Abstract
Background
Nitric oxide (NO) plays an important role in normal postnatal transition. Our aims were to determine whether adding inhaled NO (iNO) decreases supplemental oxygen exposure in preterm infants requiring positive pressure ventilation (PPV) during resuscitation and to study iNO effects on heart rate (HR), oxygen saturation (SpO2), and need for intubation during the first 20 min of life.
Methods
This was a pilot, double-blind, randomized, placebo-controlled trial. Infants 25 0/7–31 6/7 weeks’ gestational age requiring PPV with supplemental oxygen during resuscitation were enrolled. PPV was initiated with either oxygen (FiO2–0.30) + iNO at 20 ppm (iNO group) or oxygen (FiO2–0.30) + nitrogen (placebo group). Oxygen was titrated targeting defined SpO2 per current guidelines. After 10 min, iNO/nitrogen was weaned stepwise per protocol and terminated at 17 min.
Results
Twenty-eight infants were studied (14 per group). The mean gestational age in both groups was similar. Cumulative FiO2 and rate of exposure to high FiO2 (>0.60) were significantly lower in the iNO group. There were no differences in HR, SpO2, and need for intubation.
Conclusions
Administration of iNO as an adjunct during neonatal resuscitation is feasible without side effects. It diminishes exposure to high levels of supplemental oxygen.
Similar content being viewed by others
Introduction
Survival of extremely premature babies has improved in the past two decades.1,2,3 However, morbidities associated with prematurity, such as necrotizing enterocolitis (NEC), intraventricular hemorrhage (IVH), patent ductus arteriosus (PDA), neurodevelopmental delay, bronchopulmonary dysplasia (BPD), and retinopathy of prematurity (ROP) present a significant burden for surviving premature infants.1,2,3 Of these comorbidities, the latter two are associated with oxygen use and mechanical ventilation.4,5,6,7 At present, optimal inspired oxygen concentration for premature infants during resuscitation is still uncertain. Current resuscitation guidelines recommend maintaining set oxygen targets by minimizing oxygen exposure after birth.8,9 Administration of high levels of oxygen during resuscitation to maintain target oxygen saturation may be harmful, due to the generation of reactive oxygen species.10
Transition from fetal to neonatal circulation involves a complex sequence of events during which pulmonary vascular resistance drops dramatically in association with an increase in peripheral vascular resistance.11,12,13,14 This cardiovascular adaptation at birth is facilitated by the release of cortisol, catecholamines, and vasodilator mediators, such as nitric oxide (NO) and prostaglandin (PG) I2.15,16,17,18,19 NO is particularly important as it regulates pulmonary vascular tone at birth.20,21
NO is released from the vascular endothelium and plays a critical role in vascular adaptation during the perinatal period.22,23 It is a powerful vasodilator, regulates pulmonary vascular tone, facilitates fluid clearance from the alveoli, and secures the integrity of the endothelial barrier.22,23 It activates vascular smooth muscle cell soluble guanylate cyclase and cyclic guanosine monophosphate production, leading to pulmonary smooth muscle relaxation, through the regulation of intracellular calcium levels.23,24 The major emphasis of current resuscitation guidelines is on ventilation, with the expectation that pulmonary vasodilation will follow.8,9 Indeed, ventilation of the lungs with air alone promotes reduction in pulmonary vascular resistance by release of vasoactive mediators.14 However, these guidelines do not provide any additional steps to facilitate pulmonary vasodilation other than oxygen administration and lung expansion.
Both animal and human studies have shown that inhaled NO (iNO) decreases pulmonary vascular resistance during hypoxemia.25,26 Therefore, in premature infants needing resuscitation, adding iNO during resuscitation may decrease pulmonary vascular resistance, improve ventilation perfusion mismatch, and reduce the need for excess oxygen. In hypoxic near-term lamb model, exposure to 20 ppm of iNO at birth decreased pulmonary vascular resistance and resulted in an increase in pulmonary blood flow.22 iNO administration during resuscitation has never been attempted in human newborns.
