Abstract
Study design
Retrospective study of a prospective cohort of patients with traumatic spinal cord injury (SCI).
Objectives
Determine the relationship between the occurrence of early spasticity, defined as the development of signs and/or symptoms of spasticity during the hospitalization in traumatology, and the functional outcome 6–12 months following a SCI. Secondly, to determine the specific impact of early clonus, velocity-dependent hypertonia and/or muscle spasms on the functional outcome at the same timepoint.
Setting
Single trauma center specialized in SCI care.
Methods
One hundred sixty-two patients sustaining an acute traumatic SCI were included in the analyses. Comparative analysis was performed to describe the characteristics of patients with early spasticity. Correlations were performed to determine the relationship between the clinical signs of spasticity and the Spinal Cord Independence Measure (SCIM) scores collected 6–12 months after SCI.
Results
51.9% of the cohort developed clinical signs of spasticity during the hospitalization in traumatology (29.7 days) following SCI. These showed a significantly lower total SCIM score and subscores compared to individuals without early spasticity at follow-up (p < 0.05). After adjusting for confounding factors, the occurrence of early spasms was only clinical sign of spasticity significantly associated with a decreased mobility at follow-up (r = −0.17, p = 0.04).
Conclusions
The development of signs and symptoms of spasticity, in particular the occurrence of spasms in the first month following the injury may be associated with decreased functional outcome and mobility. Early assessment of spasticity following SCI is thus recommended.
Similar content being viewed by others
Introduction
Spasticity, a sensorimotor disorder characterized by intermittent or sustained involuntary muscle activation, is a common secondary condition associated with upper motor neuron lesions such as spinal cord injury (SCI) [1, 2]. Approximately 70% of individuals with chronic SCI (>1 year post injury) will experience involuntary muscle contractions (spasms), rhythmic oscillating stretch reflex (clonus) and/or velocity-dependent hypertonia below the level of injury [3]. Spasticity following SCI may have both positive and negative impacts on the patient’s outcomes [4, 5]. While spastic signs may compensate for muscle weakness, facilitating transfers, sitting balance, and standing [3,4,5], it may also lead to pain, disturbed sleep, and ineffective performance in daily living activities [6].
The impact of the timing for spasticity onset has gained interest in the SCI literature in the last years. As part of the spinal shock emergence, spasticity after SCI is attributed to a hyperexcitability state related to the development of supersensitivity of the motor neural circuit after an acute loss of supraspinal excitatory input due to the SCI [7, 8]. Accordingly, the development of spastic signs is generally reported multiple weeks after the injury [3, 8]. However, recent evidence suggested that a significant proportion (63%) of individuals with SCI may develop spastic signs as early as within the first month following the injury [9], more precisely during the hospitalization in traumatology (approximately 30 days in Canada) [10]. While it was hypothesized that early onset of spasticity signs could be associated with problematic spasticity in the chronic phase and poorer rehabilitation outcomes, experimental data rather suggested that spasticity is more prevalent in incomplete SCI associated with higher neurofunctional recovery [1, 11, 12]. Thus, the functional impact of the early onset of spastic signs following SCI remains largely elusive.
We hypothesize that these conflicting results could be related to the fact that the early onset of spastic signs (clonus, velocity-dependent hypertonia, and muscle spasms) developed during the hospitalization in traumatology, may indicate a different impact on the functional recovery following SCI. This information would greatly help clinicians in estimating the prognosis, orient the rehabilitation plan, and establish realistic long-term goals [4, 5]. It may also help in identifying clinical sign of spasticity that could be specifically targeted for treatment or for the elaboration of clinical trials. The objective of this study was thus twofold. First, to investigate the relationship between the occurrence of early spasticity, defined as the development of spastic signs during the hospitalization in traumatology, and the functional status in the subacute to chronic period following SCI. Then, to determine the specific relationship of the early development of clonus, velocity-dependent hypertonia, and muscle spasms on the same outcome, as assessed by the Spinal Cord Independence Measure 6–12 months post injury.
