Abstract
Measurable residual disease (MRD) surveillance in acute myeloid leukemia (AML) may identify patients destined for relapse and thus provide the option of pre-emptive therapy to improve their outcome. Whilst flow cytometric MRD (Flow-MRD) can be applied to high-risk AML/ myelodysplasia patients, its diagnostic performance for detecting impending relapse is unknown. We evaluated this in a cohort comprising 136 true positives (bone marrows preceding relapse by a median of 2.45 months) and 155 true negatives (bone marrows during sustained remission). At an optimal Flow-MRD threshold of 0.040%, clinical sensitivity and specificity for relapse was 74% and 87% respectively (51% and 98% for Flow-MRD ≥ 0.1%) by ‘different-from-normal’ analysis. Median relapse kinetics were 0.78 log10/month but significantly higher at 0.92 log10/month for FLT3-mutated AML. Computational (unsupervised) Flow-MRD (C-Flow-MRD) generated optimal MRD thresholds of 0.036% and 0.082% with equivalent clinical sensitivity to standard analysis. C-Flow-MRD-identified aberrancies in HLADRlow or CD34+CD38low (LSC-type) subpopulations contributed the greatest clinical accuracy (56% sensitivity, 90% specificity) and notably, by longitudinal profiling expanded rapidly within blasts in > 40% of 86 paired MRD and relapse samples. In conclusion, flow MRD surveillance can detect MRD relapse in high risk AML and its evaluation may be enhanced by computational analysis.
Similar content being viewed by others
Introduction
Detection of impending relapse in acute leukemias allows selection of patients for pre-emptive therapies that may avoid ultimate treatment failure but also the challenges of cytoreduction and morbidities following hematological relapse. In acute myeloid leukemia, the evidence that sequential MRD testing can provide an early warning of relapse comes predominantly from studies applying real-time quantitative polymerase chain reaction (RT-qPCR) assays [1, 2]. Most of this data is for common PCR MRD leukemia targets PML-RARA, CBFB-MYH11, RUNX1-RUNX1T1, and NPM1 mutations although the relapse kinetics of other PCR targets, namely rarer rearrangements and overexpressed WTI have also been examined [3,4,5]. Based on the findings of these studies, definitions of treatment failure now include molecular MRD relapse (increase of MRD copy numbers ≥ 1 log10 or conversion from MRD negativity to MRD positivity, confirmed in a second sample) and RT-qPCR surveillance for MRD relapse after treatment (3 monthly if bone marrow sampling) is recommended for CBF and NPM1 mutated AML [2]. The term MRD relapse now also incorporates conversion from MRD negativity to positivity detected by other methods including flow cytometry and is thus applicable across AML subtypes [2]. There remain however unresolved issues that limit the information from sequential MRD results and therefore the clinical benefit and opportunities from MRD detection of impending relapse. These in part arise from the challenges of determining clinical specificity and sensitivity of a result to predict relapse when applying the recommended monitoring schedule. Conversion from MRD negativity to low level MRD positivity may have low predictive accuracy for relapse (low specificity), even when the sample MRD target is a high risk leukemic transcript such as DEK-NUP214 [5]. Although a second consecutive sample showing rising MRD levels can confirm MRD relapse, this risks reducing the interval for treatment decisions in the context of often unpredictable relapse kinetics. Furthermore, the majority of hematological relapses may not be identified by a preceding MRD positive test (low clinical sensitivity) despite using the recommended 3 monthly bone marrow monitoring schedules with established highly sensitive qPCR assays such as applied to CBF AML patients [6]. Additionally, as the use of flow cytometry or NGS for surveillance of impending relapse remains exploratory in AML [2, 7], there is an unmet need to extend MRD relapse detection to all AML patients. Moreover, parallel molecular and flow cytometric serial surveillance may be necessary for some patients such as when there is a risk of clonal evolution [8] including from treatment escape with loss of the molecular MRD target [9]. Although flow cytometric MRD has the advantage of rapid turn-around time in addition to a sensitivity of at least 10-4, the current dependence on manual analysis of bidimensional plots can lead to inconsistent quantitation according to expertise [10] and also limit the potential of deeper-immunophenotyping for further optimization.
