Abstract
Background/Objectives
The occurrence of chronic inflammation in visceral adipose tissue (VAT) in obese subjects precipitates the development of insulin resistance and type 2 diabetes (T2D). Anthocyanins and their main metabolite protocatechuic acid (PCA) have been demonstrated to stimulate insulin signaling in human adipocytes. The aim of this study was to investigate whether PCA is able to modulate insulin responsiveness and inflammation in VAT from obese (OB) and normal weight (NW) subjects.
Subjects/Methods
VATs obtained from NW and OB subjects were incubated or not (control) with 100 μM PCA for 24 h. After incubation, tissues untreated and treated with PCA were acutely stimulated with insulin (20 nM, 20 min). PTP1B, p65 NF-κB, phospho-p65 NF-κB, IRS-1, IRβ, Akt, GLUT4 as well as basal and insulin-stimulated Tyr-IRS-1 and Ser-Akt phosphorylations were assessed by Western blotting in NW- and OB-VAT. Samples were assessed for PTP1B activity and adipocytokine secretion.
Results
PCA restored insulin-induced phosphorylation in OB-VAT by increasing phospho-Tyr-IRS-1 and phospho-Ser-Akt after insulin stimulation as observed in NW-VAT (p < 0.05). PTP1B activity was lower in OB-VAT treated with PCA with respect to untreated (p < 0.05). Compared to non-treated tissues, PCA reduced phospho-p65 NF-κB and IL-6 in OB-VAT, and IL-1β in NW-VAT (p < 0.05); and increased adiponectin secretion in NW-VAT (p < 0.05).
Conclusion
PCA restores the insulin responsiveness of OB-VAT by increasing IRS-1 and Akt phosphorylation which could be related with the lower PTP1B activity found in PCA-treated OB-VAT. Furthermore, PCA diminishes inflammation in VAT. These results support the beneficial role of an anthocyanin-rich diet against inflammation and insulin resistance in obesity.
Similar content being viewed by others
Introduction
It is well recognized that obesity is highly associated with the onset of pathologies such as insulin resistance, type 2 diabetes mellitus (DM2), cardiovascular disease, and cancer [1]. An important underlying cause of obesity-induced insulin resistance is chronic low-grade systemic inflammation which is originated predominantly in the visceral fraction of fat depot [2]. Visceral adipose tissue (VAT) is a heterogeneous tissue composed of pre-adipocytes, adipocytes, and immune cells [3] with the ability to produce hormones and cytokines with pro-inflammatory/pro-hyperglycemic (leptin, resistins, TNF-α, IL-1β, and IL-6) and anti-inflammatory/anti-hyperglycemic (omentin, adiponectin) actions [4]. At the cellular level, inflammatory burst may involve the phosphorylation of the transcription factor NF-κB [5, 6] which causes an increase in the gene expression of TNFα and IL-6, both implicated in the development of obesity-induced insulin resistance [4].
On the other hand, insulin resistance is defined as the impairment of the insulin signaling, namely insulin receptor (IRβ)/IRS-1/PI3K/Akt pathway, in insulin-responsive cells such as adipocytes [7]. Among insulin signaling regulators, protein phosphatases play an important role [8]. It is well recognized that protein tyrosine phosphatase 1B (PTP1B) attenuates insulin signaling transduction by removing Tyr phosphates from the activated insulin receptor and IRS-1 [9, 10]. Interestingly, mice lacking PTP1B showed increased insulin sensitivity, suggesting that insulin signaling can be enhanced by PTP1B inhibition [11].
The implementation of multiple pharmacological and non-pharmacological interventions with the aim of improving low-grade chronic inflammation, glycemic control, as well as DM2 complications is encouraged. In this regard, the consumption of food containing bioactive components has been considered as a new and promising approach in the prevention and management of such conditions [12,13,14,15]. An increasing number of epidemiological evidence has shown that diets rich in food with high content of phytochemicals, particularly polyphenols, may reduce complications linked with obesity [16, 17], supporting their use as nutraceuticals and supplementary treatments for insulin resistance, inflammation, and DM2 [12, 18].
Among polyphenols, anthocyanins (ACNs) are flavonoids of great nutritional interest because of their high daily intake [19]. At physiological pH (such as in the bloodstream), ACNs easily convert to protocatechuic acid (PCA), a main metabolite of ACNs, which is also abundantly formed and absorbed in the large intestine after microbial metabolization [20]. A strong body of evidence supports the biological activity in vitro of PCA as an antioxidant and insulin-mimetic molecule in different biological models [21,22,23]; however, the ability of PCA to modulate insulin responsiveness and inflammation in pathological conditions such as obesity has not been demonstrated yet. Therefore, the aim of this study was to evaluate the effect of PCA on insulin signaling, PTP1B activity, and inflammation in VAT from obese (OB) subjects compared to VAT from normal weight (NW) individuals.
