Abstract
TFE3-rearranged renal cell cancer (tRCC) is a rare form of RCC that involves chromosomal translocation of the Xp11.2 TFE3 gene. Despite its early onset and poor prognosis, the molecular mechanisms of the pathogenesis of tRCC remain elusive. This study aimed to identify novel therapeutic targets for patients with primary and recurrent tRCC. We collected 19 TFE3-positive RCC tissues that were diagnosed by immunohistochemistry and subjected them to genetic characterization to examine their genomic and transcriptomic features. Tumor-specific signatures were extracted using whole exome sequencing (WES) and RNA sequencing (RNA-seq) data, and the functional consequences were analyzed in a cell line with TFE3 translocation. Both a low burden of somatic single nucleotide variants (SNVs) and a positive correlation between the number of somatic variants and age of onset were observed. Transcriptome analysis revealed that four samples (21.1%) lacked the expected fusion event and clustered with the genomic profiles of clear cell RCC (ccRCC) tissues. The fusion event also demonstrated an enrichment of upregulated genes associated with mitochondrial respiration compared with ccRCC expression profiles. Comparison of the RNA expression profile with the TFE3 ChIP-seq pattern data indicated that PPARGC1A is a metabolic regulator of the oncogenic process. Cell proliferation was reduced when PPARGC1A and its related metabolic pathways were repressed by its inhibitor SR-18292. In conclusion, we demonstrate that PPARGC1A-mediated mitochondrial respiration can be considered a potential therapeutic target in tRCC. This study identifies an uncharacterized genetic profile of an RCC subtype with unique clinical features and provides therapeutic options specific to tRCC.
Similar content being viewed by others
Introduction
Transcription factor E3 (TFE3) gene-rearrangement renal cell carcinoma (tRCC) is a rare subtype of kidney cancer characterized by chromosomal rearrangements involving the XP11 locus1. This subtype, previously known as Xp11.2 translocation RCC, is the most common subtype of the MiT family of translocation RCCs2,3. Although tRCC is most commonly diagnosed in children and young adults4,5, its incidence among older adults is increasing, and it is estimated to account for approximately 4% of adult RCC cases6,7,8. In many cases, tRCC is diagnosed in an advanced stage at presentation and is usually associated with unfavorable outcomes9,10. However, its pathophysiology and genetic characteristics remain poorly understood3. Unfortunately, tRCC is not responsive to standard treatments, and no approved treatment options are available10,11.
Modifications and adaptations in cellular metabolism are hallmarks of cancer cells. After the pioneering discovery made by Otto Warburg showing that cancer cells preferentially use glycolysis to meet their energetic needs, several studies have shown that cancer cells adopt alternative metabolic methods for survival12. Recent findings have elucidated the metabolic changes, also termed metabolic reprogramming, that are observed in cancer cells in response to environmental challenges13,14. One major, well-described cell metabolism modulator is peroxisome proliferator-activated receptor gamma coactivator 1 (PPARGC1A), which regulates mitochondrial biogenesis and oxidative metabolism15.
To better understand the molecular landscape of tRCC and identify potential therapeutic targets, we performed a genetic analysis of tRCC patients diagnosed based on TFE3 overexpression using immunohistochemical (IHC) staining16. We observed distinct genetic and metabolic profiles between clear cell renal cell carcinoma (ccRCC) and normal kidney cells. Furthermore, the results of this study demonstrate that a metabolic mediator of TFE3 activation is involved in tRCC.
Materials and methods
Cell culture and transfection
The human renal clear cell carcinoma cell line Caki-1 and the Xp11.2 translocation renal cell carcinoma cell lines (UOK109, UOK120, UOK124, UOK145, and UOK146) were maintained in DMEM (Cytiva, Marlborough, MA). The human renal proximal tubular epithelial cell line HK-2 was maintained in DMEM/F-12 medium (Biowest, Bradenton, FL). All media were supplemented with 10% FBS (Cytiva, Marlborough, MA) and 1% penicillin‒streptomycin (Thermo Fisher Scientific, Waltham, MA). All cells were incubated at 37 °C in a humidified atmosphere containing 5% CO2. Transfection was performed with short interfering RNAs (siRNAs) against TFE3 and PPARGC1A (Bioneer, Daejeon, Korea) using Lipofectamine RNAiMAX transfection reagents (Thermo Fisher, Waltham, MA) following the manufacturer’s instructions.
