Abstract
Study design
Prospective observational study.
Objective
To evaluate pelvic MRI muscle signal changes and their association with early heterotopic ossification (HO) in patients with spinal cord injuries.
Setting
National Spinal Injuries Unit, Stoke Mandeville, UK.
Methods
Forty patients were imaged with at least two interval magnetic resonance (MR) studies of the pelvis in the first 6 months following a spinal cord injury. Scans were reviewed and scored for heterotopic ossification, muscle signal change and extent of muscle involvement.
Results
Muscle signal change was present in 28 (70%) on the initial MRI and 31 (77%) by the second study. Six patients developed MR changes of prodromal or immature heterotopic ossification (15%). No restricted diffusion was demonstrated and no patient developed mature HO. Patients developing MR changes of early HO were more likely to have grade 3 muscle changes.
Conclusion
Increased T2 muscle signal is common following cord injury, is frequently progressive in the subacute period and is associated with complete injury and early MR signs of heterotopic ossification.
Similar content being viewed by others
Introduction
Heterotopic ossification (HO) refers to pathological bone formation in the soft tissues around joints in a wide range of conditions including spinal cord injury [1]. Incidence is variably reported ranging from 10 to 50% of spinal injury patients, though large more recent studies approximate this to 6–10% [1,2,3,4,5]. HO also affects non-traumatic cord injury with a similar incidence [6]. It typically presents between 4 and 6 weeks from initial injury and most commonly involves the hips; knee, shoulder and elbow joints may also be affected [7]. A genetic predisposition to developing HO has been suggested based on human lymphocyte antigen (HLA)-typing with some authors suggested a relationship between HLA B18 and HLA B27 [8,9,10] although other studies have not found a significant association [11]. Other risk factors associated with HO include thoracic trauma, tracheostomy, spasticity, pressure ulcers, pneumonia and urinary tract infections [12].
HO most commonly presents with swelling, mild erythema and skin induration. C-reactive protein and alkaline phosphatase may be suggestive of active HO but imaging confirmation is usually required for diagnosis as differential diagnosis includes deep venous thrombosis and infection [13, 14]. Triple phase bone scintigraphy has been the mainstay of imaging diagnosis though normal isotope scans do not exclude subsequent development of HO [15]. Ultrasound has been demonstrated to be effective in identifying early changes which appear 3–4 weeks before radiographic signs are positive [16].
Complications of HO include ankylosis, pain, lymphoedema, decreased function and mobility that may impair rehabilitation. Localised mass effect from the oedema and bone formation may lead to peripheral nerve entrapment, vascular compression and lymphedema. These sequelae can also contribute to pressure ulcer formation [17].
MRI is sensitive for early changes of HO and demonstrates both early inflammatory change as well as mature osteoid. More recently it has been reported that widespread subcutaneous and muscle changes such as muscle, fascial and bone marrow oedema accompany many spinal cord injured patients with HO [18].
Medical treatments of HO have previously included bisphosphonates and non-steroidal anti-inflammatories [19]. Low dose radiotherapy has been advocated though has not gained widespread use in view of the relative youth of patients affected and concern regarding induction of tumours [20]. Surgical resection is reserved for late disease restricting joint movement [21].
As MRI is used increasingly frequently to assess a range of clinical problems in patients with cord injury including pelvic pressure sores [22, 23], we have noted that widespread increased T2 muscle signal is common in these patients and hypothesised a link with HO.
Patients and methods
This prospective observational study was conducted according to the Declaration of Helsinki protocols and was approved by the local research and ethics committee (REC reference number: 11/LO/1432). Data collection took place between March 2012 and January 2014. Inclusion criteria were adult patients over 18 years of age, admitted to our institution with traumatic or non-traumatic spinal cord injury within 60 days of initial trauma. The initial magnetic resonance (MR) study was undertaken typically 6 weeks from acute insult and the second after a similar interval. Patients with two normal studies did not have a third scan, as per protocol.
MR studies were undertaken on a 1.5 T Symphony Tim system (Siemens, Erlangen) using a combination of spine coils and a phased-array body coil. Typically a FOV of 40 cm was used and 25–30 slice sections acquired with a 20% slice gap. Sequences included T1SE axial (TR 460, TE 11, NSA 2, 5 mm sl th, 512 × 256 matrix. Diffusion-weighted axial (B0, B500, B1000 TR 4000, TE 98, NSA 7, 6.5 mm sl th, 128 × 96 matrix), STIR coronal (TR 4030, TE 85, NSA 2, 5 mm sl th, FA 150°, TI 160 ms, 320 × 240 matrix) and 2D FLASH Gradient echo axial (TR 750, TE 9.5, NSA 1, 5 mm sl th, 448 × 270 matrix, FA 20°).
