Abstract
Background and objective
Childhood obesity is associated with later development of significant renal morbidity. We evaluated the impact of the degree of insulin sensitivity on estimated glomerular filtration rate (eGFR) and determined the factors associated with eGFR in obese children. We further tested the relation of eGFR to clinical outcomes such as blood pressure and microalbuminuria.
Materials and methods
We evaluated the relation of whole body insulin sensitivity and estimated glomerular filtration rate (eGFR) across the spectrum of obesity in children and adolescents. eGFR was calculated using the iCARE formula, which has been validated in obese children with varying glucose tolerance.
Results
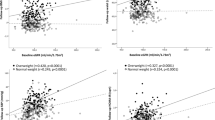
1080 children and adolescents with overweight and obesity (701 females and 379 males) participated. Insulin sensitivity was a strongly negatively associated with (B = −2.72, p < 0.001) eGFR), even after adjustment for potential confounders. Male sex emerged to be significantly associated with eGFR with boys having greater values than girls (B = 18.82, p < 0.001). Age was a positively associated (B = 2.86, p < 0.001) with eGFR. Whole body and hepatic insulin sensitivity decreased across eGFR quartiles. Adjusted eGFR was tightly positively associated with systolic blood pressure (B = 0.09, p = 0.003) and negatively associated with the presence of microalbuminuria (B = −2.18, p = 0.04).
Conclusions
eGFR tends to increase with greater degrees of insulin resistance in children and adolescents representing hyperfiltration and is associated with cardiovascular risk factors. Longitudinal studies are needed to determine the natural history of childhood insulin resistance related hyperfiltration in regards to future kidney disease.



Similar content being viewed by others
References
Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350:2362–74.
Zabarsky G, Beek C, Hagman E, Pierpont B, Caprio S, Weiss R. Impact of Severe Obesity on Cardiovascular Risk Factors in Youth. J Pediatr. 2018;192:105–14.
Chagnac A, Weinstein T, Korzets A, Ramadan E, Hirsch J, Gafter U. Glomerular hemodynamics in severe obesity. Am J Physiol Renal Physiol. 2000;278:F817–22.
Mathew AV, Okada S, Sharma K. Obesity related kidney disease. Curr Diabetes Rev. 2011;7:41–9.
Bjornstad P, Nehus E, El Ghormli L, Bacha F, Libman IM, McKay S, et al. Insulin Sensitivity and Diabetic Kidney Disease in Children and Adolescents With Type 2 Diabetes: An Observational Analysis of Data From the TODAY Clinical Trial. Am J Kidney Dis. 2018;71:65–74.
Kanbay M, Ertuglu LA, Afsar B, Ozdogan E, Kucuksumer ZS, Ortiz A, et al. Renal hyperfiltration defined by high estimated glomerular filtration rate: A risk factor for cardiovascular disease and mortality. Diabetes Obes Metab. 2019;21:2368–83.
Reaven GM. The kidney: an unwilling accomplice in syndrome X. Am J Kidney Dis. 1997;30:928–31.
Mascali A, Franzese O, Nisticò S, Campia U, Lauro D, Cardillo C, et al. Obesity and kidney disease: beyond the hyperfiltration. Int J Immunopathol Pharmacol. 2016;29:354–63.
Levey AS, Inker LA, Coresh J. GFR estimation: from physiology to public health. Am J Kidney Dis. 2014;63:820–34.
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, et al. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009;20:629–37.
Dart AB, McGavock J, Sharma A, Chateau D, Schwartz GJ, Blydt-Hansen T. Estimating glomerular filtration rate in youth with obesity and type 2 diabetes: the iCARE study equation. Pediatr Nephrol. 2019;34:1565–74.
Weiss R, Dziura JD, Burgert TS, Taksali SE, Tamborlane WV, Caprio S. Ethnic differences in beta cell adaptation to insulin resistance in obese children and adolescents. Diabetologia. 2006;49:571–9.
Weiss R, Magge SN, Santoro N, Giannini C, Boston R, Holder T, et al. Glucose effectiveness in obese children: relation to degree of obesity and dysglycemia. Diabetes Care. 2015;38:689–95.
