Abstract
Background
Sodium bicarbonate (NaHCO3) is no longer recommended by the Neonatal Resuscitation Program (NRP), but is still being used by some neonatologists. The effects of NaHCO3 on cerebral hemodynamics are unclear. Therefore, we investigated the effects of NaHCO3 on cerebral blood flow (CBF) and cerebrovascular function using a newborn piglet model.
Methods
Newborn pigs were anesthetized, intubated, and ventilated. Cranial windows were implanted to evaluate changes in pial arteriolar diameters (PADs) as a surrogate for CBF during a 4-h intravenous infusion of 3% NaHCO3. Cerebrovascular reactivity to vasodilators and vasoconstrictors was investigated during vehicle control and during NaHCO3 infusion.
Results
NaHCO3 infusion caused significant and progressive pial arteriolar vasoconstrictions. During NaHCO3 infusion, cerebrovascular reactivity was preserved. Adding vasodilators decreased cerebral vasoconstriction, while adding vasoconstrictors exaggerated cerebral vasoconstriction.
Conclusions
Intravenous infusion of NaHCO3 over 4 h caused progressive vasoconstriction of pial arterioles. Cerebrovascular function evaluated by the responses of pial arterioles to physiologically relevant vasoconstrictors and vasodilators was preserved during NaHCO3 infusion. A notable additional reduction of PADs was observed during NaHCO3 infusion in the presence of vasoconstrictors. Extrapolating our findings to human neonates should alarm the clinicians that using NaHCO3 in neonates may cause cerebral hypoperfusion.
Impact
-
Cerebral vasoconstriction occurs during slow infusion of 3% diluted NaHCO3.
-
Cerebral vasoconstriction is exaggerated when another vasoconstrictor is added during NaHCO3 infusion.
-
Cerebrovascular function is preserved during NaHCO3 infusion.
-
Clinicians should be aware of the risk of cerebral hypoperfusion with NaHCO3 infusion in vulnerable neonates.
Similar content being viewed by others
Introduction
Metabolic acidosis is a common finding in preterm and asphyxiated infants. For many years, NaHCO3 was recommended for rapid correction of acute metabolic acidosis during cardiopulmonary resuscitation (CPR).1 A presumed benefit for NaHCO3 administration was an improvement in myocardial contractility that could be impaired by acidosis.2,3 However, later it was recognized that NaHCO3 infusion does not correct but instead would worsen the intracellular acidosis when given during CPR.4,5 Therefore, NaHCO3 has been removed from the international guidelines for neonatal resuscitation.6 Despite these findings, European Resuscitation Council and UK guidelines,7 American Heart Association,8 and Neonatal Advanced Life Support6 recommended that slow infusion of diluted NaHCO3 may still be used with caution in persistent metabolic acidosis and prolonged cardiac arrest for all age groups during CPR, provided the infusion follows volume expansion, adequate ventilation, and chest compressions. NaHCO3 may also be used for chronic bicarbonate loss from gastrointestinal or renal routes. The only randomized-controlled trial of NaHCO3 in severely asphyxiated neonates did not show any beneficial effect on the rate of neurological outcomes or the survival of asphyxiated infants.9
In addition to asphyxia, other causes of metabolic acidosis in neonates include clinically significant patent ductus arteriosus (PDA) with a left to right shunt, sepsis, blood loss, hypoxia, hypotension, and metabolic disorders.10 Also, preterm infants within the first few weeks of life may experience metabolic acidosis due to renal tubular immaturity.11 A common first line of intervention practiced by the neonatologists includes improving perfusion by providing more fluids and/or blood, correcting hypoxia, and intervening the left to right shunt through the PDA by adjusting ventilator settings followed by correction of metabolic acidosis.
Although NaHCO3 is no longer recommended for correction of acute metabolic acidosis, >50% of neonatologists still use NaHCO3 with no consensus regarding the severity of metabolic acidosis or dosage, infusion rate, concentration, and dilution of NaHCO3.12,13 Complications associated with the infusion of NaHCO3 include the formation of CO2, worsening intracellular acidosis, myocardial injury, extracellular alkalosis, inhibition of oxygen release to tissues, fluctuation of cerebral blood flow (CBF) and intraventricular hemorrhage (IVH).10 Papile et al.14 and other investigators4,15 reported an increased incidence of IVH in preterm infants following a rapid infusion of hyperosmolar NaHCO3 (4.2–8.4%). Later, that practice was changed to diluting NaHCO3 further and administering it via slow infusion. However, the “slow” rate of infusion that is being practiced varies from 3 min to 4 h.13 As was eloquently stated by Howell,4 “the slow rate of infusion of one study is the rapid infusion of the next.” However, using near-infrared spectroscopy, van Alfen-van der Velden et al.,16 and Katheria et al.,17 showed that NaHCO3 infusion over 30 min may cause transient fluctuations in cerebral and cardiovascular hemodynamics in extremely premature infants with mild metabolic acidosis that could contribute to the development of IVH.
