Abstract
Background
The present study aims to evaluate possible cardiac involvement in juvenile dermatomyositis (JDM) patients by conventional methods and cardiac magnetic resonance imaging (MRI) along with a systematic review of the literature on cardiac features in JDM.
Methods
The study group consisted of JDM patients who underwent cardiac MRI. We conducted a systematic review of the published literature involving JDM patients with cardiac involvement.
Results
In the present study, although baseline cardiologic evaluations including electrocardiography and echocardiography were within normal limits, we showed late gadolinium enhancement on cardiac MRI in 3 of 11 JDM patients. In the literature review, we identified 25 articles related to cardiac involvement in JDM. However, none of them, except one case report, included cardiac MRI of JDM patients.
Conclusion
Cardiac abnormalities have been reported among the less frequent findings in patients with JDM. Cardiovascular complications during the long-term disease course are a leading cause of morbidity and mortality in these patients. Early detection of cardiac involvement by cardiac MRI in patients with JDM and aggressive treatment of them may improve the clinical course of these patients.
Impact
-
The myocardium in patients with JDM may be involved by inflammation.
-
Myocardial involvement may be evaluated by using contrast-enhanced cardiac MRI.
-
This is the first study evaluating cardiac involvement by cardiac MRI in JDM patients.
-
MRI may show early cardiac involvement in patients whose baseline cardiologic evaluations are within normal limits.
-
Early detection of cardiac involvement by cardiac MRI may improve the long-term prognosis of patients with JDM.
Similar content being viewed by others
Introduction
Juvenile dermatomyositis (JDM) is the most common idiopathic inflammatory myopathy presenting with the characteristic rash and proximal muscle weakness during childhood.1 Although proximal muscle weakness and skin findings are the predominant features of the disease, cardiac findings may be accompanied at initiation or during the course of the disease.2 Cardiac involvement in JDM is usually underestimated and studies regarding this issue are scarce. However, cardiac involvement may cause morbidity and mortality in the long-term period. Nonspecific sinus tachycardia is the most frequent cardiac abnormality in JDM. Left ventricular diastolic and systolic dysfunction, hypertension, atherosclerosis, coronary artery disease, and metabolic syndrome may also occur.2 Increasingly, magnetic resonance imaging (MRI) studies begin to take an important place both in the diagnosis of the disease and detection of subclinical organ involvement. Adult studies showed that cardiac MRI may help to detect subclinical myocardial involvement.3,4 However, there is no data about cardiac MRI findings in JDM patients. The present study aims to evaluate possible cardiac involvement in JDM patients by conventional methods and cardiac MRI along with a systematic review of the literature on cardiac features in JDM.
Material and methods
This cross-sectional study was conducted between June 2022 and December 2022. Patients who were followed up with a diagnosis of JDM were enrolled in the study. All patients fulfilled the Bohan and Peter5,6 or EULAR/ACR 2017 classification criteria.7 Demographic data, clinical manifestations, laboratory findings, treatments, and outcomes were obtained from patient charts. The disease activity was evaluated with the Childhood Myositis Assessment Scale (CMAS).8
Initially, a standard 12-lead electrocardiogram (ECG) was performed in all patients. Subsequently, all of them were examined using transthoracic echocardiography (GE Vivid E9 ultrasound system, General Electric Healthcare, Horten, Norway). B-Mode and M-Mode echocardiographic images were obtained. Finally, all patients underwent cardiac MRI in a 1.5 T MR scanner (Philips Gyroscan Intera Master; Philips, Eindhoven, The Netherlands) equipped with a 30 mT/m maximum gradient strength and 150 mT/m/ms slew rate. Data were collected by utilizing a synergy body coin with the patient in the supine position. The vital signs of patients were monitored and recorded throughout the MR examination. The left ventricle (LV) was evaluated in the standard 17-segment model9 (Supplementary Fig. 1). All images were analyzed by an experienced pediatric cardiologist (KB) and radiologist (YA).
The study respected the guidelines of the Helsinki Declaration concerning medical research in humans and received local Ethics Committee approval. Informed consent was obtained from each patient and/or parents.
