Abstract
Objective
Evaluate the association of short-term tracheal intubation (TI) outcomes with premedication in the NICU.
Study design
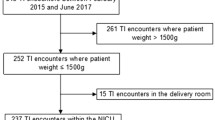
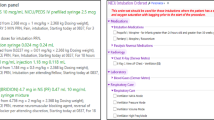
Observational single-center cohort study comparing TIs with full premedication (opiate analgesia and vagolytic and paralytic), partial premedication, and no premedication. The primary outcome is adverse TI associated events (TIAEs) in intubations with full premedication compared to those with partial or no premedication. Secondary outcomes included change in heart rate and first attempt TI success.
Results
352 encounters in 253 infants (median gestation 28 weeks, birth weight 1100 g) were analyzed. TI with full premedication was associated with fewer TIAEs aOR 0.26 (95%CI 0.1–0.6) compared with no premedication, and higher first attempt success aOR 2.7 (95%CI 1.3–4.5) compared with partial premedication after adjusting for patient and provider characteristics.
Conclusion
The use of full premedication for neonatal TI, including an opiate, vagolytic, and paralytic, is associated with fewer adverse events compared with no and partial premedication.



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sawyer T, Foglia E, Hatch LD, Moussa A, Ades A, Johnston L, et al. Improving neonatal intubation safety: a journey of a thousand miles. J Neonatal-Perinat Med. 2017;10:125–31.
Krick J, Gray M, Umoren R, Lee G, Sawyer T. Premedication with paralysis improves intubation success and decreases adverse events in very low birth weight infants: a prospective cohort study. J Perinatol [Internet]. 2018;38:681–6. http://www.nature.com/articles/s41372-018-0082-2
Foglia EE, Ades A, Napolitano N, Leffelman J, Nadkarni V, Nishisaki A. Factors associated with adverse events during tracheal intubation in the NICU. Neonatology. 2015;108:23–9.
Ozawa Y, Ades A, Foglia EE, DeMeo S, Barry J, et al. for the National Emergency Airway Registry for Neonates (NEAR4NEOS) Investigators. Premedication with neuromuscular blockade and sedation during neonatal intubation is associated with fewer adverse events. J Perinatol [Internet]. 2019;39:848–56. http://www.nature.com/articles/s41372-019-0367-0
Carbajal R, Eble B, Anand KJS. Premedication for tracheal intubation in neonates: confusion or controversy? Semin Perinatol. 2007;31:309–17.
Roberts KD, Leone TA, Edwards WH, Rich WD, Finer NN. Premedication for nonemergent neonatal intubations: a randomized, controlled trial comparing atropine and fentanyl to atropine, fentanyl, and mivacurium. Pediatrics. 2006;118:1583–91.
Wallenstein MB, Birnie KL, Arain YH, Yang W, Yamada NK, Huffman LC, et al. Failed endotracheal intubation and adverse outcomes among extremely low birth weight infants. J Perinatol J Calif Perinat Assoc. 2016;36:112–5.
Dempsey EM, Al Hazzani F, Faucher D, Barrington KJ. Facilitation of neonatal endotracheal intubation with mivacurium and fentanyl in the neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed. 2006;91:F279–82.
Sauer CW, Kong JY, Vaucher YE, Finer N, Proudfoot JA, Boutin MA, et al. Intubation attempts increase the risk for severe intraventricular hemorrhage in preterm infants—a retrospective cohort study. J Pediatr [Internet]. 2016;177:108–13. https://linkinghub.elsevier.com/retrieve/pii/S0022347616304176
Friesen RH, Honda AT, Thieme RE. Changes in anterior fontanel pressure in preterm neonates during tracheal intubation. Anesth Analg. 1987;66:874–8.
Kumar P, Denson SE, Mancuso TJ, Committee on Fetus and Newborn, Section on Anesthesiology and Pain Medicine. Premedication for nonemergency endotracheal intubation in the neonate. PEDIATRICS [Internet]. 2010;125:608–15. https://doi.org/10.1542/peds.2009-2863.
Byrne E. Should premedication be used for semi-urgent or elective intubation in neonates? Arch Dis Child [Internet]. 2005;91:79–83. https://doi.org/10.1136/adc.2005.087635.
Ballabh P. Intraventricular hemorrhage in premature infants: mechanism of disease. Pediatr Res. 2010;67:1–8.
Glenn TJ, Grathwol MM, McClary JD, Wainwright RJ, Gorman SM, Rodriguez AM, et al. Decreasing time from decision to intubation in premedicated neonates: a quality improvement initiative. Pediatr Qual Saf [Internet]. 2019;4:e234 https://journals.lww.com/10.1097/pq9.0000000000000234
Hatch LD, Grubb PH, Lea AS, Walsh WF, Markham MH, Whitney GM, et al. Endotracheal intubation in neonates: a prospective study of adverse safety events in 162 infants. J Pediatr. 2016;168:62–66.e6.
