the median PFS for the overall TCE group was 19.6 months (95% CI, 17.8–NYR), with median OS of 34.4 months (95% CI, 22.5–NYR) (Table 2). While the estimated median time to next treatment (TTNT) was not reached, 74.2% of patients were still on belantamab treatment without next line of treatment at 24 months (Fig. 2a and Supplementary Fig. 1). For all TCE patients that achieved a CR/sCR, the median PFS was not reached with 71.4% (95% CI, 47.8–100.0%) estimated to be progression free at 2 years (Supplementary Fig. 2).
a PFS, DOR and OS KM curves for all TCE (n = 69) and all TCR (n = 56). b PFS, DOR and OS for RP2D patients (n = 41). CI confidence interval, Est estimated, DOR duration of response, HR hazard ratio, KM Kaplan–Meir, NE not estimable, OS overall survival, PFS progression-free survival, RP2D recommended part 2 dose, TCE triple-class exposed, TCR triple-class refractory.
For TCR patients, refractory to all three classes of anti-myeloma drugs, 84.9% (45/53) achieved confirmed responses including 12 CR or stringent CR, 24 VGPR, and 9 PR. Median DOR was preserved at 22.5 months (95% CI, 18.1–NYR), with median PFS of 19.6 months (95% CI, 15.7–NYR) and median OS of 34.4 months (95% CI, 22.5–NYR) for patients with TCR disease.
For the 41 TCE patients treated at the RP2D the ORR was 84.6% (33/39), ≥VGPR 66.7% (26/39) with a median DOR NYR (95% CI, NYR–NYR). At a median follow up of 12.2 months (range, 1.2–28.3) the median PFS was NYR (95% CI, 18.1–NYR) while the estimate 2-year PFS, DOR and OS were 57.0% (95% CI, 41.1–79.1), 68% (95% CI, 51.0–90.7), and 77.2% (95% CI, 62.3–95.6), respectively (Fig. 2b).
Toxicity
Adverse events reported in >20% of patients in this cohort, serious adverse events (SAEs) and median belamaf dose intensity are presented in Tables 3a, b and 4 respectively, and were similar for TCE and TCR patients. Ninety one percent (63/69) and 95% (39/41) of patients experienced a least one Grade ≥3 AE in the overall cohort and at RP2D, respectively. The most common non hematologic Grade ≥3 AEs were keratopathy (48% in all patients, 46% at RP2D), decreased visual acuity (42% in all patients, 44% at the R2PD) and infection (24.6% in all patients, 19.5% at the RP2D). With respect to Grade ≥3 hematologic toxicity, thrombocytopenia was seen in 27% of the overall cohort and 27% in RP2D patients, with 36% and 34% experiencing neutropenia respectively (Table 3a). Fatal SAEs of Grade ≥3 were experienced by 3% and 2% of patients overall and at the RP2D, respectively. Median dose holds for Grade ≥3 AEs were 5 and 4, respectively (Tables 3b and 4).
Discussion
In this subgroup analysis of belamaf-Pd treated patients on the ALGONQUIN trial, we demonstrate that TCE/TCR patients attain high response rates with durable remissions, with ORRs of 86%/85%, mPFS of 19.6/19.6 months, mDOR 22.1/22.5 months, and mOS of 34.4/34.4 months respectively. Patients treated at the RP2D had an ORR of 85% with median PFS NYR and estimated 24-month PFS rate of 57%. These findings support belamaf-Pd as a highly clinically active therapeutic option in patients who are TCE/TCR.
The majority of patients with RRMM will soon be exposed and/or refractory to PIs, IMIDs, and anti-CD38 mAbs after first- or second-line therapy given the increasing use of triplet [4,5,6] and quadruplet [12,13,14] therapies earlier in the disease course. The MAMMOTH study first reported on the outcomes of patients that are refractory to anti-CD38 mAbs of which 79.1% were TCR. The data were sobering demonstrating an ORR of 31% and mOS of 8.6 months. The results of the MAMMOTH study were validated in the prospective LocoMMotion study that evaluated the outcome of TCE patients treated with widely available, real-life standard of care (SOC) treatments [15]. For patients that were TCE/TCR the ORR was 29.8%/25.1%, mPFS 4.6/3.9 months, and mOS 12.4/11.1 months, respectively. Consistently, in a retrospective cohort study of 199 TCR patients treated with SOC regimens in Canada, the ORR was 40%, the mPFS similarly poor at 4.4 months, and mOS was 10.5 months [16]. These studies not only serve as a benchmark for comparison to new therapies being evaluated in in this setting but also highlight the urgent unmet clinical need of this expanding patient population.