Systematic review of the literature
A systematic review of the literature on cardiac involvement in JDM was conducted. Relevant documents were searched according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) principles by using Medline and PubMed databases (Supplementary Fig. 2).10 The following keywords were used: (“Juvenile dermatomyositis” OR “JDM” OR “Dermatomyositis, Juvenile” OR “Juvenile Myositis” OR “Myositis, Juvenile”) AND (“cardiac involvement” OR “cardiac manifestation” OR “heart involvement” OR “heart manifestation”). Articles only in English were included in the search. All related articles, including randomized and nonrandomized controlled trials, observational studies (case-control, cohort studies, and case series), and single case reports, were included. Two authors (GA and HES) independently reviewed all possibly eligible studies. Finally, discrepancies were resolved by discussion with the two experienced authors (KB and BS).
Results
Baseline characteristics of our patients
A total of 11 patients were included in the study. Four (36.4%) were male and 7 (63.6%) were female. The median age at evaluation was 11 (7–17) years. The median duration of the disease was 24 (1–102) months. All the patients had heliotrope rash and proximal muscle weakness. Gottron papules were present in 10 patients, calcinosis in 2, and lipodystrophy in 2, concomitantly. The median CMAS score was 35 (22–48) at the time of diagnosis and 52 (41–52) at the time of cardiac evaluation. None of the patients had pulmonary or gastrointestinal involvement. Anti-nuclear antibody (ANA) was positive in 10 patients, anti-transcription intermediary factor 1γ (Anti-TIF1γ) in 2, anti-NXP2 in 1, and anti-Mi2 alfa and beta in 1 patient. Nailfold capillaroscopy findings revealed scleroderma pattern in 5 patients and non-scleroderma pattern in 5 patients (Table 1). None of them had additional cardiac risk factors including smoking, obesity, hypertension, dyslipidemia, and metabolic syndrome.
Cardiac features of our patients
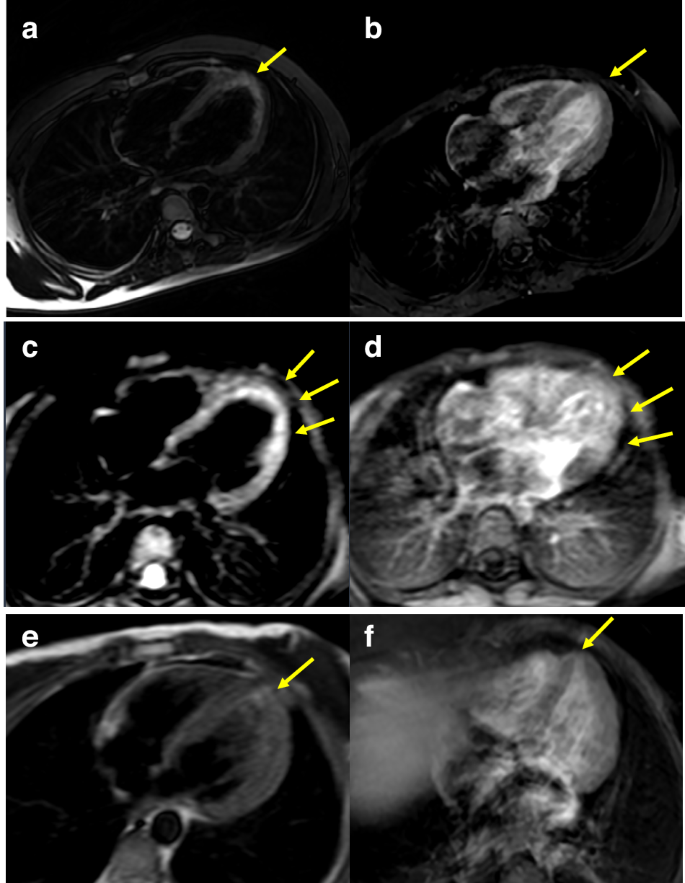
Electrocardiographic examination showed normal sinus rhythm with normal QRS voltage and axis in all patients. None of them had arrhythmia at the time of evaluation. Conventional echocardiographic parameters were within the normal range (Table 1). Three of 11 patients (27.2%) had myocardial late gadolinium enhancement (LGE) on cardiac MRI similar to the appearance in myocarditis. Segment 17 (apex) was involved in 2 patients, and segments 1,2 5,6,9,10,11,14 (basal anterior, basal anteroseptal, basal inferolateral, basal anterolateral, mid inferoseptal, mid inferior, mid inferolateral, and apical septal) were involved in 1 patient (Fig. 1). Furthermore, one patient showed impaired right ventricular ejection fraction (EF) which was not shown in conventional echocardiography. Patients with myocardial late gadolinium enhancement were younger than others, but there were no differences between these two groups in terms of clinical and laboratory findings.
