Abstract
Objective
Less invasive surfactant administration (LISA) has proved to safely improve morbidity in extreme preterms with respiratory distress syndrome (RDS). Its effect regarding intraventricular hemorrhage (IVH) remains controversial between most recent systematic reviews. We aimed to evaluate its effect over incidence of severe IVH in this population.
Study design
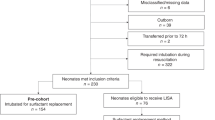
We compared the incidence of IVH in a prospective cohort of consecutively born preterm infants <34 weeks’ gestation receiving LISA (n = 108) with a historical cohort receiving surfactant delivery via tracheal tube and managed with mechanical ventilation (n = 100).
Results
No significant differences regarding perinatal characteristics were observed between both groups. There was a significant reduction in the incidence of severe IVH in LISA group as compared with the historical group [OR = 0.054 (95% CI 0.01–0.2) p = 0.000. NNT 5]. In addition, a significant trend towards decreased mortality was also observed in the study group [OR = 0.2 (95% CI 0.04–0.9) p = 0.027, NNT 9]. Intervention group infants also showed lower oxygenation requirements during the first 72 h post surfactant administration and a reduced incidence of pneumothorax. They were less frequently intubated [31 infants (28.4%) vs. 100 [100%]; P < 0.001] and required fewer days of mechanical ventilation. However, no significant difference in bronchopulmonary dysplasia incidence was observed between both groups.
Conclusions
LISA approach effectively reduces severe IVH in very low and low birth weight (BW) preterms with RDS. In addition we observe a significant trend towards reduction in both need and duration of MV support, air leak, and overall mortality in the intervention group.


Similar content being viewed by others
References
SUPPORT Study Group of the Eunice Kennedy Shriver NICHD Neonatal Research Network. Finer NN, Carlo WA, Walsh MC, Rich W, Gantz MG, et al. Early CPAP versus surfactant in extremely preterm infants. N. Engl J Med. 2010;362:1970–9.
Morley CJ, Davis PG, Doyle LW, Brion LP, Hascoet JM, Carlin JB, et al. Nasal CPAP or intubation at birth for very preterm infants. N. Engl J Med. 2008;358:700–8.
Dunn MS, Kaempf J, de Klerk A, de Klerk R, Reilly M, Howard D, et al. Randomized trial comparing 3 approaches to the initial respiratory management of preterm neonates. Pediatrics. 2011;128:1069–76.
Schmölzer GM, Kumar M, Pichler G, Aziz K, O’Reilly M, Cheung PY. Non-invasive versus invasive respiratory support in preterm infants at birth: systematic review and meta-analysis. BMJ. 2013;347:5980.
Yost CC, Soll RF. Early versus delayed selective surfactant treatment for neonatal respiratory distress syndrome. Cochrane Database Syst Rev. 2000;2:CD001456.
Soll RF, Morley CJ. Prophylactic versus selective use of surfactant in preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev. 2001;2:CD000510.
Verder H, Robertson B, Greisen G, Ebbesen F, Albertsen P, Lundstrøm K, et al. Surfactant therapy and nasal continuous positive airway pressure for newborns with respiratory distress syndrome. Danish-Swedish Multicenter Study Group. N. Engl J Med. 1994;331:1051–5.
Verder H, Albertsen P, Ebbesen F, Greisen G, Robertson B, Bertelsen A, et al. Nasal continuous positive airway pressure and early surfactant therapy for respiratory distress syndrome in newborns of less than 30 weeks’ gestation. Pediatrics. 1999;103:E24.
Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Plavka R, et al. European Consensus. Guidelines on the Management of Respiratory Distress Syndrome-2016 Update. Neonatology. 2017;111:107–25.
Bohlin K, Bouhafs RK, Jarstrand C, Cursted T, Blennow M, Robertson B. Spontaneous breathing or mechanical ventilation alters lung compliance and tissue association of exogenous surfactant in preterm newborn rabbits. Pediatr Res. 2005;57(Pt 1):624–30.
