Abstract
Mental disorders represent an increasing source of disability and high costs for societies globally. Molecular imaging techniques such as positron emission tomography (PET) represent powerful tools with the potential to advance knowledge regarding disease mechanisms, allowing the development of new treatment approaches. Thus far, most PET research on pathophysiology in psychiatric disorders has focused on the monoaminergic neurotransmission systems, and although a series of discoveries have been made, the results have not led to any material changes in clinical practice. We outline areas of methodological development that can address some of the important obstacles to fruitful progress. First, we point towards new radioligands and targets that can lead to the identification of processes upstream, or parallel to disturbances in monoaminergic systems. Second, we describe the development of new methods of PET data quantification and PET systems that may facilitate research in psychiatric populations. Third, we review the application of multimodal imaging that can link molecular imaging data to other aspects of brain function, thus deepening our understanding of disease processes. Fourth, we highlight the need to develop imaging study protocols to include longitudinal and interventional paradigms, as well as frameworks to assess dimensional symptoms such that the field can move beyond cross-sectional studies within current diagnostic boundaries. Particular effort should be paid to include also the most severely ill patients. Finally, we discuss the importance of harmonizing data collection and promoting data sharing to reach the desired sample sizes needed to fully capture the phenotype of psychiatric conditions.
Similar content being viewed by others
Background
In a given year, one out of six individuals in Europe will suffer from a mental health problem, and it is estimated that the total cost to European societies for these disorders is 600 billion euros [1]. Recovery rates for schizophrenia have not improved for several decades [2], and similarly the global disease burden of depressive and anxiety disorders, both ranked among the top 25 leading causes of burden, has not diminished since 1990 [3]. Importantly, the identification of new treatment approaches that could improve this situation is hampered by a lack of understanding of the pathophysiology of mental disorders. Molecular imaging methods such as positron emission tomography (PET) offer a unique opportunity to measure brain biochemical markers in vivo, and have since their advent in the 1980:s been considered a key approach to advance the field.
Psychiatry was indeed an early focus in the field of quantitative PET, with the very first clinical studies being conducted in patients with schizophrenia. Demonstrations of the antipsychotic mechanism of action using dopamine D2 receptor (D2-R) radioligands such as [11C]raclopride was followed by a series of occupancy studies outlining thresholds for treatment efficacy and side effects [4, 5]. Arguably, the resulting change in dosing regimens remains the most significant contribution of PET research to clinical psychiatry to date. Since then, a wealth of studies have attempted to investigate the pathophysiology of psychiatric disorders, mainly based on disease models involving monoamine neurotransmission systems. To name a few examples, studies of dopaminergic function in psychosis and schizophrenia have collectively shown increased dopamine synthesis and release capacity as indexed by increased [18F]DOPA uptake and more pronounced amphetamine-induced decreases in D2-R receptor binding, a small increase in striatal D2-R availability and lower D2-R availability in the thalamus [6, 7]. In major depressive disorder (MDD), findings point to reduced serotonin transporter [8] and serotonin 1A receptor (5HT1A-R) availability [9], whereas in patients with anxiety disorders the evidence suggests decreases in 5HT1A and benzodiazepine receptors [10]. Several new radioligands for monoaminergic neurotransmission targets have been developed in recent years, such as tracers with increased sensitivity for endogenous neurotransmitter levels [11,12,13,14], that may further advance our understanding of the involvement of these systems. However, thus far this line of research has not led to new diagnostic tools or treatments for clinical use, prompting research based on new models of disease pathophysiology.
In order to advance PET research to the point of improving the care of psychiatric patients, some important challenges remain. First, there is a need to identify disease-related processes that act upstream or parallel to the observed abnormalities in monoaminergic dysfunction. To accomplish this, radioligands for new targets need to be developed, and a wider methodological scope is required to outline molecular pathways from genetics and environmental factors to the dysfunctional information processing that underlies psychiatric symptoms. Second, psychiatric populations are characterized by considerable heterogeneity in clinical phenotype—likely corresponding to heterogeneity in pathophysiological mechanisms. It is generally acknowledged that current diagnostic boundaries are ill-matched to the underlying biology, presenting a critical challenge to advancing knowledge [15]. Third, psychiatric patients are a vulnerable group, calling for the simplification of clinical research protocols. The most severely ill patients are typically not included in research studies at all, owing to difficulties in adhering to cumbersome study procedures or not being able to provide informed consent, limiting our understanding of the full phenotype associated with mental disorders.
In this review, we aim to describe recent advancements in methodological development in PET that may address these challenges, and to what extent they have been applied in clinical psychiatric research.
New targets and radioligands
A key bottleneck in clinical PET research in general is the availability of radioligands for targets of interest. In the following, we highlight areas of development with specific relevance to psychiatric disorders.
Intracellular targets
One approach to go beyond the level of neurotransmission signalling is to target intracellular enzymes in neurons [16,17,18,19]. This approach allows for investigating the activation state of groups of neurons during a certain condition, and may also elucidate if a dysfunction of that specific intracellular mechanism is part of the underlying pathophysiology of specific disorders [20]. Examples of this strategy are studies of the cyclic nucleotide phosphodiesterase (PDE) family of enzymes, which metabolize cyclic nucleotides and thereby regulate the signalling of these second messenger systems. PDE10A has been of recent interest in schizophrenia research [17,18]. In the brain, PDE10A is highly localized to the striatum, where it regulates the output of the direct and indirect striatal pathways that are implicated in several psychiatric conditions. PDE10A radioligands have thus far only been used in small samples of schizophrenia patients, showing inconclusive results [17,18].
Another enzyme in the PDE family, PDE4, is the main enzyme in the brain responsible for metabolizing 3′,5′-monophosphate (cAMP) into its inactive state. The cAMP signalling pathway is a major second messenger pathway of G-coupled receptors, involved in a range of intracellular processes including propagating neuron-neuron signals, and is hence of high relevance for many psychiatric conditions. The radioligand [11C]rolipram, a nonselective PDE4 antagonist, was used to show reduced cAMP activity in MDD compared to controls, and an upregulation after selective serotonin reuptake inhibitor (SSRI) treatment [19]. Indeed, PDE4 inhibitors have been suggested as a treatment in psychiatric conditions based on positive effects on neuroplasticity and neuroinflammation, but adverse effects hamper their implementation [21]. More selective targeting of PDE4 subtypes (i.e. PDE4 A/B/C/D) and increased understanding of the regulation of conformational states may be keys to overcome the adverse effects. In this respect, recent efforts have been made to develop radioligands with higher specificity for certain PDE4 subtypes [22], but these have yet to be applied in MDD or other psychiatric conditions.
Immune markers
Genetic and epidemiologic data support a role for the immune system in psychotic disorders, depression and anxiety disorders as well as neurodevelopmental disorders. During the last decade, intensive efforts have aimed to identify PET markers for dysregulated immune function which for instance could be used to stratify patients for treatments targeting the immune system. To date, the most established method is to target the 18kD translocator protein (TSPO), which is expressed in activated microglia and astrocytes. Whereas initial studies in schizophrenia using the first generation TSPO radioligand [11C]PK-11195 showed increased binding in patients, this could not be confirmed in ensuing studies using TSPO radioligands with increased sensitivity such as [11C]PBR28 and [18F]FEPPA. Instead, data has converged towards lower binding across several brain regions [23, 24]. In contrast, six out of seven TSPO studies in MDD have shown increased binding compared with controls [24].
TSPO is not specific to microglia [25, 26], and in vitro studies have shown conflicting results regarding the specificity of TSPO for pro-inflammatory cells [27, 28]. There are currently several radioligands under investigation to find more specific markers for neuroinflammatory processes. Radioligands such as [11C]deprenyl and [¹¹C]SL25.1188, targeting the enzyme MAO-B, have been considered markers of astroglial activation. The latter radioligand has been used to show increased binding in the prefrontal cortex in patients with MDD [29], whereas a small study found no difference in binding in post-traumatic stress disorder (PTSD) patients [30]. With regard to microglial and proinflammatory markers, some promising candidates have been developed for Cox-1 and Cox-2, CSF1R and P2X7 [24], but to our knowledge, none of these have so farbeen used to study psychiatric disorders.
Synaptic density
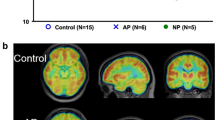
A wealth of literature supports aberrant connectivity in several psychiatric conditions, as indicated indirectly using functional magnetic resonance imaging (MRI) modalities and post-mortem studies. In order to investigate connectivity at the molecular level, there has been an increasing interest in identifying targets for synaptic density. The PET radioligand [11C]UCB-J binds to the synaptic vesicle glycoprotein 2A (SV2A), which has shown high correspondence to the established post-mortem marker synaptophysin in non-human primate studies [31]. [11C]UCB-J has been applied in patients with MDD and/or PTSD, showing an inverse correlation between depressive symptoms and SV2A density, as well as an association between SV2A density and functional connectivity in prefrontal cortex as measured using resting-state functional MR (fMRI) [32]. The radioligand has been used in medicated patients with chronic schizophrenia, showing decreases in SV2A binding across several cortical regions [33, 34]. Recently, a small study found decreased SV2A binding in the hippocampus in users of cannabis [35], a drug considered to be a major risk factor for schizophrenia [36]. An important aim following the observations in MDD and schizophrenia is to investigate if changes in synaptic density are present already in the early stages of psychiatric disorders (Fig. 1).
