Abstract
Background
Neonatal transpyloric feeding (TPF) has not been rigorously studied since the 1980s. Our objective was to evaluate early TPF, defined as TPF initiated within the first week after birth, among preterm infants in the setting of modern neonatal practice.
Study design
A retrospective cohort study was conducted between 2013 and 2017 for all extremely low birth weight (ELBW) infants born in a tertiary neonatal intensive care unit where early TPF is a common practice. Infants were excluded if they did not receive enteral feeding within the first week after birth or if they died prior to initiation of enteral feeding. The primary outcome was death or bronchopulmonary dysplasia (BPD). The association between early TPF and the primary outcome was assessed using multivariable logistic regression, with adjustment for gestational age, birth weight, and intubation status.
Result
The study sample included 368 ELBW infants. Twenty-seven percent received early TPF. Death or BPD occurred in 58% of infants who received early TPF compared with 67% of infants who received gastric feeding, adjusted odds ratio 0.6, 95% confidence interval 0.3–0.9. Growth and adverse gastrointestinal outcomes did not differ between the two groups.
Conclusion
Early TPF is associated with reduced risk of death or BPD among ELBW infants. Further investigation in the form of a randomized controlled trial is required to confirm a causal association between early TPF and improved clinical outcomes.
Similar content being viewed by others
Introduction
Lung disease is the primary cause of death for preterm infants [1,2,3]. Strategies designed to reduce or eliminate lung injury have transformed neonatology over the past several decades and decreased neonatal mortality worldwide. However, pulmonary aspiration remains a ubiquitous source of lung injury among preterm infants today [4, 5].
Two studies found that aspiration of gastric contents is pervasive among preterm infants and that the quantity of aspirated contents directly correlates with the severity of lung disease and development of bronchopulmonary dysplasia (BPD) [4, 5]. Transpyloric feeding (TPF), an effective strategy to reduce aspiration risk in adults and children [6, 7], was once a common practice in the early era of neonatal intensive care, but it fell out of favor in the 1980s due to safety concerns and has not been rigorously studied since that time [8,9,10,11,12,13,14,15,16,17].
As a result, TPF is considered a bygone practice by most neonatologists, despite its potential to prevent aspiration-associated lung injury among critically-ill preterm infants [18]. Our primary objective was to evaluate early TPF, defined as TPF initiated within the first week after birth, among extremely low birth weight (ELBW) infants in a tertiary NICU where early TPF is common practice.
Methods
A retrospective cohort study was conducted for all ELBW infants admitted to the Fairfax Neonatal Associates Neonatal Intensive Care Unit (NICU) at Inova Children’s Hospital in Falls Church, Virginia between January 2013 and December 2017. This study population represents a sample of available and extractable data from electronic health records. All inborn patients with birth weights less than 1001 g were screened for eligibility. Infants were excluded if they did not receive enteral feeding within the first week after birth or if they died prior to initiation of enteral feeding. There were no additional exclusion criteria. The study adhered to institutional ethical human research guidelines and was approved by the Institutional Review Board with waiver of informed consent at Inova Children’s Hospital.
Maternal, baseline, and outcome data were collected, including the primary composite outcome of neonatal death or BPD, defined by supplemental oxygen or positive pressure (includes high flow nasal cannula) requirement at 36 weeks’ postmenstrual age (PMA). Secondary outcomes included weight at 36 weeks’ PMA, delta z-score (z-score for weight at 36 weeks’ PMA minus z-score at birth), duration of mechanical ventilation, duration of central lines (all types, including umbilical), and umbilical lines (arterial and/or venous), length of stay, necrotizing enterocolitis (Bell stage II or greater), spontaneous intestinal perforation (pneumoperitoneum without pneumatosis), intraventricular hemorrhage (IVH) grade 3 or 4, periventricular leukomalacia, surgical patent ductus arteriosus (PDA) ligation, culture positive sepsis, and antibiotic duration greater than 7 days.
All infants adhered to an institution-specific feeding protocol. For infants less than 26 weeks’ gestation, the protocol consisted of trophic feeds (10 ml/kg/day) for 3 days, followed by daily advancement of 10–15 ml/kg/day to a goal of 160 ml/kg/day, with fortification beginning at 100 ml/kg/day. For infants ≥26 weeks’ gestation, the protocol consisted of trophic feeds (10 ml/kg/day) for 2 days, followed by daily advancement of 10–20 ml/kg/day to a goal of 160 ml/kg/day, with fortification beginning at 100 ml/kg/day. Patients less than 26 weeks’ gestation that were born prior to October 2014 adhered to a slightly different feeding protocol, in which they received trophic feeds (5 ml/kg/day) for 3 days, followed by daily advancement of 5–10 ml/kg/day to a goal of 160 ml/kg/day. Gastric feeds were given as boluses every 3 or 4 h or continuously. TPF was always given continuously at the same total daily volume in ml/kg/day. With rare exception, all infants received maternal breast milk or donor breast milk.