We recently demonstrated the prognostic value of flow cytometric MRD monitoring performed during the first year following allogeneic stem cell transplantation [11]. This study now evaluates the clinical sensitivity and specificity of flow cytometric bone marrow MRD surveillance for early relapse prediction. We compare standard MRD detection with a newly developed computational analysis approach, investigating assay performance and aberrant immunophenotypic populations that are most specific for imminent relapse.
Methods
Samples and patients
Patient samples were from AML patients > 18 years old followed for flow cytometric measurable residual disease (MRD) detection using standard published methods [2, 12,13,14,15] by a single reference laboratory (Birmingham, UK) from April 2015 to September 2022. MRD bone marrow monitoring was conducted after completion of chemotherapy or post allogeneic hematopoietic stem cell transplantation (HSCT) in patients who had achieved a complete remission (CR) or CR with incomplete hematologic recovery (CRi). MRD detection analyses were conducted with informed patient consent in accordance with the Declaration of Helsinki and subject to appropriate ethics committee approval (NHS Health Research Authority REC reference 20/NW/0286).
MRD bone marrow samples preceding a hematological relapse (excluding APML patients) were retrospectively identified and included when a paired relapse sample had been received up to 4 months after the MRD sample with the diagnosis of relapse confirmed as at the timepoint of the relapse sample (Supplementary Fig. 1).
AML MRD monitoring control samples were defined as 1) post-treatment PCR negative bone marrows from patients with acute promyelocytic leukemia (APML) maintaining molecular remission (test control cohort) and 2) post treatment / HSCT bone marrows from non-favourable risk AML patients in continuous remission >6 months after MRD sample without a treatment intervention (validation control cohort). (Supplementary Fig. 1).
Additionally, pre-transplant bone marrow files from 156 patients entered into the FIGARO trial with previously reported standard flow cytometric MRD results [14] were included for clinical validation of computational analysis.
Flow cytometric MRD testing and analysis
MRD was assessed by flow cytometry as previously described in a central reference laboratory) [13, 14] Details on sample logistics, processing, panel and analysis strategy are provided in the Supplementary Methods. AML MRD panel was 7 colour until 2017 [13] and 8 colour thereafter [15]. Routine flow cytometric MRD analysis was performed using a standardized manual gating strategy that screened blasts for different-from-normal (DfN) aberrant immunophenotypes that were established as useful and frequently observed leukemic aberrant immunophenotypes (LAIPs) and also for any previously identified baseline LAIPs when available. Samples were reported as MRD-negative if no baseline and/or different-from-normal LAIP cells could be quantitated above assay threshold (of 0.05%).
To confirm the results of standard analysis, and exclude variability arising from subjective interpretation, flow cytometry standard files from MRD testing were analysed using a computational approach (C-Flow MRD), updated following previous clinical evaluation [11, 14]. Blast cells (CD117 + /CD34 + ) from test samples were clustered together with a 40-50 control BM reference set using the FlowSOM clustering algorithm. Automated decision tree analysis was then applied to define abnormal blasts with an immunophenotype significantly different from the reference set in 7-dimensional space (light scatter and CD45 parameters excluded). C-Flow-MRD results were calculated by summating discrete abnormal blast populations above the limit of detection (LOD), and the assay result reported as the highest value of the two tubes of the AML MRD antibody panel. Analyses of specific progenitor compartments for C-Flow-MRD+ blast cells were performed in FlowJo software through progenitor pre-set sub-gating based on optimised thresholds.
Statistical analyses
Receiver operating curve (ROC) statistics with area under the curve (AUC) were generated for MRD results of the clinical cohorts to summarise the discrimination ability of testing to predict relapse, with values of > 0.75 considered as good. Clinical specificity (true negative results (TN) ÷ [TN + false positives (FP)] x 100), sensitivity (true positive results (TP) ÷ [TP + false negatives (FN)] x 100), balanced accuracy ([%sensitivity + %specificity] ÷ 2) and Youden index ([sensitivity + specificity] – 1) were determined for test performance at specific assay cut-points. Optimal assay cut-points were derived from peaks in the Youden Index or alternatively by the R-based MaxStat package [16], which uses maximally selected rank statistics. Cumulative incidence of relapse (CIR) and treatment related mortality (TRM) from C-Flow-MRD applied to the previously published Figaro pre-transplant MRD sample dataset [14] were calculated using the ‘cumulative incidence of competing events and Gray test analysis’ and ‘Fine-Gray proportional hazard regression for competing events’ functions of the EZR software package v1.61 [17]. Further details are in Supplementary Methods.