In anticipation of metabolic acidosis in preterm infants, many neonatologists during the first few weeks of life add sodium acetate, citrate, or lactate to total parenteral nutrition (TPN) as a prophylactic measure or infuse NaHCO3 periodically when some degree of metabolic acidosis is observed.13
Although limited information exists regarding the effects of rapid infusion of NaHCO3 on cerebral hemodynamics in asphyxiated infants, the effects of slow infusion of NaHCO3 in infants with mild metabolic acidosis or normal acid–base status is not clear. Rapid infusion of NaHCO3 to correct metabolic acidosis results in the immediate formation of CO2.18 There are vast reports on hypercapnia-induced increased CBF.19,20,21 We hypothesized that slow infusion of NaHCO3 would have similar effects on cerebral hemodynamics as hypercapnia does. To confirm our hypothesis, we used newborn piglets to investigate cerebrovascular hemodynamics in response to slow infusion of diluted 3% NaHCO3. During the 4 h of NaHCO3 infusion, (1) we monitored changes in pial arteriolar diameters (PADs) as a proxy for CBF and (2) evaluated cerebrovascular function by measurement of pial arteriolar responses to added vasogenic stimuli.
Methods
All experiments involving animals were reviewed and approved by the University of Tennessee Health Science Center (UTHSC), Animal Care and Use Committee (ACUC) in accordance with the National Institutes of Health guidelines for the care and use of animals in research. All experiments in the study were conducted according to ARRIVE guidelines 2.0.22 Every effort was made to ensure that any potential discomfort, distress, pain, and injury was minimized.
Subjects
We chose newborn piglets as a model of human infants due to their similarity in cerebrovascular structure and function.23,24 The maturity of piglets’ brain during the first week of life is comparable to human infants at 36–38 weeks of gestational age.24,25 The 2–5-day-old piglets that are used for this experiment are therefore a good representative of late-preterm to early-term infants.21 We believe that the findings from our piglets could be translated to human infants who receive NaHCO3.
Experiments were performed on 2–5-day-old newborn piglets of either sex, with weight ranging from 2 to 3 kg (n = 6). Piglets were purchased from a commercial breeder and Veterinary care was provided by the Department of Comparative Medicine. Piglets were anesthetized with a mixture of ketamine hydrochloride (33 mg/kg, intramuscularly (IM)) and xylazine (3.3 mg/kg, IM) and maintained on α-chloralose (30 mg/kg intravenously (IV) initially, followed by 3 mg/kg every 3 h). The femoral artery and vein were cannulated to monitor blood pressure (BP), to withdraw blood samples for blood gases and pH analysis, and to administer, drugs, anesthetics, and fluids. The trachea was cannulated and intubated; piglets were ventilated mechanically with compressed air using a newborn positive pressure ventilator (Bourne’s BP-200). Body temperature was maintained between 37.0 and 38.0 °C with a servo-controlled heating pad; this is the normal rectal temperature in piglets during the first week of life. Arterial pH, PaCO2, bicarbonate, PaO2 and mean arterial BP were monitored throughout the experiments. Arterial blood gases were measured periodically using a blood gas analyzer (Instrumentation Laboratory, Lexington, MA).
Cranial window
A closed cranial window was implanted over the left parietal cortex of each piglet for measurement of PADs, and for topical application of vasodilators and vasoconstrictors on the cerebral cortex. To implant a closed cranial window, the head was immobilized and the scalp over the left parietal cortex was cut and retracted. A hole, 2 cm in diameter, was made in the skull, and the dura was retracted. A stainless-steel ring with a premounted glass pane was inserted in the hole and sealed with bone wax. The window was cemented in place with dental acrylic, and the space under the window (500 μl) was filled with artificial cerebrospinal fluid (aCSF) composed of (mM) 3.0 KCl, 1.5 MgCl2, 1.5 CaCl2, 132 NaCl, 6.6 urea, 3.7 dextrose, and 24.6 NaHCO3, with an approximate pH of 7.33, PCO2 of 45 mm Hg, and PO2 of 42 mm Hg. The stainless-steel ring has three ports, which allow injecting aCSF, vasodilators, and vasoconstrictors directly under the cranial window and on the cortical surface. Pial arterioles were observed with a dissecting microscope, a television camera mounted on the microscope, and a video monitor. A video micrometer was used to measure the PAD.