The phase 2 DREAMM-2 trial enrolled RRMM patients who had received 3 or more lines of therapy and were refractory to IMiDs, PIs and an anti-CD38 mAb. For the patients that received single agent belamaf (2.5 mg/kg Q3W) the ORR was 32% (97.5% CI: 21.7–43.6) ref. [27]. Although the mPFS was 2.8 months, for those patients that achieved a PR or better, the responses were durable with a mDOR of 11.0 months (95% CI, 4.2–not reached) and a mOS that was not reached with estimated 1-year survival probability of 87% (95% CI, 69%–95%). Although these results confirmed the single agent activity of belamaf in TCR patients, they suggested a need to improve on the response rates. The results of the ALGONQUIN study demonstrate that adding Pd to belamaf the improvement of ORR to 85% translated to a more clinically meaningful mPFS of 19.6 months in TCR patients.
Certainly, an evolving option for patients who are TCE are the most novel T-cell re-directing therapeutics, chimeric antigen receptor (CAR) T-cell therapies and the bispecific Abs, many of which share a common target with belamaf. The anti-BCMA bispecific Abs, teclistamab and elranatamab, received regulatory approval based on the results of the single-arm phase 2 studies, MajesTEC-1 and MagnestisMM-3, respectively. Patients with a median of 5 prior treatment lines of whom 78% were TCR on the Majestec-1 trial had an ORR of 63% with median PFS of 11.3 months (95% CI, 8.8–17.1) ref. [28]. In a retrospective subgroup analysis, the ORR was preserved in TCR patients. Ninety-seven percent of patients enrolled in the MagnetisMM-3 study were TCR. Patients treated with elranatamab achieved an ORR of 61% and with an estimated 51% of patients remaining in remission at 15 months [29]. In addition, the CD3 redirecting bispecific Abs targeting antigens beyond BMCA are demonstrating clinical activity in RRMM. In the phase 2 MonumenTal-1 trial, patients with ≥3 prior lines including ≥1 PI, ≥1IMiD, and ≥1 anti-CD 38 mAb received Talquetamab, a G protein-coupled receptor, family C, group 5, member D (GPRC5D) bispecific [30]. In this cohort, of whom 84% were TCR, the ORR was 74% with median PFS of 7.5 and 11.9 months for the weekly and Q2W cohorts respectively [30]. Finally, in the first-in-human study of cevostamab, a CD3 T-cell engaging bispecific antibody that targets Fc receptor-homolog 5 (FcRH5), 84.5% of patients were TCR and the ORR was 56.7% in those receiving doses of 132–198 mg Q3W [31]. In context, and with the known limitations of cross-trial comparisons, our study using the anti-BCMA ADC belamaf in combination with Pd in this subgroup analysis of patients who were universally TCE and almost all TCR appears to have comparable if not improved ORR and PFS.
It is important to consider the updated results recently presented from the phase 1b/2 Cartitude-1 trial demonstrating unprecedented results in RRMM. In this study, patients with a median 6 prior lines of treatment, 88% TCR, treated with ciltacabtagene autoleucel (cilta-cel) had an ORR of 98% and mPFS of 34.9 months [32]. The initial results of the randomized Cartitude-4 trial of cilta-cel vs. SOC regimens (PVd or DPd) were also recently presented. In this trial, patients with one to three prior lines of treatment who were lenalidomide refractory also showed high response rates, with an ORR in the intent to treat population of 85% vs. 67% in the standard regimen group, with a 12-month PFS of 76% vs 49%, respectively [33]. Alternatively, results from the randomized KarMMa-3 trial of idecabtagene vicleucel (ide-cel) vs. SOC regimens in patients with two to four prior lines of treatment showed an ORR of 71% and mPFS 13.3 months in the ide-cel group [34], noting however that the percent of TCR patients in Cartitude-4 was much lower at 14.4% compared 65% in the KarMMa-3. Despite the exciting cilta-cel data, we currently face several issues limiting access to Car-T therapy in most jurisdictions, due to challenges with product access (manufacturing capacity, distribution, reimbursement), as well as patient factors such as rapid disease progression, access to effective bridging, financial toxicity, and fitness. As such, many patients and providers will need to consider alternative anti-BCMA treatments for most TCE/TCR patients in the immediate future, until Car-T is more accessible to the global RRMM population.