Muniraman H, Yaari J, Hand I. Premedication use before nonemergent intubation in the newborn infant. Am J Perinatol [Internet]. 2015;32:821–4. https://doi.org/10.1055/s-0034-1543987.
Sarkar S, Schumacher RE, Baumgart S, Donn SM. Are newborns receiving premedication before elective intubation? J Perinatol J Calif Perinat Assoc. 2006;26:286–9.
Lemyre B, Cheng R, Gaboury I. Atropine, fentanyl and succinylcholine for non-urgent intubations in newborns. Arch Dis Child Fetal Neonatal Ed. 2009;94:F439–42.
Nishisaki A, Turner DA, Brown CA, Walls RM, Nadkarni VM, National Emergency Airway Registry for Children (NEAR4KIDS). et al. A National Emergency Airway Registry for children: landscape of tracheal intubation in 15 PICUs. Crit Care Med. 2013;41:874–85.
Foglia EE, Ades A, Sawyer T, Glass KM, Singh N, Jung P, et al. Neonatal intubation practice and outcomes: an international registry study. Pediatrics [Internet] 2019;143:e20180902 https://doi.org/10.1542/peds.2018-0902.
Johnston L, Kwon SH. Moving from controversy to consensus: premedication for neonatal intubation. J Perinatol [Internet]. 2018;38:611–3. https://www.nature.com/articles/s41372-018-0115-x
COMMITTEE ON FETUS AND NEWBORN, Barfield WD, Papile LA, Baley JE, Benitz W, Cummings J, et al. Levels of neonatal care. Pediatr [Internet]. 2012;130:587–97. https://doi.org/10.1542/peds.2012-1999.
Stevens TP, Harrington EW, Blennow M, Soll RF. Early surfactant administration with brief ventilation vs. selective surfactant and continued mechanical ventilation for preterm infants with or at risk for respiratory distress syndrome. Cochrane Database Syst Rev. 2007. https://doi.org/10.1002/14651858.CD003063.pub3.
Sk H, Saha B, Mukherjee S, Hazra A. Premedication with fentanyl for less invasive surfactant application (LISA): a randomized controlled trial. J Trop Pediatr. 2022;68:fmac019.
Bohlin K, Gudmundsdottir T, Katz-Salamon M, Jonsson B, Blennow M. Implementation of surfactant treatment during continuous positive airway pressure. J Perinatol J Calif Perinat Assoc. 2007;27:422–7.
Marshall TA, Deeder R, Pai S, Berkowitz GP, Austin TL. Physiologic changes associated with endotracheal intubation in preterm infants. Crit Care Med. 1984;12:501–3.
Hodgson KA, Owen LS, Kamlin COF, Roberts CT, Newman SE, Francis KL, et al. Nasal high-flow therapy during neonatal endotracheal intubation. N Engl J Med [Internet]. 2022;386:1627–37. https://doi.org/10.1056/NEJMoa2116735.
Miller KE, Singh N. Association of multiple tracheal intubation attempts with clinical outcomes in extremely preterm infants: a retrospective single-center cohort study. J Perinatol Off J Calif Perinat Assoc. 2022. https://doi.org/10.1038/s41372-022-01406-5.
Zimmerman KO, Smith PB, Benjamin DK, Laughon M, Clark R, Traube C, et al. Sedation, analgesia, and paralysis during mechanical ventilation of premature infants. J Pediatr [Internet]. 2017;180:99–104.e1. https://linkinghub.elsevier.com/retrieve/pii/S0022347616305224
Acknowledgements
We would like to thank the pediatric residents, neonatal fellows, advance practice providers, and attending neonatologists at the University of Washington Medical Center, Montlake NICU, for their timely completion of the NEAR4NEOS data collection forms. We also extend thanks to Hayley Buffman at the Children’s Hospital of Philadelphia for her commitment to neonatal intubation safety and maintenance of the NEAR4NEOS database.
Author information
Authors and Affiliations
Contributions
SKN was responsible for study concept, data form auditing, extracting, and analyzing data, interpretation of results, and report writing. BKB was responsible for unit protocol changes, data form auditing, and report edits. RU contributed to the interpretation of results and provided feedback on the report. MMG guided with statistical analysis and presentation of data and provided feedback on the report. TS provided feedback on the report and AN and EF were responsible for generating the NEAR4NEOS centralized repository for neonatal intubation safety data and provided feedback on the report.
Corresponding author
Ethics declarations
Competing interests
The authors have no financial disclosures or conflicts of interest. NEAR4NEOS has been supported by NICHD HD089151. There was no direct funding for this analysis.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Neches, S.K., Brei, B.K., Umoren, R. et al. Association of full premedication on tracheal intubation outcomes in the neonatal intensive care unit: an observational cohort study. J Perinatol 43, 1007–1014 (2023). https://doi.org/10.1038/s41372-023-01632-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01632-5
- Springer Nature America, Inc.