Drugs
Two vasodilators (isoproterenol and glutamate) and two vasoconstrictors (endothelin-1 and U46619) were used to evaluate cerebrovascular function. The most appropriate molar concentrations of topical vasogenic agents that would not cause pial arteriolar damage have been established in our laboratory using escalating concentrations for different vasogenic agents.26,27 Isoproterenol (10−6 M) is a smooth muscle-dependent vasodilator that acts via cAMP. Glutamate (10−4 M) is an endothelium- and astrocyte-dependent vasodilator. Endothelin-1 was used at a concentration of 10−8 M, which induces vasoconstriction. U46619 (10−6 M) is a thromboxane A2 (TP) receptor agonist. All drugs and other compounds were purchased from Sigma Chemical Company (St. Louis, MO).
In neonates, NaHCO3 with osmolality at 4.2% (0.5 meq/ml) concentration is commonly used and administered at 2 meq/kg over 3–30 min.28 We used 3% (0.35 meq/ml) NaHCO3 solution infused at a rate of 1 meq/kg/h. Piglets also received IV infusion of 0.9% NaCl/5% dextrose (0.4 ml/kg/h) for the duration of experiments.
Protocol
Experiment in each piglet was performed in two phases: a pre-NaHCO3 (vehicle control) phase, followed by a NaHCO3 infusion phase. This approach allowed each piglet to act as its own control. After confirming that the BP and body temperature were within normal range, we made ventilator adjustments to ensure the blood gases were in the normal range (pH 7.35–7.45, PaCO2 35–45 mm Hg, PaO2 75–85 mm Hg). A small pial arteriole (40–60 μm) and a larger pial arteriole (80–100 μm) were identified in each piglet and baseline diameters were measured. The same pial arterioles were observed for the entire duration of the experiment in each piglet.
Cerebrovascular responses to vasodilators and vasoconstrictors were evaluated in six piglets during the first phase (pre-NaHCO3/vehicle control) and during the second phase (NaHCO3 infusion). Each vasodilator and vasoconstrictor were separately infused under the cranial window and remained there for 5 min, and maximum PAD responses were documented. After 5 min and before the next challenge, the space under the cranial window was flushed gently and repeatedly with aCSF to allow the return of PADs to the baseline level, which usually takes 10–15 min.
The NaHCO3 phase (second phase) was started at the end of the pre-NaHCO3 phase (vehicle control) and following the return of PADs to the baseline diameters. For this phase, 3% NaHCO3 (1:2 dilution) solution was infused via femoral vein continuously at 1 meq/kg/h for 4 h. Pial arterioles that constricted during NaHCO3 infusion were considered as the new baseline diameter and percent changes in PAD in response to vasogenic stimuli were calculated based on the new baseline. Similar to the pre-NaHCO3 infusion (vehicle control) phase, each vasodilator and vasoconstrictor were separately infused under the cranial window at 1, 2, and at 3 h. Changes in PAD were documented every min for 5 min. The maximum PAD response was selected for each vasoactive stimulus at 1, 2, and 3 h during NaHCO3 infusion.
Data analysis
Values are reported as the mean ± SEM. Proper sample sizes were calculated for a power of 0.8 in all tests. Comparisons among different time points (1, 2, and 3 h) were performed using one-way analysis of variance with repeated measures followed by Dunnett’s multiple comparison test. The maximum cerebrovascular responses to various vasodilators and vasoconstrictors were calculated from the respective baseline PADs that were obtained during NaHCO3 infusion and again from the pre-NaHCO3 (vehicle control) baseline PADs. Comparisons were made using a paired t test. A p value <0.05 was considered significant.
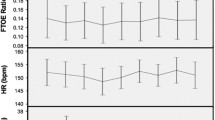
Results
Baseline arterial pH, PaCO2, bicarbonate, PaO2, and mean arterial BP were within the normal range during phase one (pre-NaHCO3/vehicle control). During phase two (NaHCO3 infusion), pH increased from 7.33 ± 0.02 to 7.40 ± 0.01 (p < 0.05), and PaCO2 increased from 43.4 ± 2 to 56.8 ± 2.8 mm Hg (p < 0.05). The bicarbonate level increased from 24.1 ± 0.8 to 36.2 ± 0.6 mmol/l (p < 0.05). PaO2 remained in the normal range (85–90 mm Hg). The mean BP decreased from 58 to 52 mm Hg at 3 h (p < 0.05) (Fig. 1).
Changes in arterial blood pH (a), PCO2 (b), bicarbonate (c), PO2 (d), and mean blood pressure (e) measured pre-NaHCO3 (vehicle control) and during NaHCO3 infusion at different time points (1, 2, and 3 h). *P < 0.05 compared to pre-NaHCO3 (vehicle control) infusion. N = 6 piglets. Values are mean ± SEM.