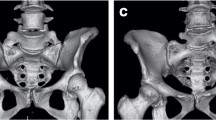
MR scans were reviewed and scored for HO, muscle signal change and extent of muscle involvement. Muscle increased STIR signal was graded 1–3 depending on extent of muscle involvement (Figs. 1, 2, 3). HO was classified as prodromal, immature and established HO (Figs. 4, 5 and Supplementary File). These studies were graded by consultant radiologists experienced in musculoskeletal radiology and in spinal cord injuries imaging. All second MR studies were reported by two radiologists to assess interobserver agreement. The level of spinal cord injury, American Spinal Injury Association Impairment Scale (AIS) [24] and date of cord injury were recorded.
Results
A total of 46 patients were consented but only 40 patients completed at least two MRI studies. Thirty-two patients were male and eight female. Average age was 41 years, median 49 years (range 21–87 years). Thirty-three patients (82%) had a traumatic cord injury and the seven had non-traumatic cord injury, most commonly cord infarction (five patients). Mean time in days from initial injury to first MRI scan was 41 days (median 42, range 25–60 days) and to the second scan was 81.2 (median 82.5, range 55–122 days). Twenty-two patients had a third MR scan. Three patients had MR changes of prodromal HO and three had MR changes of immature HO (Fig. 5). All three patients with immature HO were AIS A (P < 0.001), Table 1.
Increased T2 muscle signal change (Grade 2 and above) was present in 28 (70%) of patients on the initial MR study and this increased to 31 (77%) by the second study. Of 23 patients who had a third study 6 (26%) improved, 1 (4%) deteriorated and 16 (70%) were unchanged, Table 2.
Patients who were AIS A (sensory and motor complete SCI) were significantly less likely to have normal muscle signal (Grade 1): 1/18 AISA (5%) compared with 8/22 AISB–D (36%), Table 3.
At the initial MR study 15 (37%) had normal muscle signal and this decreased to 11 (27%) by the second study and correspondingly Grades 2 and 3 increased. Abnormal increased T2 signal was most commonly seen in the gluteal and quadriceps muscles and less commonly identified in the adductor and iliopsoas muscles, Table 4.
The incidence of Grade 3 muscle signal change was 60% in those patients with early changes of HO and in the patients who did not develop early changes was 31%.
Interobserver agreement
The calculations above only consider exact matches between observers. The number of observed agreements were 23 (82% of the observations) a Kappa of 0.73 (SE 0.104). The number of agreements expected by chance: 9.4 (34% of the observations), a 95% confidence interval from 0.528 to 0.935. The strength of agreement is considered to be ‘good’.
Discussion
Immature HO is well described, presenting clinically and appreciable on isotope scintigraphy and ultrasound [13, 14, 16, 25]. Early ossification may be visible on plain radiographs and CT but these are frequently normal up to 4 weeks after a patient develops symptoms [25, 26]. However, imaging is also known to demonstrate foci of HO which are subclinical and it is also established that foci of immature HO may reverse [13, 25].
We had noted many patients with extensive increased T2 muscle signal in the rehabilitation phase and the genesis of this study was trying to ascertain if this was linked to early HO. The cause of HO remains uncertain [12]. Suggested theories include whether the mass and swelling associated with HO might be related to ischaemia, so we also evaluated whether diffusion-weighted imaging might prove useful. None of 26 patients evaluated with DWI demonstrated restricted diffusion including all patients with prodromal HO (n = 3) and immature HO (n = 3). This suggests there is no evident benefit from using this sequence in evaluating patients with suspected HO.
Wick et al. demonstrated that abnormal muscle signal is associated with established HO. In their review of 14 patients, all had widely increased T2 muscle increased signal, most commonly affecting quadriceps [18]. Our series supports this finding in patients with HO, all of whom had bilateral extensive muscle signal change. The most commonly affected muscles in our cohort were gluteus medius in 28 (67%), gluteus maximus 24 (57%), quadriceps 20 (48%), adductors 15 (36%) and iliopsoas 14 (33%). This is consistant with previous studies of HO localisation [27, 28]. A potential limitation may have been assessment in the coronal plane which limits the assessment of the quadriceps and iliopsoas compared with other muscles. Wick also highlighted the use of gradient echo sequence (GE) in identifying early ossification [18]. This was used in 16 of our patients but did not significantly alter diagnoses.