With access becoming more widely available to anti-BCMA approaches and with studies evaluating these agents in earlier lines of therapy, the age-old question of treatment sequencing in myeloma remains relevant. Data is emerging on the effectiveness of BCMA targeted agents in patients previously exposed to an alternate BCMA directed therapy. This evolving literature, as well as further work on mechanisms of response and resistance, will be paramount as we aim to select optimal treatments for individual patients. Recently presented data are reassuring, suggesting that prior exposure to BMCA targeted ADCs such as belamaf does not preclude responses to other BMCA targeting agents. For example, in the cohort C (n = 40) of the MajesTEC-1 study 72.5% of patients were ADC exposed and received teclistamab. The ORR for patients previously treated with a BMCA targeting ADC was 52.5% ref. [35]. Furthermore, a pooled analysis of patients with prior anti-BCMA directed therapy (n = 87) treated with elranatamab on MagnetisMM studies revealed an ORR and mDOR for patients with prior BMCA-targeting ADC of 42.4% and 13.6 months, respectively [36]. Twenty-four patients treated in cohort C of the Cartitude-1 trial (n = 20) had prior anti-BCMA treatment, with ORR of 61% for those with prior ADC (n = 13) and a mPFS of 12.3 months [37], demonstrating in principle that patients treated with anti-BCMA ADCs can respond to anti-BCMA Car-T treatment. Finally, data on sequencing of belamaf after BMCA directed therapies are more limited but in a real-world study, 19 patients received anti-BMCA Car-T (n = 12), bispecific Ab (n = 6) or treatment with belamaf. Response to belamaf was similar in those with prior BMCA exposure compared to BMCA-naïve patients with a mPFS of 4 months reported in both groups [38]. Ongoing trials of the growing BCMA arsenal and their analyses in these patient subgroups will be imperative to optimizing the use of BMCA containing regimens such as belamaf-Pd in the treatment algorithm for individual patients.
The safety profile was similar for TCE patients compared to the intent to treat population (Supplementary Table 2). This includes the risk of serious infections that has emerged as a significant challenge with T-cell re-directing therapies. Indeed, the relative low rate of Grade ≥3 infections (24.6%) is consistent with what is reported in the DREAMM3 study [39] and further supports the notion that belamaf poses less infection risk. Nevertheless, it is important to discuss that ocular toxicity remains the main clinical challenge with belamaf administration, with no additional safety signals found in this analysis. In this subgroup, Grade ≥ 3 ocular AEs were keratopathy (48% in all patients, 46% at RP2D) and decreased visual acuity (42% in all patients, 44% at the R2PD). Longer dosing intervals did not compromise efficacy in our study, similar to the findings with the use of belamaf given every 12 weeks in combination with lenalidomide and dexamethasone resulting in 11–13% Grade 3 visual acuity changes [40]. To evaluate if ocular toxicity can be further improved, we have added an additional cohort to part 2 of this trial where by patients will receive belamaf 1.92 mg/m2 every 8 weeks with standard Pd, based on emerging data from the DREAMM-9 trial that this dose resulted in reduced toxicity with preserved response rates [41]. We have also embarked on an optional ocular sub-study using bandage contact lenses to attempt to reduce corneal toxicity, with results to be reported at a later date. While optimization efforts continue, routine eye examinations remain a requirement for patients being treated with belamaf, and clinicians must be informed on symptom management and dose-modification. However, there are divergent challenges with alternative novel agents in this patient population, including infection (61.8–76%) and CRS (50.6–72%) with the anti-BCMA bispecifics [28, 29], CRS/ICANS (84–92%/17–18%) with Car-T therapy [20, 32], and dysgeusia (37–65%), skin (24–67%) and nail changes (20–57%) with talquetamab [42], supporting the need for individualized treatment based on patient and disease characteristics and patient choice.
While our results are encouraging, we recognize there are several limitations to our study, including the short follow up time and small number of patients. In addition, the results of our phase 1–2 trial need to be confirmed in a large phase 3 trial with an appropriate comparator, such as the DREAMM-8 trial which compares belamaf-Pd to PVd and is expected to read out soon [43].