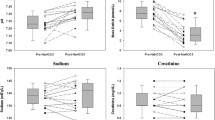
Pial arteriolar constriction was noted during NaHCO3 infusion in both small and larger arterioles. Pial arteriolar constriction progressively worsened over the 3-h period in small arterioles from 63 to 48 μm (p < 0.05) and in large arterioles from 110 to 87 μm (p < 0.05) (Fig. 2).
To evaluate cerebrovascular function during NaHCO3 infusion, we examined responses to vasodilators and vasoconstrictors and calculated percent changes in PAD from the immediate preintervention with vasogenic stimuli PAD (new baseline).
During the vehicle control phase, topical application of vasodilators (glutamate 10−4 M and isoproterenol 10−6 M) on the cerebral cortex caused vasodilation of pial arterioles. PAD responses to the vasodilators during the NaHCO3 infusion phase were similar to the vehicle control (16–20% increase) (Fig. 3). Topical application of vasoconstrictors (endothelin 10−8 M and U46619 10−6 M) during NaHCO3 infusion caused vasoconstriction of pial arterioles that were again similar to the responses observed during the vehicle control phase (12–14% decrease) (Fig. 4).
Pial arteriolar responses to glutamate 10−4 M (a) and isoproterenol 10−6M (b). These vasodilators were topically applied to the cerebral cortex during pre-sodium bicarbonate (vehicle control) infusion (open bar) and again during continuous sodium bicarbonate infusion at 1, 2, and 3 h of infusion (closed bar). The PADs are expressed as the % changes from the corresponding baseline control level (*p < 0.05). N = 6 piglets; N = 12 arterioles. Values are mean ± SEM.
Pial arteriolar responses to endothelin-1 10−8 M (a) and U46619 10−6M (b). These vasoconstrictors were topically applied to the cerebral cortex during pre-sodium bicarbonate (vehicle control) infusion (open bar) and again during continuous sodium bicarbonate infusion at 1, 2, and 3 h of infusion (closed bar). The PADs are expressed as the % changes from the corresponding baseline control level (*p < 0.05). N = 6 piglets; N = 12 arterioles. Values are mean ± SEM.
Since cerebrovascular function was preserved, we evaluated pial arteriolar responses to vasodilators and vasoconstrictors during NaHCO3 infusion relative to baseline vehicle control (pre-NaHCO3). During NaHCO3 infusion, adding vasodilators did not reverse the NaHCO3-induced vasoconstriction, but ameliorated pial arteriolar vasoconstriction by 15% (p < 0.05) (Fig. 5). However, the addition of vasoconstrictors exacerbated the reduction of PADs that were already reduced by the presence of NaHCO3, thus overall vasoconstriction was increased by 15% (p < 0.05) (Fig. 6).
Percent changes from baseline pial arteriolar diameters (vehicle control) in response to vasodilators during pre-NaHCO3 infusion (black bar), in response to continuous NaHCO3 infusion alone (closed bar), and when NaHCO3 supplemented with vasodilators glutamate 10−4 M (a) and isoproterenol 10−6 M (b) (open bar). *P < 0.05: percent changes from the baseline PAD during NaHCO3 infusion. **P <0.05: percent changes from the baseline PAD when NaHCO3 was supplemented with vasodilators. N = 6 piglets; N = 12 arterioles. Values are mean ± SEM.
Percent changes from baseline pial arteriolar diameters (vehicle control) in response to vasoconstrictors during pre-NaHCO3 infusion (black bar), in response to continuous NaHCO3 infusion alone (closed bar), and when NaHCO3 supplemented with vasoconstrictors endothelin-1 10−8 M (a) and U46619 10−6 M (b) (open bar). *P < 0.05: percent changes from the baseline PAD during NaHCO3 infusion. **P < 0.05: percent changes from the baseline PAD when NaHCO3 was supplemented with vasoconstrictors. N = 6 piglets; N = 12 arterioles. Values are mean ± SEM.
Discussion
The novel findings of the present study include (1) NaHCO3 infusion over a 4-h period caused progressive cerebral vasoconstriction; (2) during NaHCO3 infusion, cerebral vascular reactivity to vasodilators and vasoconstrictors was preserved, suggesting that cerebrovascular function remained intact; and (3) during NaHCO3 infusion, added vasodilators dampened cerebral vasoconstriction, while added vasoconstrictors exaggerated cerebral vasoconstriction. These findings suggest that NaHCO3 infusion may cause cerebral hypoperfusion specifically when another vasoconstrictor is administered simultaneously.
