Abstract
Substance use disorders represent a significant public health concern with considerable socioeconomic implications worldwide. Twin and family-based studies have long established a heritable component underlying these disorders. In recent years, genome-wide association studies of large, broadly phenotyped samples have identified regions of the genome that harbour genetic risk variants associated with substance use disorders. These regions have enabled the discovery of putative causal genes and improved our understanding of genetic relationships among substance use disorders and other traits. Furthermore, the integration of these data with clinical information has yielded promising insights into how individuals respond to medications, allowing for the development of personalized treatment approaches based on an individual’s genetic profile. This review article provides an overview of recent advances in the genetics of substance use disorders and demonstrates how genetic data may be used to reduce the burden of disease and improve public health outcomes.
Similar content being viewed by others
Introduction
Substance use disorders (SUDs) encompass a range of common and heritable psychiatric disorders that result from a complex interplay of genetic and environmental factors. Together, SUDs affect millions of people and account for a significant proportion of the global burden of disease. For example, alcohol use disorder (AUD) affected over 100 million people in 2019 and was responsible for around 160,000 deaths, while opioid use disorder (OUD) affected around 21 million people and contributed to more than 88,000 deaths [1]. Substance use disorders also increase the risk of other leading contributors of morbidity and mortality, such as poisoning, suicide and self-inflicted injuries related to alcohol and opioid use, as well as chronic diseases like chronic obstructive pulmonary disease related to tobacco use [2]. Understanding the genetic causes of SUDs will facilitate the development of more effective treatments and prevention strategies, helping to alleviate the global burden of SUDs.
Genome-wide association studies (GWAS) have emerged as a powerful tool to identify genetic variants associated with SUDs. This approach has provided valuable insights into the genetic architecture of SUDs, revealing genomic regions and candidate causal genes that contribute to susceptibility. This review will discuss recent advancements in the genetics of SUDs, including (i) the identification of robust (replicable) risk variants; (ii) how these risk variants have been used to identify novel genes and disease mechanisms; (iii) the use of GWAS for polygenic scores (PGS); (iv) how risk variants have been used to establish causal associations both within SUDs and between SUDs and other disorders; and (v) and how these genetic factors influence an individual’s response to drugs. We will conclude the review with discussion on clinical and therapeutic implications of genetic findings for SUDs.
Genetic variation underlying major substance use disorders
Genome-wide association studies have been central to the identification of common (minor allele frequency [MAF] > 0.01) SNPs associated with SUDs. In addition, it is recognized that rare genetic variants, including rare SNPs (MAF < 0.01), copy number variants (CNVs), and structural variants (SVs), may also play a significant role in the susceptibility to SUDs. Because statistical power increases with higher MAF, common SNPs underlying SUDs are routinely identified through GWAS meta-analyses of increasingly large, broadly phenotyped biobanks, such as the Million Veteran Program (MVP) [3] and the UK Biobank (UKB) [4]. Rare variants, defined by their low frequency in the population, are more challenging to detect and analyze. However, they are known to exert a larger effect compared to common variants and have the potential to advance our understanding of risk genes and biological pathways underlying SUDs [5]. This section summarizes known genetic risk factors underlying SUDs, with particular emphasis on recently published results. We provide a summary of recent genetic findings for SUDs in Fig. 1, including the number of identified loci (1a) and the amount of variation explained by common variants (SNP-based heritability, or h2snp) and polygenic scores (1b).
a Number of genomic loci associated with substance use disorders verse GWAS sample size (see Supplementary Table 1). b SNP-based heritability (h2snp) and variance explained by polygenic scores (R2 PGS) for substance use disorders (extracted from refs. [9, 18, 26, 42, 43]). Notes: AUD alcohol use disorder, CUD cannabis use disorder, OUD opioid use disorder, TUD tobacco use disorder, Effective N effective sample size.
Alcohol use disorder
The heritability of AUD from twin and family-based studies is around 50% [6], and the estimated h2snp is between 5.6% to 10.0% [7]. Early GWAS of Alcohol Dependence and measures of problematic drinking collectively identified more than 10 risk variants that mapped to several risk genes, most notably the alcohol dehydrogenase genes ADH1B (Alcohol Dehydrogenase 1B [class I], Beta Polypeptide) and ADH1C (Alcohol Dehydrogenase 1 C [class I], Gamma Polypeptide) [8]. The largest available meta-analysis of problematic alcohol use (PAU), which combined both AUD and problematic drinking data from the Million Veteran Program (MVP), the UK Biobank, and the Psychiatric Genomics Consortium (PGC), identified 29 independent risk variants, 19 of which were novel [9]. These risk variants mapped to 66 genes, including previously implicated DRD2 (Dopamine Receptor D2), along with additional genes encoding alcohol dehydrogenase enzymes ADH4, ADH5, and ADH7. Functional analyses of these genes found significant enrichment of genetic signal for problematic alcohol use in several brain tissues and neural cell types. A recent multivariate GWAS jointly modelled the genetic effects of four SUDs (AUD, CUD, OUD, and TUD) to identify both shared and unique (i.e., substance-specific) genetic effects underlying each disorder [10]. The study identified 9 independent SNPs specifically associated with problematic drinking; as expected, the most significant SNP effect mapped to the gene ADH1B, and biological pathway enrichment analysis implicated alcohol metabolism pathways.
There have been recent efforts to identify sources of structural variants underlying alcohol use disorder, however statistical power is limited with current sample sizes. A meta-analysis of five cohorts investigating AUD identified nine regions of CNVs, including a suggestive association on chromosome 5q21.3 [11]. Further replication studies confirmed the presence of these CNV regions, and additional analyses focusing on pathways and gene-drug interactions revealed the involvement of the mitogen-activated protein kinase signalling pathway and specific drugs related to AD biology or treatment. In a separate study conducted on Mission Indian families, a whole genome scan also uncovered genetic linkage between chromosome 5q21.3 and “craving for alcohol.” [12] These findings suggest genomic structural variation may play a role in the risk for alcohol dependence, although larger studies will be required to characterise the global CNV burden between cases and controls.
Cannabis use disorder
Although cannabis use is prevalent, most users do not progress to cannabis use disorders. Cannabis use disorder (CUD) has a moderate heritability of ~0.5–0.6, which slightly exceeds the estimates for cannabis use and initiation phenotypes (h2 = ~0.4–0.5) [13]. Early GWASs of cannabis use disorders identified genome-wide significant variants, however there was poor replication between studies due in part to small sample sizes (the largest study included 51,372 individuals with 2387 cases) and heterogeneity among samples [14,15,16,17]. Only one locus, associated with a cis-eQTL for CHRNA2 (Cholinergic Receptor Nicotinic Alpha 2 Subunit), was consistently identified as robustly associated with CUD.
A GWAS meta-analysis of 20,916 CUD cases and 363,116 controls replicated the CHRNA2 locus and identified a novel association in FOXP2 (Forkhead box protein P2) [18]. A cross-ancestry multivariate GWAS of substance use disorders suggested the signal for theCHRNA2 is CUD-specific (i.e., the locus is not shared with other SUDs) [10]. On the other hand, the same multivariate analysis found the FOXP2 locus was associated with both CUD and problematic tobacco use (PTU) in Europeans and CUD and OUD in African Americans, suggesting pleiotropic (i.e., not CUD-specific) SNP effects drive this association.
A recent study used whole genome sequencing (WGS) to investigate the relationship between low-frequency (MAF < 0.02) variants and DSM-IV defined CUD in a community-based sample of Native Americans and a European ancestry family-based sample [19]. The analysis used a set-based approach, where separate analyses were performed for low-frequency variants in coding regions followed by regulatory elements. A single genome-wide significant association was found in the coding region of C1orf110 and the regulatory region in the MEF2B gene in a meta-analysis of both samples. While these data point to the contribution of rare variants to the heritability of CUD, further studies in large, population-based cohorts with replication in independent samples is required.
Tobacco use disorder
Genetic factors play a significant role throughout the stages of cigarette smoking and tobacco (nicotine) use disorder (TUD). Studies suggest that there is a considerable range of heritability estimates for nicotine dependence, typically falling between approximately 0.30 and 0.70 [20, 21]. The wide range of heritability estimates may be influenced by the choice of TUD assessment, where the Fagerström Tolerance Questionnaire (FTQ) and the Fagerström Test for Nicotine Dependence (FTND) may produce different results to the gold standard DSM-IV and DSM-5 (Diagnostic and Statistical Manual of Mental Disorders) [22, 23].