Whole exome sequencing (WES) and acquisition and processing of RNA-seq data
DNA and RNA samples were prepared from the tumor and blood tissues of participants by standard procedures and were processed at the Theragen Etex Bio Institute (Suwon, Korea) for WES. The reads were processed according to GATK 4.0 Best Practices for somatic single nucleotide variant (SNV) and structural change analysis17. RNA-seq reads were aligned by STAR aligner, and DESeq2 was used to identify differentially expressed genes (DEGs)18. The data related to the gene fusion events for TCGA samples were obtained from the TCGA Fusion Gene Database19. The MR4Cancer tool was used to identify nontranscriptional master regulators in our dataset based on the TCGA kidney renal clear cell carcinoma (KIRC) dataset20. To identify a possible master regulator of the input DEG set, each set was divided into two subsets based on either a positive or a negative Spearman correlation of the expression of the regulon genes.
Chromatin immunoprecipitation (ChIP)-seq
UOK146 cells (tRCC with a PRCC-TFE3 fusion) were fixed with 1% formaldehyde and subjected to ChIP as previously described21 using an antibody against TFE3 (Sigma‒Aldrich, HPA023881). ChIP-seq data were mapped to the human genome (hg19) using the Bowtie algorithm, allowing up to two mismatches. Reads mapped to more than 20 locations along the genome were discarded. ChIP-seq data generated using an IgG antibody were used as a control22. Peaks were identified using MACS2 with an FDR-adjusted P value cutoff of 0.05. Two biological replicates were generated23.
Chromatin immunoprecipitation (ChIP)-qPCR
ChIP assays were performed using the SimpleChIP Enzymatic Chromatin IP Kit (Cell Signaling Technology, Danvers, MA) according to the manufacturer’s instructions. UOK146 cells were cross-linked with 1% formaldehyde for 10 min, and chromatin was extracted using 1 M DTT. The prepared chromatin was digested with micrococcal nuclease and sonicated to obtain fragments of approximately 150–900 base pairs. Immunoprecipitation was conducted with either an antibody against TFE3 (Abcam, ab93808) or IgG using protein G magnetic beads at 4 °C. Following immunoprecipitation, the beads were washed and reversely cross-linked, and the eluted DNA was purified. Purified DNA samples, along with input DNA samples, were subjected to quantitative real-time PCR (qRT‒PCR) analysis using SYBR® Green Master Mix (Bio‒Rad, Hercules, CA). Primers specific to the PPARGC1A promoter were designed to amplify the regions corresponding to two distinct peaks identified in the ChIP-seq data. The primer sequences for peak 1 were 5′-GGGAAGGTTAAGTGGGTGGT-3′ (forward) and 5′-TCCTGCATAGCACAGTGGAG-3′ (reverse), and those for peak 2 were 5′-GGTTCTGCCTGGAGTTGTTC-3′ (forward) and 5′-CCATCGCTAGCTTTCCAGTC-3′ (reverse).
Mitochondrial mass and cell proliferation
siRNAs against TFE3 and PPARGC1A (Bioneer, Daejeon, Korea) were transfected into UOK146 cells using Lipofectamine RNAiMAX transfection reagents (Thermo Fisher, Waltham, MA) in 6-well plates at concentrations ranging from 10–80 nM. The knockdown efficiency was checked after 72 h. At 24 h posttransfection, the cells were plated in 96-well plates at a density of 1 × 104 cells/well and incubated in the presence or absence of SR18292 (60 µM) or oligomycin (20 µM). After 48 h, cell proliferation was evaluated with a Cell Counting Kit-8 (CCK8; Dojindo, Japan) according to the manufacturer’s instructions. The absorbance was measured at 450 nm using a Glomax Discover System (Promega, Madison, WI).
Mitochondrial mass was analyzed by flow cytometry in cells labeled with MitoTracker Deep Red FM (M22426, Thermo Fisher Scientific, Waltham, MA). Forty-eight hours after transfection, the cells were incubated in warm PBS containing 50 nM MitoTracker Deep Red FM for 20 min at 37 °C. The samples were washed in PBS and then fixed with PBS containing 2.5% formaldehyde. Fluorescence was measured by a BD LSRII (BD Biosciences, San Jose, CA) flow cytometer. BD FACSDiva (BD Biosciences, San Jose, CA) software was used for data analysis.