Myocardial images of T2 scans (a, c, e) and late gadolinium enhancement T1 scans (b, d, f) on cardiac MRI. Cardiac MRI axial plane: (a, c, e) are T2 weighted fat saturated images and (b, d, f) are postcontrast late enhancement T1 weighted images. Myocardial edema is seen on segment 17 (apex) on images (a) and (e) and on segments 1, 2, 5, 6, 9, 10, 11, and 14 (basal anterior, basal anteroseptal, basal inferolateral, basal anterolateral, mid inferoseptal, mid inferior, mid inferolateral and apical septal) on the image (c). On postcontrast images (b) (d) and (f) contrast enhancement is seen on the segments parallel with myocardial edema areas on T2W-fat-saturated images.
Cardiac features of patients with JDM in the literature
Supplementary Fig. 2 lists the schematic analyzes of the systematic literature review. At first, 84 related articles were identified. After the title and abstract review, 25 articles were included.11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35 Of these 25 articles, 7 were case report and 18 were observational studies (Table 2). However, none of them, except one, included cardiac MR findings of JDM patients. Stewart et al.32 reported a 14-year-old girl diagnosed with JDM who had first-degree heart block and low voltages on ECG. Her disease evolved into multisystem involvement during hospitalization and treatment. Conduction disturbance progressed to atrial fibrillation. Her echocardiographic examination and cardiac MRI were normal. The disease course of the patient was complicated by macrophage activation syndrome. She was treated successfully with immunosuppressive therapy. Karaca et al.16 reported another case report of conduction disturbance in an 11-year-old boy with JDM. The patient had sinus bradycardia with a heart rate of 40–44 per minute. After treatment with intravenous immunoglobulin (IVIG) and steroids, bradycardia was resolved spontaneously. A case-control study by ref. 13 including 25 patients with JDM reported one patient whose initial presentation was cardiac failure due to myocarditis and another two patients with asymptomatic ECG abnormalities. Ghosh et al.30 reported a 10-year-old girl with a complete heart block secondary to JDM. She had normal systolic and diastolic functions. After treatment with methylprednisolone, ECG returned to sinus rhythm. Another case-control study by ref. 19 reported that diastolic dysfunction detected by tissue Doppler imaging was present in 22% of patients with JDM, pericarditis in 11%, and ECG abnormalities in 17% during 16 years of clinical follow-up. In their ensuing study, ref. 21 reported that patients with JDM had systolic dysfunction represented by decreased long-axis strain on color tissue Doppler echocardiography. Barth et al.23 investigated 55 JDM patients aged 6–48 years using 24-h ambulatory Holter ECG and stated that patients with JDM had decreased heart rate variability (HRV). HRV is related to the heart rate. Insufficient response of inflamed myocardium and conduction tissue to vagal and sympathetic stimulus may be the reason for decreased HRV. Cantez et al.27 reviewed retrospectively 105 patients with JDM. They found that ECG abnormalities (prolonged QTc and PR interval, bundle branch block) were present in 6% of the patients and echocardiographic abnormalities (atrioventricular-semilunar valve regurgitations) in 25%. However, their ECG and echocardiographic findings were mild or trivial and unlikely to be linked to the underlying disease. Diniz et al.31 investigated 35 patients with JDM using conventional 2D and speckle-tracking echocardiography. They found that patients with JDM had lower LV global peak longitudinal systolic strain as well as lower peak circumferential systolic strain values than controls, although all the patients had normal LV ejection fraction (EF) on 2D conventional echocardiography. These results indicate that speckle-tracking echocardiography may be more sensitive than conventional 2D echocardiography in detecting early subclinical myocardial impairment in JDM patients. Diastolic dysfunction represented by low early diastolic tissue velocity (e’) and systolic dysfunction represented by decreased longitudinal strain were reported by ref. 34 including 57 patients with JDM. Patients with JDM generally have subclinical silent cardiac involvement during childhood, although there are few case reports of pericardial tamponade resulting in congestive heart failure which was treated by open drainage11 and ventricular arrhythmias treated by amiodarone.36 Overt cardiovascular disease and death resulting from cardiovascular involvement in JDM are more common in adult populations during long-term follow-up.