A GWAS meta-analysis involving 38,602 smokers across 15 studies using the FTND and information on cigarettes per day, identified 6 replicable associations, including previously known associations with the CHRNA5-CHRNA3-CHRNB4 genes. A novel intronic variant in DNMT3B (rs910083) was linked to an increased risk of nicotine dependence, particularly severe dependence, and was replicated in the UK Biobank using a severe dependence phenotype. The integration of tissue-specific methylation and expression data found rs910083/DNMT3B was also a cis-methylation quantitative trait locus (QTL) and a cis-expression QTL, suggesting its role in influencing DNMT3B methylation levels in foetal brain and gene expression in adult cerebellum [24].
A follow-up study in 58,000 smokers of European and African ancestry using the FTND questionnaire identified five genome-wide significant loci, including previously undiscovered variants near MAGI2/GNAI1 and TENM2 [25]. Both variants influence the expression of nearby genes. The integration of tissue-specific gene expression data found rs2714700/MAGI2-AS3 affects gene expression in the hippocampus, while rs1862416/TENM2 affects expression in the lung. Interestingly, the variant rs2714700 consistently showed association with the heaviness of smoking index from the UK Biobank, while rs1862416 did not. This suggests secondary analyses based on the quantity of tobacco consumed may provide additional insight into the genetic effects on tobacco use dependence.
The availability of electronic health record (EHR) data with linked SNP genotype data has the potential to greatly increase samples sizes without the need to prospectively recruit individuals with clinical diagnoses. A recent multi-ancestry GWAS meta-analysis of TUD combined data from 898,680 individuals of European, African American, and Latin American ancestry from 5 biobanks under the PsycheMerge partnership with a further 244,890 individuals from the UK Biobank [26]. The study identified 97 genome-wide significant lead SNPs located in 72 independent loci, all of which were previously reported in much larger GWAS of smoking-related phenotypes (e.g., GWAS and Sequencing Consortium of Alcohol and Nicotine use [GSCAN] smoking initiation and cessation) [27]. This supports the use of EHRs in identifying replicable associations with smaller sample sizes. The analysis also provided support for nicotinic acetylcholine receptor genes as risk genes for smoking-related traits as well as being involved in dopaminergic transmission, including DRD2, DBH, KDM4A, PDE4B, and NCAM1.
Several studies have investigated low frequency and rare exonic variants in tobacco use, but have largely failed to identify replicable, exome-wide significant results outside of nicotinic cholinergic receptor genes [28,29,30,31]. A recent exome-wide association study of rare (MAF < 0.01) variants found a protective association with CHRNB2 (Neuronal acetylcholine receptor subunit beta-2), where carriers of rare predicted loss of function or deleterious missense variants have a 35% lower odds of heavy smoking [32] (defined as at least 10 cigarettes per day either currently or formerly) and 18% lower odds of ever smoking. A leave-one-variant-out analysis identified a deleterious missense variant in CHRNB2, which was later validated in an independent cohort. Importantly, the authors found nominally significant enrichment of protective associations of the variant with other phenotypes, including substance use disorders (excluding alcohol), suggesting a genetic effect on both tobacco consumption and dependency phenotypes.
Opioid use disorder
Approximately 50% of the variability in opioid dependence is due to additive genetic effects [33], with around 38% of the variability accounted for by genetic risk factors unique to opioid use [34]. Several GWAS with modest sample sizes (the largest comprising 10,544 cases) have reported genome-wide significant loci [35,36,37,38,39], however none were replicated using an independent sample. A GWAS of 82,707 European American individuals identified a coding variant in the OPRM1 (opioid receptor mu 1) gene, which was later replicated in 2 independent cohorts [40] and further strengthened in a larger multi-trait GWAS of opioid addiction [41]. A subsequent meta-analysis of seven cohorts identified three genome-wide significant lead SNPs in a European ancestry meta-analysis, including variants in the FURIN and OPRM1 genes [42]. Furthermore, a multi-trait analysis of GWAS (MTAG) combining OUD with AUD and CUD revealed 18 independent genome-wide significant loci, suggesting common (i.e., shared) genetic factors contribute to the development of multiple substance use disorders [42].
A recent cross-ancestry meta-analysis of 425,944 individuals in the MVP cohort used both stringent definitions of OUD (described by Zhou et al. [40]) and less stringent definitions which only required a single diagnostic code from the International Classification of Diseases (ICD-9 or ICD-10) for opioid abuse or dependence and identified 14 genome-wide significant loci [43]. In this study, a cross-ancestry meta-analysis of the less stringent OUD diagnosis in the MVP sample revealed 12 genome-wide significant variants, 3 of which replicated in a cross-ancestry GWAS meta-analysis of strictly defined OUD. These included variants in OPRM1, replicating the original MVP GWAS [40], in addition to variants in FURIN and near the gene TSNARE1. The authors found significant heritability enrichment of gene expression for OUD in multiple brain tissues previously associated with addiction. In addition, a transcriptome-wide association study found genes with differential gene expression underlying OUD in both brain and multiple peripheral tissues, such as adipose, gastrointestinal, and liver. This suggests OUD-related genetic variation may affect biological processes in both the brain and periphery.
The definition of cases (e.g., the number and type of diagnostic codes) and controls (e.g., the use of opioid-exposed, unexposed, and/or population-based controls), varies across OUD GWAS, which may decrease the generalizability of results. However, there are high genetic correlations across cohorts with different definitions of OUD cases and controls (rg > 0.9) [41], suggesting shared genetic effects contribute to OUD across a range of case/control definitions.
Little progress has been made on studies of rare variation underlying OUD, primarily due to the large sample sizes typically required to identify rare variants. The largest study to date used genotyping and copy number variation (CNV) calling methods in a sample of European–American and African American OUD cases and controls. Genome-wide association analysis of CNVs with OUD identified two deletions and one duplication that were significantly associated with OUD, including a chromosome 18q12.3 deletion with a protective effect [44].
Genetic overlap between SUDs and with other complex traits
Consistent with high rates of comorbidity, there is substantial overlap in genetic risk factors between different substance use disorders. Recent studies have observed substantial pleiotropy at genome-wide [45], regional [46], and transcriptomic [47] levels. Genetic correlations range from ~0.45 (TUD and OUD) to ~0.70 (AUD and OUD) (see Fig. 2a) suggesting that while there is extensive overlap, there are also substance-specific genetic effects.
a Genetic correlations between substance use disorders (extracted from refs. [25, 26, 138], which estimated correlations using linkage disequilibrium score regression). b Substance use disorders cluster to form a general addiction factor (path coefficients extracted from model reported in Hatoum et al. [10]., estimated using genomic structural equation modelling).
A recent study leveraged these correlations in a multivariate GWAS of four SUDs (AUD, TUD, CUD, and OUD), comprising over 1 million individuals. Using genomic structural equation modelling, the authors identified a general addiction risk factor (see Fig. 2b). A GWAS of the addiction factor identified 19 significant SNPs, the most significant of which was near DRD2, and functional enrichment analyses implicated pathways related to neural cells and immune cell processes. A separate study attempted to disentangle genetic effects underlying SUDs using exome-focussed genotyping of four SUDs (AUD, n = 4487; TUD, n = 4394; CUD, n = 954 and nonmedical prescription OUD, n = 346) in a large population-based sample (n = 36,309) [48]. An exome-wide association of common (MAF > 0.01) SNPs identified 53 experiment-wide significant SNPs associated with at least one SUD or a combined analysis of all four SUDs. A gene-based analysis of rare variants (MAF < 0.05) implicated 24 genes (using a nominal threshold of P < 10-4), all of which were previously implicated in large SUD GWAS with at least nominal (P < 0.05) significance. Finally, a “shared inheritance” (i.e., pleiotropic) analysis of all SUDs by gene-based association of rare alleles identified 9 genes associated with at least 2 SUDs. Collectively, these data suggest presence of widespread pleiotropy across SUDs.
There is also substantial pleiotropy between substance use disorders and psychiatric disorders (see Fig. 2), with the strongest overlap observed with ADHD, MDD, Anxiety, and schizophrenia. AUD has the most overlap with psychiatric disorders (mean |rg| = 0.32) while OUD has the least (mean |rg| = 0.18). While psychiatric disorders are generally positively genetically correlated with SUDs, OCD is noteworthy given its significant negative correlation with AUD (rg = −0.35, se = 0.13) and TUD (rg = −0.24, se = 0.05).
Substance use phenotypes
As ascertaining large numbers of individuals with a diagnosed SUD is challenging, many studies have focused on broader, use-based phenotypes such as initiation, frequency, or quantity of use, which are easily assessed in large-scale cohorts and biobanks. These efforts are largely driven by consortia such as GSCAN [27, 49] and the International Cannabis Consortium (ICC) [50,51,52].
A recent large-scale, multi-ancestry GWAS (up to ~3.3 million individuals) by GSCAN included four tobacco use traits (smoking initiation, age of smoking regularly, smoking cessation, and cigarettes per day) and the alcohol use trait ‘drinks per week’ [27]. This study identified a remarkably large number of associated risk loci, including 1346 loci for smoking initiation and 496 for drinks per week. The largest cannabis-related genetic study to date by the ICC is a GWAS of lifetime cannabis use [52]. This identified 8 genome-wide significant SNPs and 35 genes, the strongest association with CADM2. A GWAS of ‘age at first cannabis use’ identified a single locus (ATP2C2) [50].