The objective of this study was to test the hypothesis that iNO, added as an adjunct to positive pressure ventilation (PPV), may reduce the need for supplemental oxygen and may accelerate the transition to neonatal circulation during resuscitation in premature infants.
Our primary aims were: (1) to determine whether adding iNO decreases supplemental oxygen exposure in preterm infants requiring PPV during resuscitation as per NRP guidelines and (2) to compare heart rate (HR), oxygen saturation, and need for intubation between the two groups during the first 20 min of life.
Our secondary aims were: (1) to evaluate the effect of iNO during resuscitation on immediate postnatal respiratory support in the first 24 h and (2) to evaluate the effect of iNO on the incidence of IVH, NEC, late-onset sepsis, PDA requiring treatment, ROP, BPD, mortality, and Neonatal Intensive Care Unit length of stay.
Methods
Study design and patients
This double-blind, randomized, placebo-controlled, pilot trial was approved by the University of Oklahoma Health Sciences Center Institutional Review Board. Written informed consent was obtained prior to delivery. The study was registered with NIH Clinical Trials (Clinicaltrials.gov, identifier NCT01220687). New investigational drug approval was obtained from the Food and Drug Administration (IND110317).
The target sample size for this pilot study was 40 (20 newborns in each arm). The arbitrary sample size of 20 per group was chosen as it was deemed large enough to adequately cover the whole spectrum of the studied gestational age. Inclusion criteria were newborn 25 0/7–31 6/7 weeks’ gestational age requiring continuous positive airway pressure or PPV during delivery room (DR) resuscitation/stabilization. Exclusion criteria were known complex congenital anomalies of the heart or lungs and hydrops fetalis.
Randomization and masking
Infants meeting these criteria were randomly assigned to receive either oxygen plus iNO diluted in N2 carrier gas (iNO group) or oxygen in N2 carrier gas alone (placebo group). Subjects were randomized using blocks of size two or four, chosen randomly, to ensure proper balance of patients in each treatment arm throughout the study. To ensure proper blinding, and because of the newborn’s need for resuscitation, and thus study inclusion was unknown a priori, equipment set-up based on the randomization group was performed in advance. This was done so that DR personal would be unaware of the treatment infants received, if resuscitation was administered.
Procedures
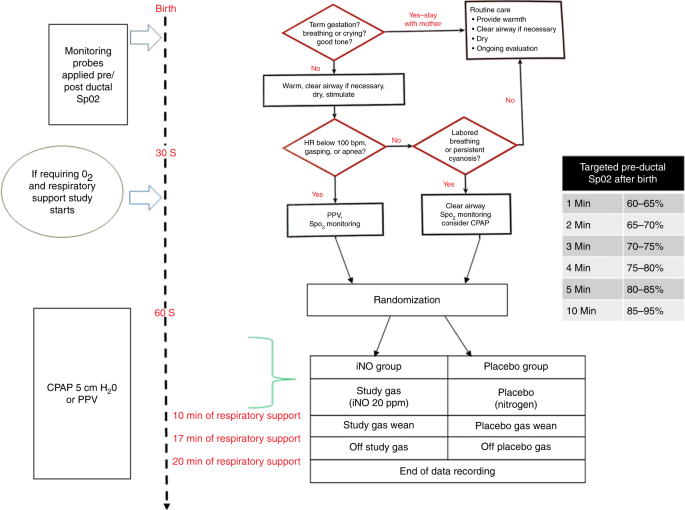
All neonatal resuscitations were done following NRP guidelines (sixth edition).27 Immediately after birth, monitoring sensors were placed for pre- (right arm) and post- (feet) ductal saturations using two pulse oximeters (Masimo SET Radical-7 RDS-3™, Irvine, CA, USA). Between 30 and 90 s, if the infant required PPV, those assigned to the iNO group received 30% oxygen and the study gas. A dose of 20 ppm iNO is the standard approved dose for neonates with persistent pulmonary hypertension of newborn (PPHN) and has been shown to be safe in preterm infants during early postnatal periods.28 Those in the placebo group received 30% oxygen and nitrogen added to the oxygen source via a delivery port built into the circuit. At 10 min of respiratory support, the study gas (iNO or placebo) was down-titrated by 5 ppm per minute until the concentration reached 5 ppm, then reduced every minute by 1 ppm until study gas was terminated (a total of 17 min). Data collection continued for another 3 min and ended at 20 min (Fig. 1).