In summary, patients with TCE/TCR disease treated with belamaf-Pd on the ALGONQUIN trial experienced clinical benefits that are markedly superior to those reported with real-life SOC therapies and competitive with other BCMA agents including the bispecifics and ide-cel. These data support the use of belamaf-Pd as a highly effective therapy to address the unmet need of particularly challenging RRMM patient population.
Data availability
The data generated for this study is available upon reasonable request from the corresponding author.
References
Mian H, Reece D, Masih-Khan E, McCurdy A, Kardjadj M, Jimenez-Zepeda VH, et al. Survival and Outcomes of Newly Diagnosed Multiple Myeloma Patients Stratified by Transplant Status 2007–2018: Retrospective Analysis from the Canadian Myeloma Research Group Database. Clin Lymphoma Myeloma Leuk. 2022;22:608–17.
Puertas B, González-Calle V, Sobejano-Fuertes E, Escalante F, Queizán JA, Bárez A, et al. Novel Agents as Main Drivers for Continued Improvement in Survival in Multiple Myeloma. Cancers. 2023;15:1558.
McCurdy A, Seow H, Pond GP, Gayowsky A, Chakraborty R, Visram A, et al. Cancer-specific mortality in multiple myeloma: a population-based retrospective cohort study. Haematologica. 2023;108:3384–91.
Richardson PG, Jacobus SJ, Weller EA, Hassoun H, Lonial S, Raje NS, et al. Triplet Therapy, Transplantation, and Maintenance until Progression in Myeloma. N Engl J Med. 2022;387:132–47.
Moreau P, Hulin C, Macro M, Caillot D, Chaleteix C, Roussel M, et al. VTD is superior to VCD prior to intensive therapy in multiple myeloma: results of the prospective IFM2013-04 trial. Blood. 2016;127:2569–74.
Facon T, Kumar SK, Plesner T, Orlowski RZ, Moreau P, Bahlis N, et al. Daratumumab, lenalidomide, and dexamethasone versus lenalidomide and dexamethasone alone in newly diagnosed multiple myeloma (MAIA): overall survival results from a randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22:1582–96.
Dimopoulos MA, Oriol A, Nahi H, San-Miguel J, Bahlis NJ, Usmani SZ, et al. Overall Survival With Daratumumab, Lenalidomide, and Dexamethasone in Previously Treated Multiple Myeloma (POLLUX): A Randomized, Open-Label, Phase III Trial. J Clin Oncol. 2023;41:1590–9.
Sonneveld P, Chanan-Khan A, Weisel K, Nooka AK, Masszi T, Beksac M, et al. Overall Survival With Daratumumab, Bortezomib, and Dexamethasone in Previously Treated Multiple Myeloma (CASTOR): A Randomized, Open-Label, Phase III Trial. J Clin Oncol. 2023;41:1600–9.
Usmani SZ, Quach H, Mateos MV, Landgren O, Leleu X, Siegel D, et al. Final analysis of carfilzomib, dexamethasone, and daratumumab vs carfilzomib and dexamethasone in the CANDOR study. Blood Adv. 2023;7:3739–48.
Richardson PG, Perrot A, San-Miguel J, Beksac M, Spicka I, Leleu X, et al. Isatuximab plus pomalidomide and low-dose dexamethasone versus pomalidomide and low-dose dexamethasone in patients with relapsed and refractory multiple myeloma (ICARIA-MM): follow-up analysis of a randomised, phase 3 study. Lancet Oncol. 2022;23:416–27.
Richardson PG, Kumar SK, Masszi T, Grzasko N, Bahlis NJ, Hansson M, et al. Final Overall Survival Analysis of the TOURMALINE-MM1 Phase III Trial of Ixazomib, Lenalidomide, and Dexamethasone in Patients With Relapsed or Refractory Multiple Myeloma. J Clin Oncol. 2021;39:2430–42.
Voorhees PM, Sborov DW, Laubach J, Kaufman JL, Reeves B, Rodriguez C, et al. Addition of daratumumab to lenalidomide, bortezomib, and dexamethasone for transplantation-eligible patients with newly diagnosed multiple myeloma (GRIFFIN): final analysis of an open-label, randomised, phase 2 trial. Lancet Haematol. 2023;10:e825–37.
Moreau P, Hulin C, Perrot A, Arnulf B, Belhadj K, Benboubker L, et al. Maintenance with daratumumab or observation following treatment with bortezomib, thalidomide, and dexamethasone with or without daratumumab and autologous stem-cell transplant in patients with newly diagnosed multiple myeloma (CASSIOPEIA): an open-label, randomised, phase 3 trial. Lancet Oncol. 2021;22:1378–90.