Materials and methods
Materials
Dulbecco’s modified Eagle’s medium (DMEM) was purchased from Flow Laboratories (Irvine, UK); glutamine and antibiotics were from Hyclone (Cramlington, UK). Insulin was from Sigma (St Louis, MO, USA). PCA was purchased from Sigma-Aldrich (St. Louis, MO, USA). Electrophoresis reagents were from Bio-Rad (Hercules, CA, USA). Anti-IRS-1 (catalog number sc-7200), anti-GLUT4 (catalog number sc-53566), anti-p65 NF-κB (catalog number sc-8008), IL-1β (catalog number sc-52865) and horseradish peroxidase-conjugate anti-goat (catalog number sc-7020), and anti-rabbit (catalog number sc-2357) antibodies were from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Horseradish peroxidase-conjugate anti-mouse (catalog number 172–1011) antibody was from Bio-Rad (Kidlington, UK). Anti-Akt (catalog number 2920S), anti-phospho Akt Ser 473 (catalog number 4060S), anti-IRβ (catalog number 81764), anti-phospho p65 NF-κB Ser536 (catalog number 3033S) antibodies were from Cell Signaling Technology (Beverly, MA, USA). Antibody against PTP1B (catalog number Ab2009) was purchased from Abcam (Cambridge, United Kingdom). Anti-phospho Tyr 608 IRS-1 (catalog number 09-432) and anti-β-actin (catalog number MABT826) antibodies were from Merck-millipore (Temecula, CA, USA). ELISA Kit for IL-6 was from Biolegend (San Diego, CA, USA) and Tyrosine Phosphatase Assay System from Promega (Madison, WI, USA).
Human VAT
VAT was collected from anesthetized female individuals. NW subjects (n = 6, age 45–75, BMI ≤ 25.0) underwent abdominal surgery or laparoscopy for benign conditions (i.e., gallbladder disease without icterus, umbilical hernia, uterine fibromatosis) while OB individuals (n = 8, age 30–55 years, BMI > 30) underwent abdominal bariatric surgery or surgery for pancreatic, duodenum, and bile duct diseases. The sample size was determined on the basis of preliminary data collected from a similar population, to detect with a negative binomial test significant differences between the two groups with a power of 80%, and a 5% significance level.
Exclusion criteria were: steroidal and non-steroidal anti-inflammatory therapies, hormonal substitutive or contraceptive therapy, hormonal therapy for any thyroid dysfunctions, drugs or alcohol abuse, diabetes mellitus, chronic renal failure, cancer, pregnancy, mental disability. The sampling was performed at the same site with the patient in anti-Trendelenburg position (25° head up) with the surgeon standing between the legs. The biopsies were obtained by monopolar electrocautery or harmonic scalpel. The standard sampling was considered 2 × 2 cm avoiding bleeding and other possible contamination. The study protocol has been approved by the Ethics Committee of the Istituto Superiore di Sanità, the Italian National Institute of Health. All the subjects were volunteers and gave their informed consent according to the Italian law on this matter (Legislative Decree of the Italian Ministry of Health, January 25, 2001, published in the Official Gazette of April 3, 2001). Rough blood vessels and connective tissue were removed from the VAT samples prior to utilization for experimental treatments. The experiments were carried out employing 200 mg of VAT cut in pieces of 50 mg, each incubated in DMEM as described below. The experiments with ELISA kits were performed in duplicate.
Treatment of VAT
To define the experimental conditions, we carried out preliminary trials, incubating 200 mg of VAT cut in pieces of 50 mg each with different concentration of the polyphenol (1–150 μmol/L) for different times in order to choose the best concentration. Such concentrations of PCA are in the same order of magnitude to those found in human plasma after the intake of a cranberry juice [24, 25]. In order to reproduce the situation that can occur in vivo through the daily consumption of polyphenol-rich food, we decided to keep VAT exposure to PCA for 24 h. The dose–response curve of the effect of PCA on glucose uptake showed that 100 µmol/L was the lowest concentration that induced a significant increase (p < 0.05) in glucose uptake compared to those tissues untreated with PCA (data not shown). Two-hundred milligrams of VATs cut in four equal pieces from OB and NW subjects incubated with PCA at 100 μmol/L for 24 h were designated as PCA-treated tissues. Untreated VATs were considered as control. Additionally, tissues were acutely insulin-stimulated. As first approach, a dose-response curve evaluating insulin-stimulated Akt phosphorylation was carried out in NW-VAT in order to determine the lowest insulin concentration that significantly increased Akt phosphorylation compared to unstimulated samples (p < 0.05; data not shown). A concentration of insulin of 20 nM for a 20-min stimulation was chosen. After corresponding treatments, an aliquot of medium from 200 mg of VAT samples was frozen for future adipocytokine determination and tissues were washed in phosphate buffer saline solution and lysed in lysis buffer in order to obtain whole-cell extracts for further analyses as previously described [26].