A T-piece resuscitator (NeoPuff™, Fisher & Paykel Healthcare, Auckland, New Zealand) was used for PPV during initial respiratory support. Oxygen administration was titrated to keep pre-ductal saturations within the target range (1 min 60–65%, 2 min 65–70%, 3 min 70–75%, 4 min 75–80%, 5 min 80–85%, and 10 min 85–95%). Positive-end expiratory pressure was kept constant at 5 cm of water. Peak inspiratory pressure was adjusted to ensure optimal chest rise. No surfactant was administered during the first 20 min after initiation of PPV.
The data capture device for this study was built around the iNO vent, as follows:
The respiratory support section consisted of a blender, T-piece resuscitator, and warmer/humidifier with an injector module to deliver study gas (iNO) or nitrogen (placebo) with positive pressure treatment.
The patient monitoring system consisted of pre- and post-ductal saturations, HR, in-line FiO2, and pressure monitor for the T-piece resuscitator.
The INO delivery/monitor consisted of an INOVENT Delivery System™ (Model number 1605-9000-000, Datex Ohmeda, Mallinckrodt, USA), which includes an in-line oxygen analyzer, NO, NO2, and delivered oxygen analyzer.
The whole set-up occupied the space of a standard transport incubator.
Data capture and collection
Data were continuously collected during the study via an integrated data acquisition system and software (BioPac™ MP 150 Data Acquisition System, BIOPAC Systems, Inc. USA). Real-time display consisted of a study clock, pre-ductal saturation, HR, analyzed and delivered FiO2, and PPV pressure waveform. The resuscitation team was blinded to both iNO delivery and display on the front of the INO vent. Prior to the study, bench testing of this device was performed in a SimnewB® non-breathing model to ensure accurate delivery of oxygen and iNO to the nasal and hypo-pharyngeal area with the T-Piece resuscitator. This test verified that there was no difference between the analyzed and the delivered oxygen.
Statistical analysis
Descriptive statistics were computed for all demographic and clinical variables. For bivariate group comparisons of continuous variables, data were first assessed for normality using Shapiro–Wilk test and then compared using Student’s t test or Wilcoxon–Mann–Whitney test, as appropriate. Similarly, bivariate group comparisons of categorical variables used the chi-square or Fisher’s exact test as appropriate. The biometric data captured were then sampled at one observation every 5 s, for a total of 240 observations per patient, for clarity and analysis. Max FiO2, cumulative FiO2 exposure, FiO2 at study end, HR, and pre- and post-ductal saturation percentages were calculated from these measures for both groups, assessed for normality, and compared using Student’s t test or Wilcoxon–Mann–Whitney test, as appropriate. The rate of hyperoxia (FiO2 > 0.60) over the study period was compared between the two groups using Poisson test. In addition, functional principal component (PC) analysis was used to estimate mean functional curves of the biometrics over the study period and to identify contiguous time points of significant variability between groups for each outcome. PC scores were assigned to each subject within regions of high variation and the scores between groups were compared using Anderson–Darling test.29,30
Results
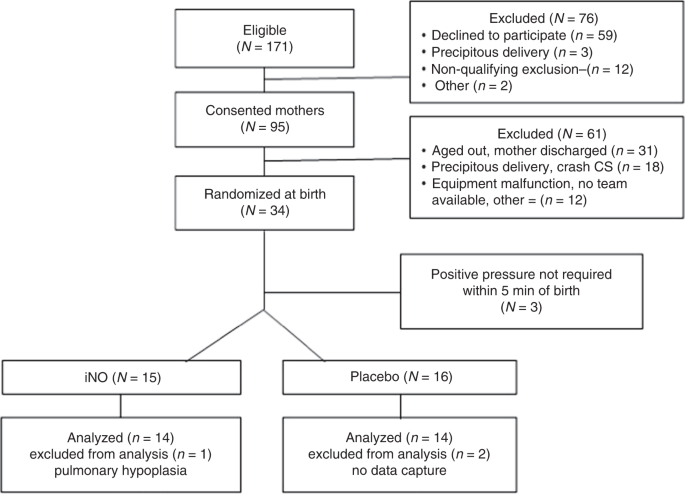
This study was conducted between March, 2012 and February, 2017. Of the 171 mothers eligible for study participation, 95 provided written informed consent and were included. Of these 95 candidates, 61 were excluded. Thirty-four infants were randomized at birth. Enrollment process was discontinued prior to reaching our target (n = 40) due to slow recruitment. In all, 28 infants (14 in each group) were included in final analysis (Fig. 2). No significant inter-group differences were found in patient demographics (Table 1).