Results
Flow cytometric MRD performance for detection of relapse during monitoring
To evaluate the diagnostic performance of routine flow cytometry MRD for detection of impending relapse at monitoring intervals of up to 4 months in a clinical setting, we interrogated the flow cytometric data of 136 MRD bone marrows preceding a paired relapse sample ( ≤ 4 months, median interval 2.45 months) from 118 patients who experienced relapse during longitudinal flow cytometric MRD monitoring (Supplementary Fig. 1, Table 1). MRD results were defined by MRD analysis that did not require a diagnostic sample (‘different-from-normal’/DfN approach, Methods).
89 of these ‘clinical positive’ samples were MRD positive resulting in a diagnostic sensitivity for subsequent relapse in 2 to 4 months of 64% for a result of MRD ≥ 0.05% and 51% for MRD ≥ 0.1%.
We then assessed the specificity of a flow cytometric MRD test to predict relapse using two reference sets of MRD bone marrow samples from non-relapsing patients (clinical negatives). In the first set compromising 55 APML follow-up bone marrows (PCR negative, no subsequent relapse), 9% had MRD ≥ 0.05%. A similar frequency of clinical false positives (8%) was observed in the second reference set, consisting of 100 monitoring MRD bone marrows identified from higher risk AML patients with sustained off-treatment relapse-free survival > 6 months after the sample, (Supplementary Fig. 1, Supplementary Table 1). This second reference set of ‘clinical negatives’ was predominantly from transplanted patients with a comparable frequency of higher risk genetics at diagnosis (39% ELN 2O22 adverse, 41% FLT3 mutations) to the relapse cohort (53% ELN 2O22 adverse, 23% FLT3 mutations).
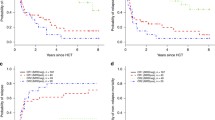
From the integrated dataset, MRD test specificity (for no relapse >6 months from test in the absence of intervention) was 91% for a result of ≥ 0.05%. From receiver operating characteristic curve analysis of combined pre-relapse and ‘clinical negative’ samples, the diagnostic accuracy of the routine flow cytometric MRD test to identify patients with imminent relapse ( < 4 months from test) was 0.85 (area under curve) with an optimal MRD clinical cut-off of 0.040% (sensitivity 74%, specificity 87%) in this retrospective cohort (Fig. 1A).
A Testing accuracy for pre-emptive detection of relapse by ‘different from normal’ MRD standard analysis. Receiver operating curve (ROC) statistics calculated from the combined cohort (136 true positives [relapse within 4 months of sample] and 121 true negatives [by sustained off-treatment remission after the sample]). Clinical specificity and sensitivity shown for routine assay thresholds (0.05% and ELN 0.10%) and optimum thresholds (derived from Maxstat package). B Relapse kinetics of high-risk AML. Relapse kinetics for 136 paired MRD and relapse bone marrows from 119 high risk AML patients. Relapse leukemic aberrant immunophenotypes were examined in MRD samples in parallel to standard ‘different-from-normal’ MRD analysis and kinetics calculated from the highest MRD values. Summary of relapse kinetics is shown for the overall sample cohort and specific diagnostic genetics subgroups; there was a significant difference (P = 0.026) in relapse kinetics between the FLT3-mutated and adverse cytogenetics /TP53 subgroups by non-parametric Mann-Whitney U testing.
Relapse kinetics
Kinetics of relapse can inform appropriate monitoring interval and choice of intervention but data as yet has been limited to PCR MRD targets. In this large sample cohort from 118 high risk AML patients experiencing relapse the median bone marrow increment was 0.78log10/month (IQR, 0.57-1.17), comparable to previous results for NPM1 mutated AML [18]. We observed similar results between different high risk genetic subgroups although there was a significantly higher median increment in patients with FLT3 mutations at diagnosis 0.92log10/month (IQR, 0.66–1.42) compared to patients with adverse risk cytogenetics or TP53 mutations (P = 0.026) (Fig. 1B).