Björklund LJ, Ingimarsson J, Curstedt T, John J, Robertson B, Werner O, et al. Manual ventilation with a few large breaths at birth compromises the therapeutic effect of subsequent surfactant replacement in immature lambs. Pediatr Res. 1997;42:348–55.
Verder H, Agertoft L, Albertsen P, Christensen NC, Curstedt T, Ebbesen F, et al. Surfactant treatment of newborn infants with respiratory distress syndrome primarily treated with nasal continuous positive air pressure. A pilot study. Ugeskr Laege. 1992;154:2136–9.
Kribs A, Pillekamp F, Hünseler C, Vierzig A, Roth B. Early administration of surfactant in spontaneous breathing with nCPAP: feasibility and outcome in extremely premature infants (postmenstrual age < /=27 weeks). Paediatr Anaesth. 2007;17(Apr):364–9.
Dargaville PA, Aiyappan A, Cornelius A, Williams C, De Paoli AG. Preliminary evaluation of a new technique of minimally invasive surfactant therapy. Arch Dis Child Fetal Neonatal Ed. 2011;96:243–8.
Göpel W, Kribs A, Ziegler A, Laux R, Hoehn T, Wieg C, et al. German Neonatal Network. Avoidance of mechanical ventilation by surfactant treatment of spontaneously breathing preterm infants (AMV): an open-label, randomized, controlled trial. Lancet. 2011;378:1627–34.
Kanmaz HG, Erdeve O, Canpolat FE, Mutlu B, Dilmen U. Surfactant administration via thin catheter during spontaneous breathing: randomized controlled trial. Pediatrics. 2013;131:502–9.
Kribs A, Roll C, Göpel W, Wieg C, Groneck P, Laux R, et al. NINSAPP trial investigators. Non intubated surfactant application vs conventional therapy in extremely preterm infants: a randomized clinical trial. JAMA Pediatr. 2015;169(Aug):723–30.
Aldana-Aguirre JC, Pinto M, Featherstone RM, Kumar M. Less invasive surfactant administration versus intubation for surfactant delivery in preterm infants with respiratory distress syndrome: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2017;102(Jan):17–23.
Härtel C, Paul P, Hanke K, Humberg A, Kribs A, Mehler K, et al. Less invasive surfactant administration and complications of preterm birth. Sci Rep. 2018;8(May):8333.
Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Te Pas A, et al. European consensus guidelines on the management of respiratory distress syndrome 2019 update. Neonatology. 2019;115(Apr):432–45.
Isayama T, Iwami H, McDonald S, Beyene J. Association of noninvasive ventilation strategies with mortality and bronchopulmonary dysplasia among preterm infants: a systematic review and meta-analysis. JAMA. 2016;316(Aug):611–24.
Volpe JJ. Intraventricular hemorrhage in the premature infant. Current concepts. Part I Ann Neurol. 1989;25:3–11.
Perlman JM, Wyllie J, Kattwinkel J, Wyckoff MH, Aziz K, Guinsburg R, et al. On behalf of the Neonatal Resuscitation Chapter Collaborators. Part 7: neonatal resuscitation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Circulation. 2015;132(suppl 1):S204–41.
Higgins RD, Jobe AH, Koso-Thomas M, Bancalari E, Viscardi RM, Hartet TV, et al. Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr. 2018;197(Jun):300–8.
Bell MJ, Ternberg J, Fengin RR. Neonatal necrotizing enterocolitis: therapeutic decisions based on clinical staging. Ann Surg. 1978;187:1–7.
Rezaie P, Dean A. Periventricular leukomalacia, inflammation and white matter lesions within the developing nervous system. Neuropathology. 2002;22:106–32.