RNA extraction and qRT‒PCR
Total RNA was isolated from cells using the RNeasy Plus Mini Kit (Qiagen, Germany) according to the manufacturer’s instructions. Complementary DNA (cDNA) was synthesized from 0.5 μg of RNA using the PrimeScript RT reagent Kit (Takara Bio, Japan). qRT‒PCR was performed using SYBR® Green Master Mix (Bio-Rad, Hercules, CA) on a Bio-Rad CFX96 instrument (Bio-Rad, Hercules, CA). Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was used as the endogenous control for mRNA normalization. Primer sequences used in qRT-PCR are listed in Supplementary Table 1.
Protein extraction and western blotting
Cells were harvested and lysed using RIPA buffer (Thermo Fisher Scientific, Waltham, MA) supplemented with a protease inhibitor cocktail (Roche, Switzerland). After centrifugation, the protein concentration was determined using a BCA assay kit (Thermo Fisher Scientific, Waltham, MA) and mixed with sample buffer at 100 °C for 5 min. An equal amount of protein was separated via SDS‒PAGE and transferred onto NC membranes (Cytiva, Marlborough, MA). The membranes were blocked with 5% skim milk (BD Biosciences, San Jose, CA) in TBS-T buffer and subsequently incubated with primary and secondary antibodies. Protein bands were visualized using the SuperSignal™ West Pico PLUS ECL kit (Thermo Fisher Scientific, Waltham, MA) on an Amersham Imager AI680 (General Electric, Boston, MA). The following antibodies were used: anti-E-cadherin (Cell Signaling Technology, #3195), anti-N-cadherin (Cell Signaling Technology, #13116), anti-vimentin (Cell Signaling Technology, #5741), anti-α-SMA (Abcam, ab5694) and anti-β-actin (Sigma‒Aldrich, A5441).
Migration assay
Cells in serum-free DMEM were reseeded into the upper chamber of a transwell insert (Corning, Corning, NY), and the lower chamber was filled with DMEM containing 10% FBS. After 24 h of incubation, the migrated cells in the upper chamber were fixed with cold methanol and stained with 1% crystal violet. The migrated cells were visualized and imaged using an EVOS XL Core microscope (Thermo Fisher Scientific, Waltham, MA).
Results
We initially collected 19 RCC samples with TFE overexpression, as determined by IHC, six ccRCC tissue samples, and four normal kidney tissue samples. The median age of the 19 patients with TFE3-positive RCC was 45 years (interquartile range [IQR]: 40–52), and 11 patients (57.9%) were female (Table 1). Six patients (31.6%) had locally advanced disease, and four (21.1%) had distant metastasis. Seven patients (36.8%) underwent partial nephrectomy, and five patients (26.3%) underwent surgery via a laparoscopic approach. The mean size of the tumors was 5.0 cm (IQR: 3.3–6.7). Recurrence was observed in four patients, and the median recurrence-free survival was 31 months (IQR: 24–54).
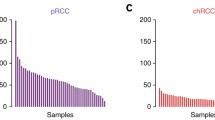
Among the 19 TFE3-positive specimens, four samples did not demonstrate a TFE3 fusion according to the results of the confirmative fluorescence in situ hybridization (FISH) assay or RNA-seq analysis. Therefore, 15 samples with confirmed tRCC remained (Fig. 1a). tRCC tumors are sometimes misdiagnosed as ccRCC24,25. Therefore, we searched for such samples in the TCGA KIRC database by screening for TFE3 translocation events via WES/RNA-seq. Among the 417 ccRCC samples, six harbored TFE3 translocations19. There were fewer somatic mutations in tRCC than in ccRCC (45.6 vs. 58.3, P = 2.5 × 10−6, Student’s t test; Fig. 1b). VHL was identified in our four ccRCC samples (Fig. 1a) but not in any of the tRCC samples. The percentage of the genome affected by structural changes in the tRCC and ccRCC samples was comparable (5.7% vs. 7.8%, P = 0.47, Student’s t test; Fig. 1b). These observations indicate the presence of a strong oncogenic driver in tRCC. No variants or genes other than TFE3 translocations have been observed recurrently, supporting this interpretation. In addition, compared to ccRCC (R = 0.60), tRCC was more strongly correlated (R = 0.84) with the number of somatic variants and the age of onset (Fig. 1c).
a A clinical and genomic overview of 15 pathologically confirmed tRCC and four ccRCC tumors. b Number of somatic SNVs and the genomic portion of structural changes between tRCC and ccRCC samples. c Differences in the correlation between the number of somatic SNVs and patient age. d Schematic diagram representing TFE3 fusion events identified by RNA-seq. For each gene, the upper diagrams denote the gene structure with alternating exons and introns. The lower diagrams show the protein structure. tRCC translocation renal cell carcinoma, ccRCC clear cell renal cell carcinoma, SNVs single nucleotide variations, WES whole exome sequencing, FISH fluorescence in situ hybridization, TCGA The Cancer Genome Atlas, LOH loss of heterozygosity.