During the period of study at Inova Children’s Hospital, TPF was a common management strategy for the prevention of aspiration and feeding intolerance among ELBWs, but there was no formal protocol to guide clinical practice. The decision to initiate TPF was at the discretion of the attending neonatologist. As a result, there was substantial variation in the timing of initiation of TPF among the study population—though the majority of ELBWs received TPF at some point during their NICU stay. Typical indications for initiating TPF included, but were not limited to, signs of gastroesophageal reflux, pulmonary aspiration, or feeding intolerance in an infant receiving positive pressure ventilation or continuous positive airway pressure—e.g., abdominal distension, emesis, apnea, or bradycardia, among others.
Statistical analysis was performed with Statistical Analysis Software, version 9.4 (SAS Institute, Cary, NC). Measures of central tendency were used to describe continuous variables, including mean, median, and interquartile range. Categorical variables were described using frequencies and percentages. Infants who received early TPF, defined as TPF initiated within the first week after birth, were compared to infants who received gastric feeding using the Student’s t-test, Wilcoxon rank sum test, Chi-squared test, Fisher’s exact test, and Wald chi-squared test as appropriate. Note that infants in the gastric-feeding group may have received TPF later in their hospital course. Multivariable logistic regression was used to estimate odds ratios, 95% confidence intervals (CI), and Wald chi-squared test, adjusting for potentially confounding variables, including gestational age, birth weight, and intubation status. Statistical significance was set at p-value < 0.05.
Results
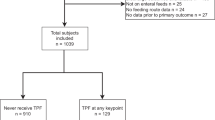
Between January 2013 and December 2017, 418 inborn ELBW infants were admitted to the NICU at Inova Children’s Hospital. Thirty-one infants died prior to initiation of enteral feeding and 19 did not receive enteral feeding during the first week after birth, leaving 368 infants that were included in the final analysis. Among these 368 infants, 27% received early TPF, defined as TPF initiated within the first week after birth. Baseline characteristics are shown in Table 1. Infants who received gastric feeding were less likely to have been intubated after birth compared to infants who received early TPF (p < 0.01), otherwise there were no significant differences between the two groups.
Growth outcomes are shown in Table 2 and did not differ between the two groups. Primary and secondary outcomes are shown in Table 3. Death or BPD occurred in 58% of infants who received early TPF compared with 67% of infants who received gastric feeding, with an adjusted odds ratio (aOR) of 0.6 (95% CI 0.3–0.9). Early TFP was also associated with shorter duration of mechanical ventilation (12.7 vs 20.6 days, p < 0.01), shorter duration of umbilical lines (5.9 vs 6.6 days, p < 0.05), and less antibiotic use for greater than 7 days (aOR 0.6, 95% CI 0.3–0.9). There were no significant differences between groups for other adverse outcomes, including necrotizing enterocolitis and spontaneous intestinal perforation. Additional analysis confirmed that BPD, IVH, and NEC did not co-occur with substantial frequency.
Discussion
In this retrospective cohort study, early TPF was associated with reduced risk of death or BPD, shorter duration of mechanical ventilation, fewer umbilical line days, and less prolonged antibiotic use, compared with gastric feeding. Growth and other adverse outcomes were no different between the two groups. Our findings suggest that early TPF may improve outcomes for ELBW infants.
However, we could not rule out confounding by indication, given the retrospective design and limited availability of patient data. To address this, we controlled for potentially confounding variables, including gestational age, birth weight, and intubation status, which served as a proxy for baseline illness severity. We found that infants who received early TPF may have been sicker at baseline compared to infants who received gastric feeding (19% never intubated in early TPF group vs 33% in gastric feeding group), which would favor a causal rather than confounded relationship with improved outcomes. The difference in illness severity at baseline was anticipated, given that typical indications for early TPF tend to occur more frequently among sicker patients (see Patients and Methods section). Shorter duration of mechanical ventilation in the early TPF group, in spite of having a significantly higher proportion of intubated patients at baseline, further supports a causal relationship. Nevertheless, it is still possible that the two groups had different baseline characteristics that we were unable to measure—characteristics that might independently predict both a positive outcome and receipt of early TPF. It is also conceivable that the decision to initiate early TPF reflected a difference in experience among neonatal providers, which might also predict positive outcomes.