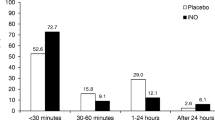
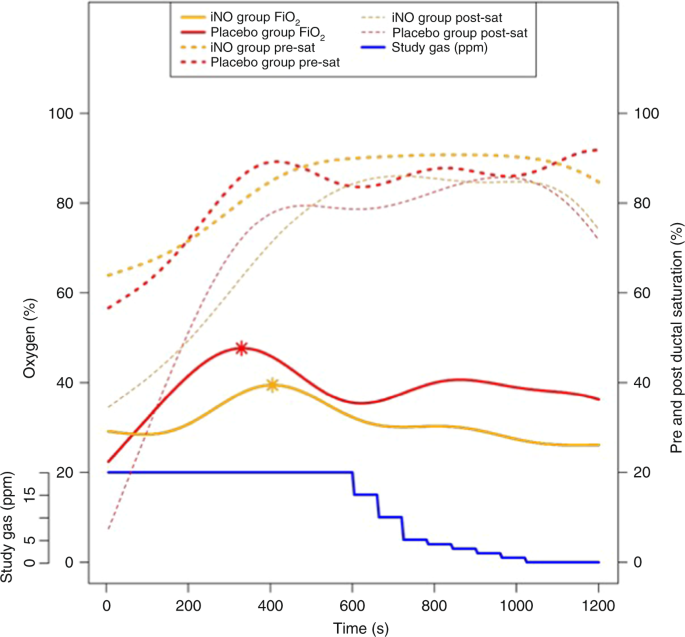
Oxygen during resuscitation
Infants in the placebo group responded to PPV with oxygen (+nitrogen) but required higher oxygen throughout resuscitation compared to the iNO group. Infants randomly assigned to the iNO (+oxygen) group received significantly less cumulative FiO2 when summed across all sample points in the study period (p = 0.0012). In addition, the maximum inspired oxygen required during the study in the iNO group tended to be lower as compared to the placebo group (0.39 vs. 0.48; p = 0.0536). This trend became more pronounced at the end of 20 min between the iNO and the placebo group, the iNO group still receiving lower oxygen concentration compared to the placebo group (26% vs. 36%; p = 0.0326; Fig. 3). The placebo group had 9 hyperoxia (FiO2 > 0.60) subjects combining for 708 FiO2 measures >0.60 over the study period compared to 6 subjects in the iNO group combining for 370 FiO2 measures >0.60 over the study period. The rate ratio of hyperoxia for the placebo group compared to the iNO group was 1.91 (95% confidence interval = 1.68, 2.18; p < 0.0001) indicating that the rate of oxygen exposure >0.60 was significantly higher in the placebo group than in the iNO group (Fig. 3).
