Abstract
Study design/setting
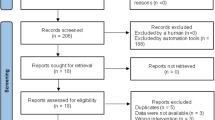
Secondary analysis.
Objectives
To compare the change in maximal inspiratory pressure (PImax) over the first 4 weeks of two different inspiratory muscle training (IMT) protocols and explore if either method is more effective for people with spinal cord injury.
Methods
Data originated from two published studies. Participants completed flow-resistive IMT (F-IMT) at 80% daily PImax, 7 days/week (supervised weekly), or threshold IMT (T-IMT) at 30–80% weekly PImax, twice-daily, 5 days/week (supervised every session). Seven participants from each trial were matched by training adherence, level of spinal cord injury, impairment grade (A–C), and height. Differences between F-IMT and T-IMT groups in training intensity, breaths taken, inspiratory work, and the change in the PImax from baseline at the end of week four were analysed.
Results
Over 4 weeks, there was no difference in the change in PImax between groups (Absolute change in PImax (cmH2O): p = 0.456, Percent change in PImax relative to baseline: p = 0.128). F-IMT participants trained at a higher intensity (median: 77 vs 22 cmH2O, p = 0.001 and 80% baseline vs 61% baseline, p = 0.038) but took fewer breaths (840 vs 1404 breaths, p = 0.017) than T-IMT participants. Inspiratory work was similar between groups (64,789 vs 65,910 (% PImax × number of breaths), p = 0.535).
Conclusions
Our findings support both methods of IMT as the change in PImax and inspiratory work were similar between groups. However, daily high-intensity F-IMT with intermittent supervision, required fewer breaths and less participant and therapist time. Future studies should examine optimal dosage and supervision required to achieve increased PImax.
Similar content being viewed by others
Introduction
Respiratory complications are a leading cause of morbidity and mortality for people with a spinal cord injury (SCI) [1]. Respiratory muscle weakness, which is a common sequela of the biomechanical and neurological changes associated with SCI [2], is predicted to be the primary cause of these respiratory complications [2]. One option to combat respiratory muscle weakness is respiratory muscle training (RMT). RMT encompasses interventions targeted to improve respiratory muscle strength and function including: inspiratory muscle training (IMT) [3, 4], expiratory muscle training (EMT) [5], combined IMT and EMT [6, 7], singing [8], breathing with abdominal weights [9], abdominal functional electrical stimulation [10], and iso- or normo-capnic hyperpnoea [11]. Two meta-analyses report significant positive effects of RMT for people with SCI [12, 13]. IMT protocols may be of greatest benefit because maximal inspiratory pressure (PImax) best predicts the risk of developing pneumonia during the initial rehabilitation stay[2] and improvements in PImax are associated with a decreased risk of experiencing a respiratory complication [7]. Despite the evidence, the clinical uptake of IMT protocols is still lacking and respiratory compromise remains a leading cause of disability and death in this population [1].
Multiple factors may limit the clinical translation of IMT protocols found in the literature. One such debated factor is the dose, or the work of breathing, completed by the trainee during the program [12, 13]. Traditionally, work of breathing is calculated by multiplying the pressure produced by the volume of air moved. For the purposes of IMT, where each breath is to total lung capacity, work is influenced by (1) training intensity, defined as either the raw pressure or the percent of baseline PImax reached during training, and (2) training volume, estimated by the number of breaths completed during the IMT program. Total training volume can be derived from the number of training days per week, the number of training sessions per day, the number of breaths per session and the volume of the breaths. Training frequencies of three to seven days per week are regularly reported, with recent trials reporting three to five training days weekly, but breaths per session and sessions per day vary [6, 7, 12,13,14]. The optimal IMT program has yet to be identified.
Another factor that limits clinical translation of IMT protocols is the varied types of IMT devices. Threshold resistance training (T-IMT) is the most widely reported mode of IMT used by people with SCI [12, 13]. Threshold devices contain a spring-loaded valve that opens to allow airflow when the trainee reaches the set pressure threshold during an inspiration. Flow-resistance training (F-IMT) devices have also been used to train people with SCI [3, 4]. F-IMT devices have small, fixed openings that create resistance as the trainee inspires. Faster inspiratory flow rates create greater pressure resistance in the F-IMT devices [15]. These two training modes have not been directly compared in the general population of people with SCI [16], leaving clinicians to guess which type of device is the most appropriate for their patients.