These substance use phenotypes overlap moderately with dependence / disorder phenotypes (tobacco use and TUD rg = ~ 0.4 − 0.8; alcohol quantity and AUD rg = ~ 0.75; cannabis use and CUD rg = ~ 0.50; see Fig. 3). This suggests there is considerable shared genetic etiology between use and dependence, and GWAS of use phenotypes can provide important biological insights into substance use disorders. But importantly, the imperfect overlap reinforces that substance use and dependence are different and GWAS of strictly defined SUDs are needed to dissect the distinct aspects that leads to substance dependence.
Genetic correlations between alcohol use disorder (AUD), cannabis use disorder (CUD), opioid use disorder (OUD), tobacco use disorder (TUD) and a range of complex traits. Genetic correlations extracted from recent studies that applied linkage disequilibrium score regression (refs. [9, 18, 25, 26, 43, 138]). Error bars represent 95% confidence intervals.
Overall, substance use phenotypes (such as initiation, frequency, and quantity) tend to have less genetic overlap with psychiatric disorders and related traits than dependence phenotypes. For example, analysis of different dimensions of alcohol use (alcohol consumption versus problematic consequences of drinking) in the Alcohol Use Disorders Identification Test (AUDIT) revealed a divergent pattern of genetic correlations with other psychiatric traits: problematic drinking was positively correlated with ADHD and MDD, while alcohol consumption was negatively correlated with these same disorders [53]. A similar pattern is also observed with tobacco, where use-based phenotypes [49] have significantly lower genetic correlations with psychiatric disorders than TUD [26].
Interesting, divergent patterns of association are also observed within different aspects of consumption (e.g., quantity vs. frequency). The genetic correlation between alcohol quantity and frequency in the UK Biobank was just 0.52 [54], and these measures display opposite patterns of association with indices of socioeconomic status, other substance use phenotypes, and psychiatric disorders. For example, alcohol frequency is negatively correlated with MDD, ADHD, and smoking initiation, while quantity is positively correlated with these same disorders. Taken together, these results suggest the presence of unique genetic factors underlying different types of consumption within the same disorder.
Polygenic prediction of substance use disorders
Genetic effect estimates from genome-wide association studies can be used to calculate PGS that provide an indication of an individual’s genetic liability to a certain trait or disease. PGS can be calculated by multiplying the number of risk alleles a person carries with the SNP effect sizes from a GWAS of that phenotype and aggregating across all SNPs (taking LD into account). In research, these scores can then be used to validate the predictive power of the GWAS results, estimate associations with other traits, or test gene-environment interplay. Moreover, PGSs also hold potential for future clinical use.
In general, PGS only explain a small proportion of a trait’s variance, but they are valuable as they provide a measure of individual level genetic risk that can be used in analytical models. The validity to predict complex behavioural and psychiatric phenotypes has been well demonstrated for many traits [55]. For substance use disorders, current PGS explain approximately 2.1% for AUD [9], 3.8% for OUD [42], and 6.3% for TUD [26] (Fig. 1B). These estimates are lower than for some other psychiatric disorders, mostly due to the larger GWAS sample sizes for these other disorders. The predictive value of polygenic scores will grow when genome-wide effect estimates become more accurate once larger, more powerful GWASs become available. An important note is that PGS are most predictive in samples of similar ancestry as the source GWAS effect estimates are based on, due to differences in allele frequencies and LD between populations. The large-scale GWASs of SUDs are predominantly based on European ancestry participants, so PGS will be most powerful in European ancestry target samples.
Since the publications of the large-scale GWASs on AUD, CUD, and other substance use disorders, their summary statistics have been used to create PGS in independent samples to predict substance use, mental health, or other phenotypes. PGS for AUD were most often utilized in PGS analyses, while only very few studies included CUD or other substance use disorder PGS.
For AUD, most studies have found that AUD PGS (or PGS based on problematic alcohol use) significantly predict AUD and related alcohol use phenotypes [56,57,58,59,60,61,62], while a few other PGS analyses have not yielded significant results (e.g [63]. and [64] [in females only]). AUD PGS predicts an earlier age of onset for first substance use, regular use, the initiation of alcohol related problems, and alcohol dependence diagnosis [65]. AUD PGS have also been found to be positively associated with use of other substances [9, 60], mental health problems, including depression, anxiety disorder, bipolar disorder, ADHD, pathological gambling [9, 66, 67], myocardial infarction type 2 [68], nutrition intake [62], and neural connectivity in males [69] and negatively associated with cognition [60, 69]. Other studies showed no significant associations of AUD PGS with for instance epigenetic aging [70], timing of first marriage or likelihood to divorce [71], impulsivity [72], resilience [73] or AUD treatment outcome [74]. Some studies also investigated PGS associations in non-European ancestry, associations separately by sex, or tested for gene-environment interaction effects. For example, an AUD PGS from African ancestry individuals predicts age of regular use, alcohol dependence, and progression from regular use to alcohol dependence diagnosis [65]. However, most of these analyses yielded non-significant associations (e.g. [63, 64, 67, 75, 76]), likely due to the lack of statistical power.
With respect to CUD, there have only been a few PGS studies. Segura et al. [77] found that CUD PGS were significantly associated with cannabis use and monthly cannabis use at baseline, but not with age at initiation of cannabis use or with various measures related to the clinical course after a first-episode psychosis. In contrast, Cheng et al. [78] showed that PGS for CUD predicted bipolar disorder with psychotic experience but not bipolar disorder without psychotic experience.
Paul et al. [79] investigated the association between polygenic risk for substance use and cognition, and found no significant association between a CUD PGS with any of the measured cognition variables, whereas the PGS for lifetime cannabis use was positively associated with general ability, executive function, and learning/memory.
PGS for other substance use disorders showed mixed results. Two studies found that OUD PGS significantly predicted opioid use phenotypes ([60, 67] [only in the European, not the African ancestry, subsample]). Significant positive associations were also found for OUD PGS with other substance use related traits, negative associations with educational attainment and SES-related traits, as well as positive associations with several mental health traits (e.g. phenotypes related to conduct disorder and depression [60]), whereas in another study no significant associations were found between OUD PGS and a range of health-related phenotypes [67].
Vilar-Ribó, et al. [66]. tested whether the genetic liability to five SUD-related phenotypes was associated with ADHD and found that PGS for cocaine dependence and ever addicted to illicit drug did not yield significant associations with ADHD, while PGS for lifetime cannabis use, alcohol dependence and smoking initiation were significantly associated. Moreover, Hatoum et al. [10]. created a latent general addiction risk factor and found that the PGS based on this factor were associated with substance use disorders, psychopathologies, somatic conditions, and environments associated with the onset of addictions. In another study, a PGS based on substance misuse was significantly predictive of COVID-19 [80].
Causes and consequences of substance use disorders
Identifying modifiable risk factors for disease is of particular interest in medicine and epidemiology, as it can inform preventive efforts and improve treatment. For many important health questions, it is not feasible to conduct a randomized controlled trial (RCT), due to practical and/or ethical reasons, making causal inference challenging. Rapid developments in the field of (substance use) genetics have led to the emergence of a powerful causal method that may solve these problems. Genetic variants robustly associated with a potential risk factor of interest, identified through GWAS, can be used as instrumental variables in an approach called ‘Mendelian randomization’ (MR) [81]. Substance use is an obvious modifiable risk factor that may be impacted by policy and preventive efforts, making MR for substance use disorders a particularly fruitful avenue to pursue [82].
MR relies on three core assumptions; the included genetic variants, the ‘genetic instrument’, should (1) be robustly associated with the exposure variable, (2) not be associated with confounders of the relationship between exposure and outcome, and (3) not be associated with the outcome through any other path than the exposure [83]. Depending on the relation of interest, there are additional assumptions [84]. To estimate the causal effect, Inverse-variance weighted (IVW) regression is conducted, which assumes no violation of the core assumptions. An important part of an MR study is to conduct sensitivity approaches to assess the robustness of a potential causal finding. For an extensive discussion about the theory and practical application of MR, we refer to two excellent reviews by Richmond and Davey Smith [84] and Davies et al. [83]. Examples of commonly applied sensitivity methods are: weighted median regression [85], weighted mode regression [86], MR-Egger [87], MR-PRESSO [88], and GSMR [89]. Apart from this selection of methods a wide range of other approaches exists (such as Bayesian MR [90] and an integration of MR and the direction of causation twin model [91]). Finally, a particularly useful addition to the MR ‘toolbox’ worth noting here is multivariable MR, where (an) additional exposure variable(s) can be added [92]. An important weakness of MR as it is often applied, is that it can be biased by assortative mating, dynastic effects, and population structure [93]. These biases can be overcome by using family-based GWAS estimates and conducting standard MR methods [93, 94] or by specific within-family MR methods [95].