Methods
Study design
This is a retrospective study of a prospective cohort of patients admitted to a single Level-1 University traumatology center specialized in SCI care. Patients were admitted between April 2010 and September 2017. This study was approved by the local institutional review board, and all individuals were enrolled on a voluntary basis.
Participants
A total of 164 patients sustaining an acute traumatic SCI were considered. Patients were included if they met the following inclusion criteria: (1) being ≥18 years of age at the time of trauma, (2) sustaining a traumatic SCI with an American Spinal Association Injury Impairment Scale (AIS) grade A, B, C, or D at admission, (3) neurological level of injury (NLI) between C1 and L1 (conus medullaris and cauda equina syndromes are not associated with upper motor neurone syndrome and spasticity), (4) had a follow-up at 6 or 12 months post injury, and (5) information about spasticity collected by a physiatrist or physiotherapist specialized in SCI care was available in the medical chart during the hospitalization in traumatology. Patients were excluded if they had any pre-existing neurological conditions (SCI, stroke, Parkinson’s disease, etc.) associated with spasticity.
Main independent variables
The development of spasticity was noted based on the physical findings of the physical medicine and rehabilitation (physiatry) and physiotherapy teams, as well as symptoms reported by patients during the hospitalization in traumatology. The expertise in SCI care in Quebec (Canada) has led to the establishment of centers specialized in SCI care, organized into a specific continuum of care consisting of three specific phases aiming to decrease morbidity and mortality in this population [13,14,15,16]: (1) hospitalization in traumatology (where medical stabilization is reached, surgical stabilization is completed, rehabilitation plan is elaborated and initiated); (2) inpatient functional rehabilitation (aiming to maximize functional recovery); (3) reintegration and community maintenance. The average number of days spent in the traumatology (acute care) center following a traumatic SCI in Canada is 24 and 34 days for individuals with para- and tetraplegia, respectively [10].
Three important clinical manifestations of spasticity were considered: (1) presence of increased velocity-dependent muscle tone at physical examination (Modified Ashworth scale score of >1); 2) spasms identified at physical examination and/or reported by the patient, and (3) clonus noted at physical examination and/or reported by the patient [3, 9, 11, 17]. Our cohort was then subdivided into two groups based on the development of these spastic signs during the trauma hospitalization. Group 1 included 78 (48.1%) individuals (“no early spasticity group”) who did not develop spasticity during the hospitalization in traumatology, while Group 2 (“early spasticity group”) included 84 individuals (51.9%) who developed at least one of the three spastic signs during the hospitalization in traumatology.
Covariates
Socio-demographic data included age, body mass index, and gender. The initial severity of the SCI was reported using the AIS grade and the NLI, based on the International Standards for the Neurological Classification of Individuals with SCI (ISNCSCI) [18]. A trained spine surgeon or physical medicine and rehabilitation specialist routinely perform the neurological examination within the first 72 h of the injury. The severity of the injury and the NLI were also assessed in a combined fashion, as suggested by Whiteneck et al. in 2012, to create four clinically relevant categories: (C1–C4 AIS grade A, B, C; C5-C8 AIS grade A, B, C; paraplegia (T9 and below) AIS grade A, B, C; and all AIS Ds) [19, 20]. The AIS motor score was also noted. The burden of associated injuries was evaluated using the Injury Severity Score (ISS) [21]. The presence of concomitant traumatic brain injury was diagnosed based on the Glasgow coma scale and brain imaging at admission [22]. The presence of comorbidities was assessed using the Charlson Comorbidity Index (CCI), which weighs 19 comorbidities based on the adjusted relative risk of 1-year mortality [23]. The CCI score was then dichotomized into a score of 0 (no comorbidities) vs. ≥1.