Oxygen delivery and pre- and post-ductal oxygen saturations during resuscitation. The solid lines (yellow and red) represent average oxygen administered to each group. The interrupted lines (yellow and red) represent pre-ductal (thick) and post-ductal (thin) oxygen saturations in each group. The asterisks represent the highest average oxygen concentration in each group. The blue line represents study gas (ppm)
HR during resuscitation
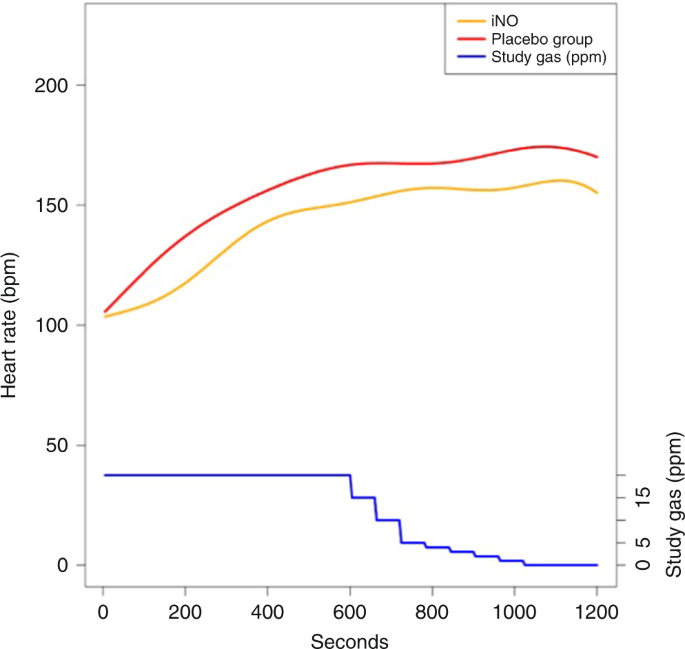
Throughout the resuscitations, the average HR appeared to be lower in the iNO group than in the placebo group (Fig. 4). Mean HR for iNO vs. placebo was 130 ± 46 vs. 139 ± 53 beats per minute (bpm) at 5 min (p = 0.920) and 149 ± 46 vs. 161 ± 53 bpm at 10 min (p = 0.354). At the end of 20 min, mean HR was 153 ± 46 vs. 168 ± 53 bpm. However, these differences were not statistically significant (p = 0.111) (Fig. 4).
Pre- and post-ductal saturation
Mean pre- and post-ductal saturations (%) were not significantly different between the groups at the end of the study (Pre: placebo 90.5 ± 5.7, iNO 82.8 ± 13.8; p = 0.757 and Post: placebo 79.9 ± 25.8, iNO 78.2 ± 20.0; p = 0.849) (Fig. 3).
Need for intubation
Twenty-nine percent of babies in each group were intubated during resuscitation (iNO 4/14, Placebo 4/14; p = 1.0).
Secondary outcomes
There were no significant group differences in any secondary outcomes (Table 2). There were no between-group differences in the need for supplemental oxygen or ventilator support in the 24 h following birth (data not shown).
There were no adverse events noted during resuscitation.
Discussion
This preliminary study demonstrated that administration of iNO as an adjunct during neonatal resuscitation is feasible without side effects. Providing iNO in addition to oxygen during PPV for extremely premature infants at birth is associated with a decreased need for supplemental oxygen treatments. Although the iNO group appeared to have a lower average HR, it was not statistically different.
This study was designed to determine whether the addition of iNO would reduce the oxygen needed when premature neonates require PPV, with or without intubation. Elevated pulmonary artery pressure in the fetus, or “physiologic pulmonary hypertension,” may persist in the immediate postnatal period and may not respond to ventilation alone, as NRP guidelines recommend. In these situations, iNO may augment pulmonary vasodilation, which is essential in the prenatal-to-perinatal pulmonary transition, just as it does in infants with PPHN.31
Studies of iNO in preterm infants with hypoxemia have shown mixed results. In animal studies, iNO showed anti-inflammatory properties, stimulated angiogenesis, increased alveolar growth, improved surfactant function, and inhibited proliferation of smooth muscle cells.32 In large randomized trials in premature infants, none of the benefits seen in animal models were seen when iNO was administered to reduce inflammation and chronic lung disease,33 although a subset of preterm infants appeared to benefit from it.28,34 Nevertheless, these trials have demonstrated that iNO is safe and does not increase oxidative stress or lung inflammation. iNO has never been evaluated in newborn resuscitation for its vasodilator properties, which is essential for extra-uterine adaptation.
