Abstract
Background
Birth defects are a major cause of poor health outcomes during both childhood and adulthood. A growing body of evidence demonstrated associations between air pollution exposure during pregnancy and birth defects. To date, there is no study looking at birth defects and exposure to wildfire-related air pollution, which is suggested as a type of air pollution source with high toxicity for reproductive health.
Objective
Our study addresses this gap by examining the association between birth defects and wildfire smoke exposure in Brazil between 2001 and 2018. Based on known differences of impacts of wildfires across different regions of Brazil, we hypothesized differences in risks of birth defects for different regions.
Methods
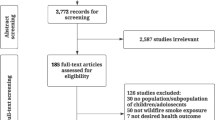
We used a logistic regression model to estimate the odds ratios (ORs) for individual birth defects (12 categories) associated with wildfire exposure during each trimester of pregnancy.
Results
Among the 16,825,497 birth records in our study population, there were a total of 7595 infants born in Brazil between 2001 and 2018 with birth defects in any of the selected categories. After adjusting for several confounders in the primary analysis, we found statistically significant OR for three birth defects, including cleft lip/cleft palate [OR: 1.007 (95% CI: 1.001; 1.013)] during the second trimester of exposure, congenital anomalies of the respiratory system [OR: 1.013 (95% CI: 1.002; 1.023)] in the second trimester of exposure, and congenital anomalies of the nervous system [OR: 1.002 (95% CI: 1.001; 1.003)] during the first trimester of exposure for the regions South, North, and Midwest, respectively.
Significance
Our results suggest that maternal exposure to wildfire smoke during pregnancy may increase the risk of an infant being born with some congenital anomaly. Considering that birth defects are associated with long-term disability, impacting families and the healthcare system (e.g., healthcare costs), our findings should be of great concern to the public health community.
Impact statement
Our study focused on the association between maternal exposure to wildfire smoke in Brazil during pregnancy and the risk of an infant being born with congenital anomalies, which presents serious public health and environmental challenges.

Similar content being viewed by others
References
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. https://doi.org/10.1016/S0140-6736(12)61728-0
Judith RB, Barbara J, Stoll AOL. Improving Birth Outcomes: Meeting the Challenge in the Developing World. Washington, D.C:The national academies press;2003.
Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379:2151–161. https://doi.org/10.1016/S0140-6736(12)60560-1
American Academy of Pediatrics. 2015. Congenital abnormalities. https://www.healthychildren.org/English/health-issues/conditions/developmental-disabilities/Pages/Congenital-Abnormalities.aspx [accessed 2 April 2021].
Centers for Disease Control and Prevention. 2008. What are Birth Defects?. https://www.cdc.gov/ncbddd/birthdefects/facts.html. [accessed 11 Dec 2020].
Nieuwenhuijsen MJ, Dadvand P, Grellier J, Martinez D, Vrijheid M. Environmental risk factors of pregnancy outcomes: a summary of recent meta-analyses of epidemiological studies. Environ Health. 2013;12:1–10. https://doi.org/10.1186/1476-069X-12-6
