Abstract
Background
Lactoferrin is an immuno-modulatory nutrient in human milk that may be neuroprotective.
Methods
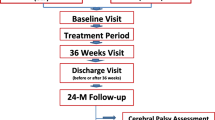
In 36 infants born <32 weeks’ gestation, we sampled human milk at 14 and 28 days of chronologic age and measured lactoferrin by electrochemiluminescence multiplex immunoassay. Using 3T quantitative brain magnetic resonance imaging scans obtained at term equivalent, we estimated total and regional brain volumes. We compared outcomes between infants exposed to low (bottom tertile, range 0.06–0.13 mg/mL) vs. high (top tertile, range 0.22–0.35 mg/mL) lactoferrin using median regression in models adjusted for gestational age, birth weight z-score, sex, and postmenstrual age.
Results
Compared to infants exposed to low lactoferrin, infants exposed to high lactoferrin had 43.9 cc (95% CI: 7.6, 80.4) larger total brain volume, 48.3 cc (95% CI: 12.1, 84.6) larger cortical gray matter, and 3.8 cc (95% CI: 0.7, 7.0) larger deep gray matter volume at term equivalent age. Other regional brain volumes were not statistically different between groups.
Conclusion
Higher lactoferrin exposure during the neonatal hospitalization was associated with larger total brain and gray matter volumes, suggesting that lactoferrin may have potential as a dietary supplement to enhance brain growth in the neonatal intensive care unit setting.
Impact
This study suggests that lactoferrin, a whey protein found in human milk, may be beneficial for preterm infant brain development, and therefore has potential as a dietary supplement in the neonatal intensive care unit setting.

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request and with approval of the IRB.
References
Chawanpaiboon, S. et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob. Health 7, e37–e46 (2019).
Rees, P. et al. Preterm brain injury and neurodevelopmental outcomes: a meta-analysis. Pediatrics 150, e2022057442 (2022).
Aarnoudse-Moens, C. S. H., Weisglas-Kuperus, N., van Goudoever, J. B. & Oosterlaan, J. Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics 124, 717–728 (2009).
Bhutta, A. T., Cleves, M. A., Casey, P. H., Cradock, M. M. & Anand, K. J. S. Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. JAMA 288, 728–737 (2002).
Ramel, S. E. & Georgieff, M. K. Preterm nutrition and the brain. World Rev. Nutr. Diet. 110, 190–200 (2014).
Belfort, M. B. et al. Associations of maternal milk feeding with neurodevelopmental outcomes at 7 years of age in former preterm infants. JAMA Netw. Open 5, e2221608 (2022).
Vohr, B. R. et al. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. Pediatrics 118, e115–e123 (2006).
Vohr, B. R. et al. Persistent beneficial effects of breast milk ingested in the neonatal intensive care unit on outcomes of extremely low birth weight infants at 30 months of age. Pediatrics 120, e953–e959 (2007).
Belfort, M. B. & Inder, T. E. Human milk and preterm infant brain development: a narrative review. Clin. Ther. https://doi.org/10.1016/j.clinthera.2022.02.011 (2022).
Brown Belfort, M. The science of breastfeeding and brain development. Breastfeed. Med. 12, 459–461 (2017).
Ochoa, T. J. & Sizonenko, S. V. Lactoferrin and prematurity: a promising milk protein? Biochem. Cell Biol. 95, 22–30 (2017).
van de Looij, Y. et al. Lactoferrin during lactation protects the immature hypoxic-ischemic rat brain. Ann. Clin. Transl. Neurol. 1, 955–967 (2014).
van de Looij, Y. et al. Nutritional intervention for developmental brain damage: effects of lactoferrin supplementation in hypocaloric induced intrauterine growth restriction rat pups. Front. Endocrinol. 10, 46 (2019).
Chen, Y. et al. Lactoferrin promotes early neurodevelopment and cognition in postnatal piglets by upregulating the BDNF signaling pathway and polysialylation. Mol. Neurobiol. 52, 256–269 (2015).
Li, F. et al. Improved neurodevelopmental outcomes associated with bovine milk fat globule membrane and lactoferrin in infant formula: a randomized, controlled trial. J. Pediatr. 215, 24–31.e8 (2019).
Pammi, M. & Suresh, G. Enteral lactoferrin supplementation for prevention of sepsis and necrotizing enterocolitis in preterm infants. Cochrane Database Syst. Rev. 3, CD007137 (2020).
Al-Alaiyan, S. et al. Effects of probiotics and lactoferrin on necrotizing enterocolitis in preterm infants. Cureus 13, e18256 (2021).
Manzoni, P. et al. Bovine lactoferrin supplementation for prevention of late-onset sepsis in very low-birth-weight neonates: a randomized trial. JAMA 302, 1421–1428 (2009).
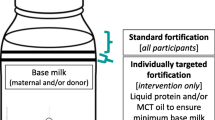
Belfort, M. et al. Macronutrient intake from human milk, infant growth, and body composition at term equivalent age: a longitudinal study of hospitalized very preterm infants. Nutrients 12, 2249 (2020).
Bell, K. A. et al. Associations of growth and body composition with brain size in preterm infants. J. Pediatr. 214, 20–26.e2 (2019).
Bell, K. A. et al. Associations of body composition with regional brain volumes and white matter microstructure in very preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. https://doi.org/10.1136/archdischild-2021-321653 (2022).
Mathur, A. M., Neil, J. J., McKinstry, R. C. & Inder, T. E. Transport, monitoring, and successful brain MR imaging in unsedated neonates. Pediatr. Radio. 38, 260–264 (2008).