Goldschmidt H, Mai EK, Bertsch U, Fenk R, Nievergall E, Tichy D, et al. Addition of isatuximab to lenalidomide, bortezomib, and dexamethasone as induction therapy for newly diagnosed, transplantation-eligible patients with multiple myeloma (GMMG-HD7): part 1 of an open-label, multicentre, randomised, active-controlled, phase 3 trial. Lancet Haematol. 2022;9:e810–21.
Mateos MV, Weisel K, De Stefano V, Goldschmidt H, Delforge M, Mohty M, et al. LocoMMotion: a prospective, non-interventional, multinational study of real-life current standards of care in patients with relapsed and/or refractory multiple myeloma. Leukemia. 2022;36:1371–6.
Visram A, De La Torre A, White D, Kardjadj M, Masih-Khan E, Chu MP, et al. Real World Data on Outcomes of Anti-CD38 Antibody Refractory, Including Triple Class Refractory, Patients with Multiple Myeloma: A Multi-Institutional Report from the Canadian Myeloma Research Group (CMRG) Database. Blood. 2022;140:4287–9.
Tai YT, Mayes PA, Acharya C, Zhong MY, Cea M, Cagnetta A, et al. Novel anti-B-cell maturation antigen antibody-drug conjugate (GSK2857916) selectively induces killing of multiple myeloma. Blood. 2014;123:3128–38.
Pillarisetti K, Powers G, Luistro L, Babich A, Baldwin E, Li Y, et al. Teclistamab is an active T cell-redirecting bispecific antibody against B-cell maturation antigen for multiple myeloma. Blood Adv. 2020;4:4538–49.
Shah N, Chari A, Scott E, Mezzi K, Usmani SZ. B-cell maturation antigen (BCMA) in multiple myeloma: rationale for targeting and current therapeutic approaches. Leukemia. 2020;34:985–1005.
Munshi NC, Anderson LD Jr, Shah N, Madduri D, Berdeja J, Lonial S, et al. Idecabtagene Vicleucel in Relapsed and Refractory Multiple Myeloma. N Engl J Med. 2021;384:705–16.
Berdeja JG, Madduri D, Usmani SZ, Jakubowiak A, Agha M, Cohen AD, et al. Ciltacabtagene autoleucel, a B-cell maturation antigen-directed chimeric antigen receptor T-cell therapy in patients with relapsed or refractory multiple myeloma (CARTITUDE-1): a phase 1b/2 open-label study. Lancet. 2021;398:314–24.
Trudel S, Lendvai N, Popat R, Voorhees PM, Reeves B, Libby EN, et al. Targeting B-cell maturation antigen with GSK2857916 antibody-drug conjugate in relapsed or refractory multiple myeloma (BMA117159): a dose escalation and expansion phase 1 trial. Lancet Oncol. 2018;19:1641–53.
Trudel S, Lendvai N, Popat R, Voorhees PM, Reeves B, Libby EN, et al. Antibody-drug conjugate, GSK2857916, in relapsed/refractory multiple myeloma: an update on safety and efficacy from dose expansion phase I study. Blood Cancer J. 2019;9:37.
Trudel S, McCurdy A, Louzada ML, Parkin S, White D, Chu MP, et al. Belantamab mafodotin, pomalidomide, and dexamethasone in refractory multiple myeloma: a phase 1/2 trial. Nat Med. 2023;30:543–51.
Kumar S, Paiva B, Anderson KC, Durie B, Landgren O, Moreau P, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 2016;17:e328–46.
Farooq AV, Degli Esposti S, Popat R, Thulasi P, Lonial S, Nooka AK, et al. Corneal Epithelial Findings in Patients with Multiple Myeloma Treated with Antibody-Drug Conjugate Belantamab Mafodotin in the Pivotal, Randomized, DREAMM-2 Study. Ophthalmol Ther. 2020;9:889–911.
Lonial S, Lee HC, Badros A, Trudel S, Nooka AK, Chari A, et al. Belantamab mafodotin for relapsed or refractory multiple myeloma (DREAMM-2): a two-arm, randomised, open-label, phase 2 study. Lancet Oncol. 2020;21:207–21.