Western blotting
Immunoblotting analyses were carried out from whole-cell extracts prepared from 200 mg of tissues using specific antibodies for IRβ, phospho-IRS-1, IRS-1, phospho-Ser-Akt, Akt, phospho-p65 NF-κB, p65 NF-κB, PTP1B, IL-1β, adiponectin. Whole-cell lysates from VAT were boiled with Laemmli sample buffer for 5 min, resolved by 12% SDS-PAGE, and transferred onto nitrocellulose membranes. Blots were treated with appropriate secondary antibodies conjugated with horseradish peroxidase followed by ECL detection (Amersham Bio-Sciences, Buckinghamshire, UK). Equal loading of proteins was verified by immunoblotting with a mouse anti-β-actin antibody. Densitometric analysis was performed using a molecular imager FX (Bio-Rad, Hercules, CA, USA).
Adipocytokine measurements
Adiponectin and IL-1β determination from culture media was assessed by Western blot; data were normalized for protein content. Evaluation of protein secretion from adipose tissue explants by Western blotting has been previously described as a suitable approach to measure the release of protein factors by adipose tissue [27]. IL-6 secretion was evaluated using a commercial ELISA kit from Biolegend (San Diego, CA, USA) according to manufacturer’s instructions. Data were normalized for mg of tissue.
Insulin-resistant model in VAT from lean individuals
NW-VATs were used to establish an insulin-resistant model induced by exposing the cells to high glucose concentration. To achieve this aim, we carried out preliminary trials by incubating 200 mg of NW-VAT samples with different concentration of glucose (20–50 mM) for 24 h; 30 mM glucose was chosen as the lowest glucose concentration that significantly (p < 0.05) impaired insulin-stimulated Akt phosphorylation compared to untreated tissues exposed to 5 mM glucose (data not shown). Mannitol was used as osmotic control. Then, to evaluate the effect of PCA on this model, four experimental conditions were evaluated in equal amount of NW-VAT as described above: (i) untreated, (ii) 100 µM PCA for 24 h, (iii) 30 mM glucose for 24 h, (iv) 100 µM PCA (1 h before and along subsequent 24 h glucose treatment) + 30 mM glucose (24 h). Additionally, an acute insulin-stimulation was performed on each condition as stated above. Unstimulated and insulin-stimulated phosphorylation of Tyr-IRS-1 and Ser-Akt was assessed by Western blotting as previously described.
PTP1B enzymatic activity
PTP1B specific activity was determined in whole cell lysates from 200 mg of tissue using a non-radioactive Tyrosine Phosphatase Assay System Kit from Promega (Madison, WI, USA) according to the manufacturer’s instructions.
Statistical analysis
The results are expressed as means ± SEM. Experiments were performed at least in four different individuals randomly chosen from the 14 recruited subjects. Comparisons between two groups were carried out by Student’s t test. Differences were considered significant when p < 0.05.
Results
OB-VAT showed different insulin signaling activation, inflammatory molecule expression, and PTP1B activity compared to NW subjects
First, we evaluated whether protein expression of molecules involved directly or indirectly with insulin pathway was deregulated in the visceral fraction of adipose tissue of OB individuals compared to lean subjects. To this purpose, protein expression of insulin signaling molecules, were studied. The results showed 52% and 43% reduction in IRS-1 and GLUT4 protein levels, respectively, in VAT samples from OB individuals compared to NW tissues (see Table 1). Interestingly, the protein expression of the phosphatase PTP1B, involved in the regulation of insulin signaling, was three times higher in VAT tissues from OB subjects compared to NW. Neither Akt and IRβ content nor PTP1B activity showed significant differences between VAT groups (Table 1 and Supplementary Information, respectively). Regarding inflammatory signals in VAT, we evaluated the activation of the inflammatory NF-κB transcription factor and adipocytokine secretion. Our data provide evidence of a higher p65 NF-κB phosphorylation level in OB-VAT than NW-VAT, despite similar protein expression of p65 NF-κB (see Table 1). Furthermore, adiponectin secretion into the culture media was significantly lower (43% reduction) in OB-VAT compared to NW-VAT (Table 1), while IL-6 showed a significant higher secretion (45%), from OB-VAT compared to NW-VAT (Fig. 1).
Effect of PCA on NW - and OB-VAT
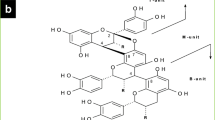
Taking into account the evidence showing that PCA can be taken up by adipose cells and it is able to upregulate insulin signaling [23], next, we assessed whether PCA had similar effects in VAT. To that aim, VAT samples from NW and OB individuals were treated or not with PCA as described in Materials and Methods. Protein expression of insulin pathway molecules (IRβ, IRS-1, Akt, GLUT4) assessed in the current study was not affected by the treatment with PCA either in NW- or OB-VAT (Table 2). However, as phosphorylation of specific amino acid residues represents a common mechanism for activating intracellular signaling proteins, we assessed the insulin-stimulated phosphorylation of two main components of insulin pathway, namely IRS-1 and Akt by PCA in VAT. Interestingly, when OB-VATs were stimulated by insulin, no increases in the phosphorylation of IRS-1 and Akt were observed showing the insulin resistance of OB-VATs. Nonetheless, when OB-VATs were pre-treated with PCA, the response to insulin increased significantly as showed by the higher levels of phospho-IRS-1 and phospho-Akt after insulin stimulation (Fig. 2b). Worthy of note, tissues from NW subjects did not show the same behavior, demonstrating a specific effect of PCA on OB tissues (Fig. 2a).