The clinical translation issues related to work and mode of IMT are compounded by the amount of supervision provided during trials and the lack of adherence reporting. Two studies investigating RMT in athletes with SCI did not provide fully supervised sessions and reported high adherence but these findings may not be generalizable to the non-athlete population [6, 17]. Most RMT studies provide fully supervised sessions which is not feasible in a community setting. Further, many trials report the target volume and intensity of IMT initially prescribed to participants but fail to report the actual adherence to those training variables. Neither of the recent meta-analyses of RMT in people with SCI report the adherence to the proposed protocols of included studies [12, 13]. To compare training programs or prescribe IMT clinically, clinicians and researchers need a better understanding of the inspiratory work that was achieved by participants in trials.
The current difficulties in between-trial comparison and the absence of program adherence data could limit RMT translation to clinical practice. A potential solution to these issues is to instead compare the actual inspiratory work that study participants complete; that is, the intensity of training based on either the absolute training pressure in cmH2O or the percent of baseline PImax at which breaths are performed multiplied by the total number of breaths completed. This exploratory secondary analysis compared two different IMT protocols based on the inspiratory work performed throughout training. The primary goal of these exploratory analyses was to identify a superior IMT program based on the change in PImax. Second, we compared training variables to identify factors that influence the efficacy of SCI-based IMT paradigms across two trials. Last, we investigated relationships between self-reported exertion and intensity; a significant relationship would aid clinicians when prescribing IMT without a PImax measurement. All exploratory analyses aimed to improve the clinical translation of IMT for people with SCI.
Methods
Study characteristics
Inspiratory muscle strength outcomes in two published original IMT studies in people with chronic SCI were compared. One study [4] used F-IMT (PrO2, PrO2Fit, Smithfield, RI, USA) and the second [7] used T-IMT (Threshold-IMT, Philips Respironics, Chichester, UK). Both studies had approval from affiliated human research ethics boards and were registered prior to trial commencement (NCT04210063; ANZCTR12612000929808). Informed written consent was obtained from participants prior to initiating study activities in accordance with the Declaration of Helsinki.
Both studies assessed maximal inspiratory pressure (PImax) at baseline prior to the start of IMT. The PrO2Fit was used to assess PImax in the F-IMT study from residual volume in a seated posture at baseline and each day that a participant trained. The Hyp’Air Pulmonary Function Test (Medisoft, Sorinnes, Belgium) was used to measure PImax from functional residual capacity in a seated posture at baseline while the MicroRPM (CareFusion, UK) was used to measure PImax weekly during the T-IMT study. In the F-IMT study 11 participants with chronic SCI completed F-IMT at 80% of a daily PImax for a target frequency of 7 days/week in their homes, supervised once weekly for 4–20 weeks, with variability in duration due to changes in the study protocol during the COVID-19 pandemic [4]. In the T- IMT study, 30 participants with acute SCI, and 32 participants with chronic SCI completed 2 daily supervised T-IMT sessions in the hospital (participants with acute SCI) or in their homes (participants with chronic SCI, >1 year duration of injury) 5 days/week for 6 weeks [7]. The T-IMT group trained at 30–80% PImax assessed at the start of each week. Inclusion and exclusion criteria and training protocols for each study are shown in Table 1. In both studies, participants were instructed to train with breaths to total lung capacity (TLC).
Seven of the 11 participants in the F-IMT study had chronic tetraplegia and were matched with active IMT participants with chronic SCI in the T-IMT trial by neurologic level of injury (and motor level or zone of partial preservation), AIS grade, height, and training adherence (% target sessions completed; Table 2). Complete data were available for all 14 participants for 4 weeks. Therefore, comparisons of the training protocols were made for the first 4 weeks of training.
Outcome measures
The following variables were calculated for each study group over 4 weeks of training: median Intensity of IMT (Intensity-absolute (PI in cmH2O) and Intensity-% (%PImax, PI normalized to baseline PImax)); the number of training breaths completed (#Breaths); and the calculated inspiratory work done (Work-absolute = Intensity-absolute × #Breaths and Work-% = Intensity-% × #Breaths). Adherence was calculated from the number of sessions completed/number of sessions prescribed in each protocol. Perceived effort, or rate of perceived exertion (RPE), during training was measured using the modified Borg Scale in the T-IMT trial and a 0 to 10 visual analog scale (0- not difficult to 10- the most difficult) in the F-IMT trial, and the medians were reported. Modified Borg Scale scores have been reported to have a linear relationship to the VAS (slope of 0.98) when used to measure dyspnea during arm crank activity [18], thus, a direct comparison of the RPE scores from the two IMT protocols was used.
