Abstract
Background:
Dexamethasone-phosphate (Dex-PO4) and the combination betamethasone-phosphate (Beta-PO4) + betamethasone-acetate (Beta-Ac) are the most used antenatal corticosteroids to promote fetal lung maturation. We compared fetal lung maturation induced by Beta-Ac+Beta-PO4, Dex-PO4, or Beta-PO4 alone.
Methods:
Pregnant ewes received two intramuscular doses 24 h apart of 0.25 mg/kg/dose of Beta-Ac+Beta-PO4, Dex-PO4 or Beta-PO4; or 2 doses of 0.125 mg/kg/dose of Beta-PO4 at 6, 12, or 24 h intervals. Fetuses were delivered 48 h after the first dose and ventilated for 30 min. We assessed ventilatory variables, vital signs, and blood gas. After ventilation pressure-volume curves were measured and lungs were sampled for analysis.
Results:
All treatments improved lung compliance and ventilation efficiency. Only Beta-Ac + Beta-PO4 required lower positive inspiratory pressure compared with control. Beta-Ac + Beta-PO4 and Beta-PO4 alone, but not Dex-PO4, increased the mRNA of surfactant proteins compared with control. Low-dose Beta-PO4 did not increase mRNA of surfactant proteins. There were no differences among Beta-PO4 treatment intervals.
Conclusion:
Beta-Ac + Beta-PO4 given as two doses 24 h apart was more effective in promoting fetal lung maturation than Dex-PO4 or Beta-PO4 alone, consistent with a prolonged exposure provided by the Beta-Ac + Beta-PO4. These results support the clinical use of combined Beta-Ac + Beta-PO4 preparations over phosphate corticosteroids alone for fetal lung maturation.
Similar content being viewed by others
Main
Antenatal corticosteroids decrease the incidence of respiratory distress syndrome and other neonatal morbidities in preterm infants and are considered standard of care for women at risk of preterm delivery (1). Despite widespread clinical use there is minimal experimental evidence regarding the formulation or dosing regimen, thus multiple different treatments are used worldwide (2).
Dexamethasone and betamethasone are the fluorinated steroids most commonly used for maternal treatment (2). Dexamethasone phosphate (Dex-PO4) is a short acting glucocorticoid usually given in four doses of 6 mg each, 12 h apart, for a total dose of 24 mg, but other dosing regimens are also frequently used such as two doses of 12 mg, 24 h apart. Betamethasone is usually given as a combination of equal parts betamethasone phosphate (Beta-PO4) and betamethasone acetate (Beta-Ac) in two doses 24 h apart of 12 mg each for a total dose of 24 mg. Beta-PO4 has a short biological half-life, similar to Dex-PO4, while Beta-Ac is a slow-release suspension with a longer half-life (3,4). In clinical practice, different formulations, such as Beta-PO4 alone, and dosing intervals are used despite limited data from animal or human studies (1,4).
A meta-analysis of the clinical trials comparing dexamethasone to betamethasone showed no difference in respiratory distress syndrome or neonatal mortality, but a decreased incidence of intraventricular hemorrhage (IVH) with Dex-PO4, mostly influenced by the trial from Elimian et al. (4,5). Subtil et al. compared the combination of Beta-PO4 + Beta-Ac to Beta-PO4 alone in 69 infants and observed no difference in the outcomes of neonatal death, respiratory distress syndrome, or IVH (6). A large randomized controlled trial of betamethasone combination drug vs. dexamethasone using a 2 dose 12 mg and 24-h treatment interval with long term follow up is currently underway in Australia (7).
A recent trial of antenatal corticosteroids using Dex-PO4 in low resource environments including almost 100,000 livebirths found no benefit for small infants but increased mortality for large infants exposed to prenatal Dex-PO4 (8). The ability to distinguish between treatment responses to different corticosteroids, doses, and treatment intervals is impractical given the number of variables and large number of patients needed for multiple trials. The sheep model of preterm birth and lung maturation allows the analysis of gas exchange and ventilatory variables in a stage of lung development similar to preterm newborns (9). To provide guidance about maturation responses we compared the fetal lung maturation from clinically used doses of antenatal Beta-PO4+Beta-Ac to Dex-PO4 or Beta-PO4 alone, as well as a lower dose of Beta-PO4 alone with different dosing intervals, in preterm sheep.