Moreau P, Garfall AL, van de Donk N, Nahi H, San-Miguel JF, Oriol A, et al. Teclistamab in Relapsed or Refractory Multiple Myeloma. N. Engl J Med. 2022;387:495–505.
Lesokhin AM, Tomasson MH, Arnulf B, Bahlis NJ, Miles Prince H, Niesvizky R, et al. Elranatamab in relapsed or refractory multiple myeloma: phase 2 MagnetisMM-3 trial results. Nat Med. 2023;29:2259–67.
Schinke CD, Touzeau C, Minnema MC, van de Donk N, Rodríguez-Otero P, Mateos MV, et al. Pivotal phase 2 MonumenTAL-1 results of talquetamab (tal), a GPRC5DxCD3 bispecific antibody (BsAb), for relapsed/refractory multiple myeloma (RRMM). J Clin Oncol. 2023;41:8036.
Trudel S, Cohen AD, Krishnan AY, Fonseca R, Spencer A, Berdeja JG, et al. Cevostamab Monotherapy Continues to Show Clinically Meaningful Activity and Manageable Safety in Patients with Heavily Pre-Treated Relapsed/Refractory Multiple Myeloma (RRMM): Updated Results from an Ongoing Phase I Study. Blood. 2021;138:157–60.
Lin Y, Martin TG, Usmani SZ, Berdeja JG, Jakubowiak AJ, Agha ME, et al. CARTITUDE-1 final results: Phase 1b/2 study of ciltacabtagene autoleucel in heavily pretreated patients with relapsed/refractory multiple myeloma. J Clin Oncol. 2023;41:8009.
Dhakal B, Yong K, Harrison SJ, Mateos MV, Moreau P, van de Donk N, et al. First phase 3 results from CARTITUDE-4: Cilta-cel versus standard of care (PVd or DPd) in lenalidomide-refractory multiple myeloma. J Clin Oncol. 2023;41:LBA106–LBA.
Rodriguez-Otero P, Ailawadhi S, Arnulf B, Patel K, Cavo M, Nooka AK, et al. Ide-cel or Standard Regimens in Relapsed and Refractory Multiple Myeloma. N Engl J Med. 2023;388:1002–14.
Touzeau C, Krishnan AY, Moreau P, Perrot A, Usmani SZ, Manier S, et al. Efficacy and safety of teclistamab (tec), a B-cell maturation antigen (BCMA) x CD3 bispecific antibody, in patients (pts) with relapsed/refractory multiple myeloma (RRMM) after exposure to other BCMA-targeted agents. J Clin Oncol. 2022;40:8013.
Nooka AK, Lesokhin AM, Mohty M, Niesvisky R, Maisel C, Arnulf B, et al. Efficacy and safety of elranatamab in patients with relapsed/refractory multiple myeloma (RRMM) and prior B-cell maturation antigen (BCMA)-directed therapies: A pooled analysis from MagnetisMM studies. J Clin Oncol. 2023;41:8008.
Cohen AD, Mateos M-V, Cohen YC, Rodriguez-Otero P, Paiva B, van de Donk N, et al. Efficacy and safety of cilta-cel in patients with progressive multiple myeloma after exposure to other BCMA-targeting agents. Blood. 2023;141:219–30.
Hultcrantz M, Kleinman D, Vij R, Escalante F, Kotoswky N, Bitetti J, et al. Belantamab Mafodotin (Belamaf) for Relapsed/Refractory Multiple Myeloma (RRMM): A Real-World Observational Study. Blood. 2022;140:10124–6.
Dimopoulos MA, Hungria VT, Radinoff A, Delimpasi S, Mikala G, Masszi T, et al. Efficacy and safety of single-agent belantamab mafodotin versus pomalidomide plus low-dose dexamethasone in patients with relapsed or refractory multiple myeloma (DREAMM-3): a phase 3, open-label, randomised study. Lancet Haematol. 2023;10:e801–e12.
Terpos E, Gavriatopoulou M, Ntanasis-Stathopoulos I, Malandrakis P, Fotiou D, Migkou M, et al. Safety and clinical activity of belantamab mafodotin plus lenalidomide and dexamethasone in transplant ineligible patients with newly diagnosed multiple myeloma: The phase 1/2, prospective, open-label, BelaRd study. J Clin Oncol. 2023;41:8050.
Usmani SZ, Alonso Alonso A, Quach H, Koh Y, Guenther A, Min C-K, et al. DREAMM-9: Phase I Study of Belantamab Mafodotin Plus Standard of Care in Patients with Transplant-Ineligible Newly Diagnosed Multiple Myeloma. Blood. 2021;138:2738.