At the end of 4 weeks of training, we measured post-IMT inspiratory muscle strength and calculated the change in absolute PImax (ΔPImax, PImax after 4 weeks training minus PImax at baseline), change in PImax normalized to baseline PImax (%ΔPImax). We calculated the predicted change in absolute PImax. The predicted change in absolute PImax was calculated based on the model from Raab et al.: Expected PImax change (cmH2O) = [7 × (absolute PImax at baseline/100)] × [(Median Intensity-%)/10] [19]. We also calculated the proportion of the expected ΔPImax represented by the actual ΔPImax.
Data and statistical analysis
Medians (IQ ranges) were calculated for baseline characteristics such as age, weight, duration of injury, and baseline PImax, as well as training related variables from the data of each participant in both groups. Mann–Whitney U tests were used to analyze between group differences for all baseline measures and all outcomes (mannwhitneyu from scipy.stats in Python v. 3.9.7). Exploratory Spearman Correlations were used to analyze relationships among work-absolute, work-%, ΔPImax, and %ΔPImax across groups to further recognize factors that may impact protocol efficacy (spearmanr from scipy.stats in Python v. 3.9.7). Additional exploratory analyses included investigating the relationship between RPE and either Intensity-absolute or Intensity-% of the IMT. Significance was set at p < 0.05. No a priori power analysis was completed as this was an exploratory secondary analysis of a subset of previously published data from two studies. We did not perform Bonferroni corrections due to the exploratory nature of the study and the small sample.
Results
Descriptive characteristics of the 14 participants selected for the matched data comparison are shown in Table 3. Characteristics used as criteria for matching did not differ significantly between groups (height or adherence), however people in the F-IMT group were younger (p = 0.002), had a shorter duration of injury (p = 0.002), weighed less (p = 0.030), and had a higher PImax (p = 0.041) at baseline than the T-IMT group (Table 3). Further descriptive information about the overall trial samples can be found in the original publications [4, 7].
After 4 weeks of IMT the PImax increased from baseline for both groups by a mean of 17.0 (95% CI: 5.2–28.9) and 24.7 (10.1–39.3) for the F-IMT and T-IMT groups, respectively (right panel Fig. 1A). However, no between-group difference was found in the absolute ΔPImax or %ΔPImax relative to baseline (p = 0.456 and p = 0.128, Table 4 and Fig. 1B). The PImax of the two groups was not significantly different after training (p = 0.073), although it was half the size in the T-IMT group. Interestingly, the actual ΔPImax as a proportion of the expected ΔPImax was lower in the F-IMT group compared to the T-IMT group (p = 0.026, Table 4).
A Individual absolute PImax (cmH2O) at baseline and after 4 weeks of IMT and (B) individual %ΔPImax (relative to baseline PImax) from the Flow-Inspiratory Muscle Training (F-IMT, solid lines, and solid markers) and Threshold-Inspiratory Muscle Training (T-IMT, dashed lines and open markers) groups (n = 7 in each group). Matched participants are represented by the same marker shape. The mean group changes and 95% confidence intervals are shown on the right of each panel for ΔPImax in (A) and %ΔPImax in (B). The 95% Confidence Intervals (95%CI) overlap between groups but do not overlap 0 cmH2O or 0%.
There was no significant difference between groups for Work-% performed over the 4-weeks, although Work-absolute was higher in the F-IMT group due to the higher baseline PImax used to calculate Intensity-absolute (Tables 3 and 4). Spearman correlations found a significant positive relationship between Work-% and % ΔPImax (rho = 0.665, p = 0.013) but not absolute ΔPImax (rho = 0.429, p = 0.114) (Fig. 2, panels B and A, respectively). RPE had a significant positive relationship to both training Intensity-absolute (rho = 0.786, p = 0.001) and Intensity-% (rho = 0.577, p = 0.039) (Fig. 3, panels A and B, respectively).