Effect of PCA on IRS-1 and Akt activation in NW- and OB-VATs. Insulin-stimulated phospho-IRS-1 and phospho-Akt in VAT untreated and treated with PCA from a NW and b OB individuals. Phosphorylations were evaluated by Western blot as described in Materials and Methods. Results are depicted as fold increase versus unstimulated VATs untreated with PCA. The data are means of six independent experiments ± SEM; *p < 0.05 versus corresponding unstimulated condition
On the basis of these findings showing impaired response to insulin in OB-VAT and the ability of PCA in increasing insulin responsiveness, we decided to test whether NW-VAT exposed to high glucose concentration may become insulin-resistant, and whether a pre-treatment with PCA may overcome this situation. In order to verify this hypothesis, firstly we established an insulin-resistant model in VAT from lean individuals as described in the Methods section. Secondly, we evaluated whether the treatment with PCA before (1 h) and along glucose exposure (24 h) counteracted high glucose effects on insulin-stimulated phosphorylation of Tyr-IRS-1 and Ser-Akt. As Fig. 3 shows, when VAT samples were incubated with 30 mM glucose and insulin-stimulated, both phospho-IRS-1 and phospho-Akt were lower with respect to tissues only stimulated with insulin. Hence, from these results we corroborated that our experimental condition by using high glucose treatment induces insulin-resistance in VAT from NW subjects. Additionally, PCA-treated NW-VAT increased insulin-stimulated phospho-IRS-1 and phospho-Akt to a similar extent than tissues stimulated with the hormone alone. Interestingly, the pre-treatment with PCA prior and along high glucose exposition restored the ability of VAT to increase insulin-stimulated phosphorylation of IRS-1 and Akt, showing a similar behavior than tissues treated with insulin alone. No differences in total protein content were found for IRβ, IRS-1, Akt, and GLUT4 between the four experimental conditions (data not shown).
Effect of high glucose on IRS-1 and Akt activation in NW-VATs. Insulin-stimulated a phospho-IRS-1 and b phospho-Akt in untreated, PCA, glucose and PCA + glucose VATs. Phosphorylations were evaluated by Western blot as described in Materials and Methods. Results are depicted as fold increase versus unstimulated VATs under the untreated condition. The data are means of four independent experiments ± SEM; *p < 0.05 versus unstimulated corresponding condition; #p < 0.05 versus insulin-stimulated VATs under the untreated condition
Effect of PCA on PTP1B
The above results showing a role for PCA in modulating phosphorylation in OB-VAT, together with data from literature exhibiting an inhibitory action exerted by plant polyphenols on protein phosphatases such as PTP1B [28, 29], led us to hypothesize that PCA might modulate IRS-1 and Akt phosphorylation by affecting PTP1B activity. In order to verify this hypothesis, we firstly investigated the protein level of PTP1B in adipose tissues untreated and treated with PCA showing no differences in its expression in both NW- and OB-VAT (Table 2). Successively, we investigated whether PCA might modulate PTP1B activity. To that aim, we assessed PTP1B activity in NW and OB samples incubated with PCA, reporting a reduction in PTP1B activity in OB-VATs treated with PCA compared to the untreated ones (Table 2).
Effect of PCA on inflammation
Because of the central role played by inflammation in modulating insulin sensitivity, we evaluated whether PCA affected the NF-κB pathway as well as the secretion of adipocytokines in VAT. To this purpose, we incubated VAT samples from NW and OB with PCA and assessed: (i) p65 NF-κB total protein content and its phosphorylation on Ser536 by Western blot and (ii) adiponectin, IL-1β and IL-6 secretion by Western blotting or ELISA as described in Materials and Methods section. PCA treatment reduced p65 NF-κB protein expression and its phosphorylation only in OB-VAT samples (Table 2).
Regarding the secretory activity of VAT, PCA induced the upregulation of adiponectin secretion and diminished IL-1β in NW-VAT samples (Fig. 4a), while IL-6 secretion was significantly reduced by PCA treatment in VAT from OB individuals (Fig. 4b).