Since the presence of concomitant medical complications was shown to be associated with the presence and severity of spasticity in the SCI population [9, 24, 25], the following complications were noted during the hospitalization in traumatology: (1) respiratory complications (e.g., pneumonia, pulmonary embolism; bronchitis; atelectasis; pneumothorax; etc.), (2) urinary tract infections (UTI) and (3) pressure injuries. The occurrence of respiratory complications was diagnosed using clinical features and confirmed by a radiologist using chest X-rays [26]. UTI were diagnosed using criteria from the 2006 Consortium for Spinal Cord Medicine Guidelines for healthcare providers, based on the significant presence of bacteriuria, pyuria (increased white blood cells in the urine), as well as signs and symptoms of UTI [27]. Finally, the presence of pressure injuries was diagnosed as per clinical guidelines defined by the National Pressure Injury Advisory Panel (NPIAP) [28, 29]. The complication rate was calculated, referring to the proportion of patients who developed one of the above-mentioned complications during the hospitalization in traumatology, and was expressed as a percentage. The length of stay was defined as the number of days from admission to discharge from the traumatology center.
Outcome variables
The main outcome variable was defined as the functional status as assessed by the third version of the Spinal Cord Independence Measure (SCIM) questionnaire completed 6–12 months post injury. The SCIM is a reliable and sensitive questionnaire specific to SCI, aimed at evaluating the patient’s ability to perform daily living activities independently [30]. The same research assistant supported patients when answering the questionnaire, to ensure a homogeneous interpretation. This research assistant was not involved in patient care nor data analysis. The SCIM assesses three specific areas of function: (1) self-care, (2) respiration and sphincter management, and (3) mobility. The total score includes all three subscores and a higher score indicates a higher functional level. The 12 months post-injury SCIM questionnaire was preferably used. If the information was not available at this timepoint, the 6-month post-injury SCIM questionnaire was used to increase study power, as the functional status in this population has previously been shown to be similar at these two timepoints [31].
Statistical analysis
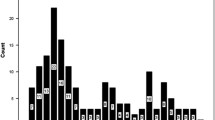
Descriptive analyses were performed to describe baseline characteristics of the entire cohort and comparison analyses were performed to compare characteristics of the two groups. Mean and standard deviation (SD) were reported for continuous variable while percentage were used for categorical variables. The normality of distributions for continuous variables was first verified using kurtosis and skewness analysis. Non-normal variables (ISS and SCIM subscore 1 and 2) were transformed using log transformation and dichotomization using top box scoring (defined as the percentage of individuals reaching the highest score possible for this subscore), respectively. Chi-square and Student t tests were then used to compare categorical and continuous variables, respectively.
Bivariate correlations were first carried out between the presence of at least one of three signs of early spasticity and the total SCIM score, in order to verify the main hypothesis of this study. Bivariate correlations were also performed between each spastic sign (clonus, velocity-dependent hypertonia, and spasms) and the total SCIM score. Bivariate correlations were then used to assess the relationship between each of the potential confounding variables (consisting of the baseline variables presented in Table 1) and the outcome. Significant variables at the univariate level were then entered as covariates in a partial correlation model investigating the relationship between the development of signs of early spasticity and the functional outcome. Secondarily, analyses were carried out for each SCIM subscore (self-care, sphincters and respiratory management and mobility) as the dependent variable. All statistical analyses were performed with SPSS software (release 26.0.0.1) with a significance level of 0.05.
Results
Amongst the 164 eligible patients, 2 were excluded based on the presence of neurological deficits potentially associated with spasticity prior to the traumatic SCI. The final cohort available for analysis included 162 patients. Table 1 presents the baseline characteristics for patients who did and did not develop signs and symptoms of spasticity during the hospitalization in traumatology. A total of 51.9% (N = 84) presented at least one sign or symptom of spasticity (early spasticity group). Within that group, 73.8% (N = 62) of patients developed spasms, while the development of hypertonia and clonus was reported in 46.4% (N = 39) and 39.3% (N = 33), respectively. A total of 26 individuals (31.0% of individuals with early spasticity) developed spasms and hypertonia. Similarly, 22 individuals (26.2%) developed spasm and clonus. Finally, ten individuals (6.2% of the early spasticity group) developed all three signs/symptoms of spasticity during the hospitalization in the traumatology center.