Future developments
PET neuroreceptor ligands are generally based on small, lipophilic molecules that can easily cross the blood-brain barrier (BBB). In oncological PET, the use of labelled antibodies with high specificity and affinity has long been of interest. To enable brain uptake sufficient for imaging, recent developments have shown the possibility of designing bi-specific antibodies that undergo active transport across the BBB by transferrin-receptor-mediated transcytosis visualizing, e.g., amyloid-beta [37]. Although these methods have only been demonstrated in small-animal studies at this point [38] and have been developed primarily for application in neurodegenerative disorders, there could be potential applications in psychiatry given the interest in immune-related disease mechanisms. A limitation with labelled antibodies is their slow clearance from the blood which may require long-lived isotopes such as 79Zr for labelling, resulting in high radiation doses. A novel approach to overcome this is so-called pre-targeting using bioorthogonal chemistry, i.e., administration of an intermediate compound such as an antibody that binds to the target of interest, which can in turn be targeted by small molecules labelled with short-lived PET isotopes after the circulating antibody has cleared [39]. Hence, the antibody is labelled after it has bound to its target in the body and cleared from the blood, improving image contrast and reducing radiation dose compared to direct imaging of labelled antibodies. A challenge with this approach that will need to be solved is how to measure target availability, as the PET signal will be dependent on the kinetics of both the antibody and the tracer. If applied to psychiatry, his approach could potentially also be used to increase the ecological validity of studies in conditions with a fluctuating course, i.e., by administering the pre-targeting compound immediately when patients are experiencing symptoms, allowing for PET scanning to be done at a later time.
Radioligand validation and availability
When exploring new radioligands for use in psychiatry, it should be kept in mind that PET tracers are typically designed to fulfil a set of specific imaging properties [40]. The development involves validating the specificity of the tracer for its target using blocking or displacement studies, identifying the optimal method for quantitative analysis by studies on tracer kinetic analysis, and establishing the precision of binding measures using test-retest studies. However, the fact that a tracer has been validated for one application does not necessarily mean that it can be utilized for other applications. For instance, a utility of the medium affinity D2-R radioligand [11C]raclopride, which has primarily been used to investigate high-density striatal regions, has been suggested also for measurements in low-density cortical brain regions based on test-retest reliability studies and between-sample comparisons. Importantly, competition studies and within-subject comparisons to high-affinity radioligands showed low validity for this approach [41, 42]. Similarly, high image quality and accurate quantification of binding potential during the time typically deemed practical for dynamic PET scans require preferably a high extraction, a relatively short time to (transient) equilibrium, and fast clearance of the tracer. These characteristics may not be optimal for steady-state PET/fMRI protocols aiming to quantify neurotransmitter release with the high temporal resolution, where both a fast association and dissociation from the target as well as a fast clearance of non-bound tracer from the brain are ideally required.
Another general challenge associated with the use of PET in clinical research is the availability and hence cost of PET tracers. Few centres around the world are able to produce 11C-labelled ligands, and these cannot be distributed to other hospitals because of the 20-min radioactive half-life. Moreover, production usually results in amounts of radioactivity that are sufficient for only one scanning time. The development of 18F-labelled ligands, that allow for scanning of a larger number of subjects for each production run as well as for transportation of tracers to other hospitals, could facilitate the more widespread and routine use of PET in clinical research. For instance, 18F-labelled analogues of UCB-J, such as [18F]SynVesT-1, have recently been developed for SV2A [43, 44]. It should be noted, however, that the longer half-life 18F-labelled radioligands render them unsuitable for multiple examinations during the same day, e.g., before and after an intervention, due to carry-over effects.
PET data quantification
Besides identifying new radioligands and targets, optimizing methods for data quantification and harmonizing across centres are other areas that could accelerate the development of clinical PET research in psychiatry, as well as in other fields. For radioligands where there is no true region devoid of target, a metabolite-corrected arterial input function is required for quantification of radioligand binding, imposing limitations on clinical research in particular for vulnerable patient groups. In attempts to increase the clinical utility of TSPO PET, the use of a pseudoreference region (i.e., a region containing specific binding, hence not fulfilling the criteria for a true reference region) has been applied in several studies, however, the reliability and validity of this approach has shown to be low in healthy subjects [45, 46]. Although pseudoreference regions may prove to be useful in certain neurological conditions where the pathology can be assumed to be more restricted [47, 48], their use is more questionable in psychiatric populations where changes in immune function are expected to be subtle and diffuse. For SV2A PET a white-matter reference region has been proposed [49], and even more simplified approaches have also been evaluated [50] but competition studies showing specific binding indicate that reference tissue approaches may introduce a bias in binding estimates [51]. To ease the experimental burden, image-based input function is one area under investigation [52, 53] but the poor resolution of current PET systems, as well as head movement artefacts, limit their utility. Importantly, even if the accurate estimation of image-based input functions is achieved, apart from a few exceptions (notably [18F]FDG and [15O]water) most tracers undergo peripheral metabolism and arterial sampling for metabolite analysis will therefore still be required to assess the amount of intact tracer in blood. The possibility of using venous instead of arterial samples for metabolite analysis would result in a less invasive procedure. Although metabolite analysis based on venous sampling has been published for several tracers, direct comparison to arterial sampling has only been done in few studies with varying results [54, 55].
When full quantification using an input function is performed, the typical outcome (total distribution volume) is the sum of specific binding and non-specific and free radioligand (=non-displaceable binding). For tracers requiring this method, novel approaches to separate specific from non-displaceable binding could potentially increase sensitivity, leading to increased power in clinical studies [56, 57]. Importantly, non-displaceable binding has also shown to be a potential confounder in clinical populations, including alcohol use disorder [58]. Finally, simultaneous multifactor estimation of binding parameters using Bayesian analysis has in initial evaluations shown promise for further reducing measurement error, although the computational cost needs to be addressed for sufficient generalizability [59]. Ideally, the development of methods for quantification should be performed using open source code, to increase transparency and harmonization [60].
PET systems
To further enhance the utility of PET in clinical studies, there is a need for new PET systems with increased sensitivity to allow for both more precise measures, increasing statistical power, and repeated measurements by means of reduced radioactive doses.
The current state of the art for brain-PET imaging, the High-resolution research tomograph (HRRT, Siemens) was designed in the early 2000s [61]. Its spatial resolution, although high, is limited by its sensitivity, i.e., the spatial resolution that can theoretically be achieved based on detector size cannot be realized in practice because of limited counts. Recent years have seen a steady increase in the axial field of view (FOV) of PET/CT systems, from a standard axial length of 15 cm about 10 years ago, to 25 or even 30 cm as standard options from most vendors [62, 63]. Since the sensitivity of PET systems is proportional to the square of their axial FOV, a factor two increase in axial FOV leads to a fourfold increase in sensitivity. More recently, total-body PET scanners have been launched, such as the uEXPLORER (United Imaging) covering the entire body with an axial FOV of 194 cm [64], or the Quadra (Siemens) head-to-thigh with an axial FOV of 106 cm [65]. In addition to an order of magnitude increase in sensitivity, these systems offer the possibility of using the left ventricle of the heart or the aorta to define image-derived input functions, and of simultaneously measuring tracer kinetics in the brain and body, allowing for studies of the brain-body connection in psychiatric disorders.
In addition to increases in sensitivity due to larger axial FOV, improved performance of time-of-flight (TOF) PET results in increases in signal to noise ratio [66]. Whereas the first commercial TOF-capable PET/CT systems from around 2010 [67] were mainly beneficial to whole-body oncological imaging due to high spatial uncertainty, the latest generation of digital PET/CT scanners has a TOF resolution of slightly over 200 ps [63], which corresponds to a spatial uncertainty of 3 cm resulting in image quality improvements also for brain measurements. Combining these lines of development, the proposed neuroEXPLORER system has an axial FOV of about 50 cm and a high TOF resolution of <250 ps with improved spatial resolution due to the reduction of detector dimensions [68]. This may result in a tenfold increase of effective sensitivity compared to the HRRT, enabling also higher spatial resolution images. The large FOV and sensitivity will for instance enable high-resolution imaging of the carotid arteries, which finally may allow for quantitatively accurate measurement of image-derived input functions from these arteries despite their small size.
The typical effective radiation dose [69] due to PET scans with 11C- and 18F-labelled ligands is around 2 mSv and between 5 and 10 mSv, respectively, limiting the possibility of performing multiple examinations in the same subjects, as the maximum effective dose in clinical research is typically limited to 10 mSv depending on the expected impact of the research. Apart from improved image quality and resolution, the development of PET systems with higher sensitivity also allows for proportional reductions in the amount of administered radioactivity. This would enable longitudinal imaging protocols with increased time resolution or studies with multiple radioligands, allowing for investigation of interactions between different molecular processes [70,71,72], and also the inclusion of young adults or even children.