Adipocytokine secretion of NW- and OB-VATs untreated and treated with PCA. a Adiponectin and IL-1β secretion to the culture media were evaluated by Western blot as described in Materials and Methods. Results are shown as fold increase versus untreated condition. The data are means of four independent experiments ± SEM; b IL-6 secretion was assessed by ELISA and data were corrected for mg of tissue as depicted in Materials and Methods section. The data are means of eight independent experiments ± SEM performed in duplicate; *p < 0.05 versus VATs untreated with PCA
Discussion
The present work intends to complement previous reports from our group which have demonstrated the biological activity of PCA, the major metabolite of dietary polyphenols, in stimulating insulin signal in murine and human adipocytes [22, 23]. Specifically, this study provides new evidence about the beneficial role of this phenolic acid on insulin pathway activation as well as on inflammation in VAT from OB individuals. Moreover, it suggests a possible role for the phosphatase PTP1B on insulin responsiveness of such tissues. Finally, we provide evidence of the counteracting effect of PCA against insulin resistance in VAT exposed to high glucose concentration.
To our knowledge, this is the first study demonstrating the ability of PCA to restore the impaired capacity of OB-VAT to raise phospho-IRS-1and phospho-Akt after an acute insulin stimulation. The capability of PCA to overcome this signaling deregulation in OB-VAT may have potential therapeutic implications for obesity-associated insulin resistance.
In adipocytes, insulin resistance is attributed to post-insulin receptor defects making IRS-1 and Akt appropriate candidates to study insulin pathway alterations [30]; thus, in the current investigation, increases in insulin-induced IRS-1 and Akt phosphorylations were interpreted as the ability of the tissue to respond to the hormone in relation to unstimulated VAT. According to our previous results, PCA shows an insulin-like activity in human visceral adipocytes. The absence of an insulin-mimetic action or an additive effect observed in NW-VAT incubated with PCA might be explained, at least in part, by the nature of biological model employed in the present research. As it was stated above, VAT is not a homogeneous tissue, besides adipocytes, it contains other cells, including preadipocytes, endothelial cells, fibroblasts, and various immune cells [31]. Thus, paracrine signals produced by the heterogeneous cell population of VAT might influence the response showed by adipocyte itself. On the other hand, it is believed that organ culture offers substantial benefits over adipocyte culture [32]. For instance, it is an accurate model for assessing adipocyte function within adipose tissue as adipocyte-specific gene expression is maintained [33,34,35], and most importantly, the model of adipose explant culture appears to correlate well with in vivo effects [31].
Potential efficacy of polyphenols in improving metabolic and/or cardiovascular morbidity and mortality, as well as carbohydrate metabolism and glucose homeostasis, has been investigated in vitro, animal models, and some clinical trials [36]. Among polyphenols, ACNs have been considered one of the most interesting class of bioactive food components that are rapidly metabolized ultimately leading to the formation of phenolic acids and aldehydes [37]. Among them, PCA deserves great nutritional interest as main human ACN metabolite that might reach tissues in such an amount to exert biological healthy effects [38, 39].
Literature has reported that glucose concentrations close to 50 mM have been found in the blood of patients with uncontrolled diabetes. Notwithstanding, glucose levels in patients are not likely to stay as high as 30 mM for 24 h, and tissue damage occurs over many years of incalculable hyperglycemic episodes [40, 41]. Therefore, the glucose concentration used in this study seems reasonable for our research scopes. On the other hand, it is well known that chronic hyperglycemia frequently occurs in OB subjects and is a characteristic of the diabetic condition. Moreover, sustained hyperglycemia participates in insulin resistance of insulin-sensitive tissues, which include adipose tissue, raising the hypothesis of a “glucose toxicity” [42]. To our knowledge, this is the first work establishing a high glucose insulin-resistant human VAT model. Furthermore, we demonstrated the ability of PCA to counteract in vitro induced-insulin resistance. It is important to note that the results depicted here do not allow us to define whether insulin responsiveness improvement by PCA occurs through amelioration of primary or secondary insulin resistance induced by glucose-mediated oxidative and/or endoplasmic reticulum stress. This finding might support phenolic acid action in restoring the response to insulin in OB-VAT.
Since PCA effects on VAT were mainly exerted on the phosphorylation of insulin pathway molecules, we then questioned whether this action might be related with the activity of the protein phosphatase PTP1B. This enzyme is a negative regulator of the insulin signaling pathway and plays important roles during obesity and diabetes, reason why it is becoming a promising drug target for the treatment of T2D and at-risk OB [43]. The novel finding of a reduction in PTP1B activity observed in OB-VAT after PCA exposure well correlates with the evidence showing that polyphenolic compounds from natural origin exhibit an inhibitory activity on PTP1B in different experimental models [44]. Hence, higher insulin-stimulated IRS-1 phosphorylation and, consequently, increased downstream activation of Akt might be related with attenuated PTP1B activity found in PCA-treated OB tissues. Nonetheless, further studies are needed to establish a possible relationship between PTP1B activity and the phosphorylation of insulin signaling molecules under these conditions. Furthermore, this investigation provides interesting evidence of an impaired protein expression of IRS-1, GLUT4, and PTP1B in VAT from obese individuals compared to lean subjects. These findings are well correlated with those from Tinahones et al. for mRNA expression of such molecules between both groups [45].