Next, we performed RNA-seq analysis using fresh-frozen samples (19 tRCC, six ccRCC, and four normal kidney tissue samples). Based on the RNA-seq data, we identified six fusion partner genes of TFE3 in 15 TFE3 translocation-positive tRCC samples (Fig. 1d, Table 2, Supplementary Fig. 1). Principal component analysis (PCA) grouped the samples into three main clusters, which corresponded to tRCC, ccRCC, and normal tissues (Fig. 2a). Remarkably, the four tumors that were initially suspected to be tRCC but lacked TFE3 fusion clustered with ccRCC, confirming that TFE3 fusion is a strong determinant of tRCC. Comparison of the tRCC and ccRCC gene expression profiles revealed 2573 differentially expressed genes (DEGs) (Fig. 2b, c). Gene Ontology (GO) analysis of upregulated DEGs in tRCC compared to those in ccRCC revealed enrichment associated with metabolic pathways, such as the tricarboxylic acid (TCA) cycle, respiratory electron transport, and mitochondrial metabolic pathways. Genes with downregulated expression in tRCC included those related to cell adhesion and cell migration (Fig. 2d). Notably, the adaptive immune response pathway was downregulated, suggesting a diminished potential for a robust response to immunotherapy interventions. Gene set enrichment analysis (GSEA) of DEGs consistently revealed enrichment associated with metabolic pathways related to the TCA cycle and respiratory electron transport (Fig. 2e). These results indicate the presence of an oncogenic metabolic regulation pathway specific to tRCC. A closer look at the upregulated pathways revealed a unique metabolic environment that may lead to poor responses to conventional chemotherapies (Fig. 2f).
a PCA plot of RCC and normal tissues. b Volcano plot, c Heatmap, d GO profiles, and e GSEA results obtained using DEGs in tRCC and ccRCC samples. f Pathways enriched with genes upregulated in tRCC. g Analysis of the master regulators of the DEGs. PCA principal component analysis, tRCC translocation renal cell carcinoma, ccRCC clear cell renal cell carcinoma, GO Gene Ontology, GSEA gene set enrichment analysis, DEGs differentially expressed genes, NES normalized enrichment score, TNFSF tumor necrosis factor superfamily, IL interleukin, TCA tricarboxylic acid, FC fold change.
To identify a possible downstream regulator of aberrant TFE3, a master regulator analysis was performed using our tRCC RNA-seq results with ARACNe26. The output was then compared to an output generated using ccRCC data from the TCGA KIRC cohort. The analysis revealed PPARGC1A as the top nontranscriptional regulator in the tRCC RNA-seq data (Fig. 2g). PPARGC1A encodes a transcriptional coactivator for steroid and nuclear receptors that plays an essential role in metabolic reprogramming15. This result suggests that PPARGC1A may play an integral role in the metabolic reprogramming of tRCC oncogenic processes.
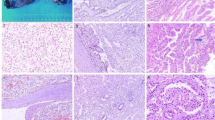
To identify the genomic targets of the fused TFE3 gene, TFE3 ChIP-seq was performed using the UOK146 cell line, which harbors a PRCC-TFE3 gene fusion27. Two biological replicates resulted in 6952 overlapping peaks enriched around transcription start sites (TSSs; Fig. 3a). Motif analysis revealed strong enrichment in CAGCTG sequences (P < 1.0 × 10−24), which completely overlapped with the known TFE3 binding motif (Fig. 3b)28. A comparison of DEGs from the RNA-seq experiment and TFE3 ChIP-seq data yielded 284 genes, including PPARGC1A (Fig. 3c). To evaluate whether the TFE3 fusion gene is associated with the regulation of PPARGC1A, we identified two TFE3 binding elements near the TSS of PPARGC1A (Fig. 3d, e and Supplementary Table 2). Combined with the master regulator analysis results (Fig. 2g), we observed that unique metabolic processes of tRCC could be regulated by the fusion of TFE3, resulting in the upregulation of PPARGC1A expression. To confirm whether the expression of PPARGC1A was indeed increased in TFE3 translocation-positive tRCC, the tumor tissues were stained with a PPARGC1A-specific antibody. The majority of tRCC samples showed increased expression of PPARGC1A (0/3 normal, 0/3 ccRCC, and 7/8 in tRCC samples; Fig. 3f). In addition, reanalysis of RNA-seq data from a previous study revealed upregulated PPARGC1A in cells with TFE3 fusion (Supplementary Fig. 2)29.
