Abstract
Study design
Retrospective cohort study.
Objective
In this pilot study, we aimed to assess the incidence, diagnostic strategies, treatment regimens, and outcomes of pyogenic vertebral osteomyelitis (PVO), in a non-urban, Northern European population during 1 year.
Setting
Region Zealand, Denmark.
Methods
All patients admitted to a hospital in Region Zealand during 2013 and subsequently discharged with a diagnosis of PVO or discitis were eligible for screening. Discharge diagnosis codes were obtained from a central register and patients were identified with unique identification numbers from the Danish Civil Registration System.
Results
Forty-one consecutive patients were included. Patients presented with back pain (78%), fever (76%), elevated C-reactive protein levels (95%), and bacteremia (76%). Nine patients (22%) were treated empirically, as no bacterial etiology was isolated from blood culture or biopsy. The median duration of antibiotic treatment was 92 days, and we report an in-hospital mortality of 15%.
Conclusions
This study supports previous findings of increasing incidence of PVO. In addition, we found a high rate of bacteremia and a high mortality in this single year cohort. Treatment regimens were heterogeneous and prolonged, due to delayed diagnosis and various or unknown microbial etiology. The study suggests that back pain, fever, and increased C-reactive protein levels are frequent in patients with PVO, and efforts should be made on securing early diagnosis and microbial etiology. Further studies of predictors of different clinical outcomes are warranted. Treatment of culture-negative cases and clinical value of bone biopsies are of special interest.
Similar content being viewed by others
Introduction
Pyogenic vertebral osteomyelitis (PVO) is a rare yet severe condition, involving bacterial infection of one or more vertebrae. Frequently, the adjacent intervertebral disc space is involved, a condition known as discitis, and the combined condition often referred to as spondylodiscitis. Infections most often occur from hematogenous spread, while other possible routes are direct inoculation from trauma or surgery, or contiguous spread from adjacent tissue. The incidence is increasing, probably due to improved diagnostics, increased life expectancy, and increased use of instrumentation and catheterization during hospital stays [1,2,3,4].
Symptoms are often non-specific and diagnosis is often delayed. To minimize the risk of complications, awareness of the condition is important for clinicians working in several areas of spinal cord medicine, including the rehabilitation area where post-operative cases or relapses should not be missed. When vertebral osteomyelitis is suspected, current guidelines suggest a diagnostic approach based on laboratory studies, blood cultures, and magnetic resonance imaging (MRI) [5]. Positron emission tomography/computed tomography (PET-CT) is currently only suggested when MRI is contra-indicated or inconclusive. In cases with negative blood cultures or inconclusive imaging, a surgical or CT-guided biopsy is suggested. Treatment is mainly based on expert opinions due to little evidence from clinical trials. In Denmark, 8–12 weeks of antibiotic treatment is standard of care in uncomplicated cases. The purpose of this pilot study was to evaluate epidemiology, diagnostic procedures, treatment, and outcome of all patients with PVO admitted to hospitals in Region Zealand, Denmark, during 2013.
Methods
Inclusion of relevant cases
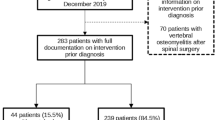
Data were obtained from a register of all patients admitted to hospitals in Region Zealand and patients were identified with unique identification numbers from the Danish Civil Registration System. Patients admitted to hospital in 2013 and subsequently discharged with a diagnosis of PVO or discitis were eligible for screening. The following ICD-10 (International Classification of Diseases, 10th edition) discharge codes were used as screening criteria, either as primary or secondary diagnosis: M46.2-9; M49.0-3. Patients were excluded if the PVO diagnosis was not confirmed in the patient record, or if no outcome data could be extracted.
Data extraction and registration
Patient records were reviewed in the electronic patient records system (OPUS, CSC Scandihealth A/S) used in Region Zealand. For each included patient, data regarding diagnostic procedures, treatment, and outcome were obtained. Patients were followed until death or 31 December 2014, whichever came first. Date of diagnosis was defined as the day a conclusion was made based on either MRI or PET-CT.