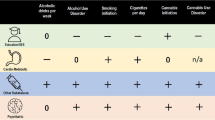
Mendelian randomization has been used to assess causal effects between SUDs and mental health, behavioural, and physical traits (Fig. 4). The most well-studied traits include cognitive functioning and educational attainment, structural brain measures, and psychiatric disorders (predominantly MDD, PTSD, ADHD). For alcohol use disorder, there is consistent evidence that higher intelligence and educational attainment causally decrease the risk of developing AUD [9, 96, 97]. One study indicated that PAU liability, which combined AUD and problematic drinking, may also causally decrease educational attainment [9], however other studies have failed to replicate this finding [97]. There is no evidence for causal effects in either direction between AUD and executive functioning [98], nor is there evidence for causal effects of alcohol dependence on late-onset Alzheimer’s disease risk [99]. While there was some evidence that AUD liability causes a later age of onset of Alzheimer’s, this is likely due to survival bias [99]. When focusing on more proximal measures, brain structure and other imaging phenotypes, there is evidence that a larger right pallidum volume increases AUD risk and in the other direction, that AUD liability decreases right putamen volume [100], amygdala volume, and hippocampal volume [101]. There is also some evidence that AUD increases markers of iron in the putamen [102] and basal ganglia [103], but this evidence is weak. Finally, with regards to psychiatric traits, there is no clear evidence of causal effects between AUD and loneliness [104], self-harm [105], or suicide [106]. While there is weak evidence of a causal effect of ADHD on AUD, but not the reverse, from one study [82] this was not replicated in another [66]. There is evidence for a causal effect of PTSD [107], insomnia [108], and of MDD [109] on AUD, but not the reverse.
This figure displays traits that have been found to causally influence the risk of major substance use disorders (“Causes”) and traits that are influenced by these disorders (“Consequences”). Negative directions of effect are displayed in green (−) while positive directions of effects are influenced in red (+). Note that this figure includes traits with a reported causal association with substance use disorders but does not consider the strength of evidence of causation or effect size of the association.
For CUD there is evidence for bidirectional causal effects with educational attainment [110] but no evidence for causal effects with suicide [106]. In addition, a causal effect of CUD on schizophrenia has been identified [111], although we cannot rule out the presence of bidirectional effects [52, 112]. Finally, there is evidence that smoking initiation causally increases the risk of CUD, acting as a gateway [113].
Higher intelligence may decrease the odds of nicotine dependence [96] and nicotine dependence increases the risk of schizophrenia (even when corrected for CUD) [111]. There is no clear evidence for causal effects between nicotine dependence and ADHD [114], nor from nicotine dependence to suicide [106].
Finally, for opioid dependence there is no clear evidence for causality with suicide [106], weak evidence of an effect of opioid dependence on increased alcohol drinking [113], and evidence that smoking initiation, MDD, and neuroticism increase and higher educational attainment decrease opioid dependence risk [40]. For cocaine dependence there is no clear evidence for causal effects with other substance use behaviours [113] or ADHD [66].
Overall, MR studies have led to the identification of important, putative causal relations between substance use disorders and (poor) mental health outcomes. This knowledge should be considered in the development of preventive efforts and health messages and followed up on with more extensive analyses to pinpoint the exact causal pathways and mechanisms. An important approach to further improve the reliability of causal findings is ‘triangulation’ [115], that is, explicitly combining MR with other types of research method in a single study [116]. If the findings of different research methods, with different biases, all point to a causal effect, it is much less likely to be spurious. For instance, MR can be combined with observational (cohort) analyses, other genetically informative designs such as discordant twin or sibling analyses, or even natural experiments such as policy changes. Given its convenience and the ongoing expansion of even more sophisticated sensitivity methods, it is expected that MR will remain an important method in the field of causal inference.
Pharmacogenomics of substance use disorders
There are several approved and effective pharmacological treatments of substance use disorders [117]. Incorporating genetic information into the treatment decision-making process may potentially improve patient management and outcomes [118]. Here, we will summarize the results of pharmacogenomics studies investigating how genes affect a person’s responses to pharmacological treatment, with a specific focus on alcohol, tobacco and opioid use disorders.
Several medications have demonstrated efficacy for the treatment of AUD, but pharmacological agents remain underutilized [119] and are only moderately effective with large variation in effects across patients. Pharmacotherapy for AUD targets neurotransmitter systems that are impacted by the consumption of alcohol, including opioidergic, dopaminergic, GABAergic, glutamatergic, and serotonergic neurotransmission [119]. Three medications are approved by the U.S. Food and Drug Administration (FDA) for the treatment of AUD: disulfiram, acamprosate, and naltrexone. There are also several drugs that are used off-label to treat AUD, including topiramate, gabapentin, baclofen, ondansetron and varenicline, among others [120].
Two recent reviews have summarized findings from pharmacogenetic studies for approved and off-label medications [119, 121]. The overall conclusion is that pharmacogenetic results are insufficient to inform clinical practice, due to small sample sizes and a lack of standardized trial designs and outcome measures. The most widely studied genetic polymorphism is rs1799971 as a potential mediator of naltrexone; this SNP encodes a non-synonymous substitution (Asn40Asp) in the mu-opioid receptor gene, OPRM1. A meta-analysis including seven RCTs found that the Asn40Asp SNP has a nominally significant moderating effect on drinks per day, while no significant associations were found for four other outcomes [122]. Therefore, the evidence for the utility of this SNP as a predictor of naltrexone response remains inconclusive. A summary of pharmacogenetic findings for the remaining medications is provided in Table 1.
While the majority of the pharmacogenetic studies have focused on candidate genes, a genome-wide pharmacogenomics study of acamprosate and naltrexone included 1083 European ancestry participants [74]. This study identified genetic variants near the PTPRD gene influencing time until drinking relapse in naltrexone-treated patients [74].
A combination of behavioural support and pharmacotherapy maximizes chances of successful long-term cessation of tobacco use. The most common pharmacological treatments of Tobacco Use Disorder are nicotine-replacement therapies, bupropion (a non-tricyclic antidepressant), and varenicline (a selective nicotinic receptor partial agonist). Meta-analyses have confirmed the efficacy of these therapies on abstinence at 6-month or longer follow-up, with varenicline being the superior treatment [123]. A large proportion of the ability to quit smoking is heritable (50–60%) [124]. Smokers with genetically slow nicotine metabolism have higher cessation success on behavioural counselling and nicotine patches compared with smokers with genetically fast nicotine metabolism [125].
Nicotine is primarily metabolized by CYP2A6, and variability in rate of metabolism contributes to vulnerability to tobacco dependence, and response to smoking cessation treatment [126]. El-Boraie and Tyndale have reviewed the results of pharmacogenomics studies on various smoking phenotypes [127]; here, we will focus primarily on summarizing data for genetic variants associated with smoking cessation and a genetically informed biomarker of nicotine clearance, the Nicotine Metabolite ratio (NMR).
Nicotine-replacement therapy
A meta-analysis of 18 trials (N = 9017) was conducted in 2019, including 40 active (bupropion, nicotine-replacement therapy [NRT], varenicline, or combination therapies) versus placebo comparisons and 16 active versus active comparisons [128]. Data were available for nine SNPs in five genes, two variable number of tandem repeat polymorphisms, and the NMR biomarker. The study revealed that non-Hispanic black smokers with rs16969968-GG genotypes were 3.5-fold and 5.8-fold more likely to abstain at 6 months and at end of treatment, respectively. This nonsynonymous variant is within the alpha-5 nicotinic acetylcholine receptor (CHRNA5) gene, and is strongly associated with smoking quantity and nicontine dependence in large-scale GWAS and functional studies [27, 49]. No evidence of rs16969968 effect modification was observed for non-Hispanic white smokers except for short-term outcomes. There was no clear statistical evidence for other genotype-by-treatment combinations nor for an association between the NMR and treatment outcomes. Most pharmacogenomics studies have focused on the role of one or more candidate genes, while treatment response is likely under polygenic influences of multiple variants with small and large effects. An elegant way to estimate the combined effect of multiple genetic variants is PGS analysis - Uhl et al. developed a PGS based on 12,058 SNPs and showed that this score significantly predicted ability to quit after nicotine patch treatment, with 43 vs 13% quit in the upper vs lower PGS terciles [129].