Dolk H. Epidemiologic approaches to identifying environmental causes of birth defects. Am J Med Genet Part C Semin Med Genet. 2004;125C:4–11. https://doi.org/10.1002/ajmg.c.30000
Clemens T, Turner S, Dibben C. Maternal exposure to ambient air pollution and fetal growth in North-East Scotland: a population-based study using routine ultrasound scans. Environ Int. 2017;107:216–26. https://doi.org/10.1016/j.envint.2017.07.018
Grazuleviciene R, Danileviciute A, Dedele A, Vencloviene J, Andrusaityte S, Uždanaviciute I, et al. Surrounding greenness, proximity to city parks and pregnancy outcomes in Kaunas cohort study. Int J Hyg Environ Health. 2015;218:358–65. https://doi.org/10.1016/j.ijheh.2015.02.004
Zhou Y, Gilboa SM, Herdt ML, Lupo PJ, Flanders WD, Liu Y, et al. Maternal exposure to ozone and PM2.5 and the prevalence of orofacial clefts in four U.S. states. Environ Res. 2017;153:35–40. https://doi.org/10.1016/j.envres.2016.11.007
Gilboa SM, Mendola P, Olshan AF, Langlois PH, Savitz DA, Loomis D, et al. Relation between ambient air quality and selected birth defects, seven county study, Texas, 1997-2000. Am J Epidemiol. 2005;162:238–52. https://doi.org/10.1093/aje/kwi189
Girguis MS, Strickland MJ, Hu X, Liu Y, Bartell SM, Vieira VM. Maternal exposure to traffic-related air pollution and birth defects in Massachusetts. Environ Res. 2016;146:1–9. https://doi.org/10.1016/j.envres.2015.12.010
Yang B, Qu Y, Guo Y, Markevych I, Heinrich J, Bloom S, et al. Maternal exposure to ambient air pollution and congenital heart defects in China. Environ Int. 2021;153:106548 https://doi.org/10.1016/j.envint.2021.106548
Šrám RJ, Binková B, Dejmek J, Bobak M. Ambient air pollution and pregnancy outcomes: a review of the literature. Environ Health Perspect. 2005;113:375–82. https://doi.org/10.1289/ehp.6362
Reid CE, Brauer M, Johnston FH, Jerrett M, Balmes JR, Elliott CT. Critical review of health impacts of wildfire smoke exposure. Environ Health Perspect. 2016;124:1334–43. https://doi.org/10.1289/ehp.1409277
Holstius DM, Reid CE, Jesdale BM, Morello-Frosch R. Birth weight following pregnancy during the 2003 southern California wildfires. Environ Health Perspect. 2012;120:1340–45. https://doi.org/10.1289/ehp.1104515
Abdo M, Ward I, O’dell K, Ford B, Pierce JR, Fischer EV, et al. 2019. Impact of wildfire smoke on adverse pregnancy outcomes in Colorado, 2007–2015. Int J Environ Res Public Health. 16; https://doi.org/10.3390/ijerph16193720.
Yang J, Carmichael SL, Canfield M, Song J, Shaw GM. Socioeconomic status in relation to selected birth defects in a large multicentered US case-control study. Am J Epidemiol. 2008;167:145–54. https://doi.org/10.1093/aje/kwm283
WHO. 2020. Congenital anomalies. https://www.who.int/news-room/fact-sheets/detail/congenital-anomalies [accessed 7 April 2021].
Oliveira-Brancati CIF, Ferrarese VCC, Costa AR, Fett-Conte AC. Birth defects in Brazil: outcomes of a population-based study. Genet Mol Biol. 2020;43:1–7. https://doi.org/10.1590/1678-4685-GMB-2018-0186
Luquetti DV, Koifman RJ. Surveillance of birth defects: Brazil and the US Vigilância epidemiológica em anomalias congênitas: Brasil e Estados Unidos. Cien Saude Colet. 2011;16:777–85.
Reddington CL, Butt EW, Ridley DA, Artaxo P, Morgan WT, Coe H, et al. Air quality and human health improvements from reductions in deforestation-related fire in Brazil. Nat Geosci. 2015;8:768–71. https://doi.org/10.1038/ngeo2535
Inpe. 2020. Wildfires. http://www.dpi.inpe.br/queimadas/ [accessed 12 August 2020].