For many years, NaHCO3 has been used for CPR and for acute correction of metabolic acidosis in newborn infants.10 NaHCO3 administration was considered beneficial during resuscitation because it was believed to improve myocardial contractility that could be impaired due to systemic acidosis.3 However, based on multiple studies showing a lack of benefits, NaHCO3 has been removed from the list of medications used for CPR.6 Recently, a recommendation for correction of metabolic acidosis due to asphyxia with NaHCO3 has been revised from rapid to slower infusion.6,7,8 Non-asphyxia-related metabolic acidosis in infants continues to be treated with slow infusion of NaHCO3 or other buffering agents.13 NaHCO3 has been used in various clinical scenarios in the neonatal intensive care unit (NICU). Our newborn piglet model is designed to reproduce clinical conditions related to mild metabolic acidosis (pH 7.30) and normal base deficit (BE −4) in neonates,12,13 as well as in anticipation of the development of metabolic acidosis in preterm infants with normal acid–base status.
The effects of NaHCO3 on cerebral hemodynamics
The effects of NaHCO3 on CBF have been attributed to various mechanisms, including (1) transient conversion of NaHCO3 to CO2 that readily crosses the blood–brain–barrier (BBB);29 (2) disruption of the BBB and passage of CO2, H+, and possibly HCO3 to the perivascular space;30,31 (3) changes in the cerebral perivascular fluid (CSF) pH;32,33 (4) direct influence of arterial HCO3 on the contractility of vascular smooth muscle cells;34 and (5) changes in intracellular pH due to accumulation of CO2.35
In 1968, Lassen36 reported that the pH of CSF that covers cerebral arterioles is the main factor that controls CBF. Later, Kontos et al.32 showed that direct changes in the pH of cranial window fluid (aCSF) in adult cats alter the cerebrovascular tone, independent of systemic HCO3 or CO2 levels. In addition, Britton et al.33 showed that ventriculo-cisternal perfusion of aCSF with different pH values caused significant changes in CBF in adult dogs. Collectively, these findings suggest CSF pH is important for the regulation of CBF. Therefore, low CSF pH is expected to cause cerebral vasodilation and increased CBF, whereas high CSF pH is expected to cause cerebral vasoconstriction and decreased CBF. Although we mixed the vasogenic stimuli in aCSF with normal pH, NaHCO3-induced vasoconstriction persisted. Most likely, other mechanisms besides perivascular pH are involved in pial arteriolar constriction during NaHCO3 infusion.29,35 We assume that, if alkalotic aCSF was infused during the experiment, the vasoconstrictive responses would have been more significant.
In addition to the possibility of developing IVH in preterm infants due to rapid infusion of hyperosmolar NaHCO3,14,15 there are other concerns such as cerebral hypoperfusion and ischemia. Lou et al.37 administered 1–8 meq/kg of 4.2% NaHCO3 at 0.5 meq/min to preterm infants with respiratory distress and measured CBF by the Xe-133 clearance technique before and 5 min after NaHCO3 administration. They observed significantly decreased CBF and, in some cases, even severe cerebral ischemia. Therefore, Lou et al.37 concluded that “infusion of Na bicarbonate should be avoided, if at all possible, in hypotensive postnatal distress.”
The effects of NaHCO3 infusion on PAD: a surrogate representative for CBF
There are conflicting findings regarding the effects of NaHCO3 infusion on CBF that may reflect differences between studies, such as differences in study subjects, metabolic acidosis severity, NaHCO3 dilution, and CBF measurement methods. Caldwell et al.38 administered 8.4% NaHCO3 in healthy adult males and measured CBF via Doppler ultrasound of the internal carotid artery and vertebral artery (large arteries), which showed that CBF increased by 7% following NaHCO3 infusion. However, large arteries are capacitance vessels and do not control CBF and cerebral autoregulation. Instead, these arteries show changes in blood volume.
To evaluate cerebral vascular effects of NaHCO3, we focused on pial arterioles that are considered resistance vessels since they are major contributors to controlling CBF and cerebral autoregulation.39 Blood flow is regulated by vascular resistance. Vascular resistance is inversely proportional to the radius of the vessels to the fourth power (Poiseuille’s equation: R = μL/r4). Thus, minor changes in PAD would have major effects on CBF.40 Therefore, changes in PAD can be used as a proxy for changes in CBF, granted the cerebrovascular function remains intact.41,42,43 Therefore, if the cerebrovascular function is intact, many clinical conditions could influence the NaHCO3-associated cerebral vasoconstriction. Our findings of pial arteriolar constriction with the infusion of NaHCO3 in piglets with normal acid–base status are consistent with findings by Lou et al.,37 who observed cerebral hypoperfusion with NaHCO3 infusion on stressed preterm infants with metabolic acidosis.