In neonatal lambs resuscitated with 21%, 50%, or 100% oxygen ventilation, those with 50% and 100% oxygen experienced a greater initial decrease in pulmonary vascular resistance compared with those resuscitated with 21% with blunted subsequent response to iNO subsequently in the 100% oxygen group. Asphyxiated lambs resuscitated with 100% oxygen showed increased superoxide anions in pulmonary arteries compared to 21% oxygen resuscitation.26,35 These observations suggest that resuscitation with high oxygen concentrations should be avoided in premature infants as it may produce morbidities, such as ROP and BPD.1,2,3 This has been shown in premature infants where resuscitation with 30% compared to 90% oxygen causes less oxidative stress and bronchopulmonary dysplasia.10 Therefore, less oxygen exposure in premature infants during resuscitation is preferable, and iNO during resuscitation may produce these desired benefits. As observed in this study, iNO group required less supplemental oxygen over the entire study period. In addition, there was less exposure to hyperoxia (FiO2 > 0.60). This is probably due to the vasodilator properties of iNO, improving ventilation–perfusion mismatch, and reducing the need for supplemental oxygen to maintain saturation targets. It is interesting to note that the iNO group maintained a lower oxygen requirement starting at 5–6 min of resuscitation, even as the iNO was slowly down-titrated, at 10 min of resuscitation. This finding indirectly indicates that the immediate vasodilator effect of iNO appears to be sustained, despite having a very short half-life (3–5 s). In contrast, the placebo group, after an initial positive response to ventilation, began requiring greater supplemental oxygen after 10 min.
The trend toward a lower HR in the iNO group was an interesting observation. Although not statistically significant, at 5, 10, and 20 min the average HR was 9, 12, and 15 bpm lower respectively in this group. HR is the main determinant of cardiac output in newborns. Cardiac output is dependent on the HR, contractility, preload, and afterload.36 We speculate that the observed differences may be due to improved lung perfusion associated with improved oxygenation and better venous return to the left side of the heart and increased left ventricular output. Therefore, improved pulmonary blood flow (i.e., enhanced preload) may be responsible for maintaining cardiac output and keeping pre-ductal saturation within the targeted range in the iNO group despite a lower HR. In addition, the mean HR in this study was similar to resuscitation studies using 90% and 100% oxygen in premature babies.37
The secondary outcomes were not different between the groups. In particular, the absence of IVH > 2 in either group is consistent with previous observations in large clinical trials in premature infants.28,33
One of the limitations of our study is the small sample size, but this was known prior to study initiation and is consistent with its design as a pilot project. We stopped recruitment before reaching our initial target sample size. The study design required consent prior to delivery, which required screening, and consenting from a large number of parents. In addition, several consented mothers were not enrolled due to precipitous delivery of extremely premature babies, unavailability of the team, or the baby aged out for enrollment. Nevertheless, we believe our final sample size was adequate as a pilot trial.
Conclusions
Administration of iNO as an adjunct gas during neonatal resuscitation is feasible and decreases the amount of exposure to supplemental oxygen in very preterm infants. This was not associated with any adverse events. These findings suggest that iNO facilitates cardiopulmonary transition at birth. This novel approach should be validated by large randomized trials.
References
Stoll, B. J. et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA 314, 1039–1051 (2015).
Horbar, J. D. et al. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics 129, 1019–1026 (2012).