Ethics
The project was approved by the Danish Data Protection Agency, journal number 2008-58-0020. According to Danish law, no approval by the Medical Ethics Committee is required for observational studies.
Results
Patients
The screening provided 52 patients. All hospital journals were reviewed systematically. Four were excluded due to erroneous coding of diagnosis, six were excluded because the diagnosis code was used for rheumatic disease, and one was excluded because the coded diagnosis was only tentative and the patient was relocated to another region of the country before treatment was initiated. This left 41 patients diagnosed with PVO in Region Zealand in 2013. There were no cases of granulomatous (tuberculous, brucellous, or fungal) or parasitic infections, and there were no confirmed post-operative cases, although two patients had preceding spinal surgery.
Epidemiology and diagnostic procedures
The mid-year population of Region Zealand in 2013 was 779,988. The incidence of PVO was 5.3 per 100,000 person years in the entire study population and 16.5 per 100,000 person years in the population aged 65 years or older. The median age at diagnosis was 71 years (range: 42–84) and the male–female ratio was 33:8.
Sixteen of 41 patients (39%) had diabetes, one was infected with human immunodeficiency virus, one was splenectomized, and four patients received immunosuppressive treatment (prednisolone or methotrexate). None of the included patients were diagnosed with cancer.
Back pain at admission was present in 32 patients (78%), with lower back pain specified in 19 of these. Fever, defined as temperature equal to or above 38.0 °C, was present in 31 patients (76%). The remaining patients were either described as repeatedly non-febrile (seven patients), or fever was not mentioned (three patients). In the patients with fever, the mean peak temperature was 38.8 °C. Twenty-three patients (56%) had combined back pain and fever and one patient had neither.
Imaging was used for diagnosis in all 41 cases, distributed on MRI with contrast (29 patients), MRI without contrast (10 patients), and PET-CT (two patients). Eight patients who were diagnosed by MRI subsequently had a PET-CT performed, and two patients had a bone scintigraphy. The reasons for performing MRI without contrast were low glomerular filtration rate (three patients), previous allergic reaction to contrast (one patient), failed intravenous access (one patient), and unexplained (five patients).
The most common site of infection was the lumbar spine, which was involved in 29 patients (71%). The thoracic spine was involved in 13 patients (32%) and the cervical spine was involved in two patients. The median number of affected vertebrae was 2 (range: 1–4). Patient characteristics, symptoms, and imaging results are summarized in Table 1.
C-reactive protein (CRP) levels, leukocytes, alkaline phosphatase levels, and erythrocyte sedimentation rate were registered on several milestones during treatment. At admission, CRP levels were elevated in 39 patients (95%) with an average value of 170 mg/L, while leukocytes were elevated (above 8.8 billion cells/L) in 29 patients (71%). Results from laboratory studies are shown in Table 2.
All patients had blood cultures performed and nine patients had a biopsy. Thirty-one blood cultures (76%) and three biopsies (33%) were positive for relevant bacterial agents. In two cases, multiple infectious agents were isolated from the culture. The most common infectious agent was Staphylococcus aureus, which was found in 21 patients (51%), including one patient with multiple infections. One of the positive biopsies was in a patient with negative blood cultures. Thus, in nine cases (22%), no infectious agent was isolated from either blood culture or biopsy (Table 1).
Treatment
All 41 patients were treated with antibiotics. In 33 cases (80%), antibiotic treatment was initiated before the date of diagnosis. In six cases (15%), antibiotic treatment was delayed more than 1 day after imaging technology verified diagnosis. Five of these cases were culture-negative. Several antibiotics were used with the most common being cefuroxime and dicloxacillin (data not shown). Of the nine culture-negative cases, seven were initially treated with cefuroxime, one with dicloxacillin, and one with dicloxacillin and penicillin.
Six patients died during antibiotic treatment, one patient was discontinued, and one patient received a prescription of lifelong antibiotic treatment. Among the remaining 33 patients, the median treatment period was 92 days (range: 58–244). Six surgical decompressions and one spondylodesis were performed.