As regards the effects on inflammation, the finding that PCA was able to significantly stimulate the secretion of adiponectin, an anti-inflammatory and anti-diabetic molecule, in VAT from lean individuals was of particular interest and shows consistency with our previous results from isolated human visceral adipocytes exposed to PCA [22]. Interestingly, protective effect of PCA on inflammation was also accompanied by a lower secretion of IL-1β after PCA treatment in VAT. This PCA-related reduction in the production of IL-1β, a potent pro-inflammatory cytokine, is coherent with the reduction found in LPS-induced acute lung injury mice injected with PCA [46]. Therefore, much attention has to be paid to anti-/pro-inflammatory adipocytokines because of their relationship with insulin sensitivity, glucose, and lipid metabolism [47].
Finally, our data demonstrating an inhibitory role for PCA on phospho-NF-κB in OB-VAT might also be related with the reduction in IL-6 since NF-κB is involved in the control of the IL-6 expression, as it was mentioned elsewhere.
Additionally, the higher activation of NF-κB found in VAT from OB subjects compared to lean subjects might be related to the enhanced IL-6 secretion observed in such tissues. In particular, chronic systemic inflammation found in VAT of overweight and OB individuals is frequently associated to an increased secretion of pro-inflammatory cytokines such as IL-6. Indeed, the expression of IL-6 is enhanced by the phosphorylation of the transcription factor NF-κB leading to the binding of NF-κB to the promoter of IL-6 gene [48]. Interestingly, the lower secretion of adiponectin we observed in VAT samples from OB subjects correlates well with data suggesting that adiponectin expression decreases with increasing adiposity [49].
Among polyphenols, ACNs have been considered one of the most interesting class of bioactive food components that are rapidly metabolized ultimately leading to the formation of phenolic acids and aldehydes [50]. In particular, at physiological pH, ACNs easily convert to PCA [20, 25]. PCA is also abundantly formed and absorbed in the large intestine because of microbial metabolization [51, 52]. This may explain why high concentration of PCA (Cmax about 10 μM) has been found in plasma after ingestion of ACN-rich juice [24]. However, it should be considered that the bioavailability can be affected by “chronic” exposure to polyphenols, as the daily consumption of ACN-rich food can provide. Furthermore, the polyphenols might concentrate in the tissue microenvironment [53]. From this point of view, the concentration of PCA tested in our experiments, although higher than that reported after ingestion of food rich in ACN, can be reached plausibly at cellular level. On the other hand, our data indicated that PCA, interacting with VAT for 24 h, modulates intracellular activities despite having a half life (t1/2) of nearly 10 h [25]. Thus, although the physiological in vivo context in which dietary polyphenols exert their influence is undoubtedly much more complex than that available from an in vitro system, it could be argued that, at least, micromolar concentrations of PCA, which are comparable to those achieved in vivo following a Mediterranean type diet, can help fight tissue impairment associated with obesity.
In conclusion, our work showed that PCA counteracts insulin resistance and diminishes inflammation in VAT during obesity by decreasing PTP1B activity. These findings offer a novel insight into the beneficial effects of an ACN-rich diet on the regulation of insulin-sensitivity, and promote the potential application of those polyphenols toward the management of insulin resistance in obesity and diabetes.
References
Stevens GA, et al. National, regional, and global trends in adult overweight and obesity prevalences. Popul Health Metr. 2012;10:22.
Johnson AR, Milner JJ, Makowski L. The inflammation highway: metabolism accelerates inflammatory traffic in obesity. Immunol Rev. 2012;249:218–38.
Wensveen FM, Valentic S, Sestan M, Turk Wensveen T, Polic B. The “Big Bang” in obese fat: events initiating obesity-induced adipose tissue inflammation. Eur J Immunol. 2015;45:2446–56.
Lee BC, Lee J. Cellular and molecular players in adipose tissue inflammation in the development of obesity-induced insulin resistance. Biochim Biophys Acta. 2014;1842:446–62.
de Winther MP, Kanters E, Kraal G, Hofker MH. Nuclear factor kappaB signaling in atherogenesis. Arterioscler Thromb Vasc Biol. 2005;25:904–14.
Ghosh S, Karin M. Missing pieces in the NF-kappaB puzzle. Cell. 2002;109:S81–96.
White MF. Insulin signaling in health and disease. Science. 2003;302:1710–1.
Moller DE. New drug targets for type 2 diabetes and the metabolic syndrome. Nature. 2001;414:821–7.
Goldstein BJ, Bittner-Kowalczyk A, White MF, Harbeck M. Tyrosine dephosphorylation and deactivation of insulin receptor substrate-1 by protein-tyrosine phosphatase 1B. Possible facilitation by the formation of a ternary complex with the Grb2 adaptor protein. J Biol Chem. 2000;275:4283–9.
Wang XY, Bergdahl K, Heijbel A, Liljebris C, Bleasdale JE. Analysis of in vitro interactions of protein tyrosine phosphatase 1B with insulin receptors. Mol Cell Endocrinol. 2001;173:109–20.
