Abstract
Introduction
Extradural spinal hemangiomas without vertebral body or intradural involvement are rare and often misdiagnosed. When present in the lumbar spine, they typically present with radiculopathy and weakness. CT imaging is helpful in assessing for bony involvement and temporal involvement while MRI imaging can be helpful in distinguishing hemangiomas from other mass lesions, however current reports on imaging features are limited. Diagnosis remains primarily dependent on tissue pathology with surgery as the mainstay of treatment.
Case presentation
We present a unique case report in which we obtain additional DSA imaging to not only visualize the vascular anatomy associated with a L4-5 neuroforaminal capillary hemangioma involving the L4 nerve root and ganglion, but to also embolize the feeding artery prior to surgical resection. Patient initially underwent a CT-guided biopsy that was suspicious for a hemangioma and confirmed on final pathology to be the capillary subtype.
Discussion
When diagnosed appropriately, patients avoid unnecessary additional testing and avoid erroneous treatment of this rare lesion. Based on our experience, we propose initial MRI imaging to characterize the hemangioma and evaluate for intradural involvement, DSA to assess vascularity followed by embolization of the lesion when able in order to minimize intra-operative hemorrhage risk, and ultimately surgery to achieve a gross total resection.
Similar content being viewed by others
Introduction
Hemangiomas are benign vascular lesions that rarely present in the nervous system; however, when the spinal column is involved, they are typically located in the vertebral body [1]. Hemangiomas located in the extradural space without vertebral body or intradural involvement are very rare and make up only <6% of all extradural spinal tumors, with less than 20 cases reported in the literature thus far [2,3,4]. Extradural hemangiomas within the spine are typically cavernous hemangioma, angiolipoma, and arteriovenous hemangioma [4], with only 8% of spinal hemangiomas of the capillary subtype [5]. Occurrence in the lumbar spine is rare as nerve roots are able to tolerate compression more than the spinal cord [6]; however, patients can present with symptoms similar to that of other tumors located in the lumbar spine, such as radiculopathy and weakness [7]. Given its low incidence, extradural hemangiomas are not typically considered in the differential and often misdiagnosed. We present a unique case of an extradural lumbar nerve root capillary hemangioma extending through the neural foramina with ganglion involvement. We first embolized the mass prior to surgical resection, which has not yet been documented in the literature. In this paper, we review the imaging and histopathological findings instrumental in the diagnosis and treatment of this tumor.
Case presentation
Patient is a 20-year-old male with no past medical history of tumors or malignancies who presented for evaluation of low back pain with radiculopathy into the left lower extremity posteriorly down to the calf and anteriorly into the thigh in L4 and L5 distribution. On neurologic exam, patient demonstrated trace weakness in left knee extension, but otherwise full strength in all remaining lower extremity muscle groups bilaterally. Patient had no sensory deficits.
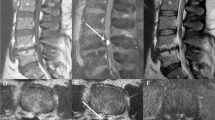
MR imaging demonstrated a well-circumscribed T1 isointense, T2 high signal intensity (Fig. 1A, B), homogenously enhancing (Fig. 2A–C) mass at the L4-5 level. In addition to compression of the thecal sac, the lesion extended laterally from the left neural foramina into the soft tissue space with L4 nerve root compression. CT of the lumbar spine re-demonstrated an extramedullary extradural lesion within the left L4-5 neural foramina and extending into the adjacent paraspinal and psoas muscles. CT showed no bony involvement of the lesion but expansion of the neuroforamen (Fig. 3). This expansion of the neuroforamen indicates a slow-growing lesion.
MRI of the lumbar spine T1 with gadolinium contrast showing a large enhancing mass located in the left L4–5 neural foraminal space that extends into the paraspinal muscles and soft tissue space posteriorly that can be seen on A axial, B midline sagittal, and C lateral sagittal T1 with contrast sequences.