Shah, P. S. et al. Outcomes of preterm infants <29 weeks gestation over 10-year period in Canada: a cause for concern? J. Perinatol. 32, 132–138 (2012).
Jobe, A. H. & Kallapur, S. G. Long term consequences of oxygen therapy in the neonatal period. Semin. Fetal Neonatal Med. 15, 230–235 (2010).
Birenbaum, H. J. et al. Chronic lung disease in very low birth weight infants: persistence and improvement of a quality improvement process in a tertiary level neonatal intensive care unit. J. Neonatal Perinat. Med. 9, 187–194 (2016).
Finer, N. N. et al. Early CPAP versus surfactant in extremely preterm infants. N. Engl. J. Med. 362, 1970–1979 (2010).
Carlo, W. A. et al. Target ranges of oxygen saturation in extremely preterm infants. N. Engl. J. Med. 362, 1959–1969 (2010).
Wyllie, J. et al. Part 7: Neonatal resuscitation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 95, e169–e201 (2015).
Weiner, G. Textbook of Neonatal Resuscitation (American Academy of Pediatrics, 2016).
Vento, M. et al. Preterm resuscitation with low oxygen causes less oxidative stress, inflammation, and chronic lung disease. Pediatrics 124, e439–e449 (2009).
Lakshminrusimha, S. & Steinhorn, R. H. Pulmonary vascular biology during neonatal transition. Clin. Perinatol. 26, 601–619 (1999).
Gao, Y. & Raj, J. U. Regulation of the pulmonary circulation in the fetus and newborn. Physiol. Rev. 90, 1291–1335 (2010).
Hillman, N. H., Kallapur, S. G. & Jobe, A. H. Physiology of transition from intrauterine to extrauterine life. Clin. Perinatol. 39, 769–783 (2012).
Teitel, D. F., Iwamoto, H. S. & Rudolph, A. M. Changes in the pulmonary circulation during birth-related events. Pediatr. Res. 27, 372–378 (1990).
Behrman, R. E. & Lees, M. H. Organ blood flows of the fetal, newborn and adult rhesus monkey: a comparative study. Biol. Neonate 18, 330–340 (1971).
Heymann, M. A., Lewis, A. B. & Rudolph, A. M. Pulmonary vascular responses during advancing gestation in fetal lambs in utero. Chest 71, 270–271 (1977).
Lewis, A. B., Heymann, M. A. & Rudolph, A. M. Gestational changes in pulmonary vascular responses in fetal lambs in utero. Circ. Res. 39, 536–541 (1976).
Lakshminrusimha, S. et al. Pulmonary hemodynamics and vascular reactivity in asphyxiated term lambs resuscitated with 21 and 100% oxygen. J. Appl. Physiol. (1985) 111, 1441–1447 (2011).
Lakshminrusimha, S. The pulmonary circulation in neonatal respiratory failure. Clin. Perinatol. 39, 655–683 (2012).
Abman, S. H., Chatfield, B. A., Hall, S. L. & McMurtry, I. F. Role of endothelium-derived relaxing factor during transition of pulmonary circulation at birth. Am. J. Physiol. 259, H1921–H1927 (1990).
Fineman, J. R., Wong, J., Morin, F. C. 3rd, Wild, L. M. & Soifer, S. J. Chronic nitric oxide inhibition in utero produces persistent pulmonary hypertension in newborn lambs. J. Clin. Invest. 93, 2675–2683 (1994).
Roberts, J. D. Jr. et al. Inhaled nitric oxide reverses pulmonary vasoconstriction in the hypoxic and acidotic newborn lamb. Circ. Res. 72, 246–254 (1993).
Cassin, S. The role of eicosanoids and endothelium-dependent factors in regulation of the fetal pulmonary circulation. J. Lipid Mediat 6, 477–485 (1993).
Lakshminrusimha, S. & Saugstad, O. D. The fetal circulation, pathophysiology of hypoxemic respiratory failure and pulmonary hypertension in neonates, and the role of oxygen therapy. J. Perinatol. 36(Suppl 2), S3–S11 (2016).