Bupropion
This dopamine and norepinephrine reuptake inhibitor and nicotine antagonist is widely used to treat depression. It is also one of the first-line pharmacotherapy options for smoking cessation [130]. Bupropion is metabolized to its active metabolite, hydroxybupropion (HB), by the genetically polymorphic cytochrome P450 2B6 (CYP2B6) enzyme [130]. Eum et al. meta-analyzed the results of ten studies (N = 413) evaluating the influence of CYP2B6 polymorphisms on bupropion exposure and on hydroxybupropion (HB), one of the three main active metabolites of bupropion and an important component for pharmacological activity and therapeutic effectiveness of the compound. The authors showed that the CYP2B6*6 allele and genotype-determined CYP2B6 poor and intermediate metabolizer phenotypes are associated with significantly lower total active moiety and reduced exposures to HB [130]. However, a meta-analysis of trials of smoking cessation pharmacotherapies did not reveal any differences between genotypes and efficacy of bupropion treatment outcomes, including 6-month abstinence, or end-of treatment abstinence [128]. However, the authors argued that the lack of significant associations may have been due to sample size limitations [128].
Varenicline
This partial agonist of nicotinic receptors in the central nervous system acts to relieve cravings and withdrawal symptoms as well as reducing the rewarding effect of smoking [123]. Varenicline undergoes almost no metabolism, but variation in the transport of varenicline throughout the body may alter treatment efficacy [125]. Similar as for bupropion, a meta-analysis of clinical trials did not reveal any differences between genotypes and efficacy of varenicline treatment outcomes, including 6-month abstinence, or end-of treatment abstinence [128]. There is some evidence that varenicline is more effective in those with rs16969968 GA/AA genotypes compared to GG genotypes in African American smokers although this finding will need to be replicated [131]. Another study found an association between CYP2B6 rs8109525 and varenicline efficacy [132], but this association did not survive correction for multiple testing and further replication is required.
Methadone maintenance therapy (MMT) is a substitute opioid therapy used to treat opioid withdrawal symptoms and is considered to be the most effective treatment for opioid addiction [133]. Genetic variability contributes to the effectiveness of MMT. Another commonly used pharmacotherapy for the treatment of OUD is buprenorphine, a weak MOR agonist and a partial kappa-opioid receptor antagonist, although buprenorphine seems to be less effective than MMT due to reduced retention in treatment [134]. A GWAS of buprenorphine treatment response revealed 6 nominally significant loci, four of which were located near previously characterized genes: rs756770 (ADAMTSL2), rs11782370 (SLC25A37), rs7205113 (CRISPLD2), and rs13169373 (LINC01947) [135]. Crist et al. reviewed pharmacogenetic findings of OUD treatment [134]. We refer the reader to this review for a full review of pharmacogenetic findings of OUD treatment dose and treatment response. In summary, due to a lack of large data sets with outcome and genotype data, there are no robust and replicable associations between genetic variants and OUD treatment outcomes. The most reproducible result is an association between the CYP2B6*6 allele and (S)-methadone plasma concentrations [134]. However, a meta-analysis of 7 articles did not find a significant association between CYP2B6*6 and methadone response [133].
Clinical implications and future work
Large-scale genetic studies have revolutionized the discovery of genetic loci associated with substance use disorders, especially for AUD, OUD, and TUD, while relatively few loci have been identified for CUD due to smaller sample sizes. The early promises of GWAS included the development of new and effective treatments and improved patient stratification. The availability of well-powered GWAS is a first step towards achieving these aims, although several barriers need to be overcome [45]. PGS explain around 2–6% of the phenotypic variation for AUD, OUD, and TUD and PGS can be used for risk stratification, diagnosis and treatment of substance use disorders, when used in combination with established risk measures [136]. In addition, the integration of GWAS data with molecular phenotypes may inform the identification of new and biologically relevant drug targets for substance use disorders through computational drug repurposing [45]. Future studies can be strengthened by the development of drug–gene databases across diverse cell types, including neuronal and other types of brain cells. In addition, new approaches have been developed to model the phenotypic complexity both within and across substance use disorders and will need to be applied at the widest possible scale, for example, by extending analyses to biobanks, such as the impending Global Biobank Meta-analysis Initiative [137].
References
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22.
American Psychiatric Association D, Association AP Diagnostic and statistical manual of mental disorders: DSM-5. vol. 5. Washington, DC: American Psychiatric Association; 2013.
Gaziano JM, Concato J, Brophy M, Fiore L, Pyarajan S, Breeling J, et al. Million Veteran Program: a mega-biobank to study genetic influences on health and disease. J Clin Epidemiol. 2016;70:214–23.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779.
Momozawa Y, Mizukami K. Unique roles of rare variants in the genetics of complex diseases in humans. J Hum Genet. 2021;66:11–23.
Verhulst B, Neale MC, Kendler KS. The heritability of alcohol use disorders: a meta-analysis of twin and adoption studies. Psychol Med. 2015;45:1061–72.
Walters RK, Polimanti R, Johnson EC, McClintick JN, Adams MJ, Adkins AE, et al. Transancestral GWAS of alcohol dependence reveals common genetic underpinnings with psychiatric disorders. Nat Neurosci. 2018;21:1656–69.
Hart AB, Kranzler HR. Alcohol dependence genetics: lessons learned from genome-wide association studies (GWAS) and post-GWAS analyses. Alcohol Clin Exp Res. 2015;39:1312–27.
Zhou H, Sealock JM, Sanchez-Roige S, Clarke T-K, Levey DF, Cheng Z, et al. Genome-wide meta-analysis of problematic alcohol use in 435,563 individuals yields insights into biology and relationships with other traits. Nat Neurosci. 2020;23:809–18.
Hatoum AS, Colbert SMC, Johnson EC, Huggett SB, Deak JD, Pathak GA, et al. Multivariate genome-wide association meta-analysis of over 1 million subjects identifies loci underlying multiple substance use disorders. Nat Ment Health. 2023;1:210–23.
Sulovari A, Liu Z, Zhu Z, Li D. Genome-wide meta-analysis of copy number variations with alcohol dependence. Pharmacogenomics J. 2018;18:398–405.
Ehlers CL, Wilhelmsen KC. Genomic scan for alcohol craving in Mission Indians. Psychiatr Genet. 2005;15:71–5.
Verweij KJH, Zietsch BP, Lynskey MT, Medland SE, Neale MC, Martin NG, et al. Genetic and environmental influences on cannabis use initiation and problematic use: a meta-analysis of twin studies. Addiction. 2010;105:417–30.
Agrawal A, Lynskey MT, Hinrichs A, Grucza R, Saccone SF, Krueger R, et al. A genome-wide association study of DSM-IV cannabis dependence. Addict Biol. 2011;16:514–8.
Sherva R, Wang Q, Kranzler H, Zhao H, Koesterer R, Herman A, et al. Genome-wide Association Study of Cannabis Dependence Severity, Novel Risk Variants, and Shared Genetic Risks. JAMA Psychiatry. 2016;73:472–80.
Agrawal A, Chou Y-L, Carey CE, Baranger DAA, Zhang B, Sherva R, et al. Genome-wide association study identifies a novel locus for cannabis dependence. Mol Psychiatry. 2018;23:1293–302.
Demontis D, Rajagopal VM, Thorgeirsson TE, Als TD, Grove J, Leppälä K, et al. Genome-wide association study implicates CHRNA2 in cannabis use disorder. Nat Neurosci. 2019;22:1066–74.
Johnson EC, Demontis D, Thorgeirsson TE, Walters RK, Polimanti R, Hatoum AS, et al. A large-scale genome-wide association study meta-analysis of cannabis use disorder. Lancet Psychiatry. 2020;7:1032–45.
Gizer IR, Bizon C, Gilder DA, Ehlers CL, Wilhelmsen KC. Whole genome sequence study of cannabis dependence in two independent cohorts. Addict Biol. 2018;23:461–73.
Sullivan PF, Kendler KS. The genetic epidemiology of smoking. Nicotine Tob Res. 1999;1 Suppl 2:S51–7; discussion S69-70.
Agrawal A, Verweij KJH, Gillespie NA, Heath AC, Lessov-Schlaggar CN, Martin NG, et al. The genetics of addiction-a translational perspective. Transl Psychiatry. 2012;2:e140.
Cohen LM, Myers MG, Kelly JF. Assessment of nicotine dependence among substance abusing adolescent smokers: a comparison of the DSM-IV criteria and the modified fagerström tolerance questionnaire. J Psychopathol Behav Assess. 2002;24:225–33.
Compton WM, Dawson DA, Goldstein RB, Grant BF. Crosswalk between DSM-IV dependence and DSM-5 substance use disorders for opioids, cannabis, cocaine and alcohol. Drug Alcohol Depend. 2013;132:387–90.
Hancock DB, Guo Y, Reginsson GW, Gaddis NC, Lutz SM, Sherva R, et al. Genome-wide association study across European and African American ancestries identifies a SNP in DNMT3B contributing to nicotine dependence. Mol Psychiatry. 2018;23:1911–9.