Evaluation of MRD relapse detection using computational flow cytometric analysis
We developed a computational flow cytometric analysis tool incorporating a clustering algorithm and machine learning for standardised multidimensional MRD analysis (C-Flow-MRD) (Methods, Supplementary Methods). This performed different-from-normal’ unsupervised analysis against reference normal staging LPD BMs and required no baseline sample or expert annotation for MRD quantitation. The technical sensitivity of C-Flow-MRD from dilution experiments of different leukemic aberrant immunophenotypes (LAIPs) characterised by standard analysis was below 0.01% for most aberrancies (range 0.002- 0.02%) (Supplementary Fig. 2). The previously reported adverse prognostic impact of pretransplant MRD on relapse risk was recently confirmed in patients who entered the FIGARO trial, a randomized trial of reduced-intensity conditioning regimens [14]. The clinical validity of C-Flow-MRD was tested on this cohort of 156 transplanted patients. The prognostic performance of results generated by C-Flow-MRD was equivalent to routine Flow-MRD (Supplementary Fig. 3). We next applied C-Flow-MRD to the dataset of pre-relapse and all reference samples processed with the 8 colour AML MRD panel (Supplementary Methods). Optimal cut-off values by ROC analysis for detection of relapse were 0.036% and 0.08% with an equivalent clinical sensitivity to standard MRD (Supplementary Fig. 4.) There was good intertechnique agreement in MRD values between C-Flow and standard MRD (86% concordance, r = 0.83) (Supplementary Fig. 5A). Although some discrepant results were observed, including C-Flow-MRD+/standard MRD- values, these were reduced by the inclusion of myeloid control BMs into the reference set of control BMs (Supplementary Methods, Supplementary Fig. 5B).
Hierarchy for relapse prediction by MRD is dependent on progenitor compartment
Depending on the AML genetic subtype, leukemic cells may be variably distributed between CD34+ and CD34- subpopulations, however data is lacking for how this impacts MRD detection. We examined this by C-Flow-MRD to enable extended, objective phenotypic characterisation of aberrancies between CD34+ and CD34- blasts. In our cohort of high-risk AML patients, clinical sensitivity for relapse by C-Flow-MRD was substantially from CD34+ aberrancies, however for 8 of 90 analysed pre-relapse samples, MRD was only detectable in the CD34-117+ compartment. CD34-CD117+ blast based MRD added up to 9% clinical sensitivity to CD34+ blast based MRD with MRD cut-offs ranging from 0.04% to 0.1% and had comparable clinical specificity (close to 90% when MRD was >0.08%). Notably only 3 of 8 patients with CD34-CD117+ restricted C-Flow-MRD had NPM1 mutated AML (all 3 were also FLT3-ITD co-mutated). All relapse samples from these patients gained CD34+ aberrant populations, although CD34-CD117+ remained the predominant population (>95% of abnormal blasts) in 6.
Relapse-initiating cells may be enriched in certain hematopoietic stem and progenitor (HSPC) compartments associated with functional resistance through leukemic stem cell properties (CD34+CD38low) or immune evasion (such as HLADR downregulated HSPC). In our cohort that was skewed to post-allogeneic transplant relapses, C-Flow-MRD-detected aberrancies in the HLADRlow compartment provided the greatest effectiveness for clinical sensitivity and specificity (44% and 98% respectively above a cut-off of 0.02%) (Supplementary Fig. 6). Aberrancies of CD34+CD38low cells (LSC-type) contributed an additional 10% sensitivity (specificity of 93% above a cut-off of 0.02%) (Supplementary Fig. 6) notwithstanding the absence of certain LSC-specific markers (such as CD45RA, CLL-1 and CD123). We then examined incremental clinical sensitivity contributed by DfN aberrancies in other progenitor compartments that constitute established LAIPs using ELN core MRD markers. Of these, aberrancies in the CD7+ compartment provided the greatest increment in sensitivity for incipient relapse. Two thirds of pre-relapse samples were identified as C-Flow-MRD positive by one or more of the above three aberrancy categories whilst the cut-off of 0.02% maintained a specificity of ≥85% in the combined non-relapse samples (Supplementary Fig. 6). Most of the other tested aberrant subpopulations co-aggregated with these three (Fig. 2, Supplementary Fig. 7).