Discussion
The myocardium in patients with JDM can be involved by inflammation just as the skeletal muscle. In the present study, we showed myocardial involvement by using contrast-enhanced cardiac MRI in 3 of 11 JDM patients whose baseline cardiologic evaluations including ECG and echocardiography were within normal limits. To our best knowledge, this is the first study evaluating cardiac involvement by cardiac MRI in JDM patients. Adults, with dermatomyositis and polymyositis frequently have cardiac involvement such as conduction abnormalities, atrial and ventricular arrhythmias, pericarditis, and myocarditis.16 Cardiac involvement in JDM may either develop acutely or manifest during the disease course. Systemic vasculopathy and elevated interferon signature play a central role in the pathogenesis of idiopathic inflammatory myopathies. Both factors result in endothelial dysfunction which leads to cardiovascular manifestation during the disease.2 Rhythm and conduction problems and myocarditis are the most observed cardiac abnormalities in the acute phase of the disease. Rider et al.20 evaluated 374 patients with juvenile idiopathic inflammatory myopathy. Abnormal ECG findings were present in 56 (15%) of the patients. However, the study did not specify the abnormal ECG findings. Cantez et al.27 showed prolonged QTc or prolonged PR in 6 of 69 JDM patients. Barth et al.29 demonstrated pathologic ECG findings in 10 (17%) of 58 JDM patients. Furthermore, patients presenting with varying degrees of heart block have been reported.30,32 Besides these acute complications, reduced aerobic capacity, systolic and diastolic dysfunction, and impaired cardiometabolic measures have been demonstrated in long-term follow-up.14,15,19,21,26,28,33,35
Current recommendation guidelines do not provide a recommendation on how often and by which method patients with JDM should be screened for cardiac aspects. Cardiac MRI may be a valuable prospective technique to detect subclinical myocardial involvement. However, it is recommended that cardiac MRI should only be performed in patients with abnormalities on ECG or echocardiography.37 Cardiac MRI studies conducted in recent years have revealed that myocardial involvement is higher than previously thought. For instance, Rosenbohm et al.38 demonstrated signs of myocardial inflammation in 62.3% of 53 polymyositis (PM)/dermatomyositis (DM) patients by cardiac MRI. In the aforementioned study, they reported that the lateral segments of the left ventricle were significantly more often affected than the anterior or septal segments. Another study by ref. 4 showed late gadolinium enhancement (LGE) involving around 5% of the mass of the myocardium in 9 of 16 adult patients with PM/DM. The most affected part of the heart was interventricular septum (n = 8) followed by lateral wall (n = 5), inferior wall (n = 3), apex (n = 2), and anterior wall of the left ventricle (n = 1). They also found that LGE was more common in patients with PM compared to those with DM.4 Diederichsen et al.39 evaluated cardiac abnormalities by cardiac MRI in newly diagnosed, untreated patients with idiopathic inflammatory myopathies. They detected systolic dysfunction by cardiac MRI in 2 of 14 patients with idiopathic inflammatory myopathies. Most recently, ref. 40 suggested that characteristics of cardiac dysfunction may be different between subgroups of idiopathic inflammatory myopathies, and they confirmed their hypothesis by mapping cardiac MRI parameters. They found higher global extracellular volume values in the PM group compared to the DM group. The number of affected ventricular segments in PM patients was higher than in DM patients. In our study, 3 of 11 patients had intramyocardial late gadolinium enhancement. Of them, 2 were diagnosed 3 months ago and the other patient was following for 12 months after the diagnosis. All three patients were in clinically inactive stage.
Due to the rare nature of the disease, there is no randomized controlled study on this subject. Accurate and timely treatment may prevent permanent cardiac damage in patients with JDM. Long-term follow-up of patients with JDM have shown frequent cardiovascular complications such as coronary artery disease, hypertension, atherosclerosis in adolescence and adulthood. Despite the fact that JDM can often cause significant cardiovascular morbidity and mortality during the long-term course of the disease, cardiac involvement is often overlooked at the onset of the disease. A cardiac MRI study by ref. 41 showed that myocardial LGE on contrast-enhanced magnetic resonance imaging of 4 adult patients with idiopathic inflammatory myopathies had markedly regressed after 6 months of corticosteroid and immunosuppressive therapy. They suggested that patients with cardiac involvement may require more aggressive treatments. IVIG is an anti-inflammatory and immunomodulatory drug commonly used in myocarditis to reduce the damage of inflammatory cytokines in cardiac myositis.42 In our study, IVIG was given to 2 patients after cardiac MRI while one could not be treated with IVIG due to financial problems.