International Committee for the Classification of Retinopathy of Prematurity. The international classification of retinopathy of prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Klebermass-Schrehof K, Wald M, Schwindt J, Grill A, Prusa AR, Haiden N, et al. Less invasive surfactant administration in extremely preterm infants: impact on mortality and morbidity. Neonatology. 2013;103:252–8.
Da Costa CS, Czosnyka M, Smielewski P, Mitra S, Stevenson GN, Austin T, et al. Monitoring of cerebrovascular reactivity for determination of optimal blood pressure in preterm infants. J Pediatr. 2015;167:86–91.
Soul JS, Hammer PE, Tsuji M, Saul JP, Bassan H, Limperopoulos C, et al. Fluctuating pressure-passivity is common in the cerebral circulation of sick premature infants. Pediatr Res. 2007;61:467–73.
Wu TW, Azhibekov T, Seri I. Transitional hemodynamics in preterm neonates: clinical relevance. Pediatr Neonatol. 2016;57:7–18.
Ballabh P, Braun A, Nedergaard M. Anatomic analysis of blood vessels in germinal matrix, cerebral cortex, and white matter in developing infants. Pediatr Res. 2004;56:117–24.
Menke J, Michel E, Rabe H, Bresser BW, Grohs B, Schmitt RM, et al. Simultaneous influence of blood pressure, PCO2, and PO2 on cerebral blood flow velocity in preterm infants of less than 33 weeks’ gestation. Pediatr Res. 1993;34:173–7.
Toledo JD, Rodilla S, Pérez-Iranzo A, Delgado A, Maazouzi Y, Vento M. Umbilical cord milking reduces the risk of intraventricular hemorrhage in preterm infants born before 32 weeks of gestation. J Perinatol. 2019;39(Apr):547–53.
Sinclair SE, Chi E, Lin HI, Altemeier WA. Positive end-expiratory pressure alters the severity and spatial heterogeneity of ventilator-induced lung injury: an argument for cyclical airway collapse. J Crit Care. 2009;24:206–11.
Hillman NH, Kallapur SG, Pillow JJ, Moss TJ, Polglase GR, Nitsos I, et al. Airway injury from initiating ventilation in preterm sheep. Pediatr Res. 2010;67:60–5.
Lau, CSM, Chamberlain RS, Sun S. Less invasive surfactant administration reduces the need for mechanical ventilation in preterm infants: a meta-analysis. Glob Pediatr Health. 2017;4:2333794X17696683. Published 2017 Mar 24. https://doi.org/10.1177/2333794X17696683.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443.
Farhath S, He Z, Nakhla T, Saslow J, Soundar S, Camacho J, et al. Pepsin, a marker of gastric contents, is increased in tracheal aspirates from preterm infants who develop bronchopulmonary dysplasia. Pediatrics. 2008;121:253–9.5.
Farhath S, Aghai ZH, Nakhla T, Saslow J, He Z, Soundar S, et al. Pepsin, a reliable marker of gastric aspiration, is frequently detected in tracheal aspirates from premature ventilated neonates: relationship with feeding and methylxanthine therapy. J Ped Gastr Nutr. 2006;43:336–41.
Ufberg JW, Bushra JS, Patel D, Wong E, Karras DJ, Kueppers F. A new pepsin assay to detect pulmonary aspiration of gastric contents among newly intubated patients. Am J Emerg Med. 2004;22:612–4.
Wallenstein MB, Brooks C, Kline TA, Beck RQ, Yang W, Shaw GM, et al. Early transpyloric vs gastric feeding in preterm infants: a retrospective cohort study. J Perinatol. 2019;39(Jun):837–41.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pérez-Iranzo, A., Jarque, A., Toledo, J.D. et al. Less invasive surfactant administration reduces incidence of severe intraventricular haemorrage in preterms with respiratory distress syndrome: a cohort study. J Perinatol 40, 1185–1192 (2020). https://doi.org/10.1038/s41372-020-0702-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0702-5
- Springer Nature America, Inc.