Outcome
Seven patients (17%) died in the follow-up period. Six of these (15%) were in-hospital deaths during antibiotic treatment (10, 12, 29, 35, 36, and 112 days after diagnosis, respectively). The last fatality was a patient with terminal liver failure, in which antibiotic treatment was discontinued 43 days after the date of diagnosis and the patient was discharged to hospice. The infectious agent in the patients who died was S. aureus in five cases, while two were culture-negative.
Five patients (12%) had ultrasound verified endocarditis, of which two died during the follow-up period. All had S. aureus bacteremia.
Twenty-one patients (51%) had at least one abscess identified on MRI, distributed on 10 paravertebral, 8 epidural, 7 psoas, and 7 intraspinal abscesses.
Fourteen patients had follow-up visits more than 8 weeks after termination of antibiotic treatment. Of these, eight patients received daily analgesics for back pain.
Four patients were registered with neurological deficits at follow-up visits. One had developed persisting paresthesia on the lateral side of the left thigh (dermatomes L3–L4) after surgical intervention for PVO at the same level, but had no motoric deficits or cauda equina symptoms (American Spinal Injury Association Impairment Scale level D). Apart from the hypersensitivity, the patient recovered. Another patient had S. aureus bacteremia and PVO complicated by endocarditis with embolization to liver, kidney, spleen, and extremities. This patient later developed a radial nerve palsy, which was most likely not related to the PVO at levels L4/L5 and L5/S1. Two patients had existing neurologic deficits which did not change in relation to their current PVO diagnosis: one was paraplegic (no motoric function) after several previous spinal surgeries and recurring PVO and the other had a light motoric deficit of the lower extremities (movement against gravity and light resistance) due to degenerative changes. Outcomes are summarized in Table 1.
Discussion
In this retrospective study, we evaluated epidemiology, diagnostic procedures, treatment, and outcomes of all 41 patients treated for PVO in Region Zealand, Denmark, during 2013. The main findings were a high rate of bacteremia and a high in-hospital mortality, compared to what has been previously reported [6, 7]. Also, the results of this study support that the incidence of PVO has increased, as we found an incidence of 5.3 per 100,000 person years.
CRP level at admission was a sensitive marker for PVO, elevated in 95% of cases with an average value of 170 mg/L, while leukocytes were less sensitive, in accordance with recent studies [4, 8]. Blood culture results were also comparable to results described in recent literature, with 51% of cases infected with S. aureus, and 24% negative cultures [1, 4, 9]. However, a meta-analysis from 2008, which included data from more than 50 years, reported a lower rate of bacteremia [6]. In our study, only three of the 10 patients with negative blood cultures had a biopsy performed. Biopsies in the remaining seven cases could possibly have diminished the number of cases treated empirically. It is our impression that the reasons biopsies were not performed were ongoing antibiotic treatment and clinical improvement.
The median duration of antibiotic treatment was 92 days (13.1 weeks), which reflects that current guidelines suggest 8–12 weeks of treatment of uncomplicated cases and at least 12 weeks of treatment in cases with complications. A randomized controlled trial (RCT) found that in culture-positive cases, 6 weeks of treatment was non-inferior to 12 weeks [2]. Our data from the 2013 cohort suggest that a more prolonged treatment regimen has been frequent in the past but the findings of this pioneer RCT might be reflected in newer cohorts. Evidence for choice of empiric antibiotic treatment in culture-negative cases is still very limited.
The 1-year mortality in this study was 17% which was comparable to two recent Danish retrospective studies [8, 10]. However, a large retrospective Japanese trial [7] and a meta-analysis including data from 12 studies [6] reported lower 1-year mortality. There are some limitations to the interpretation of the high mortality found in the present study, which should be considered. The study only includes patients with MRI or PET-CT-confirmed PVO, and a relevant ICD-10 discharge code. It is possible that undiagnosed cases could have been identified by including a wider selection of discharge codes in the search strategy, e.g., osteomyelitis. However, the severity of the diagnosis makes it unlikely that numerous cases would be missed retrospectively. Another limitation is the small sample size of this study, which is why results should be considered in comparison with other published data. Strengths of the study are the comprehensive amount of data collected on each patient, and the fact that all patients with the diagnosis during an entire year in a geographically distinct area are included.