Individuals with at least one sign of early spasticity showed significantly lower total SCIM score and subscores at follow-up compared to individuals without early spasticity (p < 0.05) (Table 1). Individuals with early spasticity sustained a lower proportion of complete SCI (AIS grade A), higher proportion of cervical (C1–C4) injuries and a lower AIS motor score, as compared to the non-early spasticity group. A higher proportion of traumatic brain injury, of medical complications and a longer length of stay in the traumatology center were also found in the early spasticity group as compared to the “no early spasticity group” (Table 1). Both groups were however similar in terms of age, body mass index, sex, and presence of comorbidities.
Table 2 presents the SCIM scores (total and subscores) at follow-up for individuals who have (or have not) developed early signs and/or symptoms of spasticity. Results show that all functional scores were decreased in individuals who developed spasms during the hospitalization in traumatology, as compared to individuals who did not (p < 10−3). Individuals with early onset of hypertonia or clonus showed similar functional scores with individuals who did not (Table 2).
Table 2 also presents results of the bivariate correlations between each spastic sign and the SCIM scores (total and subscores) following SCI. The development of spasms was the only clinical manifestation of early spasticity related to the total SCIM score at follow-up, with a moderate correlation coefficient (r = −0.4, p < 10−3). The development of spasms during acute care was also significantly associated with the three functional subscores with similar correlation coefficients (Table 2). On the other hand, the presence of clonus and hypertonia was not associated with the functional outcome at follow-up (p > 0.05).
Based on the results showing that the early onset of spasms was the only clinical sign of spasticity consistently associated with the functional outcome, partial correlations were then carried out between the development of spasms during the hospitalization in traumatology and the SCIM scores (total and subscores) at follow-up. Table 3 also shows all confounding variables that were revealed significant at the univariate level with the outcome (p < 0.05), and thus entered in each partial correlation model as covariates. After adjusting for these confounding factors, the occurrence of spasms during the acute care hospitalization was only significantly associated with a decreased mobility (SCIM subscore 3) at follow-up (r = −0.17, p = 0.04). In order to assess the impact of combined signs and symptoms of spasticity, additional analyses among individuals with early spasms showed that the additional presence of hypertonia and/or clonus had no impact on the functional scores (total and subscores) compared to individuals with early spasms only (Table 4).
Discussion
This is the first study, to our knowledge, to have assessed the relationship of an early onset of spasticity on the functional outcome in the subacute to chronic period following a SCI. This study identified that the development of muscle spasms within the hospitalization in traumatology (<30 days) following the injury may be detrimentally associated with long-term functional outcome. More specifically, the presence of early spasms was independently associated with decreased mobility (transfers, walking indoors/outdoors, stairs management) in the subacute to chronic phase following a traumatic SCI.
The incidence of spasticity in this study was 51.9%, which is inferior to the ≈70% prevalence of spasticity usually reported in the chronic SCI literature [1, 3, 32]. Considering that this study was completed during the hospitalization in traumatology (first month following the injury), this finding may suggest that a majority of individuals experiencing chronic spasticity will develop signs and/or symptoms of spasticity within the first month following a traumatic SCI. We have also observed a high proportion of cervical traumatic SCI in individuals who developed early spasticity and a lower incidence of complete SCI (AIS A) in that group. When looking at specific groups combining the level and severity of the SCI, results also suggest that early spasticity may be prevalent in individuals sustaining severe cervical injuries (C1-C8 AIS A, B, and C) and less commonly following paraplegia or functional-incomplete (AIS D) SCI. Considering that a recent Canadian study by Holtz et al. [1], suggested that the prevalence of problematic spasticity (defined as requiring anti-spasticity medication >1 year following SCI) is particularly high in individuals sustaining cervical AIS B and C injuries, may indirectly suggest that the early development of spasticity (within the first weeks following the injury) could be indicative of problematic spasticity requiring pharmaceutical treatment in the chronic phase. Recent neurophysiological evidence may potentially explain this result, providing evidence for lesser corticospinal and larger reticulospinal influences to spastic muscles in humans with SCI, with these imbalanced contributions being important for motor recovery [12].