Elchebly M, et al. Increased insulin sensitivity and obesity resistance in mice lacking the protein tyrosine phosphatase-1B gene. Science. 1999;283:1544–8.
Santangelo C, et al. Consumption of extra-virgin olive oil rich in phenolic compounds improves metabolic control in patients with type 2 diabetes mellitus: a possible involvement of reduced levels of circulating visfatin. J Endocrinol Invest. 2016;39:1295–301.
Dourado GK, Cesar TB. Investigation of cytokines, oxidative stress, metabolic, and inflammatory biomarkers after orange juice consumption by normal and overweight subjects. Food Nutr Res. 2015;59:28147.
Bahadoran Z, et al. Effect of broccoli sprouts on insulin resistance in type 2 diabetic patients: a randomized double-blind clinical trial. Int J Food Sci Nutr. 2012;63:767–71.
Perera PK, Li Y. Functional herbal food ingredients used in type 2 diabetes mellitus. Pharmacogn Rev. 2012;6:37–45.
Alkerwi A, Sauvageot N, Crichton GE, Elias MF, Stranges S. Daily chocolate consumption is inversely associated with insulin resistance and liver enzymes in the Observation of Cardiovascular Risk Factors in Luxembourg study. Br J Nutr. 2016;115:1661–8.
Hosseini B, Saedisomeolia A, Wood LG, Yaseri M, Tavasoli S. Effects of pomegranate extract supplementation on inflammation in overweight and obese individuals: a randomized controlled clinical trial. Complement Ther Clin Pract. 2016;22:44–50.
Pandey KB, Rizvi SI. Plant polyphenols as dietary antioxidants in human health and disease. Oxid Med Cell Longev. 2009;2:270–8.
Hertog MG, Hollman PC, Katan MB, Kromhout D. Intake of potentially anticarcinogenic flavonoids and their determinants in adults in The Netherlands. Nutr Cancer. 1993;20:21–9.
Vitaglione P, et al. Protocatechuic acid is the major human metabolite of cyanidin-glucosides. J Nutr. 2007;137:2043–8.
Masella R, et al. Protocatechuic acid and human disease prevention: biological activities and molecular mechanisms. Curr Med Chem. 2012;19:2901–17.
Scazzocchio B, et al. Cyanidin-3-O-beta-glucoside and protocatechuic acid exert insulin-like effects by upregulating PPARgamma activity in human omental adipocytes. Diabetes . 2011;60:2234–44.
Scazzocchio B, et al. Protocatechuic acid activates key components of insulin signaling pathway mimicking insulin activity. Mol Nutr Food Res. 2015;59:1472–81.
McKay DL, Chen CY, Zampariello CA, Blumberg JB. Flavonoids and phenolic acids from cranberry juice are bioavailable and bioactive in healthy older adults. Food Chem. 2015;168:233–40.
de Ferrars RM, et al. The pharmacokinetics of anthocyanins and their metabolites in humans. Br J Pharmacol. 2014;171:3268–82.
Masella R, et al. Oxidised LDL modulate adipogenesis in 3T3-L1 preadipocytes by affecting the balance between cell proliferation and differentiation. FEBS Lett. 2006;580:2421–9.
Crowley RK, et al. SFRP2 is associated with increased adiposity and VEGF Expression. PLoS ONE. 2016;11:e0163777.
Baumgartner RR, et al. Bioactivity-guided isolation of 1,2,3,4,6-Penta-O-galloyl-D-glucopyranose from Paeonia lactiflora roots as a PTP1B inhibitor. J Nat Prod. 2010;73:1578–81.
Muthusamy VS, et al. Inhibition of protein tyrosine phosphatase 1B and regulation of insulin signalling markers by caffeoyl derivatives of chicory (Cichorium intybus) salad leaves. Br J Nutr. 2010;104:813–3.
Lima FB, Thies RS, Garvey WT. Glucose and insulin regulate insulin sensitivity in primary cultured adipocytes without affecting insulin receptor kinase activity. Endocrinology . 1991;128:2415–26.
Fried SK, Moustaid-Moussa N. Culture of adipose tissue and isolated adipocytes. Methods Mol Biol. 2001;155:197–212.
Carswell KA, Lee MJ, Fried SK. Culture of isolated human adipocytes and isolated adipose tissue. Methods Mol Biol. 2012;806:203–14.
Smith U, Jacobsson B. Studies of human adipose tissue in culture. II. Effects of insulin and of medium glucose on lipolysis and cell size. Anat Rec. 1973;176:181–3.
Smith U. Morphologic studies of human subcutaneous adipose tissue in vitro. Anat Rec. 1971;169:97–104.
Tan BK, Chen J, Lehnert H, Kennedy R, Randeva HS. Raised serum, adipocyte, and adipose tissue retinol-binding protein 4 in overweight women with polycystic ovary syndrome: effects of gonadal and adrenal steroids. J Clin Endocrinol Metab. 2007;92:2764–72.