Giannini C, Santoro N, Caprio S, Kim G, Lartaud D, Shaw M, et al. The triglyceride-to-HDL cholesterol ratio: association with insulin resistance in obese youths of different ethnic backgrounds. Diabetes Care. 2011;34:1869–74.
Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22:1462–70.
Abdul-Ghani MA, Matsuda M, Balas B, DeFronzo RA. Muscle and liver insulin resistance indexes derived from the oral glucose tolerance test. Diabetes Care. 2007;30:89–94.
Herrington WG, Smith M, Bankhead C, Matsushita K, Stevens S, Holt T, et al. Body-mass index and risk of advanced chronic kidney disease: Prospective analyses from a primary care cohort of 1.4 million adults in England. PLoS ONE. 2017;12:e0173515.
Vivante A, Golan E, Tzur D, Leiba A, Tirosh A, Skorecki K, et al. Body mass index in 1.2 million adolescents and risk for end-stage renal disease. Arch Intern Med. 2012;172:1644–50.
D’Agati VD, Chagnac A, de Vries AP, Levi M, Porrini E, Herman-Edelstein M, et al. Obesity-related glomerulopathy: clinical and pathologic characteristics and pathogenesis. Nat Rev Nephrol. 2016;12:453–71.
Praga M. Synergy of low nephron number and obesity: a new focus on hyperfiltration nephropathy. Nephrol Dial Transplant. 2005;20:2594–7.
Brenner BM, Hostetter TH, Olson JL, Rennke HG, Venkatachalam MA. The role of glomerular hyperfiltration in the initiation and progression of diabetic nephropathy. Acta Endocrinol Suppl (Copenh). 1981;242:7–10.
Thomas MC, Cherney DZI. The actions of SGLT2 inhibitors on metabolism, renal function and blood pressure. Diabetologia. 2018;61:2098–107.
Hsu CY, Iribarren C, McCulloch CE, Darbinian J, Go AS. Risk factors for end-stage renal disease: 25-year follow-up. Arch Intern Med. 2009;169:342–50.
Hsu CY, McCulloch CE, Iribarren C, Darbinian J, Go AS. Body mass index and risk for end-stage renal disease. Ann Intern Med. 2006;144:21–8.
Önerli Salman D, Şıklar Z, Çullas İlarslan EN, Özçakar ZB, Kocaay P, Berberoğlu M. Evaluation of Renal Function in Obese Children and Adolescents Using Serum Cystatin C Levels, Estimated Glomerular Filtration Rate Formulae and Proteinuria: Which is most Useful? J Clin Res Pediatr Endocrinol. 2019;11:46–54.
Correia-Costa L, Schaefer F, Afonso AC, Bustorff M, Guimarães JT, Guerra A, et al. Normalization of glomerular filtration rate in obese children. Pediatr Nephrol. 2016;31:1321–8.
Ricotti R, Genoni G, Giglione E, Monzani A, Nugnes M, Zanetta S, et al. High-normal estimated glomerular filtration rate and hyperuricemia positively correlate with metabolic impairment in pediatric obese patients. PLoS ONE. 2018;13:e0193755.
Xargay-Torrent S, Puerto-Carranza E, Marcelo I, Mas-Parés B, Gómez-Vilarrubla A, Martínez-Calcerrada JM, et al. Estimated glomerular filtration rate and cardiometabolic risk factors in a longitudinal cohort of children. Sci Rep. 2021;11:11702.
de Vries AP, Ruggenenti P, Ruan XZ, Praga M, Cruzado JM, Bajema IM, et al. Fatty kidney: emerging role of ectopic lipid in obesity-related renal disease. Lancet Diabetes Endocrinol. 2014;2:417–26.
Kurella M, Lo JC, Chertow GM. Metabolic syndrome and the risk for chronic kidney disease among nondiabetic adults. J Am Soc Nephrol. 2005;16:2134–40.