a Profile of TFE3 ChIP-seq signals relative to the TSS determined using the UOK146 cell line. b Motif analysis of the TFE3 ChIP-seq results. c Comparison of RNA-seq and ChIP-seq analyses. d TFE3 binding sites in the PPARGC1A upstream region. *P = 1.3 × 10−9. **P = 8.1 × 10−14. e ChIP‒qPCR analysis of the TFE3 binding sites upstream of PPARGC1A. ChIP‒qPCR was applied to amplify chromatin immunoprecipitated from the PPARGC1A gene promoter with an anti-TFE3 antibody using two independent sets of primers for peaks 1 and 2 in (d). *, 0.001 < P < 0.05. **, P < 0.001. f Immunohistochemical analysis of PPARGC1A in tumor tissues used for genome analysis. Scale bar = 200 µm. ChIP chromatin immunoprecipitation, TSS transcription start site, DEG differentially expressed gene, tRCC translocation renal cell carcinoma, ccRCC clear cell renal cell carcinoma.
These findings demonstrate that PPARCG1A is a strong mediator of TFE3-mediated increases in the TCA cycle and related pathways. Thus, we tested whether treatment of cells with reduced expression of TFE3, PPARGC1A, or mitochondrial inhibitors impacted their survival. Downregulation of TFE3, PPARGC1A, or both significantly reduced mitochondrial mass and membrane potential (Fig. 4a, b). A more potent effect on cell viability was observed upon treatment with a selective PPARGC1A inhibitor, SR-1829230 and the mitochondrial respiration inhibitor oligomycin in tRCC cell lines with various TFE3 fusions (Fig. 4c–g). This effect was not observed in the normal kidney cell line. Although the effect on ccRCC cells may be dependent on VHL mutation status (Supplementary Fig. 3), these results indicate that PPARGC1A is a key regulator of mitochondrial respiration and cell proliferation in tRCC.
a Relative mitochondrial mass after knocking down TFE3, PPARGC1A, or both in UOK146 cells. b Relative ratio of red versus green JC-1 signals. FCCP was used as a positive control in UOK146 cells. c–g Relative cell viability after downregulation of TFE3, PPARGC1A, or both in UOK146 (c), UOK109 (d), UOK120 (e), UOK124 (f), and UOK145 (g) cells. Inhibitors targeting mitochondrial function (oligomycin) and PPARGC1A (SR-18292) were also applied. *0.001 < P < 0.05. **P < 0.001.
Finally, we investigated how the TFE3-mediated modulation of metabolic pathways affects the cancer phenotype. We altered PPARGC1A expression and investigated its effects on cancer aggressiveness. Treatment of UOK146 cells with siPPARGC1A upregulated E-cadherin, an epithelial marker, and downregulated N-cadherin, a mesenchymal marker, at both the mRNA and protein levels (Fig. 5a, b). Additionally, knockdown of PPARGC1A reduced the migration of UOK146 cells (Fig. 5c). These findings suggest that the TFE3-mediated modulation of the PPARGC1A-mediated modulation of metabolic pathways plays a role in epithelial–mesenchymal transition (EMT) and cancer aggressiveness.
a, b EMT markers after knocking down PPARGC1A at the mRNA (a) and protein (b) levels. The mRNA and protein expression levels of EMT markers were evaluated by real-time PCR and western blotting, respectively. *0.001 < P < 0.05. **P < 0.001. c Cell migration analysis after knocking down PPARGC1A in UOK146 cells. In vitro cell migration was assessed using transfilter migration assays; representative images of migrated cells are shown. siControl control siRNA, siPPARGC1A siRNA for PPARGC1A.