Multimodal approaches
In order to enhance the interpretation of findings from molecular imaging in psychiatry, a growing insight is that PET measures need to be aligned to other aspects of brain function, such as functional connectivity and neurophysiological measures (for a recent review, see [73]). Combining PET with blood-oxygenation-level dependent (BOLD) fMRI opens up for research on associations between molecular targets and neural activity in response to specific tasks. Early attempts have provided important insights into the serotonergic involvement in amygdala activity to threat-related cues [74], and more recently, advanced modelling approaches of the coupling between neurotransmitters and neural activity (fMRI) have shown how basic changes in neurotransmitter systems may affect large-scale brain network functioning and give rise to psychiatric symptoms [75]. Thus far, these studies have mainly performed PET scanning and fMRI at separate occasions, a design that has many drawbacks (e.g., different physiological states due to sleep, menstrual cycle, and food intake; and habituation or learning effects from performing the same task twice in the case of functional PET). The advent of combined PET/MR systems has enabled the simultaneous acquisition of both modalities, allowing for the exploration of more precise relations between molecular targets and hemodynamic responses. As an example, measurements of endogenous dopamine release were recently combined with fMRI to study Pavlovian fear conditioning, an experimental and translational model of anxiety disorders and PTSD [76].
As mentioned above, an obstacle to the realization of the full potential of combined fPET/fMRI is the lack of suitable radioligands for measuring changes in neurotransmitter levels during task or pharmacological challenge paradigms. In waiting for such radioligands, existing radioligands have been put to creative use. Hahn and co-workers used [18F]DOPA and a constant infusion design, where task-related deviation from expected linear increase in tracer uptake was calculated to study the dopaminergic underpinnings of reward processing, thereby making the temporal resolution of neurotransmitter release more equal to the level of fMRI [77]. For tracers with reversible kinetics, steady-state methods using bolus-infusion protocols can be used to measure changes in binding after a pharmacological challenge. In cases where a reference tissue is available, linear parametric neurotransmitter PET (lp-ntPET) has shown to be able to quantify and estimate the kinetics of neurotransmitter release with high temporal resolution [78].
Apart from studies on brain activation, further insight may be gained by adding functional magnetic resonance spectroscopy (fMRS) to assess neurometabolite concentrations in multimodal PET/MRS investigations. MRS is a non-invasive MR technique that exploits the change in MR signal exerted by the specific molecular surrounding of each biochemical (i.e., chemical shift) to produce a spectrum where specific peaks are associated with specific biochemicals (often called metabolites). Using MRS it is possible to quantify concentrations of a range of biochemicals including GABA, glutamate, choline, and N-acetyl-aspartate within an anatomically pre-defined brain region. However, neuroreceptors and transporters cannot be measured, and the relatively lower concentrations of, e.g., dopamine and serotonin and overlap of peaks with other more abundant chemicals hampers detection of these neurotransmitters. Moreover, most of the MRS studies to date have used single-voxel MRS with relative large voxels (>1 cm3) that need to be defined before data collection. MRS imaging (MRSI) can be used to produce a 2 or 3-dimensional map of spectra, but has not been applied to the same extent due to increased artefacts and longer scan times. Hence, although both PET and MRS are used to assess neurochemical processes, they differ in spatial resolution and targets. In a recent example of using MRS in conjunction with PET, measurements of prefrontal GABA with MRS and whole-brain GABA-receptor availability with [11C]Flumazenil PET were performed in patients with MDD compared to healthy controls [79]. A negative correlation between receptor and neurotransmitter availability was observed, which may be reflective of homoeostatic regulation. Of special interest in this context is the recent development of functional protocols to measure task-based changes in glutamate [80]. This opens up for the application of interleaved fMRS/fMRI acquisition, allowing for trimodal data collection of, e.g., glutamate and dopamine release together with hemodynamic measures of neural activity within a hybrid PET/MRI system. However, to the best of our knowledge, this approach is still to be realized.
Another emerging strategy to capture a richer picture of what molecular imaging is reflecting in terms of brain function is to combine PET with measurements of neural activity using neurophysiological techniques [79, 81]. In a recent example of this approach, the PET tracer [11C]Lu AE92686 was combined with both fMRI-derived striatal activity and neurophysiological striatal function measured using the mismatch negativity (MMN) response to show a link between intracellular enzyme levels, regional brain activity and behavioural brain function [81]. The combination of PET with electroencephalogram (EEG) recordings has been applied also to the serotonin system, by examining 5HT1A-R levels in relation to measures of loudness dependence of auditory evoked potentials (LDAEP) [82]. This design enabled a translation of knowledge from animal studies on the serotonergic basis of LDAEP to a clinical sample of patients with unipolar or bipolar depressive disorder. In a recent trimodal study, simultaneous EEG, molecular PET and fMRI was used to investigate functional microstates in cortical hubs in healthy participants [83]. This approach has yet to be applied to psychiatric populations. There are also other neurophysiological techniques that to the best of our knowledge so far have not been combined with molecular imaging in psychiatric samples, such as magnetoencephalography and functional near infrared spectroscopy.
Longitudinal and interventional studies
Determining changes in imaging markers over time is an important strategy to establish causal mechanisms as well as identifying individuals with specific disease trajectories that would benefit from directed and/or early interventions. In the field of neurodegenerative disease, the identification of early stages of Alzheimer’s disease by assessing mild cognitive impairment and amyloid depositions has prompted studies investigating the association of biomarkers to disease progression [84]. Early attempts in psychiatric populations include longitudinal [18F]DOPA examinations in individuals with clinical high risk for psychosis, showing an increase in uptake in those individuals that converted to psychosis, and the conversion was in turn predicted by higher levels of [18F]DOPA at baseline [85,86,87]. Despite the intense focus on serotonergic markers in the field of depression and anxiety disorders, there is a lack of longitudinal studies in this area, and we are not aware of any longitudinal psychiatric PET studies that include individuals before adulthood.
An additional approach to infer causal links between molecular imaging measures and clinical symptoms is to perform measurements before and after an intervention, comparing changes in the biomarker to changes in symptoms level. Ideally, the intervention should not directly target the marker of interest. A handful of studies have assessed changes in brain neurotransmission following psychotherapy, showing increases in serotonin markers after treatment in patients with MDD [88, 89], a relationship between reductions in symptoms of social phobia and changes in D2-R binding following cognitive behavioural therapy (CBT) [90] and reduced serotonin 1B receptor (5HT1B-R) binding after CBT in patients with MDD [91]. Similarly, PET has been applied before and after electroconvulsive therapy (ECT), showing changes in binding to the 5HT1B-R as well as the dopamine transporter [92, 93] whereas no change or inconclusive results were observed in small studies investigating the 5HT1A and dopamine D2 receptors [94,95,96]. A recent study of how expectations may modulate treatment effects of SSRI in social anxiety disorder revealed an influence on the dopamine system as shown using PET measurements of the dopamine transporter [72].
In repetitive transcranial stimulation (rTMS) used for MDD, a variety of treatment protocols have been associated to changes in metabolic activity in remote brain areas not subjected to the actual stimulation, including frontal areas and anterior cingulate cortex (ACC) [97]. In healthy volunteers, effects of rTMS was shown on dopamine signalling as measured using [11C]PHNO PET [98, 99]. We could not identify any longitudinal or non-pharmacological interventional studies using radioligands for intracellular targets, immune markers or synaptic density.
PET and precision medicine
An important step towards the application of molecular imaging in clinical practice is to find biomarkers that predict treatment response. With regard to specific molecular targets, a six-month longitudinal study in first-episode psychosis patients found that elevated [18F]DOPA uptake predicted a positive treatment response to antipsychotics [100]. Similarly, PET TSPO levels were recently shown to predict treatment response to celecoxib, a non-steroidal anti-inflammatory drug, in patients with the depressive disorder [101]. Earlier attempts focusing on brain metabolism include studies in obsessive-compulsive disorder where responders to paroxetine treatment showed decreased metabolism in frontal and subcortical regions [102], and a meta-analysis has suggested that metabolic activity in the ACC may have a predictive value for treatment response in geriatric depression [103]. Extending this paradigm to study treatment-specific predictors, McGrath et al. employed [18F]FDG PET in a sample of patients with the major depressive disorder before being randomized to either CBT or SSRI treatment. For CBT, hypometabolism in the insula (relative to the whole-brain mean) predicted remission and hypermetabolism in the same region predicted poor response, whereas the opposite pattern was noted for the SSRI escitalopram [104]. With regard to other treatment modalities, an early pilot study showed that insular [18F]FDG levels predicted treatment response to vagus nerve stimulation [105], and metabolism in the subgenual ACC has been observed to predict response to deep-brain stimulation (DBS) [106].