Quach BC, Bray MJ, Gaddis NC, Liu M, Palviainen T, Minica CC, et al. Expanding the genetic architecture of nicotine dependence and its shared genetics with multiple traits. Nat Commun. 2020;11:5562.
Toikumo S, Jennings MV, Pham B, Lee H, Mallard TT, Bianchi SB, et al. Multi-Ancestry Meta-Analysis of Tobacco Use Disorder Prioritizes Novel Candidate Risk Genes and Reveals Associations with Numerous Health Outcomes. medRxiv: The Preprint Server for Health Sciences. 2023. https://doi.org/10.1101/2023.03.27.23287713.
Saunders GRB, Wang X, Chen F, Jang S-K, Liu M, Wang C, et al. Genetic diversity fuels gene discovery for tobacco and alcohol use. Nature. 2022;612:720–4.
Yang J, Wang S, Yang Z, Hodgkinson CA, Iarikova P, Ma JZ, et al. The contribution of rare and common variants in 30 genes to risk nicotine dependence. Mol Psychiatry. 2015;20:1467–78.
Zuo L, Tan Y, Li C-SR, Wang Z, Wang K, Zhang X, et al. Associations of rare nicotinic cholinergic receptor gene variants to nicotine and alcohol dependence. Am J Med Genet B Neuropsychiatr Genet. 2016;171:1057–71.
Olfson E, Saccone NL, Johnson EO, Chen L-S, Culverhouse R, Doheny K, et al. Rare, low frequency and common coding variants in CHRNA5 and their contribution to nicotine dependence in European and African Americans. Mol Psychiatry. 2016;21:601–7.
Marees AT, Hammerschlag AR, Bastarache L, de Kluiver H, Vorspan F, van den Brink W, et al. Exploring the role of low-frequency and rare exonic variants in alcohol and tobacco use. Drug Alcohol Depend. 2018;188:94–101.
Rajagopal VM, Watanabe K, Mbatchou J, Ayer A, Quon P, Sharma D, et al. Rare coding variants in CHRNB2 reduce the likelihood of smoking. Nat Genet. 2023;55:1138–48.
Berrettini W. A brief review of the genetics and pharmacogenetics of opioid use disorders. Dialogues Clin Neurosci. 2017;19:229–36.
Tsuang MT, Lyons MJ, Meyer JM, Doyle T, Eisen SA, Goldberg J, et al. Co-occurrence of abuse of different drugs in men: the role of drug-specific and shared vulnerabilities. Arch Gen Psychiatry. 1998;55:967–72.
Nelson EC, Lynskey MT, Heath AC, Wray N, Agrawal A, Shand FL, et al. Association of OPRD1 polymorphisms with heroin dependence in a large case-control series. Addict Biol. 2014;19:111–21.
Gelernter J, Kranzler HR, Sherva R, Koesterer R, Almasy L, Zhao H, et al. Genome-wide association study of opioid dependence: multiple associations mapped to calcium and potassium pathways. Biol Psychiatry. 2014;76:66–74.
Cheng Z, Zhou H, Sherva R, Farrer LA, Kranzler HR, Gelernter J. Genome-wide association study identifies a regulatory variant of RGMA associated with opioid dependence in European Americans. Biol Psychiatry. 2018;84:762–70.
Polimanti R, Walters RK, Johnson EC, McClintick JN, Adkins AE, Adkins DE, et al. Leveraging genome-wide data to investigate differences between opioid use vs. opioid dependence in 41,176 individuals from the Psychiatric Genomics Consortium. Mol Psychiatry. 2020;25:1673–87.
Song W, Kossowsky J, Torous J, Chen C-Y, Huang H, Mukamal KJ, et al. Genome-wide association analysis of opioid use disorder: a novel approach using clinical data. Drug Alcohol Depend. 2020;217:108276.
Zhou H, Rentsch CT, Cheng Z, Kember RL, Nunez YZ, Sherva RM, et al. Association of OPRM1 functional coding variant with opioid use disorder: a genome-wide association study. JAMA Psychiatry. 2020;77:1072–80.
Gaddis N, Mathur R, Marks J, Zhou L, Quach B, Waldrop A, et al. Multi-trait genome-wide association study of opioid addiction: OPRM1 and beyond. Sci Rep. 2022;12:16873.
Deak JD, Zhou H, Galimberti M, Levey DF, Wendt FR, Sanchez-Roige S, et al. Genome-wide association study in individuals of European and African ancestry and multi-trait analysis of opioid use disorder identifies 19 independent genome-wide significant risk loci. Mol Psychiatry. 2022;27:3970–9.
Kember RL, Vickers-Smith R, Xu H, Toikumo S, Niarchou M, Zhou H, et al. Cross-ancestry meta-analysis of opioid use disorder uncovers novel loci with predominant effects in brain regions associated with addiction. Nat Neurosci. 2022;25:1279–87.
Li D, Zhao H, Kranzler HR, Li MD, Jensen KP, Zayats T, et al. Genome-wide association study of copy number variations (CNVs) with opioid dependence. Neuropsychopharmacology. 2015;40:1016–26.
Derks EM, Thorp JG, Gerring ZF. Ten challenges for clinical translation in psychiatric genetics. Nature Genetics. 2022;54:1457–65.
Gerring ZF, Thorp JG, Gamazon ER, Derks EM. A local genetic correlation analysis provides biological insights into the shared genetic architecture of psychiatric and substance use phenotypes. Biol Psychiatry. 2022;92:583–91.
Gerring ZF, Thorp JG, Gamazon ER, Derks EM. An analysis of genetically regulated gene expression and the role of co-expression networks across 16 psychiatric and substance use phenotypes. Eur J Hum Genet. 2022;30:560–6.
Zhang H, Grant BF, Hodgkinson CA, Ruan WJ, Kerridge BT, Huang B, et al. Strong and weak cross-inheritance of substance use disorders in a nationally representative sample. Mol Psychiatry. 2022;27:1742–53.
Liu M, Jiang Y, Wedow R, Li Y, Brazel DM, Chen F, et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat Genet. 2019;51:237–44.
Minică CC, Verweij KJH, van der Most PJ, Mbarek H, Bernard M, van Eijk KR, et al. Genome-wide association meta-analysis of age at first cannabis use. Addiction. 2018;113:2073–86.
Stringer S, Minică CC, Verweij KJH, Mbarek H, Bernard M, Derringer J, et al. Genome-wide association study of lifetime cannabis use based on a large meta-analytic sample of 32 330 subjects from the International Cannabis Consortium. Transl Psychiatry. 2016;6:e769.
Pasman JA, Verweij KJH, Gerring Z, Stringer S, Sanchez-Roige S, Treur JL, et al. GWAS of lifetime cannabis use reveals new risk loci, genetic overlap with psychiatric traits, and a causal effect of schizophrenia liability. Nat Neurosci. 2018;21:1161–70.
Sanchez-Roige S, Palmer AA, Fontanillas P, Elson SL, Adams MJ, Howard DM, et al. Genome-wide association study meta-analysis of the Alcohol Use Disorders Identification Test (AUDIT) in two population-based cohorts. Am J Psychiatry. 2019;176:107–18.
Marees AT, Smit DJA, Ong J-S, MacGregor S, An J, Denys D, et al. Potential influence of socioeconomic status on genetic correlations between alcohol consumption measures and mental health. Psychol Med. 2020;50:484–98.
Murray GK, Lin T, Austin J, McGrath JJ, Hickie IB, Wray NR. Could polygenic risk scores be useful in psychiatry?: A review. JAMA Psychiatry. 2021;78:210–9.
Zhou H, Kalayasiri R, Sun Y, Nuñez YZ, Deng H-W, Chen X-D, et al. Genome-wide meta-analysis of alcohol use disorder in East Asians. Neuropsychopharmacology. 2022;47:1791–7.
Yeung EW, Spychala KM, Miller AP, Otto JM, Deak JD, Kim H, et al. Effects of genetic risk for alcohol dependence and onset of regular drinking on the progression to alcohol dependence: A polygenic risk score approach. Drug Alcohol Depend. 2022;230:109117.
Wang FL, Hicks BM, Zhou H, Kranzler HR, Gelernter J, Zucker RA. Polygenic risk score for problematic alcohol use predicts heavy drinking and alcohol use disorder symptoms in young adulthood after accounting for adolescent alcohol use and parental alcohol use disorder. Drug Alcohol Depend. 2023;248:109909.
Lai D, Wetherill L, Bertelsen S, Carey CE, Kamarajan C, Kapoor M, et al. Genome-wide association studies of alcohol dependence, DSM-IV criterion count and individual criteria. Genes Brain Behav. 2019;18:e12579.