Discussion
It is estimated that tRCC comprises approximately one-third of pediatric RCC cases and 15% of RCC cases in patients aged 45 years or younger4,7. Our group previously identified 61 patients out of 8384 consecutive patients with RCC (0.7%) in the largest multicenter study to date31. Despite the increased recognition of tRCC, its diagnosis remains challenging. tRCCs typically display papillary and/or alveolar architecture and are composed of cells with voluminous eosinophilic and/or clear cytoplasm2,6,32. Therefore, they can be histologically confused with papillary or ccRCCs. Indeed, TFE3 fusions were identified in six ccRCC samples and ten papillary RCC samples out of 417 KIRC and 289 KIRP TCGA samples, respectively19. This finding indicates that tRCCs are frequently misclassified as ccRCC or papillary RCC without accurately evaluating fusion events. The overexpression of TFE3 can be detected by IHC32, which is widely used as a diagnostic tool. However, accumulating evidence suggests that IHC-based diagnosis of tRCC may generate false-positives33. Our study had a 21.1% (4/19) false-positive rate in immunohistochemical diagnosis, as these falsely diagnosed patients showed greater genetic resemblance to patients with ccRCC than to those with tRCC. This result was confirmed by the presence of VHL mutations (Fig. 1a) and PCA of the RNA-seq data (Fig. 2a). These patients were also older than patients with TFE3 fusions, and their oncological outcomes were inferior to those of the other patients. Our comprehensive genomic profiling of tRCC tumor tissues revealed fewer somatic mutations in tRCC than in ccRCC, suggesting that tRCC is strongly associated with oncogenes (Fig. 1b). Our transcriptomic profiling of tRCC tissues revealed that tRCC is associated with a unique metabolic profile that is highly enriched in mitochondrial respiration and the TCA cycle. Our transcriptomic analysis identified PPARGC1A as a master regulator of the transcriptomic changes observed in tRCC tissues (Fig. 2g). Subsequent ChIP-seq analysis using a tRCC cell line (UOK146) demonstrated that TFE3 binds to the PPARGC1A promoter to upregulate DEGs more often than to downregulate DEGs (Fig. 3d, e). These findings indicate a gain-of-function effect of the TFE3 fusion, resulting in unique mitochondria-focused metabolic reprogramming via activation of PPARGC1A. In addition, TFE3-overexpressing cells and cells harboring various TFE3 fusions clustered together, supporting our conclusion29.
Many glycolytic tumor cells rely on lactate production to generate NAD+ for their anabolic metabolism (known as the Warburg effect)34. Our analyses suggest that tRCC tumors are highly dependent on mitochondrial respiration for energy. The dependence on oxidative phosphorylation for energy production is consistent with that of leukemic stem cells35 and surviving pancreatic cancer cells12. The inability of cells to compensate for mitochondrial energy deprivation by increasing glycolysis renders them highly vulnerable to various therapeutics that inhibit oxidative phosphorylation. Although MTOR inhibitors have been identified as potential targets for treating tRCC36,37, this signal appeared only when we compared matched tumor and normal samples (BP:0002224, Padj = 1.5 × 10−5), suggesting that the MTOR signaling pathway is less prominent than the metabolic pathway that we investigated (Supplementary Figs. 4 and 5).
Through the most comprehensive integrated genetic study to date using 19 TFE3-positive RCC cases, we provide a genomic landscape and a deeper understanding of the oncogenic mechanism of tRCC, facilitating further discovery of a therapeutic strategy for tRCC. Our results indicate that inhibitors of mitochondrial function or PPARGC1A could be efficiently utilized as monotherapy or combination therapy for treating tRCC.
In conclusion, we have demonstrated that PPARGC1A-mediated mitochondrial respiration can be considered a potential therapeutic target in tRCC. This study has identified an uncharacterized genetic profile of an RCC subtype with unique clinical features and provides therapeutic options specific to tRCC.
Data availability
The data generated in this study are available upon request from the corresponding author.
References
Wei, S. et al. Molecular characterization of TFE3-rearranged renal cell carcinoma: a comparative study with papillary and clear cell renal cell carcinomas. Mod. Pathol. 37, 100404 (2024).
Argani, P. MiT family translocation renal cell carcinoma. Semin. Diagn. Pathol. 32, 103–113 (2015).
Kauffman, E. C. et al. Molecular genetics and cellular features of TFE3 and TFEB fusion kidney cancers. Nat. Rev. Urol. 11, 465–475 (2014).
Malouf, G. G. et al. Transcription factor E3 and transcription factor EB renal cell carcinomas: clinical features, biological behavior and prognostic factors. J. Urol. 185, 24–29 (2011).