Although PaCO2 increased from 43 to 57 mm Hg, during NaHCO3 infusion in our piglets, the expected hypercapnia-induced cerebrovascular dilation did not occur. Instead, we observed progressive constriction of pial arterioles (both small and larger arterioles). Similarly, Arvidsson et al.31 showed that intravenous infusion of alkali in hypercapnic dogs caused a significant reduction in CBF. These authors suggested hypercapnia would facilitate bicarbonate passage through the BBB, resulting in increased perivascular pH and cerebral vasoconstriction. Moreover, Hoiland et al.43 reported that regulation of CBF is dependent not only on extracellular pH within the perivascular space but also on its relationship with PaCO2. Although HCO3 and H+ do not readily cross the BBB, systemic changes in PaCO2 may indirectly affect extravascular pH via CSF.44 Increased cerebral vasoconstriction over 4 h in our piglets likely can be explained by slow changes in CSF extracellular pH in response to HCO3 accumulation in CSF.45,46
During chronic metabolic acidosis and alkalosis, the CSF pH that controls CBF is well regulated irrespective of marked changes in arterial pH.47 However, with acute changes in arterial pH such as those in our experiment, it is unclear whether cerebral vasoconstriction would have continued over a longer duration or would have normalized upon discontinuation of NaHCO3.
Cerebrovascular function during NaHCO3 infusion
The reassuring findings of our study were that although pial arterioles were constricted during induced acute metabolic alkalosis (NaHCO3 infusion), cerebrovascular functions were preserved with normal responses to vasodilators and vasoconstrictors. Consistent with our findings, Caldwell et al.38 showed responses to hypercapnia were preserved during acute metabolic alkalosis in healthy adult humans. In contrast, Pannier et al.45 observed decreased vasodilatory responses to hypercapnia during a 1 h NaHCO3 infusion in cats.
In our piglets, added vasodilators did not reverse the vasoconstriction that was induced by NaHCO3 infusion, but rather diminished pial arteriolar vasoconstriction. Importantly, we observed worsening of cerebral vasoconstriction when a vasoconstrictor was added during NaHCO3 infusion. These findings are concerning since vasopressors are commonly administered to sick infants in the NICU during the correction of a severe metabolic acidosis of various causes.
Limitation of our study
Our study has several limitations. First, we administered NaHCO3 to piglets with normal acid–base status and not severe metabolic acidosis. Therefore, our model does not represent severe metabolic acidosis due to asphyxia or other serious clinical conditions. However, in anticipation of metabolic acidosis in preterm infants, many neonatologists add sodium acetate or sodium citrate to TPN as a prophylactic measure during the early days of life or intermittently administer NaHCO3 for correction of mild metabolic acidosis. In addition, based on a recent survey of European neonatologists, there is no specified pH threshold for NaHCO3 infusion.13 Second, our piglet model does not represent early preterm infants since the maturity of piglets’ brain during the first week of life is comparable to human infants at 36–38 weeks of gestational age.22,23,24 Third, we did not monitor PADs beyond the 4-h infusion or after discontinuation of NaHCO3. Thus, we do not know if vasoconstriction would have remained, worsened, or resolved after discontinuation of NaHCO3 infusion. Finally, we did not compare pial arteriolar responses to other buffering agents such as Na acetate or Na citrate, which are converted in the body to bicarbonate, to determine if they would have similar effects as NaHCO3 if administered over 4 h.
Conclusion
Our findings indicate that NaHCO3 infusion causes cerebral vasoconstriction, but does not alter cerebrovascular function in newborn piglets with normal acid–base status. During NaHCO3 infusion, the constricted cerebral vessels are capable of further constriction when exposed to additional cerebral vasoconstrictors. Preterm infants who receive NaHCO3 may also receive vasopressors that can cause worsening cerebral vasoconstriction. Thus, we suggest that the use of NaHCO3 should be avoided if at all possible since it may cause cerebral hypoperfusion. Although Aschner and Poland called NaHCO3 “basically useless therapy,”10 we may consider “NaHCO3 to be a potentially harmful therapy in preterm infants if it is not used cautiously.”
References
Bloom, R. Textbook of Neonatal Resuscitation (American Heart Association, 1987).
Gaskell, W. H. On the tonicity of the heart and blood vessels. J. Physiol. 3, 48–92 16 (1880).
Orchard, C. H. & Kentish, J. C. Effects of changes of pH on the contractile function of cardiac muscle. Am. J. Physiol. 258, C967–C981 (1990).
Howell, J. H. Sodium bicarbonate in the perinatal setting–revisited. Clin. Perinatol. 14, 807–16. (1987).
Kette, F., Weil, M. H., von Planta, M., Gazmuri, R. J. & Rackow, E. C. Buffer agents do not reverse intramyocardial acidosis during cardiac resuscitation. Circulation 81, 1660–1666 (1990).