We have observed that the independent presence of spasms during acute care was associated with decreased mobility at follow-up. It has been suggested that spasms may impede mobility by decreasing motor control, disturb balance and/or cause pain impeding effective transfer and ambulation [6]. While it has been suggested that hypertonia of leg extensor muscles may enable supporting the body for facilitating transfers and locomotion [33, 34], our results did not show an independent and consistent association between early hypertonia (or clonus) and function. We also observed that the addition of hypertonia or clonus to early spasms did not influence the total SCIM score nor the mobility (subscore 3) compared to the occurrence of early spasms alone (p > 0.05). However, the co-occurrence of spasms and hypertonia (or clonus) showed a tendency (p = 0.06) toward a higher proportion of individuals reaching the maximum self-care score (subscore 1) compared with individuals with spasms alone, which may suggest a possible beneficial influence of early hypertonia (and clonus) following SCI on this functional aspect.
This study highlights the importance of an extensive assessment of spasticity early after a SCI by acknowledging its various clinical manifestations. In particular, assessing the occurrence of spasms (reported by the patient or noted at physical examination) during the hospitalization in traumatology is of primary importance. Early assessment and interventions (e.g., repetitive goal-oriented therapy, stretching, muscle strengthening, splinting/orthosis, targeted pharmacologic treatment, etc.) for spasticity may create a transient plastic state of the neuromotor system allowing higher motor re-learning and neurofunctional recovery [9, 35, 36]. Pharmaceutical interventions such as anti-spastic drugs should be considered in cases of problematic spasticity, but clinical judgment is warranted due to the lack of evidence of clinically significant effectiveness [37]. In addition, medical complications should be prevented, monitored, and treated closely by the acute rehabilitation team. Indeed, while early complications can impede functional recovery [37], it has been suggested that the nociceptive input due to pressure injuries, UTI, and pneumonia can increase spasticity [3, 9, 38]. It is interesting to note that individuals who developed early spasticity sustained a greater proportion of traumatic brain injury as opposed to the no early spasticity group. This supports the literature that suggests that traumatic brain injury-induced spasticity, as another central nervous system lesion, may develop rapidly, as early as 1 week following the injury [39]. Thus, it might not be surprising to note a higher incidence of early spasticity in individuals with concomitant diagnosis (SCI and traumatic brain injury). Table 1 also shows a higher AIS motor score in individuals who did not develop early spasticity, also reflecting the high proportion of individuals with AIS D SCI within that group. Because the motor function and presence of concomitant traumatic brain injury are acknowledged to influence the functional outcome [40], these two variables were considered as potential confounding factors in the analyses. The AIS motor score was significantly associated with the total SCIM scores and all subscores at the univariate level, and was thus included in all partial correlation models to verify the hypotheses of this study (Table 3). However, despite being significantly different between individuals with vs. without early development of spasticity, the presence of concomitant traumatic brain injury was not significantly associated with the outcome at the univariate level and was thus not included in the multivariable analysis.