Importantly, taking the next step into true precision medicine requires evaluating the utility of a candidate biomarker for selecting treatment in prospective trials. However, these are still very scarce. Following the results by McGrath et al., the same group recently assigned treatment based on pre-treatment insular [18F]FDG levels, but could not provide support for insula metabolism as a treatment selection biomarker [107], and another relatively large retrospective trial including over 60 patients with MDD failed to identify any [18F]FDG PET derived cerebral biomarkers of citalopram or placebo response [108]. PET might also be used to identify individualized targets for brain stimulation therapies such as rTMS, DBS and transcranial focused ultrasound. However, early attempts using [18F]FDG PET for localization of targets for rTMS have not been successful [109, 110]. Arguably, more specific molecular targets that show a closer link to pathophysiological mechanisms are needed for treatment prediction studies, as well as the addition of multimodal functional measurements.
Once a causal mechanistic model has been established, adding relevant genetic information or blood and cerebrospinal fluid biomarkers to PET data could be a way of further enhancing the performance of prediction models. An important general aspect that needs to be taken into consideration when it comes to the use of PET in precision psychiatry is the cost-benefit trade-off including both the cost and patient radiation exposure.
Transdiagnostic studies
An important overarching limitation in research on the biological underpinnings of psychiatric disorders is the reliance on current diagnostic boundaries. Over a century of research has led to the insight that disturbances in human brain function and subsequent behaviour does not translate into the current diagnostic systems. As a consequence, trying to identify neurobiological determinants based on heterogeneous clinical diagnoses becomes an inefficient strategy [15], instead it is considered that the field should move towards employing transdiagnostic samples selected on more specific symptoms or behaviours. An extensive and ambitious initiative to aid researchers in this pursuit is the Research Domain Criteria (RDoC) framework [111], which consists of five domains of human behaviour that are proposed to reflect similar underlying neurobiology, with several dimensions that would allow the investigation of disease pathways from genes, to molecules, circuits and symptoms. This brings clear theoretical advantages for translational studies, but thus far no consensus exists on how to specifically assess these domains in clinical samples. Moreover, since the criteria were launched in 2011 only a minority of the first 48 published proposals of RDoC-related studies included more than one diagnostic category in the study sample, and only 10 examined more than one domain [112]. To date, there are only a few PET studies fully embracing the RDoC-strategy. Langenecker et al. studied patients with MDD, finding that lowered 5HT1A-R binding corresponded to a subtype with the decreased engagement of the cognitive control network and impaired resolution of interfering cognitive stimuli [113].
Approaches to increase sample size
Another general limitation in psychiatric PET research, as in other areas of molecular imaging, is the use of small samples. Notably, this gives rise not only to low sensitivity for true effects but also increases the risk for type II errors [114]. Given the high costs and sometimes cumbersome research protocols, data sharing across centres is an important way to increase sample sizes. For instance, in the field of TSPO, data from 140 healthy individuals examined using [11C]PBR28 was pooled to show the effects of gender, age and body mass index which had not been conclusively demonstrated before [115]. Similarly, employing an individual participant data metanalysis approach, Plavén-Sigray et al. synthesized TSPO data from psychosis and schizophrenia data collected at six different centres, using three different second-generation radioligands. The best fit was obtained was for the statistical model where differences in standardized binding did not vary between centres, indicating that methodological differences in data collection were not a key factor [23, 116].
In order to examine both within-diagnosis heterogeneity as well as cross-diagnostic research questions, combining samples becomes even more essential. To facilitate this development, it would of great value to collect data on dimensional symptoms, to allow for diagnostic-agnostic investigations of the biological basis for symptoms, across samples. Similarly, it is advised to include in the informed consent that data may be shared as part of international collaborations [117]. Data sharing has since long been employed in the field of dementia in the form of the Alzheimer’s Disease Neuroimaging Initiative, generating more than 3500 publications [118], as well as for MR imaging and genetics in psychiatry through the ENIGMA consortium [119]. In the field of PET, harmonized protocols for data acquisition, pre-processing and data structure, for instance, using the Brain Imaging Data Structure (BIDS) specifications could additionally facilitate data sharing [120].
Ethical issues
Another challenge when performing molecular imaging in psychiatry is the population of severely ill patients who may not be able to provide informed consent to research participation. An example is catatonia, a striking clinical presentation of a severe psychomotor disturbance, which can occur across diagnostic categories. It has been hypothesized that the symptom may have distinct neurobiological underpinnings, based on the dramatic effects of interventions such as lorazepam injection or ECT [121]. Yet, our understanding of the neurobiology of catatonia is precluded by the lack of systematic large-scale studies. Case reports reporting molecular imaging findings have pointed to a frontal-parietal hypofunction [122], however, all these studies investigated patients only after having been successfully treated with lorazepam. In one of the few studies using informed consent from peers instead of from the patients, patients were investigated during the actual catatonic state before and after ECT. In this study another pattern emerged, with increased blood flow in parietal, temporal, and occipital regions [123], suggesting that examining patients during the actual state can provide more relevant information. Difficulties of investigating severe illnesses in patients who cannot provide informed consent are shared with other areas of research such as emergency research and dementia studies, where there are recommendations available on situations where a consent waiver could be applied for intervention studies [124].
Other areas where ethical issues can be present are studies of paediatric populations or young individuals with prodromal signs of psychotic illness. Studies using molecular imaging early in the development of a brain disorder can be critical for the understanding of key disease mechanisms and how they may be modified or even prevented. An example of this is studies of autism during childhood and adolescence where an aberrant development of the serotonergic system has been revealed, suggesting new possible interventions [125]. Hence, whereas it could be considered ethical to refrain from studying individuals who cannot provide informed consent from an individual level, it could at the same time be considered unethical not to study the disorder from a patient population level.
Conclusions and future directions
The contribution of mental disorders to the global disease burden has increased from 3.1 to 4.9% between 1990 and 2019, corresponding to 125.3 million disability-adjusted life-years (DALYs) [126]. This disability is distributed across all age groups, with a peak between 25 and 34 years. Notably, these estimates did not include substance use disorders which together account for similar proportions of disability [127]. For Alzheimer’s disease, a brain disorder causing approximately 5.2 million DALYs [128], the estimated research budget for the National Institute of Health in the US for 2022 was 3.2 billion USD, whereas for all mental disorders (except substance use disorders) the corresponding amount was 1.7 billion USD [129]. Although not necessarily reflecting global priorities, these figures indicate that an increased focus on research on mental disorders is highly warranted, including investing in the development of methods specifically designed for this purpose (Fig. 2).
The discovery and marketing of antipsychotics, acting mainly on the dopamine system, in the 1950s and serotonergic antidepressants in the 1980s, was the main basis for two major disease models in psychiatry – the dopamine hypothesis of schizophrenia, and the serotonin hypothesis of depression. These conceptualizations have been a powerful driver of research into pathophysiology, resulting in a strong focus of psychiatric molecular imaging research on monoaminergic brain neurotransmission systems. The lack of resulting diagnostic tools or new treatment approaches indicate that causal mechanisms may involve other aspects of brain function, hence identifying new targets and radioligands is a critical step to advance psychiatric PET research. A concern is that programs for radioligand development are often driven by the pharmaceutical industry to validate compounds based on existing disease models, such as those above, or aimed towards other disease areas such as neurodegeneration or oncology, rather than being informed by new hypotheses regarding psychiatric disorders. The immune system has been implicated in both genetic and biomolecular studies across several psychiatric diagnoses [24], and with regard to schizophrenia, recent genetic and experimental data have suggested a mechanistic model involving immune-neuronal interactions, converging on aberrant synaptic development and plasticity [130,131,132]. These new disease models have indeed led to a shift of focus, and new radioligands for immune markers and synaptic density have to some extent been applied in psychiatric conditions, but much remains unexplored. For instance, we could not identify any longitudinal, intervention or treatment prediction studies involving these radioligands.
Psychiatric conditions in general are likely not caused by loss of neurons or tissue damage. Instead, symptoms are thought to reflect changes in dynamic brain function and plasticity, leading to aberrant information processing. Hence, these aspects need to be incorporated in order to fully understand the results of molecular imaging studies. A growing number of studies are combining PET with other imaging modalities such as fMRI as well as neurophysiological measures. These paradigms have mainly targeted monoaminergic brain neurotransmission systems, and should now also be extended to new putative markers of pathophysiology. In addition, there is increasing evidence indicating that psychiatric symptoms may be a result of an interplay between the brain and other organs such as the gut [133], suggesting that molecular imaging studies in some cases could be extended to include also whole-body examinations.
Whereas some psychiatric conditions are by definition considered neurodevelopmental disorders (autism spectrum disorders and attention-deficit/hyperactivity disorder), an emerging view also for other diagnoses is that genetic and environmental risk factors interact over longer time periods before symptoms present (e.g. refs. [134, 135]). Hence, for many conditions, investigations may need to be initiated already during childhood or adolescence to fully capture the entire disease course. One important aspect of methodological development is to increase sensitivity such that radioactivity dosing can be reduced, allowing both for repeated examinations and studies in early life, as well as investigating multiple targets in the same individual. Moreover, disease trajectories are often heterogeneous, spanning from continuous symptom presentation and disability to relapsing-remitting courses. There is a clear lack of molecular imaging studies in psychiatric patients over longer time periods, for instance comparing periods of active disease to periods of higher functioning. Again, an important requisite for this development is a new methodology to allow for the administration of lower amounts of radioactivity.