Each column represents one relapse. Samples grouped as MRD positive, MRD low positive and MRD negative by C-Flow MRD analysis of MRD timepoint. Results show presence for aberrant phenotype types detected at MRD timepoint (top 3 aberrancies of MRD blasts) and relapse timepoint (subsequent row, red = highest frequency aberrancy where top 3 MRD aberrancies are not detected).
Evolution in blast composition in months preceding relapse
Non-genetic modes of evolution may potentially contribute to progression to relapse and could be reflected by changes in the abundance of specific immunophenotypic aberrant populations within the progenitor compartment. We investigated this by C-Flow-MRD in 86 paired pre-relapse (MRD timepoint) and relapse samples. In 94% of cases with pre-relapse MRD positivity, one or more of the 3 most frequent MRD aberrancies were present at relapse (Fig. 2). Consistent with previous observations [19, 20], LSC or HLADR-low type aberrant subpopulations were frequent (Fig. 2) and abundant in blasts across relapsed patients (Fig. 3A). Additionally, in over 40% of relapse samples with these populations, we observed rapid expansion (≥10 fold) within blasts during the pre-relapse interval (median 2.45 months) (Fig. 3B). Overall, rapid expansion in LSC and /or HLADR-low type aberrant blasts occurred for 59% (51/86) of paired MRD and relapse samples. Prevalence was similar across the higher risk genetic categories for HLADR-low subpopulations; however 60% of relapses in patients with MDS-like mutations had a rapid expansion of LSC-like subpopulations compared to 32% with FLT3-ITD mutated AML.
A Frequency of displayed aberrant phenotypic subtype within relapse sample blasts. Overall frequency for CD34+ and CD34- compartments shown at end of graph. Box plots indicate the median and interquartile range for relapse samples where aberrancy is detectable as assessed objectively by computational unsupervised analysis (whiskers = 5-95th percentiles). Inset table displays detected versus non-detected frequency for each aberrant subtype (% of relapses). B Distribution of fold-changes in specific aberrant subtype frequency within blasts from pre-relapse MRD timepoint to relapse in paired samples (86 MRD samples paired with 76 relapses). Fold changes in total CD34+ and CD34- aberrancies shown at end of graph.
Other categories of detectable leukemic aberrant immunophenotypes had significantly lower abundance and relative expansion across patients. For example, CD11b+ type progenitor aberrancies, despite high MRD test specificity for relapse, remained as a relatively minor blast subpopulation (<10% of blasts) in most patients. We observed instability of certain aberrant populations between MRD and relapse, defined by a ≥ 10 fold reduction within blasts, in 21 of 86 relapse samples; 71% of the 21 had adverse cytogenetics and/or FLT3 mutations. Instability was most frequently observed with CD7+ type aberrancies. In all cases of instability, 1 or more other detectable MRD aberrant blast subpopulations expanded within relapse blasts (examples provided Supplementary Fig. 8).
Evolution to relapse resulted in loss of the major (first ranked) aberrancy of MRD positive samples or a shift in its immunophenotypic profile (up to ~0.5 log decade change for 1 or more markers) in 20% and 2% of relapse samples respectively (Supplementary Fig. 9). Loss or shift was more frequent if MRD sample had only low level positivity. In ~50% of cases the first ranked MRD aberrancy was no longer predominant at relapse.
Discussion
Although there is a clinical need for pre-emptive relapse detection in high-risk AML patients, there has been a gap in evidence for the predictive capability of serial off-treatment flow cytometric MRD testing. To address this, we evaluated flow cytometric MRD assay clinical performance in a large set of pre-relapse and non-relapse AML MRD samples. This evaluation was then extended to a potential tool for standardised interpretation of flow cytometric MRD, computational ‘different-from-normal’ flow cytometric MRD by an unsupervised analysis pipeline (C-Flow-MRD). Finally we applied the objective approach of C-Flow MRD to construct a hierarchy of aberrant progenitor compartments according to clinical specificity/sensitivity for relapse and examine their evolution profile in paired relapse samples.