Although physiatrists and physical therapists systematically assessed spasticity for all SCI individuals in our institution throughout the trauma hospitalization, the main limitation of this study relates to its retrospective nature. Therefore, we have not collected information pertaining to the severity, precise onset, and location of spasticity during the acute care, although such data could be helpful for future prospective studies to better understand its relationship with the functional outcome. Considering that we have only assessed spasticity during the hospitalization in traumatology, the timeframe for observing spasticity onset has been variable for all included individuals. It is also possible that patients have developed spasticity after discharge from the trauma center, but this study suggested that a great proportion of individuals might develop spasticity signs within the first month following the injury. But more importantly, assessing spasticity during the hospitalization in the traumatology center has the advantage of providing early information on the spasticity development process that can be used for early prognostication, particularly for planning and achieving the rehabilitation phase during which restoring function is a major aim. It is also important to mention that treatment (non-pharmaceutical or pharmaceutical) of spasticity during the hospitalization was not assessed in this study. However, it should be mentioned that the general consensus in spasticity is to initiate pharmaceutical treatment when deemed harmful or bothersome by the patient and/or involved healthcare professionals [3, 36, 41]. As pharmaceutical measures for spasticity are not generally used prophylactically, it is very unlikely to have influenced spasticity onset. However, authors acknowledge that the relationship between the use of pharmaceutical treatment and functional recovery remains largely elusive and could have influenced results of this study.
This study is the first study, to our knowledge, to investigate the potential impact of early spasticity on the functional outcome in the subacute to chronic period after traumatic SCI. Results show that the occurrence of at least one sign and/or symptoms of early spasticity was associated with decreased functional scores at follow-up. More precisely, the development of early spasms was the single clinical manifestation of spasticity associated with decreased mobility in the subacute to chronic phase, when adjusted for confounding factors. It is thus possible that the early development of spasms is associated with subsequent problematic spasticity, which may impede mobility by decreasing motor control, disturbing balance and/or cause pain during transfer and ambulation. This study highlights the importance of the assessment of spasticity early after a SCI by acknowledging the various clinical manifestations of spasticity, particularly by assessing the occurrence of spasms (reported by the patient or noted at physical examination) during the traumatology hospitalization.
Data availability
The datasets generated during and/or analyzed during current study are no publicly available due to the regulations defined by the ethics committee of the CIUSS Nord-de-l’île-de-Montréal, but are available from the corresponding author on reasonable request.
References
Holtz KA, Lipson R, Noonan VK, Kwon BK, Mills PB. Prevalence and effect of problematic spasticity after traumatic spinal cord injury. Arch Phys Med Rehabil. 2017;98:1132–8.
Pandyan AD, Gregoric M, Barnes MP, Wood D, Van Wijck F, Burridge J, et al. Spasticity: clinical perceptions, neurological realities and meaningful measurement. Disabil Rehabil. 2005;27:2–6.
Adams MM, Hicks AL. Spasticity after spinal cord injury. Spinal Cord. 2005;43:577–86.
Ayoub S, Smith JG, Cary I, Dalton C, Pinto A, Ward C, et al. The positive and the negative impacts of spasticity in patients with long-term neurological conditions: an observational study. Disabil Rehabil. 2020;1–8.
Ehrmann C, Mahmoudi SM, Prodinger B, Kiekens C, Ertzgaard P. Impact of spasticity on functioning in spinal cord injury: an application of graphical modelling. J Rehabil Med. 2020;52:jrm00037.
D’Amico JM, Condliffe EG, Martins KJ, Bennett DJ, Gorassini MA. Recovery of neuronal and network excitability after spinal cord injury and implications for spasticity. Front Integr Neurosci. 2014;8:36.
Hiersemenzel LP, Curt A, Dietz V. From spinal shock to spasticity: neuronal adaptations to a spinal cord injury. Neurology. 2000;54:1574–82.
Ditunno JF, Little JW, Tessler A, Burns AS. Spinal shock revisited: a four-phase model. Spinal Cord. 2004;42:383–95.
Richard-Denis A, Nguyen BH, Mac-Thiong JM. The impact of early spasticity on the intensive functional rehabilitation phase and community reintegration following traumatic spinal cord injury. J Spinal Cord Med. 2020;43:435–43.
A look at traumatic spinal cord injury in Canada: Rick Hansen Spinal Cord Registry (RHSCIR). J Spinal Cord Med. 2017;40:870–1.
Trompetto C, Marinelli L, Mori L, Pelosin E, Curra A, Molfetta L, et al. Pathophysiology of spasticity: implications for neurorehabilitation. Biomed Res Int. 2014;2014:354906.