Beare, R. J. et al. Neonatal brain tissue classification with morphological adaptation and unified segmentation. Front. Neuroinform. 10, 12 (2016).
Kidokoro, H., Neil, J. J. & Inder, T. E. New MR imaging assessment tool to define brain abnormalities in very preterm infants at term. Am. J. Neuroradiol. 34, 2208–2214 (2013).
Horbar, J. D. The vermont Oxford network: evidence-based quality improvement for neonatology. Pediatrics 103, 350–359 (1999).
Committee Opinion No 700: Methods for Estimating the Due Date. Obstet. Gynecol. 129, e150–e154 (2017).
Fenton, T. R. & Kim, J. H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 13, 59 (2013).
Richardson, D. K., Corcoran, J. D., Escobar, G. J. & Lee, S. K. SNAP-II and SNAPPE-II: Simplified newborn illness severity and mortality risk scores. J. Pediatr. 138, 92–100 (2001).
Duerden, E. G. et al. Early protein intake predicts functional connectivity and neurocognition in preterm born children. Sci. Rep. 11, 4085 (2021).
de Weerth, C. et al. Human milk: from complex tailored nutrition to bioactive impact on child cognition and behavior. Crit. Rev. Food Sci. Nutr. 63, 7945–7982 (2023).
Ochoa, T. J. et al. Randomized controlled trial of bovine lactoferrin for prevention of sepsis and neurodevelopment impairment in infants weighing less than 2000 grams. J. Pediatr. 219, 118–125.e5 (2020).
Bell, K. A. et al. Associations of macronutrient intake determined by point-of-care human milk analysis with brain development among very preterm infants. Children 9, 969 (2022).
Volpe, J. J. Commentary - The late preterm infant: Vulnerable cerebral cortex and large burden of disability. J. Neonatal Perinat. Med. 15, 1–5 (2022).
Volpe, J. J. Dysmaturation of premature brain: importance, cellular mechanisms, and potential interventions. Pediatr. Neurol. 95, 42–66 (2019).
Volpe, J. J. Primary neuronal dysmaturation in preterm brain: important and likely modifiable. J. Neonatal Perinat. Med. 14, 1–6 (2021).
Kitagawa, H. et al. Persorption of bovine lactoferrin from the intestinal lumen into the systemic circulation via the portal vein and the mesenteric lymphatics in growing pigs. J. Vet. Med. Sci. 65, 567–572 (2003).
Kamemori, N. et al. Trans-endothelial and trans-epithelial transfer of lactoferrin into the brain through BBB and BCSFB in adult rats. J. Vet. Med. Sci. 70, 313–315 (2008).
Sriramoju, B., Kanwar, R. K. & Kanwar, J. R. Lactoferrin induced neuronal differentiation: a boon for brain tumours. Int. J. Dev. Neurosci. 41, 28–36 (2015).
Ginet-Puyal, V., van de Looij, Y., Huppi, P. S. & Sizonenko, S. V. O-013 lactoferrin in inflammatory neonatal rat brain injury: a nutrient for neuroprotection? Arch. Dis. Child 99, A26.2–A26 (2014).
Strunk, T. et al. Infection-induced inflammation and cerebral injury in preterm infants. Lancet Infect. Dis. 14, 751–762 (2014).
Kartam, M. et al. Late-onset sepsis in preterm neonates is associated with higher risks of cerebellar hemorrhage and lower motor scores at three years of age. Oman Med. J. 37, e368 (2022).
Garg, P. M. et al. Brain injury in preterm infants with surgical necrotizing enterocolitis: clinical and bowel pathological correlates. Pediatr. Res. 91, 1182–1195 (2022).
ELFIN trial investigators group. Enteral lactoferrin supplementation for very preterm infants: a randomised placebo-controlled trial. Lancet 393, 423–433 (2019).
Ochoa, T. J. et al. Randomized controlled trial of lactoferrin for prevention of sepsis in peruvian neonates less than 2500 g. Pediatr. Infect. Dis. J. 34, 571–576 (2015).
Acknowledgements
Ms. Chloe Sermet provided technical assistance.
Funding
This research was funded by Brigham and Women’s Hospital Department of Pediatric Newborn Medicine, Bill and Melinda Gates Foundation Call to Action Grant (OPP1211778), NICHD (K23 HD091390, A.C.C.L.), Brigham & Women’s Hospital Stork Fund, Brigham Research Institute Fund to Sustain Research Excellence, Harvard Clinical and Translational Science Center (National Center for Advancing Translational Science, grants 1UL1TR001102 and 1UL1TR002541).
Author information
Authors and Affiliations
Contributions
A.M.P.A, N.R.K. and M.B.B conceptualized the study; L.B., S.C., K.B. M.B.B., T.I. and K.D. contributed to data acquisition; S.C. assisted in data analysis; A.M.P.A. wrote the initial manuscript draft; all authors provided critical review and editing of the manuscript and approved the final draft. All authors met the Pediatric Research authorship requirements.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
Parents provided written informed consent for their infant(s) to participate in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Atayde, A.M.P., Kapoor, N.R., Cherkerzian, S. et al. Lactoferrin intake from maternal milk during the neonatal hospitalization and early brain development among preterm infants. Pediatr Res (2024). https://doi.org/10.1038/s41390-023-03002-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-023-03002-5
- Springer Nature America, Inc.
This article is cited by
-
Maternal milk in the NICU: An everyday intervention to improve brain development
Pediatric Research (2024)