Correlations between Work-% (calculated by multiplying the number of training breaths completed by the intensity of training as a percent of baseline maximal inspiratory pressure (PImax)) and (A) absolute change in PImax (ΔPImax, cmH2O) and (B) %ΔPImax, (%ΔPImax relative to baseline PImax). Participants in the Flow-Inspiratory Muscle Training (F-IMT) group (n = 7) are represented by solid markers while participants in the Threshold-Inspiratory Muscle Training (T-IMT) group (n = 7) are represented open markers. Matched pairs are plotted in the same marker shape. p < 0.05 indicates significant correlation.
Correlations between rate of perceived exertion (RPE) and (A) Intensity-Absolute and (B) Intensity-% (calculated as a percent of baseline maximal inspiratory pressure). Participants in the Flow-Inspiratory Muscle Training (F-IMT) group (n = 6, one person was not compliant with RPE reporting) are represented by solid markers while participants in the Threshold-Inspiratory Muscle Training (T-IMT) group (n = 7) are represented by open markers. Matched pairs are plotted in the same marker shape. p < 0.05 indicates significant correlation.
Discussion
This is the first analysis to compare the efficacy of two IMT protocols that used different devices and training programs in the general population of people with chronic tetraplegia. While both training protocols improved PImax after 4 weeks of training, the findings of this secondary analysis do not identify a superior IMT protocol based on ΔPImax or %ΔPImax. However, the findings do identify factors that may impact overall IMT protocol efficiency and show relationships that are clinically important. We found a positive correlation between Work-% performed and %ΔPImax, regardless of the device or protocol used. The Work-based findings are evidence that the Work-% construct may be used when comparing IMT protocols. Further, the relationship between perceived exertion and intensity of training may help clinicians grade IMT training intensity in the absence of facilities to assess inspiratory pressure or PImax.
After 4 weeks training, no group difference was found in %ΔPImax or ΔPImax, despite the large difference in PImax between the F-IMT and T-IMT groups at baseline, where the PImax of the F-IMT group was more than three times that of the T-IMT group. However, the post-intervention PImax, ΔPImax and %ΔPImax, although not different between groups, in the F-IMT group were 1.8, 0.6, and 0.4 times the median values for the T-IMT group, respectively. The lack of significant differences may be due to the low numbers of participants included in the comparison analysis, as well as large inter-participant variability in PImax resulting in an underpowered analysis and possible Type 2 error. Similar to our current findings in SCI, IMT training in people with chronic obstructive pulmonary disease (COPD) increased PImax, but with no difference in ΔPImax after F-IMT compared to T-IMT [15]. Additionally, between group differences in ΔPImax were not found in a study investigating T-IMT vs F-IMT vs no IMT in elite rugby athletes, most of whom had SCI [16]. However, it is unclear whether a significant increase in PImax occurred within groups based on the analyses reported and the small numbers in each group (T-IMT group, n = 4; F-IMT group, n = 5; no IMT control group, n = 7)[16]. Therefore, while IMT in either form can increase PImax, further research is needed to identify if there is an optimal mode of training or training protocol for each diagnostic population.
The similar improvements in ΔPImax or %ΔPImax across F-IMT and T-IMT in the current study suggest that supervision of every training session may not be mandatory in every case to obtain positive results. All IMT sessions were supervised in the T-IMT group, while only one session per week was supervised in the F-IMT group. There are financial, transportation, and staffing barriers that may limit the clinical translation of fully supervised training protocols [20, 21]. However, supervision may be required for individuals with hand function impairments if adaptations are not available to allow for independent use of devices. Some form of clinical supervision is likely beneficial even for individuals with the ability to perform IMT independently or with assistance from a carer. Both the original F-IMT and T-IMT studies included follow-up phases where no supervision was provided. During the non-supervised phase, only 1 of 3 active participants (33%) and 16 of 62 participants (26%) continued to train in the F-IMT and T-IMT studies, respectively [4, 7]. No supervision seems to be detrimental to continued training after an exposure to supervised IMT in people with SCI. Similarly, a meta-analysis investigated the impact of supervision on adherence of people with non-neurologic chronic disease during follow-up exercise programs after participants had completed a 4–6 week supervised exercise program [22]. A pooled and weighted analysis of two studies found the proportion of people who were “partially adherent” to a home exercise program without any supervision was low (29%). This reported proportion is very similar to the unsupervised adherence rates reported by the studies included in this secondary analysis [4, 7, 22]. Future studies should continue to investigate supervision models, including remote supervision, that are sustainable and tailored to the individual abilities of people with SCI and clinicians, more importantly so in the era of telehealth consultations and treatments.