Sangari S, Perez MA. Imbalanced corticospinal and reticulospinal contributions to spasticity in humans with spinal cord injury. J Neurosci. 2019;39:7872–81.
Parent S, Barchi S, LeBreton M, Casha S, Fehlings MG. The impact of specialized centers of care for spinal cord injury on length of stay, complications, and mortality: a systematic review of the literature. J Neurotrauma. 2011;28:1363–70.
Richard-Denis A, Ehrmann Feldman D, Thompson C, Bourassa-Moreau E, Mac-Thiong JM. Costs and length of stay for the acute care of patients with motor-complete spinal cord injury following cervical trauma: the impact of early transfer to specialized acute SCI center. Am J Phys Med Rehabil. 2017;96:449–56.
Richard-Denis A, Feldman D, Thompson C, Albert M, Mac-Thiong JM. The impact of a specialized spinal cord injury center as compared with non-specialized centers on the acute respiratory management of patients with complete tetraplegia: an observational study. Spinal Cord. 2018;56:142–50.
Richard-Denis A, Feldman DE, Thompson C, Mac-Thiong JM. The impact of acute management on the occurrence of medical complications during the specialized spinal cord injury acute hospitalization following motor-complete cervical spinal cord injury. J Spinal Cord Med. 2018;41:388–96.
Bhimani R, Anderson L. Clinical understanding of spasticity: implications for practice. Rehabil Res Pract. 2014;2014:279175.
Kirshblum S, Waring W 3rd. Updates for the international standards for neurological classification of spinal cord injury. Phys Med Rehabil Clin N Am. 2014;25:505–17. vii
Teeter L, Gassaway J, Taylor S, LaBarbera J, McDowell S, Backus D, et al. Relationship of physical therapy inpatient rehabilitation interventions and patient characteristics to outcomes following spinal cord injury: the SCIRehab project. J Spinal Cord Med. 2012;35:503–26.
Whiteneck G, Gassaway J, Dijkers MP, Heinemann AW, Kreider SE. Relationship of patient characteristics and rehabilitation services to outcomes following spinal cord injury: the SCIRehab project. J Spinal Cord Med. 2012;35:484–502.
Baker SP, O’Neill B, Haddon W Jr., Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96.
Ghajar J. Traumatic brain injury. Lancet. 2000;356:923–9.
Charlson M, Wells MT, Ullman R, King F, Shmukler C. The Charlson comorbidity index can be used prospectively to identify patients who will incur high future costs. PLoS ONE 2014;9:e112479.
Ghai A, Garg N, Hooda S, Gupta T. Spasticity - pathogenesis, prevention and treatment strategies. Saudi J Anaesth. 2013;7:453–60.
Thompson AJ, Jarrett L, Lockley L, Marsden J, Stevenson VL. Clinical management of spasticity. J Neurol Neurosurg Psychiatry. 2005;76:459–63.
Cosortium for Spinal Cord M. Respiratory management following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2005;28:259–93.
Consortium for Spinal Cord M. Bladder management for adults with spinal cord injury: a clinical practice guideline for health-care providers. J Spinal Cord Med. 2006;29:527–73.
Kottner J, Cuddigan J, Carville K, Balzer K, Berlowitz D, Law S, et al. Prevention and treatment of pressure ulcers/injuries: The protocol for the second update of the international Clinical Practice Guideline 2019. J Tissue Viability. 2019;28:51–8.
European Pressure Ulcer Panel NpiaPaPPPIA. Prevention and treatment of pressure ulcers/injuries: Clinical Practice Guideline.: the international guideline; 2019. https://internationalguideline.com/.
Itzkovich M, Shefler H, Front L, Gur-Pollack R, Elkayam K, Bluvshtein V, et al. SCIM III (Spinal Cord Independence Measure version III): reliability of assessment by interview and comparison with assessment by observation. Spinal Cord. 2018;56:46–51.