In conclusion, we found a high rate of bacteremia and a high mortality from PVO in this single-year Danish cohort. In addition, the data support previous findings of increased incidence. Although the condition remains rare, the findings in this study suggest that PVO should often be suspected in patients presenting with back pain and fever in various areas of clinical practice ranging from emergency departments to rehabilitation clinics. Efforts should be made to secure early diagnosis and microbial etiology. Further studies of predictors for different outcomes are warranted, especially regarding culture-negative cases and the clinical value of performing bone biopsies.
References
Zimmerli W. Vertebral osteomyelitis. N Engl J Med. 2010;362:1022–9.
Bernard L, Dinh A, Ghout I, Simo D, Zeller V, Issartel B, et al. Antibiotic treatment for 6 weeks versus 12 weeks in patients with pyogenic vertebral osteomyelitis: an open-label, non-inferiority, randomised, controlled trial. Lancet. 2014;385:875–82.
Lew D, Waldvogel F. Osteomyelitis. Lancet. 2004;364:369–79.
Kehrer M, Pedersen C, Jensen TG, Lassen AT. Increasing incidence of pyogenic spondylodiscitis: a 14-year population-based study. J Infect. 2014;68:313–20.
Dahl B, Ebdrup L, Gormsen LC, Katzenstein T, Larsen VA, Friis Møller A, et al. Guidelines for diagnostik og behandling af spondylodiskit. 2003. http://neuroradiologi.dk/onewebmedia/Spondylodiscitis Guidelines 2013.pdf. Accessed 25 Feb 2018.
Mylona E, Samarkos M, Kakalou E, Fanourgiakis P, Skoutelis A. Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Semin Arthritis Rheum. 2009;39:10–7.
Akiyama T, Chikuda H, Yasunaga H, Horiguchi H, Fushimi K, Saita K. Incidence and risk factors for mortality of vertebral osteomyelitis: a retrospective analysis using the Japanese diagnosis procedure combination database. BMJ Open. 2013;3:e002412.
Aagaard T, Roed C, Dragsted C, Skinhøj P. Microbiological and therapeutic challenges in infectious spondylodiscitis: a cohort study of 100 cases, 2006-2011. Scand J Infect Dis. 2013;45:417–24.
Valancius K, Hansen ES, Hoy K, Helmig P, Niedermann B, Bünger C. Failure modes in conservative and surgical management of infectious spondylodiscitis. Eur Spine J. 2013;22:1837–44.
Kehrer M, Pedersen C, Jensen TG, Hallas J, Lassen AT. Increased short- and long-term mortality among patients with infectious spondylodiscitis compared with a reference population. Spine J. 2015;15:1233–40.
Acknowledgements
The authors wish to kindly thank Dr. Yashar Ostad Ahmadli for his assistance in the data registration process.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Brummerstedt, M., Bangstrup, M. & Barfod, T.S. High mortality from pyogenic vertebral osteomyelitis: a retrospective cohort study. Spinal Cord Ser Cases 4, 59 (2018). https://doi.org/10.1038/s41394-018-0099-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-018-0099-y
- Springer Nature Limited
This article is cited by
-
Postoperative prolonged mechanical ventilation in patients with surgically treated pyogenic spondylodiscitis: a surrogate endpoint for early postoperative mortality
Neurosurgical Review (2023)
-
Treatment of MRSA-infected osteomyelitis using bacterial capturing, magnetically targeted composites with microwave-assisted bacterial killing
Nature Communications (2020)
-
Treatment outcomes in patients with pyogenic vertebral osteomyelitis who have cirrhosis
Scientific Reports (2019)
-
Therapie der Spondylodiszitis
Trauma und Berufskrankheit (2019)