Niermeyer, S. et al. International Guidelines for Neonatal Resuscitation: An excerpt from the Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care: International Consensus on Science. Contributors and Reviewers for the Neonatal Resuscitation Guidelines. Pediatrics 106, E29 (2000).
Madar, J. et al. European Resuscitation Council Guidelines 2021: Newborn resuscitation and support of transition of infants at birth. Resuscitation 161, 291–326 (2021).
John, K. Textbook of Neonatal Resuscitation 5th edn (American Heart Association & American Academy of Pediatrics, 2006).
Lokesh, L., Kumar, P., Murki, S. & Narang, A. A randomized controlled trial of sodium bicarbonate in neonatal resuscitation-effect on immediate outcome. Resuscitation 60, 219–223 (2004).
Aschner, J. L. & Poland, R. L. Sodium bicarbonate: basically useless therapy. Pediatrics 122, 831–835 (2008).
Bourchier, D. & Weston, P. J. Metabolic acidosis in the first 14 days of life in infants of gestation less than 26 weeks. Eur. J. Pediatr. 174, 49–54 (2015).
Saenz, P. et al. A survey of intravenous sodium bicarbonate in neonatal asphyxia among European neonatologists: gaps between scientific evidence and clinical practice. Neonatology 99, 170–176 (2011).
Massenzi, L., Aufieri, R., Donno, S., Agostino, R. & Dotta, A. Neonatal Pharmacotherapy Study Group of the Italian Society of N. Use of intravenous sodium bicarbonate in neonatal intensive care units in Italy: a nationwide survey. Ital. J. Pediatr. 47, 63 (2021).
Papile, L. A., Burstein, J., Burstein, R., Koffler, H. & Koops, B. Relationship of intravenous sodium bicarbonate infusions and cerebral intraventricular hemorrhage. J. Pediatr. 93, 834–836 (1978).
Simmons, M. A., Adcock, E. W. 3rd, Bard, H. & Battaglia, F. C. Hypernatremia and intracranial hemorrhage in neonates. N. Engl. J. Med. 291, 6–10 (1974).
van Alfen-van der Velden, A. A. et al. Effects of rapid versus slow infusion of sodium bicarbonate on cerebral hemodynamics and oxygenation in preterm infants. Biol. Neonate 90, 122–127 (2006).
Katheria, A. C. et al. Hemodynamic effects of sodium bicarbonate administration. J. Perinatol. 37, 518–20. (2017).
Singer, R. B., Deering, R. C. & Clark, J. K. The acute effects in man of a rapid intravenous infusion of hypertonic sodium bicarbonate solution. II. Changes in respiration output carbon dioxide. J. Clin. Invest. 35, 245–253 (1956).
Parfenova, H. & Leffler, C. W. Effects of hypercapnia on prostanoid and cAMP production by cerebral microvascular cell cultures. Am. J. Physiol. 270, C1503–C1510 (1996).
Nnorom, C. C. et al. Contributions of KATP and KCa channels to cerebral arteriolar dilation to hypercapnia in neonatal brain. Physiol. Rep. 2 (2014).
Pourcyrous, M., Chilakala, S., Elabiad, M. T., Parfenova, H. & Leffler, C. W. Does prolonged severe hypercapnia interfere with normal cerebrovascular function in piglets? Pediatr. Res. 84, 290–295 (2018).
Percie du Sert, N. et al. The ARRIVE guidelines 2.0: updated guidelines for reporting animal research. J. Cereb. Blood Flow Metab. 40, 1769–1777 (2020).
Dobbing, J. & Sands, J. Comparative aspects of the brain growth spurt. Early Hum. Dev. 3, 79–83 (1979).
Buckley, N. M., Gootman, P. M., Yellin, E. L. & Brazeau, P. Age-related cardiovascular effects of catecholamines in anesthetized piglets. Circ. Res. 45, 282–292 (1979).
Pond, W. G. & Haupt, K. A. The Biology of the Pig (Cornell University Press, 1978).
Armstead, W. M., Mirro, R., Leffler, C. W. & Busija, D. W. Influence of endothelin on piglet cerebral microcirculation. Am. J. Physiol. 257, H707–H710 (1989).
Busija, D. W., Leffler, C. W. & Beasley, D. G. Effects of leukotrienes C4, D4, and E4 on cerebral arteries of newborn pigs. Pediatr. Res. 20, 973–976 (1986).
Laptook, A. R. The effects of sodium bicarbonate on brain blood flow and O2 delivery during hypoxemia and acidemia in the piglet. Pediatr. Res. 19, 815–819 (1985).
Kety, S. S. & Schmidt, C. F. The effects of altered arterial tensions of carbon dioxide and oxygen on cerebral blood flow and cerebral oxygen consumption of normal young men. J. Clin. Invest. 27, 484–492 (1948).