Beyond supervision, other training factors differed between the F-IMT and T-IMT groups including a higher number of breaths (#Breaths) taken in the T-IMT group with a lower training intensity. Overall, these differences did not result in significantly different ΔPImax or %ΔPImax outcomes in the current study. Raab et al. have reported on the predictive relationship of training Intensity-% and ΔPImax in a retrospective study of an inpatient cohort (n = 67) with SCI ranging from C4-T12 levels of injury (AIS A-D) [19]. They found that median training Intensity-% and PImax at baseline, but not #Breaths, were predictive of the ΔPImax after a median of 6 weeks (interquartile range of 5–8 weeks) of training [19]. The expected ΔPImax for each group in the current study (based on the Raab et al (2019) equation) indicated that the T-IMT group performed much better than expected (167%) while the F-IMT group performed much worse than expected (26%) [19]. These differences from expected changes in each group raise doubt about the utility of this predictive equation. The equation may be inaccurate when comparing community dwelling individuals with variable injury characteristics, training devices, protocols including number of sessions, intensities of training, duration of training and levels of supervision. Our limited data cannot determine the utility of the equation and variability of sample and training factors is not accounted for in previous meta-analyses [12, 13].
Across all 14 participants in the current study, there was a strong positive correlation between Work-% (calculated from #Breaths × Intensity-%) and %ΔPImax, regardless of the training paradigm. Work was not included in the model by Raab et al. [19] despite work being a predictor of increased strength in limb resistance training [23, 24]. However, work is not commonly reported in IMT trials [12, 13], and in the current study, we have calculated work relative to baseline PImax across the first 4 weeks of training only. The relationship of Work-% and %ΔPImax is unknown beyond this. Nevertheless, the strong correlation suggests that higher levels of work produce higher %ΔPImax even if the Intensity-% of training is reduced and the #Breaths is increased to compensate. This occurred for the T-IMT group, in which the Intensity of training relative to baseline (Intensity-%) was 30% of that for the F-IMT group. The calculation of work relative to PImax at baseline (Work-%) could allow comparison of the impact of different IMT protocols to a common outcome (%ΔPImax) and may offer a more complete analysis of the effect of IMT on respiratory function in people with SCI. Future studies could report Work-% to improve between-protocol comparison and translation to clinical practice as well as allow for tailored approaches to IMT.
The data from the current study also showed that across both groups, training intensity (both Intensity-% and Intensity-absolute) are positively correlated with RPE, a measure of the effort required to do the training. Similar relationships between effort and pressure have been reported previously in able-bodied people [25], people with COPD with and without anxiety [26], and people with chronic tetraplegia [27]. Further, a meta-analysis reported that peak oxygen uptake and peak power output improve when individuals with SCI complete perceptually regulated exercise protocols [28]. Although IMT protocols were not included in that meta-analysis, our findings support that perceptually regulated IMT may be effective at determining the dose for intensity of IMT via RPE scores since a respiratory pressure meter is not always available in clinical settings. Clinicians may be able to prescribe the Intensity-% of IMT based on RPE; for example, from our limited data in Fig. 3, training at an RPE of 5 is likely to represent a training intensity of at least 65% PImax. The relationship between Intensity% and RPE suggests that individuals with tetraplegia can generally perceive the intensity at which they are performing IMT and warrants further investigation to confirm.
The introduction of the Work-% variable, calculated from training Intensity-% and #Breaths, and the recognition of the correlation between perceived exertion and training intensity are clinically important and should be considered in future research. However, this secondary analysis is limited by its small sample size (and low power) and the existing baseline differences in study participant groups. In general, the participants in the F-IMT study were younger and had a shorter injury duration than participants in the T-IMT groups. Older age and longer injury duration are related to poorer respiratory function [29,30,31] which may have contributed to the lower average baseline PImax of participants in the T-IMT study. The higher baseline PImax of the F-IMT group may have resulted in a ceiling effect in ΔPImax.