Qiu Rao et al. Renal cell carcinoma in children and young adults: clinicopathological, immunohistochemical, and VHL gene analysis of 46 cases with follow-up. Int. J. Surg. Pathol. 19, 170–179 (2011).
Argani, P. et al. Xp11 translocation renal cell carcinoma in adults: expanded clinical, pathologic, and genetic spectrum. Am. J. Surg. Pathol. 31, 1149–1160 (2007).
Komai, Y. et al. Adult Xp11 translocation renal cell carcinoma diagnosed by cytogenetics and immunohistochemistry. Clin. Cancer Res. 15, 1170–1176 (2009).
Zhong, M. et al. Dual-color, break-apart FISH assay on paraffin-embedded tissues as an adjunct to diagnosis of Xp11 translocation renal cell carcinoma and alveolar soft part sarcoma. Am. J. Surg. Pathol. 34, 757–766 (2010).
Boilève, A. et al. Immune checkpoint inhibitors in MITF family translocation renal cell carcinomas and genetic correlates of exceptional responders. J. Immunother. Cancer 6, 159 (2018).
Kakoki, K. et al. Long-term treatment with sequential molecular targeted therapy for Xp11.2 translocation renal cell carcinoma: a case report and review of the literature. Clin. Genitourin. Cancer 15, e503–e506 (2017).
Choueiri, T. K. et al. Vascular endothelial growth factor-targeted therapy for the treatment of adult metastatic Xp11.2 translocation renal cell carcinoma. Cancer 116, 5219–5225 (2010).
Viale, A. et al. Oncogene ablation-resistant pancreatic cancer cells depend on mitochondrial function. Nature 514, 628–632 (2014).
Lee, H. & Yoon, H. Mitochondrial sirtuins: energy dynamics and cancer metabolism. Mol. Cells 47, 100029 (2024).
Martínez-Reyes, I. & Chandel, N. S. Cancer metabolism: looking forward. Nat. Rev. Cancer 21, 669–680 (2021).
Schreiber, S. N., Knutti, D., Brogli, K., Uhlmann, T. & Kralli, A. The transcriptional coactivator PGC-1 regulates the expression and activity of the orphan nuclear receptor estrogen-related receptor α (ERRα). J. Biol. Chem. 278, 9013–9018 (2003).
Akgul, M. et al. Diagnostic approach in TFE3-rearranged renal cell carcinoma: a multi-institutional international survey. J. Clin. Pathol. 74, 291–299 (2021).
Poplin, R. et al. Scaling Accurate Genetic Variant Discovery to Tens of Thousands of Samples. http://biorxiv.org/lookup/doi/10.1101/201178 (2017).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Hu, X. et al. TumorFusions: an integrative resource for cancer-associated transcript fusions. Nucleic Acids Res. 46, D1144–D1149 (2018).
Ru, B., Tong, Y. & Zhang, J. MR4Cancer: a web server prioritizing master regulators for cancer. Bioinformatics 35, 636–642 (2019).
Ha, S. D. et al. Transcription-dependent targeting of Hda1C to hyperactive genes mediates H4-specific deacetylation in yeast. Nat. Commun. 10, 4270 (2019).
Langmead, B. & Salzberg, S. L. Fast gapped-read alignment with Bowtie 2. Nat. Methods 9, 357–359 (2012).
Zhang, Y. et al. Model-based Analysis of ChIP-Seq (MACS). Genome Biol. 9, R137 (2008).
Magers, M. J., Udager, A. M. & Mehra, R. MiT family translocation-associated renal cell carcinoma: a contemporary update with emphasis on morphologic, immunophenotypic, and molecular mimics. Arch. Pathol. Lab. Med. 139, 1224–1233 (2015).
Cheng, J. et al. Computational analysis of pathological images enables a better diagnosis of TFE3 Xp11.2 translocation renal cell carcinoma. Nat. Commun. 11, 1778 (2020).
Margolin, A. A. et al. ARACNE: an algorithm for the reconstruction of gene regulatory networks in a mammalian cellular context. BMC Bioinforma. 7, S7 (2006).
Sidhar, S. The t(X;1)(p11.2;q21.2) translocation in papillary renal cell carcinoma fuses a novel gene PRCC to the TFE3 transcription factor gene. Hum. Mol. Genet. 5, 1333–1338 (1996).