Kember RL, Hartwell EE, Xu H, Rotenberg J, Almasy L, Zhou H, et al. Phenome-wide association analysis of substance use disorders in a deeply phenotyped sample. Biol Psychiatry. 2023;93:536–45.
Johnson EC, Sanchez-Roige S, Acion L, Adams MJ, Bucholz KK, Chan G, et al. Polygenic contributions to alcohol use and alcohol use disorders across population-based and clinically ascertained samples. Psychol Med. 2021;51:1147–56.
Hunjan AK, Hübel C, Lin Y, Eley TC, Breen G. Association between polygenic propensity for psychiatric disorders and nutrient intake. Commun Biol. 2021;4:1–9.
Su J, Trevino AD, Kuo SI-C, Aliev F, Williams CD, Guy MC, et al. Racial discrimination and alcohol problems: examining interactions with genetic risk and impulsivity among African American young adults. J Youth Adolesc. 2022;51:1552–67.
Li JJ, Cho SB, Salvatore JE, Edenberg HJ, Agrawal A, Chorlian DB, et al. The impact of peer substance use and polygenic risk on trajectories of heavy episodic drinking across adolescence and emerging adulthood. Alcohol: Clin Exp Res. 2017;41:65–75.
Kranzler HR, Feinn R, Xu H, Ho BL, Saini D, Nicastro OR, et al. Does polygenic risk for substance-related traits predict ages of onset and progression of symptoms? Addiction. 2023;118:1675–86.
Vilar-Ribó L, Sánchez-Mora C, Rovira P, Richarte V, Corrales M, Fadeuilhe C, et al. Genetic overlap and causality between substance use disorder and attention-deficit and hyperactivity disorder. Am J Med Genet Part B Neuropsychiatr Genet. 2021;186:140–50.
Hartwell EE, Merikangas AK, Verma SS, Ritchie MD, Regeneron Genetics Center, Kranzler HR, et al. Genetic liability for substance use associated with medical comorbidities in electronic health records of African- and European-ancestry individuals. Addict Biol. 2022;27:e13099.
Lee WJ, Cheng H, Whitney BM, Nance RM, Britton SR, Jordahl K, et al. Polygenic risk scores point toward potential genetic mechanisms of type 2 myocardial infarction in people with HIV. Int J Cardiol. 2023;383:15–23.
Meyers JL, Chorlian DB, Johnson EC, Pandey AK, Kamarajan C, Salvatore JE, et al. Association of polygenic liability for alcohol dependence and EEG connectivity in adolescence and young adulthood. Brain Sci. 2019;9:280.
Zindler T, Frieling H, Fliedner L, Veer IM, Neyazi A, Awasthi S, et al. How alcohol makes the epigenetic clock tick faster and the clock reversing effect of abstinence. Addiction Biol. 2022;27:e13198.
Thomas NS, Kuo SI-C, Aliev F, McCutcheon VV, Meyers JM, Chan G, et al. Alcohol use disorder, psychiatric comorbidities, marriage and divorce in a high-risk sample. Psychol Addictive Behav. 2022;36:364–74.
Su J, Trevino A, Jamil B, Aliev F. Genetic risk of AUDs and childhood impulsivity: Examining the role of parenting and family environment. Dev Psychopathol. 2022;34:1827–40.
Cusack SE, Aliev F, Bustamante D, Dick DM, Amstadter AB. A statistical genetic investigation of psychiatric resilience. Eur J Psychotraumatol. 2023;14:2178762.
Biernacka JM, Coombes BJ, Batzler A, Ho AM-C, Geske JR, Frank J, et al. Genetic contributions to alcohol use disorder treatment outcomes: a genome-wide pharmacogenomics study. Neuropsychopharmacol. 2021;46:2132–9.
Taquet M, Smith SM, Prohl AK, Peters JM, Warfield SK, Scherrer B, et al. A structural brain network of genetic vulnerability to psychiatric illness. Mol Psychiatry. 2021;26:2089–2100.
Edwards AC, Heron J, Hibbeln J, Schuckit MA, Webb BT, Hickman M, et al. Long-chain ω-3 levels are associated with increased alcohol sensitivity in a population-based sample of adolescents. Alcohol Clin Exp Res. 2019;43:2620–6.
Segura AG, Mané A, Prohens L, Rodriguez N, Mezquida G, Cuesta MJ, et al. Exploration of cannabis use and polygenic risk scores on the psychotic symptom progression of a FEP cohort. Psychiatry Res. 2023;325:115249.
Cheng W, Parker N, Karadag N, Koch E, Hindley G, Icick R, et al. The relationship between cannabis use, schizophrenia, and bipolar disorder: a genetically informed study. Lancet Psychiatry. 2023;10:441–51.
Paul SE, Hatoum AS, Barch DM, Thompson WK, Agrawal A, Bogdan R, et al. Associations between cognition and polygenic liability to substance involvement in middle childhood: Results from the ABCD study. Drug Alcohol Depend. 2022;232:109277.
Chen W, Zeng Y, Suo C, Yang H, Chen Y, Hou C, et al. Genetic predispositions to psychiatric disorders and the risk of COVID-19. BMC Med. 2022;20:314.
Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet. 2014;23:R89–98.
Treur JL, Munafò MR, Logtenberg E, Wiers RW, Verweij KJH. Using Mendelian randomization analysis to better understand the relationship between mental health and substance use: a systematic review. Psychol Med. 2021;51:1593–624.
Davies NM, Holmes MV, Davey Smith G. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ. 2018;362:k601.
Richmond RC, Davey Smith G. Mendelian randomization: concepts and scope. Cold Spring Harb Perspect Med. 2022;12:a040501.
Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40:304–14.
Hartwig FP, Davey Smith G, Bowden J. Robust inference in summary data Mendelian randomization via the zero modal pleiotropy assumption. Int J Epidemiol. 2017;46:1985–98.
Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44:512–25.
Verbanck M, Chen C-Y, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. 2018;50:693–8.
Zhu Z, Zheng Z, Zhang F, Wu Y, Trzaskowski M, Maier R, et al. Causal associations between risk factors and common diseases inferred from GWAS summary data. Nat Commun. 2018;9:224.
Shapland CY, Zhao Q, Bowden J. Profile-likelihood Bayesian model averaging for two-sample summary data Mendelian randomization in the presence of horizontal pleiotropy. Stat Med. 2022;41:1100–19.
Minică CC, Dolan CV, Boomsma DI, de Geus E, Neale MC. Extending causality tests with genetic instruments: an integration of mendelian randomization with the classical twin design. Behav Genet. 2018;48:337–49.
Sanderson E, Davey Smith G, Windmeijer F, Bowden J. An examination of multivariable Mendelian randomization in the single-sample and two-sample summary data settings. Int J Epidemiol. 2019;48:713–27.
Brumpton B, Sanderson E, Heilbron K, Hartwig FP, Harrison S, Vie GÅ, et al. Avoiding dynastic, assortative mating, and population stratification biases in Mendelian randomization through within-family analyses. Nat Commun. 2020;11:3519.
Howe LJ, Nivard MG, Morris TT, Hansen AF, Rasheed H, Cho Y, et al. Within-sibship genome-wide association analyses decrease bias in estimates of direct genetic effects. Nat Genet. 2022;54:581–92.
Hwang L-D, Davies NM, Warrington NM, Evans DM. Integrating family-based and Mendelian randomization designs. Cold Spring Harb Perspect Med. 2021;11:a039503.
Li H, Zhang X, Zhang X, Wang Z, Feng S, Zhang G. Can intelligence affect alcohol-, smoking-, and physical activity-related behaviors? A Mendelian randomization study. J Intell. 2023;11:29.
Rosoff DB, Clarke T-K, Adams MJ, McIntosh AM, Davey Smith G, Jung J, et al. Educational attainment impacts drinking behaviors and risk for alcohol dependence: results from a two-sample Mendelian randomization study with ~780,000 participants. Mol Psychiatry. 2021;26:1119–32.
Burton SMI, Sallis HM, Hatoum AS, Munafò MR, Reed ZE. Is there a causal relationship between executive function and liability to mental health and substance use? A Mendelian randomization approach. R Soc Open Sci. 2022;9:220631.
Andrews SJ, Goate A, Anstey KJ. Association between alcohol consumption and Alzheimer’s disease: a Mendelian randomization study. Alzheimers Dement. 2020;16:345–53.
Mavromatis LA, Rosoff DB, Cupertino RB, Garavan H, Mackey S, Lohoff FW. Association between brain structure and alcohol use behaviors in adults: a Mendelian randomization and multiomics study. JAMA Psychiatry. 2022;79:869–78.
Logtenberg E, Overbeek MF, Pasman JA, Abdellaoui A, Luijten M, van Holst RJ, et al. Investigating the causal nature of the relationship of subcortical brain volume with smoking and alcohol use. Br J Psychiatry. 2022;221:337–85.