Conclusion
This novel secondary analysis compared outcomes from F-IMT and T-IMT protocols in individuals with chronic tetraplegia. Both the protocols elicited similar improvements in PImax after 4 weeks of training and therefore, the most efficacious protocol could not be determined. This may be due to significant differences between groups in PImax at baseline and a relatively small sample size. However, the findings suggest that in-person supervision may not be required for all IMT sessions. The positive correlation between perceived effort and training Intensity-absolute and Intensity-%, support the use of perceived effort as a potential surrogate for Intensity-% when clinicians prescribe IMT without the ability to monitor inspiratory pressure or PImax. This prescriptive relationship is especially important since Work-% is derived from Intensity-% and increased Work-% was related to increased PImax after 4 weeks. Measurement of Work-% may be used in future research or clinical practice to help researchers and clinicians to compare IMT protocols and to determine the best options for people with SCI. We recommend that future IMT clinical trials should report adherence and Work-%, where possible, to improve generalizability and comparisons between protocols.
Data availability
Data use requests in line with the ethical approval of the initial studies submitted to the corresponding author will be considered for approval.
References
DeVivo MJ, Chen Y, Wen H. Cause of death trends among persons with spinal cord injury in the united states: 1960-2017. Arch Phys Med Rehabilit. 2021;103:634–41.
Raab AM, Krebs J, Perret C, Michel F, Hopman MT, Mueller G. Maximum inspiratory pressure is a discriminator of pneumonia in individuals with spinal-cord injury. Respir Care. 2016;61:1636–43.
McDonald T, Stiller K. Inspiratory muscle training is feasible and safe for patients with acute spinal cord injury. J Spinal Cord Med. 2019;42:220–7.
Palermo AE, Nash MS, Kirk-Sanchez NJ, Cahalin LP. Adherence to and impact of home-based high-intensity IMT in people with spinal cord injury: a pilot study. Spinal Cord Ser Cases. 2022;8:85.
Roth EJ, Stenson KW, Powley S, Oken J, Primack S, Nussbaum SB, et al. Expiratory muscle training in spinal cord injury: a randomized controlled trial. Arch Phys Med Rehabilit. 2010;91:857–61.
Gee CM, Williams AM, Sheel AW, Eves ND, West CR. Respiratory muscle training in athletes with cervical spinal cord injury: effects on cardiopulmonary function and exercise capacity. J Physiol. 2019;597:3673–85.
Boswell-Ruys CL, Lewis CRH, Wijeysuriya NS, McBain RA, Lee BB, McKenzie DK, et al. Impact of respiratory muscle training on respiratory muscle strength, respiratory function and quality of life in individuals with tetraplegia: a randomised clinical trial. Thorax. 2020;75:279–88.
Zhang XY, Yu WY, Teng WJ, Song YC, Yang DG, Liu HW, et al. Effect of vocal respiratory training on respiratory function and respiratory neural plasticity in patients with cervical spinal cord injury: a randomized controlled trial. Neural Regen Res. 2022;17:1065–71.
Derrickson J, Ciesla N, Simpson N, Imle PC. A comparison of two breathing exercise programs for patients with quadriplegia. Phys Ther. 1992;72:763–9.
McCaughey EJ, Borotkanics RJ, Gollee H, Folz RJ, McLachlan AJ. Abdominal functional electrical stimulation to improve respiratory function after spinal cord injury: a systematic review and meta-analysis. Spinal Cord. 2017;55:798.
Mueller G, Hopman MT, Perret C. Comparison of respiratory muscle training methods in individuals with motor and sensory complete tetraplegia: a randomized controlled trial. J Rehabil Med. 2013;45:248–53.
Tamplin J, Berlowitz DJ. A systematic review and meta-analysis of the effects of respiratory muscle training on pulmonary function in tetraplegia. Spinal Cord. 2014;52:175–80.
Wang X, Zhang N, Xu Y. Effects of respiratory muscle training on pulmonary function in individuals with spinal cord injury: an updated meta-analysis. Biomed Res Int. 2020;2020:7530498.
Soumyashree S, Kaur J. Effect of inspiratory muscle training (IMT) on aerobic capacity, respiratory muscle strength and rate of perceived exertion in paraplegics. J Spinal Cord Med. 2020;43:53–9.
Madariaga VB, Iturri JB, Manterola AG, Buey JC, Sebastian NT, Pena VS. Comparison of 2 methods for inspiratory muscle training in patients with chronic obstructive pulmonary disease. Arch Bronconeumol. 2007;43:431–8.
Litchke LG, Lloyd LK, Schmidt EA, Russian CJ, Reardon RF. Comparison of two concurrent respiratory resistance devices on pulmonary function and time trial performance of wheel chair athletes. Ther Recreat J. 2010;44:51–62.