Martina, J. A. et al. The nutrient-responsive transcription factor TFE3 promotes autophagy, lysosomal biogenesis, and clearance of cellular debris. Sci. Signal. 7, ra9 (2014).
Bakouny, Z. et al. Integrative clinical and molecular characterization of translocation renal cell carcinoma. Cell Rep. 38, 110190 (2022).
Sharabi, K. et al. Selective chemical inhibition of PGC-1α gluconeogenic activity ameliorates type 2 diabetes. Cell 169, 148–160.e15 (2017).
Choo, M. S. et al. Clinicopathologic characteristics and prognosis of Xp11.2 translocation renal cell carcinoma: multicenter, propensity score matching analysis. Clin. Genitourin. Cancer 15, e819–e825 (2017).
Argani, P. et al. Aberrant nuclear immunoreactivity for TFE3 in neoplasms with TFE3 gene fusions: a sensitive and specific immunohistochemical assay. Am. J. Surg. Pathol. 27, 750–761 (2003).
Lee, H. J. et al. Combination of immunohistochemistry, FISH and RT-PCR shows high incidence of Xp11 translocation RCC: comparison of three different diagnostic methods. Oncotarget 8, 30756–30765 (2017).
Liberti, M. V. & Locasale, J. W. The Warburg effect: how does it benefit cancer cells? Trends Biochem. Sci. 41, 211–218 (2016).
Škrtić, M. et al. Inhibition of mitochondrial translation as a therapeutic strategy for human acute myeloid leukemia. Cancer Cell 20, 674–688 (2011).
Damayanti, N. P. et al. Therapeutic targeting of TFE3/IRS-1/PI3K/mTOR axis in translocation renal cell carcinoma. Clin. Cancer Res. 24, 5977–5989 (2018).
Yin, X. et al. TFE3 fusions escape from controlling of mTOR signaling pathway and accumulate in the nucleus promoting genes expression in Xp11.2 translocation renal cell carcinomas. J. Exp. Clin. Cancer Res. 38, 119 (2019).
Acknowledgements
The authors thank Dr. W. Marston Linehan (National Cancer Institute, Bethesda, MD) for providing the UOK109, UOK120, UOK124, UOK145, and UOK146 cell lines. The functional part of the study was performed with the support of the Korean Basic Science Institute (C170200). The biospecimens for this study were provided by the SNUH Cancer Tissue Bank (R15-14, R16-3, R17-3, and R17-20), the SNUH Human Biobank (SNUH2017-0009, SNUH2017-0036, and SNUH2017-0046), and the Asan Bio-Resource Center (BRC-26[138]), a member of the Korea Biobank Network, which is supported by the Ministry of Health and Welfare. All samples obtained from these banking systems were obtained with informed consent following institutional review board-approved protocols.
Funding
This study was supported by grants from the SNUH Research Fund (2620150050 to CWJ), the National R&D Program for Cancer Control, Ministry of Health and Welfare, Republic of Korea (HA17C0039 to C.W.J.), and the National Research Foundation (2021R1A2C3014067 to M.C. and 2021R1A2C3008021 to S.Y.C.).
Author information
Authors and Affiliations
Contributions
C.W.J. and M.C. had full access to all of the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. Study concept and design: C.W.J. and M.C. Acquisition, analysis, or interpretation of data: C.R.L., J.S., D.J., B.Y.J., J.C., M.L., H.S., M.K., J.L., J.H.P., K.H.L., G.S.H., K.C.M., C.S., J.H.K., C.K., H.H.K. Drafting of the paper: C.R.L., J.S., J.C. Statistical analysis: C.R.L., J.S., B.Y.J., J.C., M.L., H.S. Administrative, technical, and material support: C.W.J., M.C., S.Y.C., G.S.H., K.C.M., C.S. Study supervision: C.W.J., M.C., S.Y.C.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Our study protocol was approved by the Institutional Review Boards of Seoul National University Hospital (SNUH; C-1509-031-702) and Asan Medical Center (2016-1252), tertiary referral hospitals in Korea. Written informed consent was obtained from the patients. The requirement for informed consent was waived for patients who underwent nephrectomy before February 2013 and who either died or could not be followed up with.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Consent for publication Not applicable.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, CR., Suh, J., Jang, D. et al. Comprehensive molecular characterization of TFE3-rearranged renal cell carcinoma. Exp Mol Med (2024). https://doi.org/10.1038/s12276-024-01291-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s12276-024-01291-2
- Springer Nature Limited