Late gadolinium enhancement on cardiac MRI may be seen in various cardiac diseases. Cardiomyopathies, autoimmune and inflammatory diseases, and metabolic and storage diseases cause LGE on cardiac MRI. Accumulation of amyloid fibrils in amyloidosis and glycosphingolipids in Anderson-Fabry disease deteriorate myocardial structure and cause intramyocardial fibrosis. Viral myocarditis, sarcoidosis, and systemic sclerosis are other causes of intramyocardial fibrosis due to inflammation with ischemic damage. Intramyocardial fibrosis and LGE can be found in arrhythmogenic right ventricular cardiomyopathy and dilated or hypertrophic cardiomyopathies.43 Myocardial segments involved by contrast media and the pattern of gadolinium distribution may vary from patient to patient even if they have the same disease. Therefore, the clinical value of LGE distribution patterns in providing precise diagnosis remains to be clarified. In our 2 patients, intramyocardial LGE was present in the left ventricular apex. The remaining patient had more diffuse myocardial contrast enhancement (basal anterior, basal anteroseptal, basal anterolateral, basal inferolateral, mid inferior, mid inferoseptal, mid inferolateral, and apical septal segments).
Although conventional echocardiography and ECG findings were completely normal, myocardial involvement was detected in 3 patients in our study. All patients underwent repeat cardiac MRIs. Intramyocardial LGE was resolved in both patients after 6 months of treatment. A similar result was present in Allanore et al.’s study.41
The small sample size is one of the important limitations of the study. Furthermore, all patients were at different periods of the disease. Another limitation is that our findings are not enough to make a contribution to predictive factors for cardiac involvement. Cardiac MRIs are difficult to implement in childhood patients. Unfortunately, it was inevitable that motion artifacts would occur. Changes seen may be the result of slow flow within the trabeculae and could be artifacts. However, in the present study, complete myocardial involvement suggests actual myocardial involvement rather than an artifact. Furthermore, there was an absence of involvement in the basal segment of the left ventricular free wall. Thus, the present involvement should not be construed as an artifact. Additionally, myocardial suppression was performed via a look-locker program that provides different TI values, and the best one was chosen. However, due to motion artifacts and high cardiac rate, the images included were a little inferior quality. Therefore, we believe that further studies are needed to decide on which JDM patients should be evaluated by cardiac MRI, and further studies in a larger cohort are needed to confirm our results.
Conclusion
Juvenile dermatomyositis is a multisystemic disease characterized by diffuse inflammation of skin and muscles. Cardiac involvement may occur in the course of the disease, however, remains unrecognized due to the lack of overt clinical manifestations in childhood. When considering that long-term cardiovascular complications seen in patients with JDM have significant effects on morbidity and mortality, early detection of cardiac involvement by cardiac MRI and aggressive treatment of these patients may improve the long-term prognosis of patients with JDM.
Data availability
All data generated or analyzed during this study are included in this published article. For additional information concerning these data, the corresponding author can be contacted.
References
McCann, L. J., Livermore, P., Wilkinson, M. G. L. & Wedderburn, L. R. Juvenile dermatomyositis. Where are we now? Clin. Exp. Rheumatol. 40, 394–403 (2022).
Mondal, S., Barman, P. & Vignesh, P. Cardiovascular abnormalities in juvenile dermatomyositis: a scoping review for the clinical rheumatologists. Front. Med. 9, 827539 (2022).
Mavrogeni, S. et al. Myocarditis during acute inflammatory myopathies: evaluation using clinical criteria and cardiac magnetic resonance imaging. Int. J. Cardiol. 164, e3–e4 (2013).
Mavrogeni, S., Douskou, M. & Manoussakis, M. N. Contrast-enhanced CMR imaging reveals myocardial involvement in idiopathic inflammatory myopathy without cardiac manifestations. JACC Cardiovasc. Imaging 4, 1324–1325 (2011).