The MR imaging appearances described by Ledermann et al. are of more established neurogenic HO with progressive and mature ossification seen in a patient cohort consisting of thirty-one patients with traumatic spinal cord injury, two patients with spinal cord infarctions, and three patients were with multiple sclerosis (MS), ischemic brain damage, and spina bifida [29]. MRI also depicted high signal change in the Grade 1 classification of this group (gradation established by CT appearance) and increased MR signal in muscle and para-articular tissues is similarly described. The patient group included MS and head injury.
Results from our cohort indicate progressive muscle signal change with time between 40 and 80 days, the average time between scans, but more patients improved by the third scan than deteriorated. This accords with the observation that the most common onset of symptomatic HO is around 6–8 weeks from acute injury. Increased muscle signal was also more prevalent in AIS A and of a higher grade (Tables 1, 3) compared with incomplete grades. This is also in keeping with known association of HO incidence.
There are many limitations to this study. Numbers are small, sequences did not include contrast which can be helpful in depicting HO and GE series was not used on all patients. There was no comparison with other modalities including CT to correlate with early calcinosis. Despite these limitations, the data suggests a significant link between incremental muscle signal change and the development of HO. Pelvic MRI 40 days following injury may be helpful to detect these changes and identify those at risk of HO. Further studies are required to determine whether early medical intervention is associated with less severe disease and associated complications.
Conclusion
The incidence of HO in this study of patients with SCI is 7%, and approximates to previously published rates. MRI using STIR and T1 weighted sequences is useful in depicting HO but diffusion-weighted sequences were unhelpful. Increased muscle signal is common and progressive in the initial months following cord injury and is associated with AIS A injury and development of immature HO. Imaging with MRI ~40 days following injury may help identify those at risk of early HO.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Bravo-Payno P, Esclarin A, Arzoz T, Arroyo O, Labarta C. Incidence and risk factors in the appearance of heterotopic ossification in spinal cord injury. Spinal Cord. 1992;30:740–5.
Colachis SC, Clinchot DM. The association between deep venous thrombosis and heterotopic ossification in patients with acute traumatic spinal cord injury. Spinal Cord. 1993;31:507–12.
Prakash V. Radionuclide assessment of heterotopic ossification in spinal cord injury patients. J Am Paraplegia Soc. 1983;6:10–2.
Wittenberg RH, Peschke U, Bötel U. Heterotopic ossification after spinal cord injury. Epidemiology and risk factors. J Bone Jt Surg Br. 1992;74:215–8.
Reznik JE, Biros E, Marshall R, Jelbart M, Milanese S, Gordon S, et al. Prevalence and risk-factors of neurogenic heterotopic ossification in traumatic spinal cord and traumatic brain injured patients admitted to specialised units in Australia. J Musculoskelet Neuronal Interact. 2014;14:19–28.
Taly A, Nair K, Kumar MV, Jayakumar P, Vasudev M, Ravishankar D, et al. Heterotopic ossification in non-traumatic myelopathies. Spinal Cord. 1999;37:47–9.
Goodman TA, Merkel PA, Perlmutter G, Doyle MK, Krane SM, Polisson RP. Heterotopic ossification in the setting of neuromuscular blockade. Arthritis Rheum. 1997;40:1619–27.
Minaire P, Betuel H, Girard R, Pilonchery G. Neurologic injuries, paraosteoarthropathies, and human leukocyte antigens. Arch Phys Med Rehabil. 1980;61:214–5.
van Kuijk A, Geurts A, van Kuppevelt H. Neurogenic heterotopic ossification in spinal cord injury. Spinal Cord. 2002;40:313–26.
Vanden Bossche L, Vanderstraeten G. Heterotopic ossification: a review. J Rehabil Med. 2005;37:129–36.
Garland DE, Alday B, Venos KG. Heterotopic ossification and HLA antigens. Arch Phys Med Rehabil. 1984;65:531–2.
Citak M, Suero EM, Backhaus M, Aach M, Godry H, Meindl R, et al. Risk factors for heterotopic ossification in patients with spinal cord injury: a case-control study of 264 patients. Spine. 2012;37:1953–7.