Topiwala A, Wang C, Ebmeier KP, Burgess S, Bell S, Levey DF, et al. Associations between moderate alcohol consumption, brain iron, and cognition in UK Biobank participants: observational and mendelian randomization analyses. PLoS Med. 2022;19:e1004039.
Adams AR, Li X, Byanyima JI, Vesslee SA, Nguyen TD, Wang Y, et al. Peripheral and central iron measures in alcohol use disorder and aging: a quantitative susceptibility mapping pilot study. Int J Mol Sci. 2023;24:4461.
Wootton RE, Greenstone HSR, Abdellaoui A, Denys D, Verweij KJH, Munafò MR, et al. Bidirectional effects between loneliness, smoking and alcohol use: evidence from a Mendelian randomization study. Addiction. 2021;116:400–6.
Lim KX, Rijsdijk F, Hagenaars SP, Socrates A, Choi SW, Coleman JRI, et al. Studying individual risk factors for self-harm in the UK Biobank: a polygenic scoring and Mendelian randomisation study. PLoS Med. 2020;17:e1003137.
Colbert SMC, Hatoum AS, Shabalin A, Li QS, Coon H, Nelson EC, et al. Exploring the genetic overlap of suicide-related behaviors and substance use disorders. Am J Med Genet B Neuropsychiatr Genet. 2021;186:445–55.
Bountress KE, Wendt F, Bustamante D, Agrawal A, Webb B, Gillespie N, et al. Potential causal effect of posttraumatic stress disorder on alcohol use disorder and alcohol consumption in individuals of European descent: a Mendelian Randomization Study. Alcohol: Clin Exp Res. 2021;45:1616–23.
Pasman JA, Smit DJA, Kingma L, Vink JM, Treur JL, Verweij KJH. Causal relationships between substance use and insomnia. Drug Alcohol Depend. 2020;214:108151.
Polimanti R, Peterson RE, Ong J-S, MacGregor S, Edwards AC, Clarke T-K, et al. Evidence of causal effect of major depression on alcohol dependence: findings from the psychiatric genomics consortium. Psychol Med. 2019;49:1218–26.
Chen D, Wang X, Huang T, Jia J. Genetic support of a causal relationship between cannabis use and educational attainment: a two-sample Mendelian randomization study of European ancestry. Addiction. 2023;118:698–710.
Johnson EC, Hatoum AS, Deak JD, Polimanti R, Murray RM, Edenberg HJ, et al. The relationship between cannabis and schizophrenia: a genetically informed perspective. Addiction. 2021;116:3227–34.
Gillespie NA, Kendler KS. Use of genetically informed methods to clarify the nature of the association between cannabis use and risk for schizophrenia. JAMA Psychiatry. 2021;78:467–8.
Reed ZE, Wootton RE, Munafò MR. Using Mendelian randomization to explore the gateway hypothesis: possible causal effects of smoking initiation and alcohol consumption on substance use outcomes. Addiction. 2022;117:741–50.
Vink JM, Treur JL, Pasman JA, Schellekens A. Investigating genetic correlation and causality between nicotine dependence and ADHD in a broader psychiatric context. Am J Med Genet B Neuropsychiatr Genet. 2021;186:423–9.
Lawlor DA, Tilling K, Davey Smith G. Triangulation in aetiological epidemiology. Int J Epidemiol. 2016;45:1866–86.
Munafò MR, Higgins JPT, Smith GD. Triangulating evidence through the inclusion of genetically informed designs. Cold Spring Harb Perspect Med. 2021;11:a040659.
van den Brink W. Evidence-based pharmacological treatment of substance use disorders and pathological gambling. Curr Drug Abus Rev. 2012;5:3–31.
Patriquin MA, Bauer IE, Soares JC, Graham DP, Nielsen DA. Addiction pharmacogenetics: a systematic review of the genetic variation of the dopaminergic system. Psychiatr Genet. 2015;25:181–93.
Hartwell EE, Kranzler HR. Pharmacogenetics of alcohol use disorder treatments: an update. Expert Opin Drug Metab Toxicol. 2019;15:553–64.
Kranzler HR, Soyka M. Diagnosis and Pharmacotherapy of Alcohol Use Disorder: A Review. JAMA. 2018;320:815–24.
Lohoff FW. Pharmacotherapies and personalized medicine for alcohol use disorder: a review. Pharmacogenomics. 2020;21:1117–38.
Hartwell EE, Feinn R, Morris PE, Gelernter J, Krystal J, Arias AJ, et al. Systematic review and meta-analysis of the moderating effect of rs1799971 in OPRM1, the mu-opioid receptor gene, on response to naltrexone treatment of alcohol use disorder. Addiction. 2020;115:1426–37.
Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta‐analysis. Cochrane Database Syst Rev. 2013;2013:CD009329.
Broms U, Silventoinen K, Madden PAF, Heath AC, Kaprio J. Genetic architecture of smoking behavior: A study of Finnish adult twins. Twin Res Hum Genet. 2006;9:64–72.
Chenoweth MJ, Tyndale RF. Pharmacogenetic optimization of smoking cessation treatment. Trends Pharmacol Sci. 2017;38:55–66.
Benowitz NL. Pharmacology of nicotine: addiction, smoking-induced disease, and therapeutics. Annu Rev Pharmacol Toxicol. 2009;49:57–71.
El-Boraie A, Tyndale RF. The role of pharmacogenetics in smoking. Clin Pharmacol Ther. 2021;110:599–606.
Panagiotou OA, Schuit E, Munafò MR, Bennett DA, Bergen AW, David SP. Smoking cessation pharmacotherapy based on genetically-informed biomarkers: what is the evidence? Nicotine Tob Res. 2019;21:1289–93.
Uhl GR, Walther D, Musci R, Fisher C, Anthony JC, Storr CL, et al. Smoking quit success genotype score predicts quit success and distinct patterns of developmental involvement with common addictive substances. Mol Psychiatry. 2014;19:50–4.
Eum S, Sayre F, Lee AM, Stingl JC, Bishop JR. Association of CYP2B6 genetic polymorphisms with bupropion and hydroxybupropion exposure: a systematic review and meta-analysis. Pharmacotherapy J Hum Pharmacol Drug Ther. 2022;42:34–44.
Chen L-S, Baker TB, Miller JP, Bray M, Smock N, Chen J, et al. Genetic variant in CHRNA5 and response to varenicline and combination nicotine replacement in a randomized placebo-controlled trial. Clin Pharmacol Ther. 2020;108:1315–25.
Tomaz PRX, Kajita MS, Santos JR, Scholz J, Abe TO, Gaya PV, et al. Cytochrome P450 2A6 and 2B6 polymorphisms and smoking cessation success in patients treated with varenicline. Eur J Clin Pharmacol. 2019;75:1541–5.
Dennis BB, Bawor M, Thabane L, Sohani Z, Samaan Z. Impact of ABCB1 and CYP2B6 genetic polymorphisms on methadone Metabolism, dose and treatment response in patients with opioid addiction: a systematic review and meta-analysis. PLoS ONE. 2014;9:e86114.
Crist RC, Clarke T-K, Berrettini WH. Pharmacogenetics of opioid use disorder treatment. CNS Drugs. 2018;32:305–20.
Crist RC, Vickers-Smith R, Kember RL, Rentsch CT, Xu H, Edelman EJ, et al. Analysis of genetic and clinical factors associated with buprenorphine response. Drug Alcohol Depend. 2021;227:109013.
Lewis CM, Vassos E. Polygenic risk scores: from research tools to clinical instruments. Genome Med. 2020;12:44.
Zhou W, Kanai M, Wu K-HH, Rasheed H, Tsuo K, Hirbo JB, et al. Global Biobank Meta-analysis Initiative: Powering genetic discovery across human disease. Cell Genomics. 2022;2:100192.
Grotzinger AD, Singh K, Miller-Fleming TW, Lam M, Mallard TT, Chen Y, et al. Transcriptome-wide structural equation modeling of 13 major psychiatric disorders for cross-disorder risk and drug repurposing. JAMA Psychiatry. 2023;80:811–21.
Acknowledgements
EMD, and ZFG are supported by NIH/NIA AG068026. KJHV and JL.T are supported by the Foundation Volksbond Rotterdam. JLT is supported by a European Research Council (ERC) Starting grant (UNRAVEL-CAUSALITY, grant number 101076686).
Author information
Authors and Affiliations
Contributions
ZFG, JTP, and EMD conceived and designed the study. ZFG and JT conducted the analyses. ZFG, JGT, JLT, KJHV, and EMD wrote the paper. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gerring, Z.F., Thorp, J.G., Treur, J.L. et al. The genetic landscape of substance use disorders. Mol Psychiatry (2024). https://doi.org/10.1038/s41380-024-02547-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41380-024-02547-z
- Springer Nature Limited