Methods
Antenatal Corticosteroid Treatments
The animal ethics committee of The University of Western Australia approved the animal studies (RA/3/100/1378). All animals received an i.m. injection of 150 mg medroxyprogesterone acetate (Depo-Provera, Pfizer, New York, NY) at 115 ± 1 d gestation to decrease the risk of steroid-induced premature labor. Time-mated Merino ewes with singleton fetuses received maternal i.m. injections based on maternal weight of normal saline or corticosteroid treatments with the first dose given on 120 ± 1 d of gestation (80% of gestation, term = 150 d). A composite group of control ewes received two doses of normal saline i.m. 6, 12, or 24 h apart. Treatment groups received: two doses of Beta-PO4+Beta-Ac (Celestone Chronodose, Merck Sharp & Dohme, Australia) 0.25 mg/kg/dose i.m. 24 h apart; two doses of Dex-PO4 (DBL Dexamethasone sodium phosphate, Hospira NZ, New Zealand) 0.25 mg/kg/dose i.m. 24 h apart; two doses of Beta-PO4 (Betnesol, Focus Pharmaceuticals, UK) 0.25 mg/kg/dose i.m. 24 h apart. Other groups received two doses of Beta-PO4 0.125 mg/kg/dose i.m. 6, 12, or 24 h apart. We adopted the standard dose of 0.25 mg/kg/dose of Beta-PO4 + Beta-Ac to maintain dosing regimens comparable with previous studies from our group. All animals were delivered 48 h after the first i.m. injection at 122 ± 1 d of gestation.
Ventilatory Assessment
For delivery pregnant ewes received i.v. midazolam (0.5 mg/kg) and ketamine (10 mg/kg) for sedation. Then, 3 ml of 2% (20 mg/ml) lidocaine was given for spinal anesthesia for delivery of the fetus. The head of the fetus was delivered through abdominal and uterine incisions and the fetal skin over the trachea was infiltrated with lidocaine. A 4 mm endotracheal tube was secured by tracheostomy. After delivery of the fetus the ewe was killed with pentobarbital. The lamb was weighed and dried, and temperature maintained with a radiant warmer (Cozy Cot, Fisher & Paykel Healthcare, New Zealand) and a plastic cover (Neowrap, Fisher & Paykel, NZ). Mechanical ventilation (Fabian HFO, Accutronic Medical Systems AG, Switzerland) was immediately started with the following settings: peak inspiratory pressure (PIP) of 40 cmH2O, positive end expiratory pressure (PEEP) of 5 cmH2O, respiratory rate of 50 breaths per minute, inspiratory time of 0.6 s, and 100% heated and humidified oxygen. The standard use of 100% oxygen allows the comparison of oxygenation trough the partial arterial pressure of oxygen among the groups. The umbilical artery was catheterized for blood sampling and administration of supplemental anesthesia with ketamine (5 mg/kg) if necessary. The tidal volume (VT) was continuously measured and the PIP was adjusted to keep the VT between 8.5 and 9.5 ml/kg but with a maximal pressure limited of 40 cmH2O. At 10, 20, and 30 min of ventilation we measured temperature, blood pressure, ventilator data (PIP, VT, and compliance), and performed blood gas measurements. Dynamic compliance was recorded as measured by the ventilator. The ventilation efficiency index (VEI) was calculated using the formula VEI = 3,800/(respiratory rate (PIP − PEEP) × PCo2 (mm Hg)).
Lung Assessment
After ventilation for 30 min lambs were disconnected from the ventilator and the endotracheal tube was clamped for 2 min to achieve atelectasis by oxygen absorption. The lambs received a lethal dose of pentobarbital, were weighed and the chest was opened for visual evaluation of gross lung injury–pulmonary hemorrhage, pulmonary interstitial emphysema, gas pockets within the lung or subpleural dissection—performed by the same investigator. A deflation pressure-volume curve was measured after air inflation of the lungs to a pressure of 40 cmH2O (8).
Quantitation of mRNA
Total RNA was isolated from frozen lungs after homogenization with TRIzol (Invitrogen, Carlsbad, CA). Reverse transcription was performed using Verso cDNA kit (Thermo Scientific, Waltham, MA) to produce single-strand cDNA. The genes for surfactant protein A (SPA), surfactant protein B (SPB), surfactant protein C (SPC), surfactant protein D (SPD), ATP-binding cassette subfamily A member 3 (ABCA3)——expressed by type 2 alveolar cells, and aquaporin 5 (AQP5)—expressed by type 1 alveolar cells, were amplified using the cDNA template and sheep-specific primers along with Taqman probes (Applied Biosystems, Foster City, CA). The mRNA expression for each gene was normalized to the mRNA for the ribosomal protein 18s as internal standard. Final data are expressed as fold increase over the control value.
Statistical Analysis
Data are presented as mean ± SEM. Statistical tests were performed with Prism software 6.0 (GraphPad Software, San Diego, CA). Initial comparisons were performed with ANOVA followed by multiple groups comparison with Tukey’s post-hoc test, with separate ANOVA tests performed for the comparison among Beta-PO4 + Beta-Ac, Dex-PO4, and Beta-PO4 alone, among Beta-PO4 + Beta-Ac, standard and low dose Beta-PO4, and among the low-dose Beta-PO4 intervals. Selected group comparisons were performed by t-tests where appropriate and are indicated in the results section. Significance was attributed for P-values < 0.05.