Banovac K, Gonzalez F. Evaluation and management of heterotopic ossification in patients with spinal cord injury. Spinal Cord. 1997;35:158–62.
Cassar-Pullicino VN, McClelland M, Badwan DA, McCall IW, Pringle RG, el Masry W. Sonographic diagnosis of heterotopic bone formation in spinal injury patients. Paraplegia. 1993;31:40–50.
Svircev JN, Wallbom AS. False-negative triple-phase bone scans in spinal cord injury to detect clinically suspect heterotopic ossification: a case series. J Spinal Cord Med. 2008;31:194–6.
Rosteius T, Suero EM, Grasmücke D, Aach M, Gisevius A, Ohlmeier M, et al. The sensitivity of ultrasound screening examination in detecting heterotopic ossification following spinal cord injury. Spinal Cord. 2017;55:71–3.
Behery OA, Dai AZ, McLaurin TM. Posttraumatic heterotopic ossification of the hip. J Orthop Trauma. 2018;32 Suppl 1:S18–9.
Wick L, Berger M, Knecht H, Glücker T, Ledermann HP. Magnetic resonance signal alterations in the acute onset of heterotopic ossification in patients with spinal cord injury. Eur Radiol. 2005;15:1867–75.
Banovac K. The effect of etidronate on late development of heterotopic ossification after spinal cord injury. J Spinal Cord Med. 2000;23:40–4.
Pakos EE, Ioannidis JPA. Radiotherapy vs. nonsteroidal anti-inflammatory drugs for the prevention of heterotopic ossification after major hip procedures: a meta-analysis of randomized trials. Int J Radiat Oncol Biol Phys. 2004;60:888–95.
de l’Escalopier N, Salga M, Gatin L, Genêt F, Denormandie P. Resection of heterotopic ossification around the hip after trauma. EFORT Open Rev. 2019;4:263–8.
Hauptfleisch J, Meagher TM, Hughes RJ, Singh JP, Graham A, López de Heredia L. Interobserver agreement of magnetic resonance imaging signs of osteomyelitis in pelvic pressure ulcers in patients with spinal cord injury. Arch Phys Med Rehabil. 2013;94:1107–11.
López de Heredia L, Hauptfleisch J, Hughes R, Graham A, Meagher TMM. Magnetic resonance imaging of pressure sores in spinal cord injured patients: accuracy in predicting osteomyelitis. Top Spinal Cord Inj Rehabil. 2012;18:146–8.
Greenspan L, McLellan BA, Greig H. Abbreviated injury scale and injury severity score: a scoring chart. J Trauma. 1985;25:60–4.
Freebourn TM, Barber DB, Able AC. The treatment of immature heterotopic ossification in spinal cord injury with combination surgery, radiation therapy and NSAID. Spinal Cord. 1999;37:50–3.
Mujtaba B, Taher A, Fiala MJ, Nassar S, Madewell JE, Hanafy AK, et al. Heterotopic ossification: radiological and pathological review. Radiol Oncol. 2019;53:275–84.
Ohlmeier M, Suero EM, Aach M, Meindl R, Schildhauer TA, Citak M. Muscle localization of heterotopic ossification following spinal cord injury. Spine J. 2017;17:1519–22.
Arduini M, Mancini F, Farsetti P, Piperno A, Ippolito E. A new classification of peri-articular heterotopic ossification of the hip associated with neurological injury: 3D CT scan assessment and intra-operative findings. Bone Jt J. 2015;97-B:899–904.
Ledermann HP, Schweitzer ME, Morrison WB. Pelvic heterotopic ossification: MR imaging characteristics. Radiology. 2002;222:189–95.
Funding
This project was in receipt of funding from the Davenport Award, Buckinghamshire NHS Trust Charitable Fund and also received NHS Portfolio support funding.
Author information
Authors and Affiliations
Contributions
The authors confirm that all authors have made substantial contributions to all four categories established by the International Committee of Medical Journal Editors (http://www.icmje.org) to include: (1) conception and design, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be published, and (4) agree to be accountable for all aspects of the work if questions arise related to its accuracy or integrity.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
We certify that all applicable institutional and governmental regulations concerning the ethical use of patients were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
McKean, D., Ather, S., Gandhi, A. et al. Pelvic MRI in spinal cord injury patients: incidence of muscle signal change and early heterotopic ossification. Spinal Cord 59, 635–641 (2021). https://doi.org/10.1038/s41393-020-00539-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-020-00539-8
- Springer Nature Limited