Bohan, A. & Peter, J. B. Polymyositis and dermatomyositis (first of two parts). N. Engl. J. Med. 292, 344–347 (1975).
Bohan, A. & Peter, J. B. Polymyositis and dermatomyositis (second of two parts). N. Engl. J. Med. 292, 403–407 (1975).
Lundberg, I. E. et al. 2017 European League Against Rheumatism/American College of rheumatology classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups. Arthritis Rheumatol. 69, 2271–2282 (2017).
Huber, A. M. et al. Validation and clinical significance of the childhood myositis assessment scale for assessment of muscle function in the juvenile idiopathic inflammatory myopathies. Arthritis Rheum. 50, 1595–1603 (2004).
Cerqueira, M. D. et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105, 539–542 (2002).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, 71 (2021).
Pereira, R. M., Lerner, S., Maeda, W. T., Goldenstein-Schainberg, C. & Cossermelli, W. Pericardial tamponade in juvenile dermatomyositis. Clin. Cardiol. 15, 301–303 (1992).
Jimenez, C., Rowe, P. C. & Keene, D. Cardiac and central nervous system vasculitis in a child with dermatomyositis. J. Child Neurol. 9, 297–300 (1994).
Shehata, R. et al. Juvenile dermatomyositis: clinical profile and disease course in 25 patients. Clin. Exp. Rheumatol. 17, 115–118 (1999).
Hicks, J. E., Drinkard, B., Summers, R. M. & Rider, L. G. Decreased aerobic capacity in children with juvenile dermatomyositis. Arthritis Rheum. 47, 118–123 (2002).
Takken, T., Spermon, N., Helders, P. J., Prakken, A. B. & Van Der Net, J. Aerobic exercise capacity in patients with juvenile dermatomyositis. J. Rheumatol. 30, 1075–1080 (2003).
Karaca, N. E., Aksu, G., Yeniay, B. S. & Kutukculer, N. Juvenile dermatomyositis with a rare and remarkable complication: sinus bradycardia. Rheumatol. Int. 27, 179–182 (2006).
Sallum, A. M. et al. Risk factors associated with calcinosis of juvenile dermatomyositis. J. Pediatr. 84, 68–74 (2008).
Sakurai, N., Nagai, K., Tsutsumi, H. & Ichimiya, S. Anti-CADM-140 antibody-positive juvenile dermatomyositis with rapidly progressive interstitial lung disease and cardiac involvement. J. Rheumatol. 38, 963–964 (2011).
Schwartz, T., Sanner, H., Husebye, T., Flato, B. & Sjaastad, I. Cardiac dysfunction in juvenile dermatomyositis: a case-control study. Ann. Rheum. Dis. 70, 766–771 (2011).
Rider, L. G. et al. The myositis autoantibody phenotypes of the juvenile idiopathic inflammatory myopathies. Medicine 92, 223–243 (2013).
Schwartz, T., Sanner, H., Gjesdal, O., Flato, B. & Sjaastad, I. In juvenile dermatomyositis, cardiac systolic dysfunction is present after long-term follow-up and is predicted by sustained early skin activity. Ann. Rheum. Dis. 73, 1805–1810 (2014).
Schwartz, T. et al. In active juvenile dermatomyositis, elevated eotaxin and MCP-1 and cholesterol levels in the upper normal range are associated with cardiac dysfunction. Rheumatology 53, 2214–2222 (2014).
Barth, Z. et al. In juvenile dermatomyositis, heart rate variability is reduced, and associated with both cardiac dysfunction and markers of inflammation: a cross-sectional study median 13.5 years after symptom onset. Rheumatology 55, 535–543 (2016).
Khera, R., Khare, S. & Singh, S. K. Acute presentation of juvenile dermatomyositis with subclinical cardiac involvement: a rare case. J. Clin. Diagn. Res. 10, SD01–SD03 (2016).
Saini, I., Kalaivani, M. & Kabra, S. K. Calcinosis in juvenile dermatomyositis: frequency, risk factors and outcome. Rheumatol. Int. 36, 961–965 (2016).
Berntsen, K. S. et al. Submaximal exercise capacity in juvenile dermatomyositis after longterm disease: the contribution of muscle, lung, and heart involvement. J. Rheumatol. 44, 827–834 (2017).