Our results point to standard flow cytometric MRD as a highly specific predictor of relapse (98% ≥ 0.1%, 92% ≥ 0.05%) in higher risk AML for monitoring off-treatment by ‘different-from-normal’ analysis. This may obviate the requirement for a confirmatory repeat testing of a positive test as recommended based on experience from monitoring by PCR. Although over 60% of incipient relapses were detected by flow cytometric MRD ≥ 0.05%, this reduced to 50% when the higher current ELN threshold of 0.1% was applied. It is likely that extending monitoring interval beyond 2–3 months will further reduce clinical sensitivity. Our data underlines why a single MRD negative test should be interpreted with caution, notwithstanding the relatively short intervals of serial testing, due to rapid kinetics in a proportion of patients. The median log increase estimate per month in this high-risk cohort is comparable to that reported for NPM1 mutated patients by PCR derived results (0.7 log10 per month) [18]. Consistent with clinical observations, results here show the highest median monthly log increase was apparent in the FLT3 mutated subgroup even compared to those with adverse cytogenetics. More sensitive targeted deep sequencing-based assays for FLT3-ITD mutated variants (threshold of 0.01-0.001%) have the technical capacity to allow earlier MRD detection, but as a counterpoint, instability of these mutations risks false negatives, and the assays currently have a higher cost and slower turnaround time than flow cytometric MRD.
Importantly this study demonstrates the potential of computational unsupervised pipelines for analysis of flow cytometric MRD, not only to facilitate standardised interpretation but also to objectively distinguish aberrant immunophenotypes that have the greatest accuracy for pre-emptive relapse detection. Incorporating myeloid controls into the reference or ‘training set’ allowed further exclusion of what we term candidate ‘aberrant immunophenotypes with indeterminate potential’ (AIP-IP). Such AIP-IPs may be associated with clonal hematopoiesis [21,22,23] but screening for this by NGS molecular profiling was not possible in these samples. We anticipate that single cell genotypic and immunophenotypic approaches are most likely to resolve whether specific AIP-IPs are restricted to cells with clonal mutations or represent epigenetic mechanisms [24, 25]. Once AIP-IPs are identified, in our pipeline they can be incorporated into the unsupervised training sample set, analogous to the process that informs expert manual MRD analysis.
Unsupervised analysis by C-Flow-MRD allowed broad characterisation of immunophenotypic aberrant blast subpopulations. Leveraging this for the paired MRD and relapse samples, we examined blast composition longitudinally through disease progression in order to identify aberrant HSPC subtypes most likely to escape disease control. We observed positive selection of aberrant HSPC subpopulations with weak/negative expression of CD38 (on CD34+) and/or HLADR– a finding in ~45% of this high-risk AML cohort by the metric of >10-fold relative expansion within the blast compartment in the months preceding relapse. MRD detection of these subpopulations also had the highest accuracy for relapse. These results require validation with larger data sets and there are other limitations to consider. Aberrant subpopulation evolution is likely to depend on preceding treatments; the majority of our paired MRD and relapse samples were post-transplant. Additionally, our assay had a restricted number of markers and was limited to blasts expressing CD34 and/or CD117. However extending this approach to further paired pre-relapse and relapse sample sets in AML and MDS may map immunophenotypic compartments enriched for leukemic cells with competitive advantage versus neutral evolution. This provides a potential tool for targeted multiomic profiling of relapse cell subpopulations to decipher the properties of fitness advantage and rapid relapse kinetics according to treatment. Our findings also have implications with regards future optimisation of recently proposed strategies to improve MRD detection depth by mutational screening on sorted HSPC populations [26, 27].
In summary this study supports the utility of flow cytometric MRD for pre-emptive relapse surveillance in high-risk AML and provides a platform for the application of unsupervised MRD analysis to standardise and enhance evaluation of emerging leukemia.
Data availability
All data generated and analyzed in this study are included in this published article and its supplementary materials and figures. Raw datasets are available on reasonable request to corresponding author.
References
Schuurhuis GJ, Heuser M, Freeman S, Bene MC, Buccisano F, Cloos J, et al. Minimal/measurable residual disease in AML: a consensus document from the European LeukemiaNet MRD Working Party. Blood. 2018;131:1275–91.