The most compelling argument for a causal relationship between early TPF and improved outcomes is its biological plausibility. It is intuitive that aspiration of caustic stomach contents is likely to exacerbate lung disease in preterm infants. Extrapolation from the adult literature is also persuasive. Meta-analysis of 14 clinical trials found that TPF effectively reduces the risk of aspiration [7], which is widely known to exacerbate lung disease and increase mortality in adults [19].
Among neonates, the data are sparse but intriguing. Farhath et al. collected 495 tracheal aspirate samples from 104 ventilator-dependent infants less than 32 weeks’ gestation [4, 5]. The authors detected pepsin, a sensitive and specific marker of gastric contents [20,21,22], in 92% of tracheal aspirate samples and in 100% of infants at least once. A similar study among critically-ill adults detected pepsin in only 10% of patients [23]. Aspiration is uniquely prevalent among preterm infants due to immature tone of the lower esophageal sphincter, delayed gastric emptying, and use of uncuffed endotracheal tubes, among other factors [24,25,26,27].
Further analysis by Farhath et al. revealed that infants who developed BPD or died had three-fold higher tracheal pepsin concentrations in the first week after birth, compared with infants who did not develop BPD (865 vs 269 ng/mg protein, p < 0.01). In addition, the authors found evidence of a dose-response effect, in which the concentration of pepsin in tracheal aspirates directly correlated with severity of BPD [4].
Early (or prophylactic) TPF, which is initiated shortly after birth and is the focus of the present study, should be distinguished from late (or indicated) TPF, which is initiated after lung injury has already occurred among older neonates with severe BPD or clinically-apparent gastroesophageal reflux. The latter is a relatively common practice in NICUs today. Two retrospective studies among preterm infants with suspected gastroesophageal reflux found that late TPF reduced episodes of apnea and bradycardia, compared to gastric feeding [28, 29]. One of these studies found potential hazard associated with use of formula during TPF [28].
To the best of our knowledge, the present study represents the first evaluation of early TPF in almost three decades. Early TPF was common practice among neonatologists until a single trial demonstrated increased mortality in the 1980s [10], causing a chilling effect on further research. A 2013 Cochrane review of nine randomized controlled trials (primarily from the 1970s and 1980s) of transpyloric vs gastric feeding found no significant difference in mortality after controlling for allocation bias, although the author does note that “some evidence of harm exists” [8]. In the decades since the most recent TPF trial, neonatology has made progress in nearly every other facet of preterm lung injury. Lung injury from aspiration, however, remains understudied and unabated as a result [18].
There are several limitations that should be noted. In addition to the potential for residual confounding described above, our study population was obtained from a single NICU with unique management strategies, which casts some doubt on the generalizability of our findings. We were also unable to collect detailed patient data that would have been informative, including duration of TPF and additional measures of baseline illness severity. As a result, our findings should be interpreted with caution.
Conclusion
Early TPF is associated with reduced the risk of death or BPD among ELBW infants. Further investigation in the form of a randomized controlled trial is required to confirm a causal relationship between early TPF and improved clinical outcomes.
References
Liu L, Oza S, Hogan D, Perin J, Rudan J, Rudan I, et al. Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet. 2015;385:430–40.
Patel RM, Kandefer S, Walsh MC, Bell EF, Carlo WA, Laptook AR, et al. Causes and timing of death in extremely premature infants from 2000 through 2011. N Engl J Med. 2015;331:340.
Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol. 2013;196:147. e1-8
Farhath S, He Z, Nakhla T, Saslow J, Soundar S, Camacho J, et al. Pepsin, a marker of gastric contents, is increased in tracheal aspirates from preterm infants who develop bronchopulmonary dysplasia. Pediatrics. 2008;121:253–9.
Farhath S, Aghai ZH, Nakhla T, Saslow J, He Z, Soundar S, et al. Pepsin, a reliable marker of gastric aspiration, is frequently detected in tracheal aspirates from premature ventilated neonates: relationship with feeding and methylxanthine therapy. J Ped Gastr Nutr. 2006;43:336–41.
McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition. J Parenter Enter Nutr. 2016;40:156–211.
Alkhawaja S, Martin C, Butler RJ, Gwadry-Sridhar F. Post-pyloric versus gastric tube feeding for preventing pneumonia and improving nutritional outcomes in critically ill adults. Cochrane Data System Rev. 2015;8:CD008875.
Watson J, McGuire W. Transpyloric versus gastric tube feeding for preterm infants. Cochrane Data System Rev. 2013;2:CD003487.
Drew JH, Johnston R, Finocchiaro C, Taylor PS, Goldberg HJ. A comparison of nasojejunal with nasogastric feedings in low-birth-weight infants. Aust Paediatr J. 1979;15:98–100.