Ritz B, Yu F, Fruin S, Chapa G, Shaw GM, Harris JA. Ambient air pollution and risk of birth defects in southern california. Am J Epidemiol. 2002;155:17–25. https://doi.org/10.1093/aje/155.1.17
Hansen CA, Barnett AG, Jalaludin BB, Morgan GG. Ambient air pollution and birth defects in Brisbane, Australia. PLoS ONE. 2009;4:6–13. https://doi.org/10.1371/journal.pone.0005408
Vinikoor-Imler LC, Davis JA, Meyer RE, Luben TJ. Early prenatal exposure to air pollution and its associations with birth defects in a state-wide birth cohort from North Carolina. Birth Defects Res Part A - Clin Mol Teratol. 2013;97:696–701. https://doi.org/10.1002/bdra.23159
Wegesser TC, Pinkerton KE, Last JA. California wildfires of 2008: coarse and fine particulate matter toxicity. Environ Health Perspect. 2009;117:893–97. https://doi.org/10.1289/ehp.0800166
Wegesser TC, Franzi LM, Mitloehner FM, Eiguren-Fernandez A, Last JA. Lung antioxidant and cytokine responses to coarse and fine particulate matter from the great California wildfires of 2008. Inhal Toxicol. 2010;22:561–70. https://doi.org/10.3109/08958370903571849
Nordenvall M, Sandstedt B. Placental villitis and intrauterine growth retardation in a Swedish population. APMIS. 1990;98:19–24. https://doi.org/10.1111/j.1699-0463.1990.tb00996.x
Knottnerus JA, Delgado LR, Knipschild PG, Essed GGM, Smits F. Haematologic parameters and pregnancy outcome A prospective cohort study in the third trimester. J Clin Epidemiol. 1990;43:461–66. https://doi.org/10.1016/0895-4356(90)90134-B
Wick P, Malek A, Manser P, Meili D, Maeder-Althaus X, Diener L, et al. Barrier capacity of human placenta for nanosized materials. Environ Health Perspect. 2010;118:432–36. https://doi.org/10.1289/ehp.0901200
Smarr MM, Vadillo-Ortega F, Castillo-Castrejon M, O’Neill MS. The use of ultrasound measurements in environmental epidemiological studies of air pollution and fetal growth. Curr Opin Pediatr. 2013;25:240–6.
Teng C, Wang Z, Yan B. Fine particle-induced birth defects: impacts of size, payload, and beyond. Birth Defects Res Part C Embryo Today Rev. 2016;108:196–206. https://doi.org/10.1002/bdrc.21136
Avissar-Whiting M, Veiga KR, Uhl KM, Maccani MA, Gagne LA, Moen EL, et al. Bisphenol A exposure leads to specific microRNA alterations in placental cells. Reprod Toxicol. 2010;29:401–06. https://doi.org/10.1016/j.reprotox.2010.04.004
Kenner C. Fetal development: environmental influences and critical periods. In: Comprehensive Neonatal Nursing Care. New York:Springer Publishing Company; 2019. p. 1–2019.
CDC. 2021. Fetal development chart. https://www.cdc.gov/ncbddd/fasd/documents/fasdbrochure_final.pdf.
Lapola DM, Martinelli LA, Peres CA, Ometto JPHB, Ferreira ME, Nobre CA, et al. Pervasive transition of the Brazilian land-use system. Nat Clim Chang. 2014;4:27–35. https://doi.org/10.1038/nclimate2056
Howards PP, Johnson CY, Honein MA, Flanders WD. Adjusting for bias due to incomplete case ascertainment in case-control studies of birth defects. Am J Epidemiol. 2015;181:595–607. https://doi.org/10.1093/aje/kwu323
Leung M, Kioumourtzoglou MA, Raz R, Weisskopf MG. Bias due to selection on live births in studies of environmental exposures during pregnancy: a simulation study. Environ Health Perspect. 2021;129:1–8. https://doi.org/10.1289/EHP7961
Funding
This work was supported by the Brazilian Agencies National Council for Scientific and Technological Development (CNPq) and by the Ministry of Science, Technology and Innovation (MCTI).
Author information
Authors and Affiliations
Contributions
WJR conceived and the work, acquired data, played an important role in interpreting the results, and drafted the first version of the paper. EK worked on the exposure data analysis. SP, PK, and JS played an important role in interpreting the results and suggesting edits in the methodological design.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Requia, W.J., Kill, E., Papatheodorou, S. et al. Prenatal exposure to wildfire-related air pollution and birth defects in Brazil. J Expo Sci Environ Epidemiol 32, 596–603 (2022). https://doi.org/10.1038/s41370-021-00380-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-021-00380-y
- Springer Nature America, Inc.
Keywords
This article is cited by
-
Science communication on the public health risks of air pollution: a computational scoping review from 1958 to 2022
Archives of Public Health (2023)
-
Health Impacts of Wildfire Smoke on Children and Adolescents: A Systematic Review and Meta-analysis
Current Environmental Health Reports (2023)
-
Obstetric care for environmental migrants
Irish Journal of Medical Science (1971 -) (2023)
-
Natural Disaster Epidemiology and Reproductive Health
Current Epidemiology Reports (2023)