West CR, Taylor BJ, Campbell IG, Romer LM. Effects of inspiratory muscle training on exercise responses in paralympic athletes with cervical spinal cord injury. Scand J Med Sci Sports. 2014;24:764–72.
Capodaglio EM. Comparison between the CR10 Borg’s scale and the VAS (visual analogue scale) during an arm-cranking exercise. J Occup Rehabilit. 2001;11:69–74.
Raab AM, Krebs J, Pfister M, Perret C, Hopman M, Mueller G. Respiratory muscle training in individuals with spinal cord injury: effect of training intensity and -volume on improvements in respiratory muscle strength. Spinal Cord. 2019;57:482–9.
Frasunska J, Wojdasiewicz P, Tederko P, Wasiak K, Tarnacka B. Adherence to prescriptions of therapeutic exercises in patients with traumatic spinal cord injury. Ann Agric Environ Med. 2021;28:331–8.
Stillman MD, Frost KL, Smalley C, Bertocci G, Williams S. Health care utilization and barriers experienced by individuals with spinal cord injury. Arch Phys Med Rehabilit. 2014;95:1114–26.
Jansons PS, Haines TP, O’Brien L. Interventions to achieve ongoing exercise adherence for adults with chronic health conditions who have completed a supervised exercise program: systematic review and meta-analysis. Clin Rehabilit. 2016;31:465–77.
Krieger JW. Single vs. multiple sets of resistance exercise for muscle hypertrophy: a meta-analysis. J Strength Cond. Res. 2010;24:1150–9.
Schoenfeld BJ, Ogborn D, Krieger JW. Dose-response relationship between weekly resistance training volume and increases in muscle mass: a systematic review and meta-analysis. J Sports Sci. 2017;35:1073–82.
Killian KJ, Bucens DD, Campbell EJ. Effect of breathing patterns on the perceived magnitude of added loads to breathing. J Appl Physiol Respir Environ Exerc Physiol. 1982;52:578–84.
Livermore N, Butler JE, Sharpe L, McBain RA, Gandevia SC, McKenzie DK. Panic attacks and perception of inspiratory resistive loads in chronic obstructive pulmonary disease.Am J Resp Crit Care. 2008;178:7–12.
Luu BL, Lewis RHC, Gandevia SC, Boswell-Ruys CL, Butler JE. The detection and sensory perception of inspiratory resistive loads in people with chronic tetraplegia. J Appl Physiol. 2022;133:1192–201.
Valentino SE, Hutchinson MJ, Goosey-Tolfrey VL, MacDonald MJ. Effects of perceptually regulated exercise training on cardiorespiratory fitness and peak power output in adults with spinal cord injury: a systematic review and meta-analysis. Arch Phys Med Rehabilit. 2022;103:1398–409.
Sharma G, Goodwin J. Effect of aging on respiratory system physiology and immunology. Clin Interv Aging. 2006;1:253–60.
Pili R, Gaviano L, Pili L, Petretto DR. Ageing, disability, and spinal cord injury: some issues of analysis. Curr Gerontol Geriatr Res. 2018;2018:4017858.
Linn WS, Adkins RH, Gong H, Waters RL. Pulmonary function in chronic spinal cord injury: a cross-sectional survey of 222 Southern California adult outpatients. Arch Phys Med Rehabilit. 2000;81:757–63.
Acknowledgements
The authors would like to acknowledge Dr Georgia Fisher, PhD and Dr Euan McCaughey for their efforts in the preparation of this manuscript.
Funding
One of the original studies was funded by the Foundation for Physical Therapy Research through a PODS II Award. The other original study was completed with support from the National Health and Medical Research Council and the Prince of Wales Hospital Foundation. Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
AEP and CLB-R initiated the secondary analysis with input from JEB. AEP completed the analyses, drafted the manuscript and prepared it for submission. CLB-R and JEB provided feedback and edits on the analyses and manuscript. All authors provided final approval of the manuscript prior to submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Palermo, A.E., Butler, J.E. & Boswell-Ruys, C.L. Comparison of two inspiratory muscle training protocols in people with spinal cord injury: a secondary analysis. Spinal Cord Ser Cases 9, 42 (2023). https://doi.org/10.1038/s41394-023-00594-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-023-00594-2
- Springer Nature Limited