Examining individuals with severe mental disorders involves both practical and ethical challenges. In order to gain information regarding these conditions, it is vital to simplify experimental procedures as well as limit the number of research visits. Methods to quantify radioligand binding without the use of an arterial input function, methodology allowing for shorter times of acquisition, as well as simultaneous multimodal measurements are important steps in this direction.
The definition of psychiatric diagnoses has essentially remained the same since before the advent of genetic research and modern neuroscience. Despite that psychiatric diagnoses are generally acknowledged to not reflect underlying biology, most research using molecular imaging have aimed to compare specific diagnostic populations to unaffected individuals. Initiatives such as the RDoC [111] have been applied to a very limited extent in psychiatric PET research, limiting the disentangling of specific symptom domains from the imposed diagnostic framework. Ideally, researchers should strive to include both diagnostic information and assessment of dimensional symptoms in studies. This would allow both for the identification of subgroups within diagnoses and common biological aberrations across disorders.
A general constraint in PET research has been small samples, both limiting the inferential value of results and hampering research into diagnostic heterogeneity. In a field with limited resources, systems for grant distribution and publication lead to a focus on novelty rather than broad, systematic research programs. At present, in order to reach desired sample sizes, collaboration and pooling across centres are necessary. Initiatives to harmonize research protocols and data acquisition is an important development towards this goal. This would also require a shift of focus in grant providers, as well as legislators regarding the possibility of sharing information across regional and national boundaries, such that researchers can engage in a concerted action to diminish the global burden of mental disorders.
In conclusion, by being the only method that can directly access brain molecular processes we believe that PET will play an increasingly important part in understanding the aetiology, progression, and treatment of the highly impairing psychiatric disorders. However, this requires substantial investments to accelerate the development across several areas, including identifying and validating suitable radioligands, more precise acquisition and quantification methods, multimodal imaging protocols, longitudinal and interventional paradigms in large samples, as well as data sharing and collaboration.
References
Health at a Glance: Europe 2020. OECD, 2020. https://doi.org/10.1787/82129230-en.
Jääskeläinen E, Juola P, Hirvonen N, McGrath JJ, Saha S, Isohanni M, et al. A systematic review and meta-analysis of recovery in schizophrenia. Schizophr Bull. 2013;39:1296–306.
Patel V, Chisholm D, Parikh R, Charlson FJ, Degenhardt L, Dua T, et al. Addressing the burden of mental, neurological, and substance use disorders: key messages from disease control priorities, 3rd edition. Lancet. 2016;387:1672–85.
Farde L, Hall H, Ehrin E, Sedvall G. Quantitative analysis of D2 dopamine receptor binding in the living human brain by PET. Science. 1986;231:258–61.
Nordström AL, Farde L, Wiesel FA, Forslund K, Pauli S, Halldin C, et al. Central D2-dopamine receptor occupancy in relation to antipsychotic drug effects: a double-blind PET study of schizophrenic patients. Biol Psychiatry. 1993;33:227–35.
Cervenka S, Farde L. Molecular imaging. In: Kubicki M, Shenton ME, editors. Neuroimaging in schizophrenia. Switzerland: Springer Nature; 2020;145–59.
Plavén-sigray P, Victorsson PI, Santillo A, Matheson GJ, Lee M, Fatouros-bergman H, et al. Thalamic dopamine D2-receptor availability in schizophrenia: a study on antipsychotic-naive patients with first-episode psychosis and a meta-analysis. Mol Psychiatry. 2022;27:1233–40.
Spies M, Knudsen GM, Lanzenberger R, Kasper S. The serotonin transporter in psychiatric disorders: Insights from PET imaging. Lancet Psychiatry. 2015;2:743–55.
Wang L, Zhou C, Zhu D, Wang X, Fang L, Zhong J, et al. Serotonin-1A receptor alterations in depression: a meta-analysis of molecular imaging studies. BMC Psychiatry. 2016;16:319.
Fredrikson M, Faria V, Furmark T. A review of PET and SPECT studies in anxiety disorders. In: Dierckx R, Otte A, de Vries E, van Waarde A, den Boer J, editors. PET and SPECT in psychiatry. Berlin: Springer; 2014;349–70.
Erritzoe D, Ashok AH, Searle GE, Colasanti A, Turton S, Lewis Y, et al. Serotonin release measured in the human brain: a PET study with [11C]CIMBI-36 and d-amphetamine challenge. Neuropsychopharmacology. 2020;45:804–10.
Yang K-C, Takano A, Halldin C, Farde L, Finnema SJ. Serotonin concentration enhancers at clinically relevant doses reduce [11C]AZ10419369 binding to the 5-HT1B receptors in the nonhuman primate brain. Transl Psychiatry. 2018;8:132.
Caravaggio F, Nakajima S, Borlido C, Remington G, Gerretsen P, Wilson A, et al. Estimating endogenous dopamine levels at D2 and D3 receptors in humans using the agonist radiotracer [(11)C]-(+)-PHNO. Neuropsychopharmacology. 2014;39:866–74.
Finnema SJ, Stepanov V, Nakao R, Sromek AW, Zhang T, Neumeyer JL. et al. (18)F-MCL-524, an (18)F-Labeled Dopamine D2 and D3 Receptor Agonist Sensitive to Dopamine: A Preliminary PET Study. J Nucl Med. 2014;55:1164–70.
Insel TR. Rethinking schizophrenia. Nature. 2010;468:187–93.
Gómez-Vallejo V, Ugarte A, García-Barroso C, Cuadrado-Tejedor M, Szczupak B, Dopeso-Reyes IG, et al. Pharmacokinetic investigation of sildenafil using positron emission tomography and determination of its effect on cerebrospinal fluid cGMP levels. J Neurochem. 2016;136:403–15.
Bodén R, Persson J, Wall A, Lubberink M, Ekselius L, Larsson E-M, et al. Striatal phosphodiesterase 10A and medial prefrontal cortical thickness in patients with schizophrenia: a PET and MRI study. Transl Psychiatry. 2017;7:e1050.
Marques TR, Natesan S, Niccolini F, Politis M, Gunn RN, Searle GE, et al. Phosphodiesterase 10A in schizophrenia: A PET study using [11C]IMA107. Am J Psychiatry. 2016;173:714–21.
Fujita M, Richards EM, Niciu MJ, Ionescu DF, Zoghbi SS, Hong J, et al. cAMP signaling in brain is decreased in unmedicated depressed patients and increased by treatment with a selective serotonin reuptake inhibitor. Mol Psychiatry. 2017;22:754–9.
Grauer SM, Pulito VL, Navarra RL, Kelly MP, Kelley C, Graf R, et al. Phosphodiesterase 10A inhibitor activity in preclinical models of the positive, cognitive, and negative symptoms of schizophrenia. J Pharm Exp Ther. 2009;331:574–90.
Blokland A, Heckman P, Vanmierlo T, Schreiber R, Paes D, Prickaerts J. Phosphodiesterase type 4 inhibition in CNS diseases. Trends Pharm Sci. 2019;40:971–85.
Zhang L, Chen L, Beck EM, Chappie TA, Coelho RV, Doran SD, et al. The discovery of a novel phosphodiesterase (PDE) 4B-preferring radioligand for positron emission tomography (PET) imaging. J Med Chem. 2017;60:8538–51.
Plavén-Sigray P, Matheson GJ, Coughlin JM, Hafizi S, Laurikainen H, Ottoy J, et al. Meta-analysis of the glial marker TSPO in psychosis revisited: reconciling inconclusive findings of patient-control differences. Biol Psychiatry. 2021;89:e5–e8.
Meyer JH, Cervenka S, Kim M-J, Kreisl WC, Henter ID, Innis RB. Neuroinflammation in psychiatric disorders: PET imaging and promising new targets. Lancet Psychiatry. 2020;7:1064–74.
Lavisse S, Guillermier M, He A, Petit F, Delahaye M, Camp N Van, et al. Reactive astrocytes overexpress TSPO and are detected by TSPO positron emission tomography imaging. J Neurosci. 2012;32:10809–18.
Toth M, Little P, Arnberg F, Mulder J, Halldin C, Ha J, et al. Acute neuroinflammation in a clinically relevant focal cortical ischemic stroke model in rat: longitudinal positron emission tomography and immunofluorescent tracking. Brain Struct Funct. 2016;221:1279–90.
Owen DR, Narayan N, Wells L, Healy L, Smyth E, Rabiner EA, et al. Pro-inflammatory activation of primary microglia and macrophages increases 18 kDa translocator protein expression in rodents but not humans. J Cereb Blood Flow Metab. 2017;37:2679–90.
Pannell M, Economopoulos V, Wilson TC, Kersemans V, Isenegger PG, Larkin JR, et al. Imaging of translocator protein upregulation is selective for pro‐inflammatory polarized astrocytes and microglia. Glia. 2020;68:280–97.