Laing IA, Lang MA, Callaghan O, Hume R. Nasogastric compared with nasoduodenal feeding in low birth weight infants. Arch Dis Child. 1986;61:138–41.
Macdonald PD, Skeoch CH, Carse H, Dryburgh F, Alroomi LG, Galea P, et al. Randomised trial of continuous nasogastric, bolus nasogastric, and transpyloric feeding in infants of birth weight under 1400 g. Arch Dis Child. 1992;67:429–31.
Pereira GR, Lemons JA. Controlled study of transpyloric and intermittent gavage feeding in the small preterm infant. Pediatrics. 1981;67:68–72.
Pyati S, Ramamurthy R, Pildes R. Continuous drip nasogastric feedings: a controlled study (Abstract). Pediatr Res. 1976;10:359.
Roy RN, Pollnitz RP, Hamilton JR, Chance GW. Impaired assimilation of nasojejunal feeds in healthy low birthweight infants. J Pediatr. 1977;90:431–4.
Caillie MV, Powell GK. Nasoduodenal versus nasogastric feeding in the very low birth weight infant. Pediatrics. 1975;56:1065–72.
Wells DH, Zachman RD. Nasojejunal feedings in low birthweight infants. J Pediatr. 1975;87:276–9.
Whitfield MF. Poor weight gain of the low birthweight infant fed nasojejunally. Arch Dis Child. 1982;57:597–601.
Wallenstein MB, Stevenson DK. Need for reassessment of early tranpsyloric feeding in preterm infants. JAMA Pediatr. 2018;172:997.
Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344:665.
Krishnan U, Mitchell JD, Messina I, Day AS, Bohane TD. Assay of tracheal pepsin as a marker of reflux aspiration. J Pediatr Gastroenterol Nutr. 2002;35:303–8.
Ufberg JW, Bushra JS, Patel D, Wong E, Karras DJ, Kueppers F. A new pepsin assay to detect pulmonary aspiration of gastric contents among newly intubated patients. Am J Emerg Med. 2004;22:612–4.
Meert KL, Daphtary KM, Metheny NA. Detection of pepsin and glucose in tracheal secretions as indicators of aspiration in mechanically ventilated children. Pediatr Crit Care Med. 2002;3:19–22.
Metheny NA, Chang YH, Ye JS, Edwards SJ, Defer J, Dahms TE, et al. Pepsin as a marker for pulmonary aspiration. Am J Crit Care. 2002;11:150–4.
Omari TI, Barnett CP, Snel A, Goldsworthy W, Haslam R, Davidson G, et al. Mechanisms of gastroesophageal reflux in healthy premature infants. J Pediatr. 1998;133:650–4.
Omari TI, Barnett CP, Benninga MA, Lontis R, Goodchild L, Haslam RR, et al. Mechanisms of gastroesophageal reflux in preterm and term infants with reflux disease. Gut. 2002;51:475–9.
Newell SJ, Booth IW, Morgan ME, Durbin GM, McNeish AS. Gastro-esophageal reflux in preterm infants. Arch Dis Child. 1989;64:780–6.
Ewer AK, Durbin GM, Morgan ME, Booth IW. Gastric emptying and gastroesophageal reflux in preterm infants. Arch Dis Child Fetal Neonatal Ed. 1996;75:F117–F121.
Malcolm WF, Smith PB, Mears S, Goldberg RN, Cotton CM. Transpyloric tube feeding in very low birthweight infants with suspected gastroesophageal reflux: impact on apnea and bradycardia. J Perinatol. 2009;29:372–5.
Misra S, Macwan K, Albert V. Transpyloric feeding in gastroesophageal-reflux-associated apnea in premature infants. Acta Paediatr. 2007;96:1426–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wallenstein, M.B., Brooks, C., Kline, T.A. et al. Early transpyloric vs gastric feeding in preterm infants: a retrospective cohort study. J Perinatol 39, 837–841 (2019). https://doi.org/10.1038/s41372-019-0372-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0372-3
- Springer Nature America, Inc.
This article is cited by
-
Transpyloric feeding in severe BPD: a call for prospective trials
Journal of Perinatology (2024)
-
Transpyloric feeding is associated with adverse in-hospital outcomes in infants with severe bronchopulmonary dysplasia
Journal of Perinatology (2024)
-
Less invasive surfactant administration reduces incidence of severe intraventricular haemorrage in preterms with respiratory distress syndrome: a cohort study
Journal of Perinatology (2020)
-
Early transpyloric feeding: an old wine in a new bottle
Journal of Perinatology (2019)
-
Reply to: ‘Early transyploric feeding: an old wine in a new bottle’
Journal of Perinatology (2019)