Hanhineva K, et al. Impact of dietary polyphenols on carbohydrate metabolism. Int J Mol Sci. 2010;11:1365–402.
Kay CD, Mazza G, Holub BJ, Wang J. Anthocyanin metabolites in human urine and serum. Br J Nutr. 2004;91:933–42.
Kay CD, Mazza GJ, Holub BJ. Anthocyanins exist in the circulation primarily as metabolites in adult men. J Nutr. 2005;135:2582–8.
Kay CD, Kroon PA, Cassidy A. The bioactivity of dietary anthocyanins is likely to be mediated by their degradation products. Mol Nutr Food Res. 2009;53:S92–101.
Candiloros H, et al. Decreased erythrocyte membrane fluidity in poorly controlled IDDM. Influence of ketone bodies. Diabetes Care. 1995;18:549–51.
Jain SK, et al. Low levels of hydrogen sulfide in the blood of diabetes patients and streptozotocin-treated rats causes vascular inflammation? Antioxid Redox Signal. 2010;12:1333–7.
Kawahito S, Kitahata H, Oshita S. Problems associated with glucose toxicity: role of hyperglycemia-induced oxidative stress. World J Gastroenterol. 2009;15:4137–42.
Cho H. Protein tyrosine phosphatase 1B (PTP1B) and obesity. Vitam Horm. 2013;91:405–24.
Jiang CS, Liang LF, Guo YW. Natural products possessing protein tyrosine phosphatase 1B (PTP1B) inhibitory activity found in the last decades. Acta Pharmacol Sin. 2012;33:1217–45.
Tinahones FJ, et al. Caspase induction and BCL2 inhibition in human adipose tissue: a potential relationship with insulin signaling alteration. Diabetes Care. 2013;36:513–21.
Zhang X, et al. Protective effects of protocatechuic acid on acute lung injury induced by lipopolysaccharide in mice via p38MAPK and NF-kappaB signal pathways. Int Immunopharmacol. 2015;26:229–36.
Lee YA, et al. Synergy between adiponectin and interleukin-1beta on the expression of interleukin-6, interleukin-8, and cyclooxygenase-2 in fibroblast-like synoviocytes. Exp Mol Med. 2012;44:440–7.
Wang LH, Yang XY, Zhang X, Farrar WL. Inhibition of adhesive interaction between multiple myeloma and bone marrow stromal cells by PPARgamma cross talk with NF-kappaB and C/EBP. Blood. 2007;110:4373–84.
Yadav A, Kataria MA, Saini V, Yadav A. Role of leptin and adiponectin in insulin resistance. Clin Chim Acta. 2013;417:80–4.
Czank C, et al. Human metabolism and elimination of the anthocyanin, cyanidin-3-glucoside: a (13)C-tracer study. Am J Clin Nutr. 2013;97:995–1003.
Hidalgo M, et al. Metabolism of anthocyanins by human gut microflora and their influence on gut bacterial growth. J Agric Food Chem. 2012;60:3882–90.
Williamson G, Clifford MN. Colonic metabolites of berry polyphenols: the missing link to biological activity? Br J Nutr. 2010;104:S48–66.
Vari R, et al. Protocatechuic acid induces antioxidant/detoxifying enzyme expression through JNK-mediated Nrf2 activation in murine macrophages. J Nutr Biochem. 2011;22:409–17.
Acknowledgements
We thank Patrizia De Sanctis, Center for Gender-Specific Medicine, Italian National Institute of Health, for her technical assistance. This work was funded by the Grant ISS/USA “Preventive/Therapeutic potential of food anthocyanins against insulin resistance and related metabolic disorders - 11US/23” to RM. PO was funded by Becas-Chile Postdoctoral Fellowship No. 74140009 from CONICYT. Grant ISS/USA “Preventive/Therapeutic potential of food anthocyanins against insulin resistance and related metabolic disorders - 11US/23”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ormazabal, P., Scazzocchio, B., Varì, R. et al. Effect of protocatechuic acid on insulin responsiveness and inflammation in visceral adipose tissue from obese individuals: possible role for PTP1B. Int J Obes 42, 2012–2021 (2018). https://doi.org/10.1038/s41366-018-0075-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0075-4
- Springer Nature Limited
This article is cited by
-
Encapsulated phenolic compounds: clinical efficacy of a novel delivery method
Phytochemistry Reviews (2024)
-
Protocatechuic acid abrogates oxidative insults, inflammation, and apoptosis in liver and kidney associated with monosodium glutamate intoxication in rats
Environmental Science and Pollution Research (2022)
-
Sarsasapogenin improves adipose tissue inflammation and ameliorates insulin resistance in high-fat diet-fed C57BL/6J mice
Acta Pharmacologica Sinica (2021)
-
The role of anthocyanins as antidiabetic agents: from molecular mechanisms to in vivo and human studies
Journal of Physiology and Biochemistry (2021)