Abstract
Objective
Given that regionalization of extremely preterm births (EPTBs) is associated with improved infant outcomes, we assessed between-hospital variation in EPTB stratified by hospital level of neonatal care, and determined the proportion of variance explained by differences in maternal and hospital factors.
Study design
We assessed 7,046,253 births in California from 1997 to 2011, using hospital discharge, birth, and death certificate data. We estimated the association between maternal and hospital factors and EPTB using multivariable regression, calculated hospital-specific EPTB frequencies, and estimated between-hospital variances and median odds ratios, stratified by hospital level of care.
Result
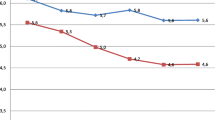
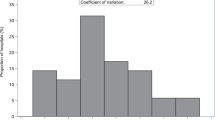
Hospital frequencies of EPTB ranged from 0% to 2.5%. Between-hospital EPTB frequencies varied substantially, despite stratifying by hospital level of care and accounting for confounding factors.
Conclusion
Our results demonstrate differences in EPTBs among hospitals with level 1 and 2 neonatal care, an area to target for future research and quality improvement.


Similar content being viewed by others
Data availability
The datasets used in this study are publicly available from the California Office of Statewide Planning and Development. The coding and raw data generated during our analyses are available from the corresponding author upon reasonable request.
References
Lau C, Ambalavanan N, Chakraborty H, Wingate MS, Carlo WA. Extremely low birth weight and infant mortality rates in the United States. Pediatrics. 2013;131:855–60.
Hamilton BE, Hoyert DL, Martin JA, Strobino DM, Guyer B. Annual summary of vital statistics: 2010-2011. Pediatrics. 2013;131:548–58.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 2015;314:1039–51.
Taylor HG, Klein N, Minich NM, Hack M. Long-term family outcomes for children with very low birth weights. Arch Pediatr Adolesc Med. 2001;155:155–61.
Lakshmanan A, Agni M, Lieu T, Fleegler E, Kipke M, Friedlich PS, et al. The impact of preterm birth <37 weeks on parents and families: a cross-sectional study in the 2 years after discharge from the neonatal intensive care unit. Health Qual Life Outcomes. 2017;15:38.
Grosse SD, Waitzman NJ, Yang N, Abe K, Barfield WD. Employer-sponsored plan expenditures for infants born preterm. Pediatrics. 2017; 140. https://doi.org/10.1542/peds.2017-1078.
Beam AL, Fried I, Palmer N, Agniel D, Brat G, Fox K, et al. Estimates of healthcare spending for preterm and low-birthweight infants in a commercially insured population: 2008-2016. J Perinatol J Calif Perinat Assoc. 2020;40:1091–9.
Holmstrom ST, Phibbs CS. Regionalization and mortality in neonatal intensive care. Pediatr Clin North Am. 2009;56:617–30.
Neto MT. Perinatal care in Portugal: effects of 15 years of a regionalized system. Acta Paediatr. 2006;95:1349–52.
Rautava L, Lehtonen L, Peltola M, Korvenranta E, Korvenranta H, Linna M, et al. The effect of birth in secondary- or tertiary-level hospitals in Finland on mortality in very preterm infants: a birth-register study. Pediatrics. 2007;119:e257–263.
Jensen EA, Lorch SA. Effects of a birth hospital’s neonatal intensive care unit level and annual volume of very low-birth-weight infant deliveries on morbidity and mortality. JAMA Pediatr. 2015;169:e151906.
Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH. Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N. Engl J Med. 2007;356:2165–75.
Shah KP, deRegnier R-AO, Grobman WA, Bennett AC. Neonatal mortality after interhospital transfer of pregnant women for imminent very preterm birth in Illinois. JAMA Pediatr. 2020;174:358–65.
Redpath S, Shah PS, Moore GP, Yang J, Toye J, Perreault T, et al. Do transport factors increase the risk of severe brain injury in outborn infants <33 weeks gestational age? J Perinatol. 2020;40:385–93.
Whitham M, Dudley DJ. Delivering neonates at high risk in the right place: back to the future again. JAMA Pediatr. 2020;174:329–30.
Bullens LM, Moors S, van Runnard Heimel PJ, van der Hout-van der Jagt MB, Oei SG. Practice variation in the management of intrapartum fetal distress in The Netherlands and the Western world. Eur J Obstet Gynecol Reprod Biol. 2016;205:48–53.
Bannister-Tyrrell M, Patterson JA, Ford JB, Morris JM, Nicholl MC, Roberts CL. Variation in hospital caesarean section rates for preterm births. Aust NZ J Obstet Gynaecol. 2015;55:350–6.
Herrchen B, Gould JB, Nesbitt TS. Vital statistics linked birth/infant death and hospital discharge record linkage for epidemiological studies. Comput Biomed Res Int J. 1997;30:290–305.
How does CDC identify severe maternal morbidity? | CDC. 2021. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/smm/severe-morbidity-ICD.htm.
Regional Perinatal Programs of California. https://www.cdph.ca.gov/Programs/CFH/DMCAH/RPPC/Pages/Default.aspx.
American Academy of Pediatrics Committee on Fetus and Newborn. Levels of neonatal care. Pediatrics. 2012;130:587–97.
Stark AR. American Academy of Pediatrics Committee on Fetus and Newborn. Levels of neonatal care. Pediatrics. 2004;114:1341–7.
Merlo J, Chaix B, Ohlsson H, Beckman A, Johnell K, Hjerpe P, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006;60:290–7.
Binder S, Hill K, Meinzen-Derr J, Greenberg JM, Narendran V. Increasing VLBW deliveries at subspecialty perinatal centers via perinatal outreach. Pediatrics. 2011;127:487–93.
Acknowledgements
This work was supported by the March of Dimes Prematurity Research Center at Stanford University and by the Stanford Maternal and Child Health Research Institute. Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under award number R01HD098287. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
GPG, PK, CSP, EM, GMS, and HCL planned and designed the study. PK and HCL acquired the data. PK and GPG analyzed the data. GPG wrote the initial manuscript draft. All authors edited the manuscript. GPG had the primary responsibility for the final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Goldstein, G.P., Kan, P., Phibbs, C.S. et al. Hospital variation in extremely preterm birth. J Perinatol 42, 1686–1694 (2022). https://doi.org/10.1038/s41372-022-01505-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01505-3
- Springer Nature America, Inc.