Heuser M, Freeman SD, Ossenkoppele GJ, Buccisano F, Hourigan CS, Ngai LL, et al. 2021 Update on Measurable Residual Disease (MRD) in Acute Myeloid Leukemia (AML): A Consensus Document from the European LeukemiaNet MRD Working Party. Blood. 2021;138:2753–67.
Ommen HB, Hokland P, Haferlach T, Abildgaard L, Alpermann T, Haferlach C, et al. Relapse kinetics in acute myeloid leukaemias with MLL translocations or partial tandem duplications within the MLL gene. Br J Haematol. 2014;165:618–28.
Ommen HB, Schnittger S, Jovanovic JV, Ommen IB, Hasle H, Ostergaard M, et al. Strikingly different molecular relapse kinetics in NPM1c, PML-RARA, RUNX1-RUNX1T1, and CBFB-MYH11 acute myeloid leukemias. Blood. 2010;115:198–205.
Ommen HB, Touzart A, MacIntyre E, Kern W, Haferlach T, Haferlach C, et al. The kinetics of relapse in DEK-NUP214-positive acute myeloid leukemia patients. Eur J Haematol. 2015;95:436–41.
Puckrin R, Atenafu EG, Claudio JO, Chan S, Gupta V, Maze D, et al. Measurable residual disease monitoring provides insufficient lead-time to prevent morphologic relapse in the majority of patients with core-binding factor acute myeloid leukemia. Haematologica. 2021;106:56–63.
Dohner H, Wei AH, Appelbaum FR, Craddock C, DiNardo CD, Dombret H, et al. Diagnosis and Management of AML in Adults: 2022 ELN Recommendations from an International Expert Panel. Blood. 2022;140:1345–77.
Hollein A, Meggendorfer M, Dicker F, Jeromin S, Nadarajah N, Kern W, et al. NPM1 mutated AML can relapse with wild-type NPM1: persistent clonal hematopoiesis can drive relapse. Blood Adv. 2018;2:3118–25.
Schmalbrock LK, Dolnik A, Cocciardi S, Strang E, Theis F, Jahn N, et al. Clonal evolution of acute myeloid leukemia with FLT3-ITD mutation under treatment with midostaurin. Blood. 2021;137:3093–104.
Lawrence L. Making MRD Assessment Work for AML. 2023.
Loke J, McCarthy N, Jackson A, Siddique S, Hodgkinson A, Mason J, et al. Posttransplant MRD and T-cell chimerism status predict outcomes in patients who received allografts for AML/MDS. Blood Adv. 2023;7:3666–76.
Tettero JM, Freeman S, Buecklein V, Venditti A, Maurillo L, Kern W, et al. Technical Aspects of Flow Cytometry-based Measurable Residual Disease Quantification in Acute Myeloid Leukemia: Experience of the European LeukemiaNet MRD Working Party. Hemasphere. 2022;6:e676.
Freeman SD, Hills RK, Virgo P, Khan N, Couzens S, Dillon R, et al. Measurable Residual Disease at Induction Redefines Partial Response in Acute Myeloid Leukemia and Stratifies Outcomes in Patients at Standard Risk Without NPM1 Mutations. J Clin Oncol. 2018;36:1486–97.
Craddock C, Jackson A, Loke J, Siddique S, Hodgkinson A, Mason J, et al. Augmented Reduced-Intensity Regimen Does Not Improve Postallogeneic Transplant Outcomes in Acute Myeloid Leukemia. J Clin Oncol. 2021;39:768–78.
Freeman SD, Thomas A, Thomas I, Hills RK, Vyas P, Gilkes A, et al. Fractionated vs single-dose gemtuzumab ozogamicin with determinants of benefit in older patients with AML: the UK NCRI AML18 trial. Blood. 2023;142:1697–707.
Hothorn T, Lausen B. On the exact distribution of maximally selected rank statistics. Computational Stat Data Anal. 2003;43:121–37.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48:452–8.
Ivey A, Hills RK, Simpson MA, Jovanovic JV, Gilkes A, Grech A, et al. Assessment of Minimal Residual Disease in Standard-Risk AML. N. Engl J Med. 2016;374:422–33.