Moriguchi S, Wilson AA, Miler L, Rusjan PM, Vasdev N, Kish SJ, et al. Monoamine oxidase B total distribution volume in the prefrontal cortex of major depressive disorder: an [11C]SL25.1188 positron emission tomography study. JAMA psychiatry. 2019;76:634–41.
Gill T, Watling SE, Richardson JD, McCluskey T, Tong J, Meyer JH, et al. Imaging of astrocytes in posttraumatic stress disorder: A PET study with the monoamine oxidase B radioligand [11C]SL25.1188. Eur Neuropsychopharmacol. 2021;54:54–61.
Finnema SJ, Nabulsi NB, Eid T, Detyniecki K, Lin S, Chen M, et al. Imaging synaptic density in the living human brain. Sci Transl Med. 2016;8:348ra96.
Holmes SE, Scheinost D, Finnema SJ, Naganawa M, Davis MT, Dellagioia N, et al. Lower synaptic density is associated with depression severity and network alterations. Nat Commun. 2019;10:1529.
Onwordi EC, Halff EF, Whitehurst T, Mansur A, Cotel MC, Wells L, et al. Synaptic density marker SV2A is reduced in schizophrenia patients and unaffected by antipsychotics in rats. Nat Commun. 2020;11:246.
Radhakrishnan R, Skosnik PD, Ranganathan M, Naganawa M, Toyonaga T, Finnema S, et al. In vivo evidence of lower synaptic vesicle density in schizophrenia. Mol Psychiatry. 2021;26:7690–8.
D’Souza DC, Radhakrishnan R, Naganawa M, Ganesh S, Nabulsi N, Najafzadeh S, et al. Preliminary in vivo evidence of lower hippocampal synaptic density in cannabis use disorder. Mol Psychiatry. 2021;26:3192–3200.
Marconi A, Di Forti M, Lewis CM, Murray RM, Vassos E. Meta-analysis of the association between the level of cannabis use and risk of psychosis. Schizophr Bull. 2016;42:1262–9.
Sehlin D, Syvänen S. MINC faculty. Engineered antibodies: new possibilities for brain PET? Eur J Nucl Med Mol Imaging. 2019;46:2848–58.
Fang XT, Hultqvist G, Meier SR, Antoni G, Sehlin D, Syvänen S. High detection sensitivity with antibody-based PET radioligand for amyloid beta in brain. Neuroimage. 2019;184:881–8.
Sarrett SM, Keinänen O, Dayts EJ, Dewaele-Le Roi G, Rodriguez C, Carnazza KE, et al. Inverse electron demand Diels-Alder click chemistry for pretargeted PET imaging and radioimmunotherapy. Nat Protoc. 2021;16:3348–81.
Laruelle M, Slifstein M, Huang Y. Relationships between radiotracer properties and image quality in molecular imaging of the brain with positron emission tomography. Mol Imaging Biol. 2003;5:363–75.
Svensson JE, Schain M, Plavén-Sigray P, Cervenka S, Tiger M, Nord M, et al. Validity and reliability of extrastriatal [11C]raclopride binding quantification in the living human brain. Neuroimage. 2019;202:116143.
Freiburghaus T, Svensson JE, Matheson GJ, Plavén-Sigray P, Lundberg J, Farde L, et al. Low convergent validity of [11C]raclopride binding in extrastriatal brain regions: A PET study of within-subject correlations with [11C]FLB 457. Neuroimage. 2021;226:117523.
Li S, Naganawa M, Pracitto R, Najafzadeh S, Holden D, Henry S, et al. Assessment of test-retest reproducibility of [18F]SynVesT-1, a novel radiotracer for PET imaging of synaptic vesicle glycoprotein 2A. Eur J Nucl Med Mol Imaging. 2021;48:1327–38.
Naganawa M, Li S, Nabulsi N, Henry S, Zheng MQ, Pracitto R, et al. First-in-Human Evaluation of 18 F-SynVesT-1, a Radioligand for PET Imaging of Synaptic Vesicle Glycoprotein 2A. J Nucl Med. 2021;62:561–7.
Matheson GJ, Plavén-Sigray P, Forsberg A, Varrone A, Farde L, Cervenka S. Assessment of simplified ratio-based approaches for quantification of PET [11C]PBR28 data. EJNMMI Res. 2017;7:58.
Plavén-sigray P, Matheson GJ, Cselenyi Z, Jučaite A, Farde L, Cervenka S. Test-retest reliability and convergent validity of (R) - [11 C] PK11195 outcome measures from pseudo-reference region, supervised cluster analysis and standardized uptake values. 2018;8:102.
Gershen LD, Zanotti-Fregonara P, Dustin IH, Liow J-S, Hirvonen J, Kreisl WC, et al. Neuroinflammation in temporal lobe epilepsy measured using positron emission tomographic imaging of translocator protein. JAMA Neurol. 2015;72:882–8.
Datta G, Colasanti A, Rabiner EA, Gunn RN, Malik O, Ciccarelli O, et al. Neuroinflammation and its relationship to changes in brain volume and white matter lesions in multiple sclerosis. Brain. 2017;140:2927–38.
Koole M, van Aalst J, Devrome M, Mertens N, Serdons K, Lacroix B, et al. Quantifying SV2A density and drug occupancy in the human brain using [11C]UCB-J PET imaging and subcortical white matter as reference tissue. Eur J Nucl Med Mol Imaging. 2019;46:396–406.
Naganawa M, Gallezot J-D, Finnema SJ, Matuskey D, Mecca A, Nabulsi NB, et al. Simplified quantification of 11C-UCB-J PET evaluated in a large human cohort. J Nucl Med. 2021;62:418–21.
Rossano S, Toyonaga T, Finnema SJ, Naganawa M, Lu Y, Nabulsi N, et al. Assessment of a white matter reference region for 11C-UCB-J PET quantification. J Cereb Blood Flow Metab. 2020;40:1890–901.
Kanegawa N, Schain M, Collste K, Amini N, Takano A, Halldin C, et al. Towards less-invasive quantification of [11C]PBR28: image-derived and population-based input functions. In: International Conference on Quantification of Brain Function with PET. 2015.
Mabrouk R, Rusjan PM, Mizrahi R, Jacobs MF, Koshimori Y, Houle S, et al. Image derived input function for [18F]-FEPPA: application to quantify translocator protein (18 kDa) in the human brain. PLoS ONE. 2014;9:e115768.
Greuter H, Lubberink M, Hendrikse NH, van der Veldt A, Wong Y, Schuit R, et al. Venous versus arterial blood samples for plasma input pharmacokinetic analysis of different radiotracer PET studies. J Nucl Med. 2011;52:1974.
Ng Y, Moberly SP, Mather KJ, Brown-Proctor C, Hutchins GD, Green MA. Equivalence of arterial and venous blood for [11C]CO2-metabolite analysis following intravenous administration of 1-[11C]acetate and 1-[11C]palmitate. Nucl Med Biol. 2013;40:361–5.
Plavén-Sigray P, Schain M, Zanderigo F, Farde L, Halldin C, Forsberg A, et al. Accuracy and reliability of [11 C]PBR28 specific binding estimated without the use of a reference region. Neuroimage. 2019;188:102–10.
Schain M, Zanderigo F, Ogden RT, Kreisl WC. Non-invasive estimation of [11C]PBR28 binding potential. Neuroimage. 2018;169:278–85.
Laurell GL, Plavén-Sigray P, Jucaite A, Varrone A, Cosgrove KP, Svarer C, et al. Nondisplaceable binding is a potential confounding factor in 11C-PBR28 translocator protein PET studies. J Nucl Med. 2021;62:412–7.
Matheson GJ, Ogden RT. Simultaneous Multifactor Bayesian Analysis (SiMBA) of PET Time Activity Curve Data. Neuroimage. 2022;256:119195.
Tjerkaski J, Cervenka S, Farde L, Matheson GJ. Kinfitr – an open source tool for reproducible PET modelling: validation and evaluation of test-retest reliability. EJNMMI Res. 2020;10:77.
de Jong HWAM, van Velden FHP, Kloet RW, Buijs FL, Boellaard R, Lammertsma AA. Performance evaluation of the ECAT HRRT: an LSO-LYSO double layer high resolution, high sensitivity scanner. Phys Med Biol. 2007;52:1505–26.
Hsu DFC, Ilan E, Peterson WT, Uribe J, Lubberink M, Levin CS. Studies of a next-generation silicon-photomultiplier-based time-of-flight PET/CT system. J Nucl Med. 2017;58:1511–8.
Van Sluis J, De Jong J, Schaar J, Noordzij W, Van Snick P, Dierckx R, et al. Performance characteristics of the digital biograph vision PET/CT system. J Nucl Med. 2019;60:1031–6.
Spencer BA, Berg E, Schmall JP, Omidvari N, Leung EK, Abdelhafez YG, et al. Performance evaluation of the uEXPLORER total-body PET/CT scanner based on NEMA NU 2-2018 with additional tests to characterize PET scanners with a long axial field of view. J Nucl Med. 2021;62:861–70.