Cantez, S., Gross, G. J., MacLusky, I. & Feldman, B. M. Cardiac findings in children with juvenile Dermatomyositis at disease presentation. Pediatr. Rheumatol. Online J. 15, 54 (2017).
Silverberg, J. I., Kwa, L., Kwa, M. C., Laumann, A. E. & Ardalan, K. Cardiovascular and cerebrovascular comorbidities of juvenile dermatomyositis in US children: an analysis of the National Inpatient Sample. Rheumatology 57, 694–702 (2018).
Barth, Z. et al. Association between nailfold capillary density and pulmonary and cardiac involvement in medium to longstanding juvenile dermatomyositis. Arthritis Care Res. 71, 492–497 (2019).
Ghosh, R. et al. Juvenile dermatomyositis presenting as complete heart block in a 10-year-old girl. Paediatr. Int. Child Health 40, 251–254 (2020).
Diniz, M. F. R. et al. Echocardiographic study of juvenile dermatomyositis patients: new in sights from speckle-tracking-derived strain. Clin. Rheumatol. 40, 1497–1505 (2021).
Stewart, J. A., Price, T., Moser, S., Mullikin, D. & Bryan, A. Progressive, refractory macrophage activation syndrome as the initial presentation of anti-MDA5 antibody positive juvenile dermatomyositis: a case report and literature review. Pediatr. Rheumatol. Online J. 20, 16 (2022).
Witczak, B. N. et al. Body composition in long-standing juvenile dermatomyositis: associations with disease activity, muscle strength and cardiometabolic measures. Rheumatology 61, 2959–2968 (2022).
Witczak, B. N. et al. Associations between cardiac and pulmonary involvement in patients with juvenile dermatomyositis-a cross-sectional study. Rheumatol. Int. 42, 1213–1220 (2022).
Marstein, H. S. et al. Adipose tissue distribution is associated with cardio-metabolic alterations in adult patients with juvenile-onset dermatomyositis. Rheumatology 62, SI196–SI204 (2023).
Singh, S. & Bansal, A. Twelve years experience of juvenile dermatomyositis in North India. Rheumatol. Int. 26, 510–515 (2006).
Zhang, L., Wang, G. C., Ma, L. & Zu, N. Cardiac involvement in adult polymyositis or dermatomyositis: a systematic review. Clin. Cardiol. 35, 686–691 (2012).
Rosenbohm, A. et al. Early diagnosis of cardiac involvement in idiopathic inflammatory myopathy by cardiac magnetic resonance tomography. J. Neurol. 262, 949–956 (2015).
Diederichsen, L. P. et al. Cardiac abnormalities assessed by non-invasive techniques in patients with newly diagnosed idiopathic inflammatory myopathies. Clin. Exp. Rheumatol. 33, 706–714 (2015).
Feng, C. et al. Myocardial involvement characteristics by cardiac MR imaging in patients with polymyositis and dermatomyositis. Rheumatology 61, 572–580 (2022).
Allanore, Y. et al. Effects of corticosteroids and immunosuppressors on idiopathic inflammatory myopathy related myocarditis evaluated by magnetic resonance imaging. Ann. Rheum. Dis. 65, 249–252 (2006).
Canter, C. E. & Simpson, K. E. Diagnosis and treatment of myocarditis in children in the current era. Circulation 129, 115–128 (2014).
Satoh, H. et al. Distribution of late gadolinium enhancement in various types of cardiomyopathies: significance in differential diagnosis, clinical features and prognosis. World J. Cardiol. 6, 585–601 (2014).
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and Affiliations
Contributions
G.A., B.S., E.Z.B., and Y.A. were involved in gathering data, formal analysis, and writing the original draft. N.Ş., Y.E.B., K.U., H.S.G., M.D., T.Ö., M.K., K.B., supported gathering data and contributed to analyzing and interpreting data. H.E.S. conceived the study and revised the manuscript. All authors reviewed and revised the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclosures
No financial disclosures.
Informed Consent Written informed consent was obtained from patients and their parents.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Akgün, G., Sözeri, B., Başar, E.Z. et al. Cardiac evaluation of patients with juvenile dermatomyositis. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03336-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03336-8
- Springer Nature America, Inc.