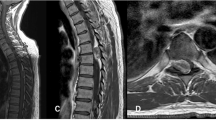
Patient initially underwent minimally invasive CT-guided biopsy of the lesion, which preliminarily revealed a benign vascular lesion that was suspicious for hemangioma. Subsequently, patient underwent a digital subtraction angiography (DSA) of the spine which demonstrated the vasculature of this lesion more fully. An enlarged left L4 lumbar segmental artery was visualized with multiple feeders in the region of the L4 nerve root and known tumor. The right lumbar segmental artery was of slightly increased caliber but did not feed the left-sided tumor. No additional arteries were noted to be filling the tumor. A Mickelson catheter followed by a Prowler microcatheter and Headliner microwire was used to enter the left L4 lumbar segmental artery to embolize the tumor with a total of 3 milliliters of N-Butyl Cyanoacrylate (NBCA) glue and ethiodol with the goal of minimizing intra-operative blood loss. Follow-up angiography demonstrated penetration of the embolysate into the tumor with a significant decrease in vascularity of the tumor (Fig. 4A, B). However, the definitive treatment at present remains surgical resection; given the suspected proangiogenic nature of hemangiomas, complete tumor removal is desired in order to prevent further growth and neural involvement. As patient was also symptomatic at the time of presentation, patient agreed to proceed with surgical intervention.
Patient underwent a complete L4 laminectomy, partial L3 laminectomy, and left-sided L4-5 facetectomy to expose the tumor and decompress the thecal sac. An ultrasound was used to evaluate for an intradural component, which revealed free nerve roots within. Laterally, the nerve roots were visualized, and the tumor was noted to be integrated into the exiting L4 nerve root with strong adherence to the dural sheath. Neuromonitoring and direct stimulation were utilized to determine the lesion was coming off a functional nerve root. As the tumor could not be separated without sacrifice of the nerve root, the tumor was maximally debulked rather than fully resected given the benign nature of the lesion. Although the tumor tissue still bled during resection, bleeding was easily controllable and total blood loss remained only 300 mL. Pedicle screws were placed bilaterally at L4 and L5 and connected with rods to obtain fusion for stability. No complications were encountered intra-operatively. Post-operatively, the patient’s minimal proximal left leg weakness remained stable however his radicular pain was improved. By time of discharge on postoperative day 3, patient’s proximal left leg weakness had improved.
Final pathology confirmed the diagnosis of hemangioma. Sections of the biopsy and resection specimens revealed benign hemangioma dominated by closely packed capillary proliferation involving peripheral nerve and ganglion and consistent with capillary hemangioma. Figure 6 and 7 demonstrate the histopathologic and immunohistochemical features of the resection specimen. Capillaries in the lesion were lined by a single layer of endothelial cells, lacked atypia, and were uniformly bland. The lesion involved the peripheral nerve and ganglion parenchyma including numerous ganglion cells (Fig. 5A, B). The morphological findings described were further supported by the immunohistochemical profile of the lesion with blood vessels demonstrating immunopositivity for CD31, CD34, and SMA (Fig. 6A–C). Peripheral nerve and ganglion parenchyma were highlighted by S100, neurofilament, and synaptophysin immunohistochemical stains (Fig. 6A–C).
The patient was scheduled for follow-up imaging to evaluate residual tumor and/or growth, however, he was unfortunately lost to follow-up and post-operative imaging is not available.
Discussion
Capillary hemangiomas are uncommonly found within the neuro-axis; most of the extraosseous spinal cases that have been reported are located in the intradural space. Capillary hemangiomas with an intradural component can be difficult to differentiate from other spinal lesions, such as meningiomas or neuromas if serpiginous retromedullary regions of signal void are not present [8]. Extradural capillary hemangiomas with nerve root and ganglion involvement are extremely rare, and even more likely to be misdiagnosed and mistreated due to its low incidence, consideration, and familiarity. Imaging alone may not be sufficient for diagnosis as current reports on CT and MR features of lumbar hemangiomas without direct bone involvement are limited [9]; thus, tissue pathology is key. MR imaging can still be helpful in distinguishing vascular from non-vascular lesions as differential diagnoses can include epidural tumor, such as Schwannoma or neurofibroma; epidural abscess; epidural cyst; and free-fragment herniated disc. The natural course of extradural capillary hemangiomas is still unclear as diagnoses are often made post-operatively based on pathology and typically treated surgically once diagnosed. Definitive differentiation of hemangioma from other vascular spinal cord tumors, such as hemangioblastoma and hemangiopericytoma, requires histological evaluation [10, 11].