Chari A, Minnema MC, Berdeja JG, Oriol A, van de Donk N, Rodriguez-Otero P, et al. Talquetamab, a T-Cell–Redirecting GPRC5D Bispecific Antibody for Multiple Myeloma. N Engl J Med. 2022;387:2232–44.
Trudel S, Davis R, Lewis NM, Bakshi KK, Chopra B, Montes de Oca R, et al. DREAMM-8: A Phase III Study of the Efficacy and Safety of Belantamab Mafodotin with Pomalidomide and Dexamethasone (B-Pd) Vs Pomalidomide Plus Bortezomib and Dexamethasone (PVd) in Patients with Relapsed/Refractory Multiple Myeloma (RRMM). Blood. 2020;136:4.
Acknowledgements
ST is supported by grants from the Canadian Institute for Health Research (grant number 175267). Medical editorial support was provided by Lama Yamani (Veristat, LLC) and funded by the CMRG. The authors thank the patients who participated in this study as well as their caregivers, families, the members and the following individuals from GSK: Dr Antonio Palumbo (data interpretation and manuscript review) and Anna Lowry (clinical trial management).
Funding
This study was sponsored by the Canadian Myeloma Research Group (CMRG) with support from Glaxo-Smith-Kline.
Author information
Authors and Affiliations
Contributions
All authors participated in study design and conduct; data acquisition, analysis, and interpretation; drafting and revising the article; and approved the final version before submission. JS performed statistical analyses. ST, AM, AK, and DR verified the underlying data. All authors had access to the study data and had final responsibility for the decision to submit the article for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare the following competing interests: AM received honoraria from Celgene, Janssen, Amgen, Takeda, Sanofi, and GSK. DR received research funding and honoraria from, and is on the advisory board of, Janssen, BMS, and Takeda; received research funding from Millennium Pharmaceuticals; and received honoraria from Amgen, Sanofi, and GSK. ML received research support from BMS/Celgene and Janssen; and honoraria from BMS/Celgene, Janssen, Gilead, AbbVie, AstraZeneca, and Takeda. SP received consultancy honoraria from Janssen, BMS, FORUS, and Apotex; study funding from GSK; and funding from BMS. DW received honoraria from Amgen, Antengene, BMS, FORUS Therapeutics, GSK, Janssen, Karyopharm, Pfizer, Sanofi, and Takeda. MC received research support from BMS/Celgene and Janssen; and honoraria from BMS/Celgene, Janssen, Gilead, AbbVie, AstraZeneca, and Takeda. RK received honoraria from Akcea Therapeutics, Amgen, BMS, Janssen, Merck, Sanofi, Celgene, Pfizer, and Takeda; received research funding from Merck and Sanofi; and is a current equity holder in the private company Karyopharm. HM received advisory fees from Janssen, Takeda, Amgen, Pfizer, BMS, FORUS, and Sanofi; received research funding from Janssen; and is supported by the early career award from Hamilton Health Sciences. IO participated in advisory boards for and received honoraria from Amgen, BMS, Celgene, FORUS Therapeutics, Janssen, Pfizer, Sanofi-Genzyme, and Takeda; and received research funding from Janssen. JS, AK, and EG are employees of CMRG. ST received grant support from GSK, Bristol Myers Squibb (BMS), Janssen, Pfizer, Amgen, Roche, and Genentech; consulting fees from BMS, GSK, and Roche; and honoraria from BMS, Janssen, Amgen, Sanofi, and Pfizer.
Ethics approval and consent to participate
The trial was conducted in accordance with the Declaration of Helsinki, International Council Harmonization Good Clinical Practice Guidelines, local regulation governing the conduct of clinical studies and institutional guidelines. Approval to conduct the trial was provided by Ontario Cancer Research Ethics Board (OCREB; IRB00003960); project ID 1598. Informed consent was obtained from all patients.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
McCurdy, A., Reece, D., Louzada, M.L. et al. Belantamab mafodotin, pomalidomide, and dexamethasone for triple class exposed/refractory relapsed multiple myeloma: a subgroup analysis of the ALGONQUIN trial. Blood Cancer J. 14, 155 (2024). https://doi.org/10.1038/s41408-024-01135-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41408-024-01135-2
- Springer Nature Limited