Rapoport, S. I., Hori, M. & Klatzo, I. Testing of a hypothesis for osmotic opening of the blood-brain barrier. Am. J. Physiol. 223, 323–331 (1972).
Arvidsson, S., Haggendal, E. & Winso, I. Influence on cerebral blood flow of infusion of sodium bicarbonate during respiratory acidosis and alkalosis in the dog. Acta Anaesthesiol. Scand. 25, 146–52. (1981).
Kontos, H. A., Raper, A. J. & Patterson, J. L. Analysis of vasoactivity of local pH, PCO2 and bicarbonate on pial vessels. Stroke 8, 358–360 (1977).
Britton, S. L., Lutherer, L. O. & Davies, D. G. Effect of cerebral extracellular fluid acidity on total and regional cerebral blood flow. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 47, 818–26 (1979).
Boedtkjer, E., Hansen, K. B., Boedtkjer, D. M. B., Aalkjaer, C. & Boron, W. F. Extracellular HCO3- is sensed by mouse cerebral arteries: regulation of tone by receptor protein tyrosine phosphatase gamma. J. Cereb. Blood Flow Metab. 36, 965–980 (2016).
Nakashima, K. et al. The effect of sodium bicarbonate on CBF and intracellular pH in man: stable Xe-CT and 31P-MRS. Acta Neurol. Scand. Suppl. 166, 96–98 (1996).
Lassen, N. A. Brain extracellular pH: the main factor controlling cerebral blood flow. Scand. J. Clin. Lab. Invest. 22, 247–251 (1968).
Lou, H. C., Lassen, N. A. & Fris-Hansen, B. Decreased cerebral blood flow after administration of sodium bicarbonate in the distressed newborn infant. Acta Neurol. Scand. 57, 239–247 (1978).
Caldwell, H. G. et al. Arterial carbon dioxide and bicarbonate rather than pH regulate cerebral blood flow in the setting of acute experimental metabolic alkalosis. J. Physiol. 599, 1439–57. (2021).
Greisen, G. Autoregulation of cerebral blood flow in newborn babies. Early Hum. Dev. 81, 423–428 (2005).
Pryds, A., Tonnesen, J., Pryds, O., Knudsen, G. M. & Greisen, G. Cerebral pressure autoregulation and vasoreactivity in the newborn rat. Pediatr. Res. 57, 294–298 (2005).
Leffler, C. W., Beasley, D. G. & Busija, D. W. Cerebral ischemia alters cerebral microvascular reactivity in newborn pigs. Am. J. Physiol. 257, H266–H271 (1989).
Pourcyrous, M., Parfenova, H., Bada, H. S., Korones, S. B. & Leffler, C. W. Changes in cerebral cyclic nucleotides and cerebral blood flow during prolonged asphyxia and recovery in newborn pigs. Pediatr. Res. 41, 617–23. (1997).
Hoiland, R. L., Fisher, J. A. & Ainslie, P. N. Regulation of the cerebral circulation by arterial carbon dioxide. Compr. Physiol. 9, 1101–54. (2019).
Messeter, K. & Siesjo, B. K. Regulation of the CSF pH in acute and sustained respiratory acidosis. Acta Physiol. Scand. 83, 21–30 (1971).
Pannier, J. L., Demeester, G. & Leusen, I. The influence of nonrespiratory alkalosis on cerebral blood flow in cats. Stroke 5, 324–329 (1974).
Abeysekara, S. et al. Infusion of sodium bicarbonate in experimentally induced metabolic acidosis does not provoke cerebrospinal fluid (CSF) acidosis in calves. Can. J. Vet. Res. 76, 16–22 (2012).
Siesjo, B. K. Symposium on acid-base homeostasis. The regulation of cerebrospinal fluid pH. Kidney Int. 1, 360–374 (1972).
Acknowledgements
We thank Courtney Bricker-Anthony for editorial assistance and Alex Fedinec for technical assistance.
Funding information
This work was supported by the NIH R01NS101717 (to H.P.) and R01NS105655 (to H.P.).
Author information
Authors and Affiliations
Contributions
S.K.C. performed the animal experiments, carried out the initial and final analysis, made the figures, drafted the initial manuscript, and reviewed the final manuscript. H.P. coordinated experiments, supervised data collection, carried out the initial and the final analysis, and reviewed the final manuscript. M.P. conceptualized and designed the study, supervised data collection, reviewed the first draft, and revised the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chilakala, S.K., Parfenova, H. & Pourcyrous, M. The effects of sodium bicarbonate infusion on cerebrovascular function in newborn pigs. Pediatr Res 92, 729–736 (2022). https://doi.org/10.1038/s41390-021-01876-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01876-x
- Springer Nature America, Inc.