Sarafidis PA, Ruilope LM. Insulin resistance, hyperinsulinemia, and renal injury: mechanisms and implications. Am J Nephrol. 2006;26:232–44.
Oterdoom LH, de Vries AP, Gansevoort RT, de Jong PE, Gans RO, Bakker SJ. Fasting insulin modifies the relation between age and renal function. Nephrol Dial Transplant. 2007;22:1587–92.
Lovshin JA, Škrtić M, Bjornstad P, Moineddin R, Daneman D, Dunger D, et al. Hyperfiltration, urinary albumin excretion, and ambulatory blood pressure in adolescents with Type 1 diabetes mellitus. Am J Physiol Renal Physiol. 2018;314:F667–F74.
DeFronzo RA, Ferrannini E, Groop L, Henry RR, Herman WH, Holst JJ, et al. Type 2 diabetes mellitus. Nat Rev Dis Primers. 2015;1:15019. https://doi.org/10.1038/nrdp.2015.19.
Moran A, Jacobs DR, Steinberger J, Steffen LM, Pankow JS, Hong CP, et al. Changes in insulin resistance and cardiovascular risk during adolescence: establishment of differential risk in males and females. Circulation. 2008;117:2361–8.
Burgert TS, Dziura J, Yeckel C, Taksali SE, Weiss R, Tamborlane W, et al. Microalbuminuria in pediatric obesity: prevalence and relation to other cardiovascular risk factors. Int J Obes (Lond). 2006;30:273–80.
de Paula RB, da Silva AA, Hall JE. Aldosterone antagonism attenuates obesity-induced hypertension and glomerular hyperfiltration. Hypertension. 2004;43:41–7.
Weiss R. Fat distribution and storage: how much, where, and how? Eur J Endocrinol. 2007;157:S39–45.
Foster MC, Hwang SJ, Porter SA, Massaro JM, Hoffmann U, Fox CS. Fatty kidney, hypertension, and chronic kidney disease: the Framingham Heart Study. Hypertension. 2011;58:784–90.
Armstrong MJ, Adams LA, Canbay A, Syn WK. Extrahepatic complications of nonalcoholic fatty liver disease. Hepatology. 2014;59:1174–97.
Sasaki M, Sasako T, Kubota N, Sakurai Y, Takamoto I, Kubota T, et al. Dual Regulation of Gluconeogenesis by Insulin and Glucose in the Proximal Tubules of the Kidney. Diabetes. 2017;66:2339–50.
van Bommel EJM, Ruiter D, Muskiet MHA, van Baar MJB, Kramer MHH, Nieuwdorp M, et al. Insulin Sensitivity and Renal Hemodynamic Function in Metformin-Treated Adults With Type 2 Diabetes and Preserved Renal Function. Diabetes Care. 2020;43:228–34.
Acknowledgements
This paper is in loving memory of Bridget Pierpont, the research coordinator of the Yale Pathophysiology of Type 2 Diabetes in Youth Study cohort, who passed away unexpectedly during the preparation of this paper. We wish to thank the participants and their families for their willingness and cooperation. This study was supported by the National Institutes of Health, National Institute of Child Health and Human Development (grants R01-HD-40787, R01DK111038, R01-HD-28016, and K24-HD-01464 to S.C.), the National Center for Research Resources (Clinical and Translational Science Award [grant UL1-RR-0249139] to SC), the American Diabetes Association (Distinguished Clinical Scientist Award to SC), the National Institute of Diabetes and Digestive and Kidney Diseases (grant R01-DK-111038 to SC; grant R01-DK-114504-01A1)
Author information
Authors and Affiliations
Contributions
DM and RN performed the analysis and wrote the paper, AG took part in the clinical care and added to the discussion; SC and RW designed the study, took part in the clinical care and the analysis and added to the discussion. All authors read, edited and approved the paper. RW is the guarantor of this analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Magen, D., Halloun, R., Galderisi, A. et al. Relation of glomerular filtration to insulin resistance and related risk factors in obese children. Int J Obes 46, 374–380 (2022). https://doi.org/10.1038/s41366-021-01001-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-01001-2
- Springer Nature Limited