Prenosil GA, Sari H, Fürstner M, Afshar-Oromieh A, Shi K, Rominger A, et al. Performance characteristics of the biograph vision quadra PET/CT system with long axial field of view using the NEMA NU 2-2018 standard. J Nucl Med. 2022;63:476–84.
Surti S. Update on time-of-flight PET imaging. J Nucl Med. 2015;56:98–105.
Surti S, Kuhn A, Werner ME, Perkins AE, Kolthammer J, Karp JS. Performance of Philips Gemini TF PET/CT scanner with special consideration for its time-of-flight imaging capabilities. J Nucl Med. 2007;48:471–80.
Carson R, Berg E, Badawi R, Cherry S, Du J, Feng T, et al. Design of the NeuroEXPLORER, a next-generation ultra-high performance human brain PET imager. J Nucl Med. 2021;62:(supplement 1)1120.
ICRP. The 2007 recommendations of the international commission on radiological protection. ICRP Publication 103. Ann ICRP. 2007;37:2–4.
Frick A, Åhs F, Palmquist ÅM, Pissiota A, Wallenquist U, Fernandez M, et al. Overlapping expression of serotonin transporters and neurokinin-1 receptors in posttraumatic stress disorder: a multi-tracer PET study. Mol Psychiatry. 2016;21:1400–7.
Hjorth OR, Frick A, Gingnell M, Hoppe JM, Faria V, Hultberg S, et al. Expression and co-expression of serotonin and dopamine transporters in social anxiety disorder: a multitracer positron emission tomography study. Mol Psychiatry. 2021;26:3970–9.
Hjorth OR, Frick A, Gingnell M, Hoppe JM, Faria V, Hultberg S, et al. Expectancy effects on serotonin and dopamine transporters during SSRI treatment of social anxiety disorder: a randomized clinical trial. Transl Psychiatry. 2021;11:559.
Sander CY, Hansen HD, Wey H-Y. Advances in simultaneous PET/MR for imaging neuroreceptor function. J Cereb Blood Flow Metab. 2020;40:1148–66.
Fisher PM, Meltzer CC, Ziolko SK, Price JC, Moses-Kolko EL, Berga SL, et al. Capacity for 5-HT1A-mediated autoregulation predicts amygdala reactivity. Nat Neurosci. 2006;9:1362–3.
Kringelbach ML, Cruzat J, Cabral J, Knudsen GM, Carhart-Harris R, Whybrow PC, et al. Dynamic coupling of whole-brain neuronal and neurotransmitter systems. Proc Natl Acad Sci USA. 2020;117:9566–76.
Frick A, Björkstrand J, Lubberink M, Eriksson A, Fredrikson M, Åhs F. Dopamine and fear memory formation in the human amygdala. Mol Psychiatry. 2022;27:1704–11.
Hahn A, Reed MB, Pichler V, Michenthaler P, Rischka L, Godbersen GM, et al. Functional dynamics of dopamine synthesis during monetary reward and punishment processing. J Cereb Blood Flow Metab. 2021;41:2973–85.
Cosgrove KP, Wang S, Kim S-J, McGovern E, Nabulsi N, Gao H, et al. Sex differences in the brain’s dopamine signature of cigarette smoking. J Neurosci. 2014;34:16851–5.
Persson J, Wall A, Weis J, Gingnell M, Antoni G, Lubberink M, et al. Inhibitory and excitatory neurotransmitter systems in depressed and healthy: A positron emission tomography and magnetic resonance spectroscopy study. Psychiatry Res Neuroimaging. 2021;315:111327.
Mullins PG. Towards a theory of functional magnetic resonance spectroscopy (fMRS): a meta-analysis and discussion of using MRS to measure changes in neurotransmitters in real time. Scand J Psychol. 2018;59:91–103.
Persson J, Szalisznyó K, Antoni G, Wall A, Fällmar D, Zora H, et al. Phosphodiesterase 10A levels are related to striatal function in schizophrenia: a combined positron emission tomography and functional magnetic resonance imaging study. Eur Arch Psychiatry Clin Neurosci. 2020;270:451–9.
Pillai RLI, Bartlett EA, Ananth MR, Zhu C, Yang J, Hajcak G, et al. Examining the underpinnings of loudness dependence of auditory evoked potentials with positron emission tomography. Neuroimage. 2020;213:116733.
Rajkumar R, Régio Brambilla C, Veselinović T, Bierbrier J, Wyss C, Ramkiran S, et al. Excitatory-inhibitory balance within EEG microstates and resting-state fMRI networks: assessed via simultaneous trimodal PET-MR-EEG imaging. Transl Psychiatry. 2021;11:60.
Jack CR, Wiste HJ, Schwarz CG, Lowe VJ, Senjem ML, Vemuri P, et al. Longitudinal tau PET in ageing and Alzheimer’s disease. Brain. 2018;141:1517–28.
Howes O, Bose S, Turkheimer F, Valli I, Egerton A, Stahl D, et al. Progressive increase in striatal dopamine synthesis capacity as patients develop psychosis: a PET study. Mol Psychiatry. 2011;16:885–6.
Howes OD, Bose SK, Turkheimer F, Valli I, Egerton A, Valmaggia LR, et al. Dopamine synthesis capacity before onset of psychosis: a prospective [18 F]-DOPA PET imaging study. Am J Psychiatry. 2011;168:1311–7.
Egerton A, Chaddock CA, Winton-Brown TT, Bloomfield MAP, Bhattacharyya S, Allen P, et al. Presynaptic striatal dopamine dysfunction in people at ultra-high risk for psychosis: findings in a second cohort. Biol Psychiatry. 2013;74:106–12.
Lehto SM, Tolmunen T, Joensuu M, Saarinen PI, Valkonen-Korhonen M, Vanninen R, et al. Changes in midbrain serotonin transporter availability in atypically depressed subjects after one year of psychotherapy. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32:229–37.
Karlsson H, Hirvonen J, Kajander J, Markkula J, Rasi-Hakala H, Salminen JK, et al. Research letter: Psychotherapy increases brain serotonin 5-HT1A receptors in patients with major depressive disorder. Psychol Med. 2010;40:523–8.
Cervenka S, Hedman E, Ikoma Y, Djurfeldt DR, Rück C, Halldin C, et al. Changes in dopamine D2-receptor binding are associated to symptom reduction after psychotherapy in social anxiety disorder. Transl Psychiatry. 2012;2:e120.
Tiger M, Rück C, Forsberg A, Varrone A, Lindefors N, Halldin C, et al. Reduced 5-HT(1B) receptor binding in the dorsal brain stem after cognitive behavioural therapy of major depressive disorder. Psychiatry Res. 2014;223:164–70.
Masuoka T, Tateno A, Sakayori T, Tiger M, Kim W, Moriya H, et al. Electroconvulsive therapy decreases striatal dopamine transporter binding in patients with depression: a positron emission tomography study with [18F]FE-PE2I. Psychiatry Res Neuroimaging. 2020;301:111086.
Tiger M, Gärde M, Tateno A, Matheson GJ, Sakayori T, Nogami T, et al. A positron emission tomography study of the serotonin1B receptor effect of electroconvulsive therapy for severe major depressive episodes. J Affect Disord. 2021;294:645–51.
Tiger M, Svensson J, Liberg B, Saijo T, Schain M, Halldin C, et al. [11 C]raclopride positron emission tomography study of dopamine-D2/3 receptor binding in patients with severe major depressive episodes before and after electroconvulsive therapy and compared to control subjects. Psychiatry Clin Neurosci. 2020;74:263–9.
Saijo T, Takano A, Suhara T, Arakawa R, Okumura M, Ichimiya T, et al. Effect of electroconvulsive therapy on 5-HT1A receptor binding in patients with depression: a PET study with [11C]WAY 100635. Int J Neuropsychopharmacol. 2010;13:785–91.
Saijo T, Takano A, Suhara T, Arakawa R, Okumura M, Ichimiya T, et al. Electroconvulsive therapy decreases dopamine D2receptor binding in the anterior cingulate in patients with depression: a controlled study using positron emission tomography with radioligand [11C]FLB 457. J Clin Psychiatry. 2010;71:793–9.
Tremblay S, Tuominen L, Zayed V, Pascual-Leone A, Joutsa J. The study of noninvasive brain stimulation using molecular brain imaging: a systematic review. Neuroimage. 2020;219:117023.
Cho SS, Strafella AP. rTMS of the left dorsolateral prefrontal cortex modulates dopamine release in the ipsilateral anterior cingulate cortex and orbitofrontal cortex. PLoS ONE. 2009;4:e6725.
Malik S, Jacobs M, Cho SS, Boileau I, Blumberger D, Heilig M, et al. Deep TMS of the insula using the H-coil modulates dopamine release: a crossover [11 C] PHNO-PET pilot trial in healthy humans. Brain Imaging Behav. 2018;12:1306–17.
Jauhar S, Veronese M, Nour MM, Rogdaki M, Hathway P, Turkheimer FE, et al. Determinants of treatment response in first-episode psychosis: an 18F-DOPA PET study. Mol Psychiatry. 2019;24:1502–12.