Zeng AGX, Bansal S, Jin L, Mitchell A, Chen WC, Abbas HA, et al. A cellular hierarchy framework for understanding heterogeneity and predicting drug response in acute myeloid leukemia. Nat Med. 2022;28:1212–23.
Christopher MJ, Petti AA, Rettig MP, Miller CA, Chendamarai E, Duncavage EJ, et al. Immune Escape of Relapsed AML Cells after Allogeneic Transplantation. N. Engl J Med. 2018;379:2330–41.
Loghavi S, DiNardo CD, Furudate K, Takahashi K, Tanaka T, Short NJ, et al. Flow cytometric immunophenotypic alterations of persistent clonal haematopoiesis in remission bone marrows of patients with NPM1-mutated acute myeloid leukaemia. Br J Haematol. 2021;192:1054–63.
Jevremovic D, Nanaa A, Geyer SM, Timm M, Azouz H, Hengel C, et al. Abnormal CD13/HLA-DR Expression Pattern on Myeloblasts Predicts Development of Myeloid Neoplasia in Patients With Clonal Cytopenia of Undetermined Significance. Am J Clin Pathol. 2022;158:530–6.
Porwit A, Bene MC, Duetz C, Matarraz S, Oelschlaegel U, Westers TM, et al. Multiparameter flow cytometry in the evaluation of myelodysplasia: Analytical issues: Recommendations from the European LeukemiaNet/International Myelodysplastic Syndrome Flow Cytometry Working Group. Cytom B Clin Cytom. 2023;104:27–50.
Dillon LW, Ghannam J, Nosiri C, Gui G, Goswami M, Calvo KR, et al. Personalized Single-Cell Proteogenomics to Distinguish Acute Myeloid Leukemia from Non-Malignant Clonal Hematopoiesis. Blood Cancer Discov. 2021;2:319–25.
Robinson TM, Bowman RL, Persaud S, Liu Y, Neigenfind R, Gao Q, et al. Single-cell genotypic and phenotypic analysis of measurable residual disease in acute myeloid leukemia. Sci Adv. 2023;9:eadg0488.
Stasik S, Burkhard-Meier C, Kramer M, Middeke JM, Oelschlaegel U, Sockel K, et al. Deep sequencing in CD34+ cells from peripheral blood enables sensitive detection of measurable residual disease in AML. Blood Adv. 2022;6:3294–303.
Dimitriou M, Mortera-Blanco T, Tobiasson M, Mazzi S, Lehander M, Hogstrand K, et al. Identification and surveillance of rare relapse-initiating stem cells during complete remission post-transplantation. Blood. 2024;143:953–66.
Acknowledgements
We would like to thank Blood Cancer UK for research support. This research was supported in part by the Intramural Research Program of the NIH and NHLBI.
Author information
Authors and Affiliations
Contributions
Conception and design: Sylvie D Freeman, Nicholas McCarthy, Christophe Roumier, Adriana Plesa, Florent Dumezy, Gege Gui. Collection and assembly of data: Sylvie D Freeman, Alexandra Adams, Georgia Andrew, Sarah Green, Naeem Khan, Nicholas McCarthy. Data analysis and interpretation: Nicholas McCarthy, Sylvie D. Freeman, Madeleine Jenkins, Gege Gui, Christophe Roumier, Adriana Plesa, Florent Dumezy. Manuscript writing: Sylvie D Freeman, Nicholas McCarthy. Final approval of manuscript: All authors. Accountable for all aspects of the work: All authors.
Corresponding author
Ethics declarations
Competing interests
NM, FD, AP, CR, GA, SG, AA, MJ, and AP, have no conflicts to declare. SDF declares research funding from Jazz and BMS; Speakers Bureau with Jazz, Pfizer and Novartis; advisory committee with MPAACT. CH and GG, The National Heart, Lung, and Blood Institute receives research funding for the laboratory of Dr. Hourigan from the Foundation of the NIH AML MRD Biomarkers Consortium.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
McCarthy, N., Gui, G., Dumezy, F. et al. Pre-emptive detection and evolution of relapse in acute myeloid leukemia by flow cytometric measurable residual disease surveillance. Leukemia (2024). https://doi.org/10.1038/s41375-024-02300-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41375-024-02300-z
- Springer Nature Limited