Richard-Denis A, Chatta R, Thompson C, Mac-Thiong JM. Patterns and predictors of functional recovery from the subacute to the chronic phase following a traumatic spinal cord injury: a prospective study. Spinal Cord. 2020;58:43–52.
Maynard FM, Karunas RS, Waring WP 3rd. Epidemiology of spasticity following traumatic spinal cord injury. Arch Phys Med Rehabil. 1990;71:566–9.
Sommerfeld DK, Gripenstedt U, Welmer AK. Spasticity after stroke: an overview of prevalence, test instruments, and treatments. Am J Phys Med Rehabil. 2012;91:814–20.
Yoshizaki S, Yokota K, Kubota K, Saito T, Tanaka M, Konno DJ, et al. The beneficial aspects of spasticity in relation to ambulatory ability in mice with spinal cord injury. Spinal Cord. 2020;58:537–43.
Li S, Francisco GE. The Use of Botulinum Toxin for Treatment of Spasticity. Handb Exp Pharmacol. 2019;263:127–46.
Graham LA. Management of spasticity revisited. Age Ageing 2013;42:435–41.
Taricco M, Pagliacci MC, Telaro E, Adone R. Pharmacological interventions for spasticity following spinal cord injury: results of a Cochrane systematic review. Eura Medicophys. 2006;42:5–15.
Kheder A, Nair KP. Spasticity: pathophysiology, evaluation and management. Pract Neurol. 2012;12:289–98.
Bose P, Hou J, Thompson FJ. Traumatic brain injury (TBI)-induced spasticity: neurobiology, treatment, and rehabilitation. In: Kobeissy FH, editor. Brain neurotrauma: molecular, neuropsychological, and rehabilitation aspects. Frontiers in Neuroengineering. Boca Raton (FL): Springer International Publishing; 2015.
Richard-Denis A, Beausejour M, Thompson C, Nguyen BH, Mac-Thiong JM. Early predictors of global functional outcome after traumatic spinal cord injury: a systematic review. J Neurotrauma. 2018;35:1705–25.
Bell K, DiTommaso C, Model Systems Knowledge Translation C. Information/education page. spasticity and traumatic brain injury. Arch Phys Med Rehabil. 2016;97:179–80.
Acknowledgements
The authors would like to thanks Dr. Jean Bégin, for his guidance in the design of statistical analysis. We also want to thank the patients for the participation in our research projects.
Funding
This research was funded by the Fonds de recherche du Québec – Santé (Consortium in traumatology) (AR-D), the Medtronic Research Chair in Spinal Trauma at Université de Montréal (JMMT), and part of the data was collected through the Rick Hansen Spinal Cord Registry.
Author information
Authors and Affiliations
Contributions
AR-D was responsible for designing the protocol, conducting the search, screening for potentially eligible patients, extracting, and analyzing data. AL was responsible for extracting data, performing statistical analysis, and analyzing data. J-MM-T contributed to the design of the research protocol. All the authors participated in the interpretation of the results, writing, and editing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
AR-D has received a scholarship and research grants from the Fonds de recherche du Québec – Santé, an investigator-initiated research grant from Medline Industries, and a research grant from Praxis Spinal Cord Institute. J-MM-T is chairholder of the Medtronic research chair in spinal trauma at Université de Montréal, owns stocks and is a board member in Spinologics, and has received a scholarship and research grants from the Fonds de recherche du Québec – Santé, an investigator-initiated research grant from Medline Industries, educational grants from Medtronic and Depuy-Synthes, as well as research grants from the U.S. Department of Defense – Congressionally directed medical research programs.
Ethical approval
We certify that all applicable institutional and governmental regulation concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Levasseur, A., Mac-Thiong, JM. & Richard-Denis, A. Are early clinical manifestations of spasticity associated with long-term functional outcome following spinal cord injury? A retrospective study. Spinal Cord 59, 910–916 (2021). https://doi.org/10.1038/s41393-021-00661-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00661-1
- Springer Nature Limited