Kinsella, J. P. & Abman, S. H. Clinical approach to inhaled nitric oxide therapy in the newborn with hypoxemia. J. Pediatr. 136, 717–726 (2000).
Lakshminrusimha, S. et al. Oxygen concentration and pulmonary hemodynamics in newborn lambs with pulmonary hypertension. Pediatr. Res. 66, 539–544 (2009).
Kattwinkel, J. Textbook of Neonatal Resuscitation (American Academy of Peditarics/American Heart Association, Chicago, 2011).
Schreiber, M. D. et al. Inhaled nitric oxide in premature infants with the respiratory distress syndrome. N. Engl. J. Med. 349, 2099–2107 (2003).
Lin, N., Jiang, J., Guo, S. & Xiong, M. Functional principal component analysis and randomized sparse clustering algorithm for medical image analysis. PLoS ONE 10, e0132945 (2015).
Greven, S., Crainiceanu, C., Caffo, B. & Reich, D. Longitudinal functional principal component analysis. Electron. J. Stat. 4, 1022–1054 (2010).
Lakshminrusimha, S., Konduri, G. G. & Steinhorn, R. H. Considerations in the management of hypoxemic respiratory failure and persistent pulmonary hypertension in term and late preterm neonates. J. Perinatol. 36, S12–S19 (2016).
McCurnin, D. C. et al. Inhaled NO improves early pulmonary function and modifies lung growth and elastin deposition in a baboon model of neonatal chronic lung disease. Am. J. Physiol. Lung Cell. Mol. Physiol. 288, L450–L459 (2005).
Barrington, K. J., Finer, N., Pennaforte, T. & Altit, G. Nitric oxide for respiratory failure in infants born at or near term. Cochrane Database Syst. Rev. CD000399 (2017).
Ballard, R. A. et al. Inhaled nitric oxide in preterm infants undergoing mechanical ventilation. N. Engl. J. Med. 355, 343–353 (2006).
Lakshminrusimha, S. et al. Pulmonary hemodynamics in neonatal lambs resuscitated with 21%, 50%, and 100% oxygen. Pediatr. Res. 62, 313–318 (2007).
Vincent, J. L. Understanding cardiac output. Crit. Care 12, 174 (2008).
Oei, J. L. et al. Targeted oxygen in the resuscitation of preterm infants, a randomized clinical trial. Pediatrics 139, e20161452 (2017).
Acknowledgements
We thank Karen Corff, Clara Song, and Ted Jeffers for obtaining consent from the parents; Susan James, Stephanie Montgomery, and Gary Revas for randomization and equipment set-up in the delivery room; Richard Wade, UCSD, USA for providing technical support for the study; Doug Swanton, Mallinckrodt Pharmaceuticals, USA for support during bench testing; and Gene Halford for editing and reviewing the manuscript. We also thank the members of the Data Safety Monitoring Board: R. Ramanathan, MD, and P. Friedlich, MD, MS Epi, MBA, University of Southern California, USA. This study was funded by an unrestricted grant from Mallinckrodt Pharmaceuticals, USA.
Author information
Authors and Affiliations
Contributions
K.S. and S.N. conceptualized and designed the study. K.S. wrote the first draft of the manuscript. E.S., S.N., and S.L. reviewed and revised the manuscript. M.A. analyzed the data and provided the statistical support. M.M. built the iNO delivery and monitoring system and collected the data. M.M., A.W., D.D., A.H., J.R., and A.M. obtained informed consent and conducted the study in the DR. All the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sekar, K., Szyld, E., McCoy, M. et al. Inhaled nitric oxide as an adjunct to neonatal resuscitation in premature infants: a pilot, double blind, randomized controlled trial. Pediatr Res 87, 523–528 (2020). https://doi.org/10.1038/s41390-019-0643-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-019-0643-x
- Springer Nature America, Inc.
This article is cited by
-
Nitric oxide and preterm resuscitation: some words of caution
Pediatric Research (2020)