Preoperative diagnosis is important as surgical resection is the only treatment and intraoperative hemorrhage is a risk; no cases reported in the literature thus far have had an accurate preliminary diagnosis of hemangioma. Our case demonstrates that a minimally invasive biopsy for tissue sampling may be a helpful additional step when formulating treatment plans for spinal lesions that are indeterminate based on imaging. By performing a biopsy prior to resection, the preliminary diagnosis allowed us to individualize our interventions to incorporate preoperative angiography and embolization to minimize our perioperative surgical risk. There are currently no reports in the literature studying the use of DSA to understand the vasculature of hemangiomas. While some authors state that DSA has no role in diagnosis with the argument that epidural hemangiomas do not communicate with the spinal arterial circulation and are angiographically occult [12], our case supports the use of DSA to not only visualize the vascular relationship between the lesion and spinal vasculature but to also reduce the risk of significant intraoperative blood loss. In our case, DSA served the dual purposes of both diagnosing and treating the lesion with embolization. The preliminary results of the biopsy also guided our level of aggressiveness in resection based on the benign nature of the lesion and risk of achieving total resection with nerve root sacrifice. Available case reports all describe total resection when possible; however, limited data is currently available on long-term follow-up recommendations after either total or partially resected lesions. Recurrence is possible given the propangiogenic features of hemangiomas, however, the rate of recurrence is unknown; given the patient’s young age and minimal neurologic deficit at time of presentation, the risk of new neurologic deficit was weighed against total resection.
Although rare, hemangiomas should be considered in the differential diagnosis of a spinal epidural soft tissue masses as treatment can be definitive. When diagnosed appropriately, patients avoid unnecessary additional testing and avoid erroneous treatment. We propose initial MRI imaging to characterize the hemangioma and evaluate for intradural involvement, DSA to assess vascularity, followed by embolization of the lesion when able to minimize intra-operative hemorrhage risk, and ultimately surgery to achieve total resection.
References
Ciftdemir M, Kaya M, Selcuk E, Yalniz E. Tumors of the spine. World J Orthop. 2016;7:109–16.
Sağlam D, Sari A, Cansu A. Spinal epidural cavernous hemangioma: a rare site of involvement. Spine J. 2016;251.
Padovani R, Tognetti F, Proietti D, Pozzati D, Servadei F. Extrathecal cavernous hemangioma. Surg Neurol. 1982;18:463–5.
Rovira A, Rovira A, Capellades J, Zauner M, Bella R, Rovira M. Lumbar extradural hemangiomas: report of three cases. J Neurorad. 1999;20:27–31.
Tunthanathip T, Rattanalert S, Oearsakul T, Kanjanapradit K. Spinal capillary hemangiomas: two cases reports and review of the literature. Asian J Neurosurg. 2017;12(Jul-Sept):556–62.
Lim WJ, Hur JW, Ahn SY, Rhee JJ, Lee JW, Lee HK. Pure spinal epiudural cavernous hemangioma: a case report. Nerve. 2016;2:87–9.
Nowak DA, Widenka DC. Spinal intradural capillary haemangioma: a review. Eur Spine J. 2001;10:464–72.
Vilanova JC, Barcelo J, Smirniotopoulos JG, Perez-Andres R, Villalon M, Miro J, Ferran M, Capellades J, Ros PR. Hemangioma from head to toe: MR imaging with pathologic correlation. Radiographics. 2004;24:367–85.
Roncaroli F, Scheithauer BW, Krauss WE. Hemangioma of spinal nerve root. J Neurosurg Spine. 1999;91:175–80.
Roncaroli F, Scheithauer BW, Krauss WE. Capillary hemangioma of the spinal cord: report of four cases. J Neurosurg. 2000;93:148–51.
Sulochana S, Sundaram M. Cavernous hemangioma of the spinal cord: a rare case. J Clin Diagn Res. 2012;6:1781–2.
Sanghvi D, Munshi M, Kulkarni B, Kumar A. Dorsal spinal epidural cavernous hemangioma. J Craniovertebr Junction Spine. 2010;1:122–5.
Acknowledgements
This article was made possible with the support of Dr. Ankit Mehta who performed the surgery and guided us on the importance of this rare pathology; Drs. Sophia Peng and Laura S. McGuire who researched for and compiled this article; Drs. Tibor Valyi-Nagy and Karimi Saman provided the background in Pathology that was essential in our diagnosis and treatment; and Drs. Ali Alaraj and Jason Choi who performed the diagnostic cerebral angiogram and embolization.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Peng, S., McGuire, L.S., Saman, K. et al. Extradural lumbar nerve root and ganglion capillary hemangioma: case report. Spinal Cord Ser Cases 7, 74 (2021). https://doi.org/10.1038/s41394-021-00438-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00438-x
- Springer Nature Limited