Attwells S, Setiawan E, Rusjan PM, Xu C, Hutton C, Rafiei D, et al. Translocator protein distribution volume predicts reduction of symptoms during open-label trial of celecoxib in major depressive disorder. Biol Psychiatry. 2020;88:649–56.
Saxena S, Brody AL, Maidment KM, Dunkin JJ, Colgan M, Alborzian S, et al. Localized orbitofrontal and subcortical metabolic changes and predictors of response to paroxetine treatment in obsessive-compulsive disorder. Neuropsychopharmacology. 1999;21:683–93.
De Crescenzo F, Ciliberto M, Menghini D, Treglia G, Ebmeier KP, Janiri L. Is 18F-FDG-PET suitable to predict clinical response to the treatment of geriatric depression? A systematic review of PET studies. Aging Ment Health. 2017;21:889–94.
McGrath CL, Kelley ME, Holtzheimer PE, Dunlop BW, Craighead WE, Franco AR, et al. Toward a neuroimaging treatment selection biomarker for major depressive disorder. JAMA Psychiatry. 2013;70:821–9.
Conway CR, Chibnall JT, Gangwani S, Mintun MA, Price JL, Hershey T, et al. Pretreatment cerebral metabolic activity correlates with antidepressant efficacy of vagus nerve stimulation in treatment-resistant major depression: a potential marker for response? J Affect Disord. 2012;139:283–90.
Brown EC, Clark DL, Forkert ND, Molnar CP, Kiss ZHT, Ramasubbu R. Metabolic activity in subcallosal cingulate predicts response to deep brain stimulation for depression. Neuropsychopharmacology. 2020;45:1681–8.
Kelley ME, Choi KS, Rajendra JK, Craighead WE, Rakofsky JJ, Dunlop BW, et al. Establishing evidence for clinical utility of a neuroimaging biomarker in major depressive disorder: prospective testing and implementation challenges. Biol Psychiatry. 2021;90:236–42.
Hill KR, Gardus JD, Bartlett EA, Perlman G, Parsey RV, DeLorenzo C. Measuring brain glucose metabolism in order to predict response to antidepressant or placebo: a randomized clinical trial. NeuroImage Clin. 2021;32:102858.
Paillère Martinot M-L, Galinowski A, Ringuenet D, Gallarda T, Lefaucheur J-P, Bellivier F, et al. Influence of prefrontal target region on the efficacy of repetitive transcranial magnetic stimulation in patients with medication-resistant depression: a [(18)F]-fluorodeoxyglucose PET and MRI study. Int J Neuropsychopharmacol. 2010;13:45–59.
Garcia-Toro M, Salva J, Daumal J, Andres J, Romera M, Lafau O, et al. High (20-Hz) and low (1-Hz) frequency transcranial magnetic stimulation as adjuvant treatment in medication-resistant depression. Psychiatry Res. 2006;146:53–7.
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research Domain Criteria (RDoC): Toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–51.
Carcone D, Ruocco AC. Six Years of Research on the National Institute of Mental Health’s Research Domain Criteria (RDoC) Initiative: A Systematic Review. Front Cell Neurosci. 2017;11:46.
Langenecker SA, Mickey BJ, Eichhammer P, Sen S, Elverman KH, Kennedy SE, et al. Cognitive control as a 5-HT1A-based domain that is disrupted in major depressive disorder. Front Psychol. 2019;10:691.
Button KS, Ioannidis JPA, Mokrysz C, Nosek BA, Flint J, Robinson ESJ, et al. Power failure: why small sample size undermines the reliability of neuroscience. Nat Rev Neurosci. 2013;14:365–76.
Tuisku J, Plavén-Sigray P, Gaiser EC, Airas L, Al-Abdulrasul H, Brück A, et al. Effects of age, BMI and sex on the glial cell marker TSPO — a multicentre [11C]PBR28 HRRT PET study. Eur J Nucl Med Mol Imaging. 2019;46:2329–38.
Plavén-Sigray P, Matheson GJ, Collste K, Ashok AH, Coughlin JM, Howes OD, et al. Positron emission tomography studies of the glial cell marker translocator protein in patients with psychosis: a meta-analysis using individual participant data. Biol Psychiatry. 2018;84:433–42.
Matheson GJ, Plavén-sigray P, Tuisku J, Rinne J, Matuskey D, Cervenka S. Clinical brain PET research must embrace multi-centre collaboration and data sharing or risk its demise. Eur J Nucl Med Mol Imaging. 2020;47:502–4.
Veitch DP, Weiner MW, Aisen PS, Beckett LA, DeCarli C, Green RC, et al. Using the Alzheimer’s disease neuroimaging initiative to improve early detection, diagnosis, and treatment of Alzheimer’s disease. Alzheimers Dement. 2022;18:824–57.
Thompson PM, Jahanshad N, Schmaal L, Turner JA, Winkler AM, Thomopoulos SI, et al. The Enhancing neuroimaging genetics through meta-analysis consortium: 10 years of global collaborations in human brain mapping. Hum Brain Mapp. 2022;43:15–22.
Knudsen GM, Ganz M, Appelhoff S, Boellaard R, Bormans G, Carson RE, et al. Guidelines for the content and format of PET brain data in publications and archives: a consensus paper. J Cereb Blood Flow Metab. 2020;40:1576–85.
Fink M. Rediscovering catatonia: the biography of a treatable syndrome. Acta Psychiatr Scand Suppl. 2013:1–47.
Haroche A, Rogers J, Plaze M, Gaillard R, Williams SC, Thomas P, et al. Brain imaging in catatonia: systematic review and directions for future research. Psychol Med. 2020;50:1585–97.
Escobar R, Rios A, Montoya ID, Lopera F, Ramos D, Carvajal C, et al. Clinical and cerebral blood flow changes in catatonic patients treated with ECT. J Psychosom Res. 2000;49:423–9.
Rebers S, Aaronson NK, van Leeuwen FE, Schmidt MK. Exceptions to the rule of informed consent for research with an intervention. BMC Med Ethics. 2016;17:9.
Hwang BJ, Mohamed MA, Brašić JR. Molecular imaging of autism spectrum disorder. Int Rev Psychiatry. 2017;29:530–54.
GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study. Lancet Psychiatry. 2022;9:137–50.
Degenhardt L, Charlson F, Ferrari A, Santomauro D, Erskine H, Mantilla-Herrara A, et al. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5:987–1012.
Deuschl G, Beghi E, Fazekas F, Varga T, Christoforidi KA, Sipido E, et al. The burden of neurological diseases in Europe: an analysis for the Global Burden of Disease Study 2017. Lancet Public Heal. 2020;5:e551–67.
National Institute of health. Estimates of Funding for Various Research, Condition, and Disease Categories (RCDC). 2021. https://report.nih.gov/funding/categorical-spending#/9).
Sekar A, Bialas AR, de Rivera H, Davis A, Hammond TR, Kamitaki N, et al. Schizophrenia risk from complex variation of complement component 4. Nature. 2016;530:177–83.
Sellgren CM, Gracias J, Watmuff B, Biag JD, Thanos JM, Whittredge PB, et al. Increased synapse elimination by microglia in schizophrenia patient-derived models of synaptic pruning. Nat Neurosci. 2019;22:374–85.
Hall J, Bray NJ. Schizophrenia genomics: convergence on synaptic development, adult synaptic plasticity, or both? Biol Psychiatry. 2022;91:709–17.
Bastiaanssen TFS, Cowan CSM, Claesson MJ, Dinan TG, Cryan JF. Making sense of … the microbiome in psychiatry. Int J Neuropsychopharmacol. 2019;22:37–52.
Millan MJ, Andrieux A, Bartzokis G, Cadenhead K, Dazzan P, Fusar-Poli P, et al. Altering the course of schizophrenia: progress and perspectives. Nat Rev Drug Discov. 2016;15:485–515.
Pine DS, Fox NA. Childhood antecedents and risk for adult mental disorders. Annu Rev Psychol. 2015;66:459–85.
Acknowledgements
AF is supported by the Kjell and Märta Beijer Foundation. RB and SC are supported by the Swedish Research Council (Grant No. 2016-02362, 523–2014–3467).
Funding
Open access funding provided by Uppsala University.
Author information
Authors and Affiliations
Contributions
SC, AF, RB and ML all drafted the manuscript, revised it and approved the final version.
Corresponding author
Ethics declarations
Competing interests
ML is co-founder and part-time employee of Medtrace Pharma A/S. All other authors report no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cervenka, S., Frick, A., Bodén, R. et al. Application of positron emission tomography in psychiatry—methodological developments and future directions. Transl Psychiatry 12, 248 (2022). https://doi.org/10.1038/s41398-022-01990-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-022-01990-2
- Springer Nature Limited
This article is cited by
-
Challenges and rewards of in vivo synaptic density imaging, and its application to the study of depression
Neuropsychopharmacology (2024)
-
Nuclear psychiatric imaging: the trend of precise diagnosis for mental disorders
European Journal of Nuclear Medicine and Molecular Imaging (2024)
-
The Imageable Genome
Nature Communications (2023)
-
Feature engineering of EEG applied to mental disorders: a systematic mapping study
Applied Intelligence (2023)