Results
Delivery Data and Animals
The number of animals, weights, sex distribution, and cord blood gas values are given in Table 1 . The group means for birth weight were lower for animals that received Beta-PO4 (P < 0.05). There were no differences between the birth weights of animals that received Beta-PO4 + Beta-Ac or Dex-PO4 compared with controls. One animal, which received two doses of 0.25 mg/kg of Beta-PO4 alone delivered prematurely and was excluded from the analysis. Two other animals in this group were in preterm labor with bulging membranes on the day of delivery. The cord blood gas measurements were similar between the groups.
Dexamethasone vs. Betamethasone 0.25 mg/kg
Vital signs, ventilatory results, and injury. Table 2 gives the blood pressures, blood gas measurements, and ventilator data at 30 min of ventilation. The diastolic, systolic, and mean blood pressures were higher in the animals treated with Beta-PO4 + Beta-Ac or Beta-PO4 alone compared with controls, while only the mean blood pressure was higher in animals exposed to Dex-PO4 compared with controls (P < 0.05). The mean pH values were higher and the mean pCO2 values were lower in the three groups compared with controls at 30 min of ventilation (P < 0.05). Animals treated with Beta-PO4 + Beta-Ac had PIP at 30 min significantly lower than control (P < 0.05), while animals treated with Beta-PO4 alone or Dex-PO4 had PIP at 30 min similar to control.
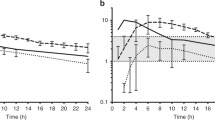
Dynamic compliance, VEI and lung gas volume at 40 cmH2O was higher in animals treated with Beta-PO4 + Beta-Ac, Beta-PO4 alone, or Dex-PO4 than the control animals (P < 0.05, Figure 1 ). There was no statistical difference in these variables among animals that received Beta-PO4 + Beta-Ac compared with Beta-PO4 alone and Dex-PO4 ( Figure 1 ). By t-test comparison between Beta-PO4 + Beta-Ac and Dex-PO4 there was a nonsignificant trend toward better volume at 40 cmH2O and VEI in the Beta-PO4 + Beta-Ac group (P = 0.09).
Physiological data after 30 min of ventilation. (a) Pressure volume curves: Deflation limbs of pressure-volume curves after 30 min of ventilation compared by ANOVA for control (♦); Beta-PO4 + Beta-Ac (▪); Dex-PO4 0.25 mg/kg (Ο); Beta-PO4 0.25 mg/kg (▯). (b) Dynamic compliance; (d) Ventilatory efficiency index (VEI) at 30 min of ventilation; (c) Volume at a pressure of 40 cmH2O (V40) after ventilation. Beta-PO4 + Beta-Ac, Beta-PO4 alone, and Dex-PO4 improved all ventilator parameters compared with control. Standard and low-dose Beta-PO4 resulted in similar improvements in lung compliance and VEI (*P < 0.05). Beta-PO4, betamethasone-phosphate; Beta-Ac, betamethasone-acetate; Dex-PO4, Dexamethasone-phosphate.
Gross lung injury—subpleural air dissection, hemorrhage, or air leak—was observed in three control animals (27%, two animals with hemorrhage and one with air leak) and four animals that received Dex-PO4 (44%, two animals with air leak and two animals with subpleural dissection) but in only one animal treated with Beta-PO4 + Beta-Ac (11%, subpleural dissection).
mRNA Quantitation
Figure 2 gives the relative mRNA quantitation for the surfactant proteins, ABCA3, and AQP5 and statistical significance by ANOVA. Beta-PO4 + Beta-Ac and Beta-PO4 alone significantly increased the mRNA level for SPA, SPB, SPC, and ABCA3 (P < 0.05). Only Beta-PO4 + Beta-Ac significantly increased the mRNA level of SPD (P < 0.05). Dex-PO4 did not significantly increase the mRNA levels of the surfactant proteins or ABCA3. Beta-PO4 + Beta-Ac, Beta-PO4 alone, and Dex-PO4 increased the mRNA levels of AQP5 compared with control (P < 0.05).
mRNA quantitation in fold change relative to control compared by ANOVA for (a) surfactant protein A (SPA); (b) surfactant protein B (SPB); (c) surfactant protein C (SPC); (d) surfactant protein D (SPD); (e) ATP-binding cassette family A member 3 (ABCA3); (f) Aquaporin 5 (AQP5). Beta-PO4 + Beta-Ac or Beta-PO4 alone significantly increased the expression of SPA, SPB, SPC, and ABCA3 (P < 0.05). Only Beta-PO4 + Beta-Ac significantly increased the expression of SPD (P < 0.05). Beta-PO4 + Beta-Ac, Beta-PO4 alone, and Dex-PO4 increased the expression of AQP5 (P < 0.05). Dexamethasone did not significantly change the expression of any surfactant proteins or ABCA3. Low-dose Beta-PO4 only increased mRNA expression AQP5 at 24 h interval (P < 0.05).
Beta-PO4 0.125 mg/kg ×2 vs. Beta-PO4 0.25 mg/kg ×2
Vital signs, ventilator results, and injury. Lambs treated with either the standard (0.25 mg/kg ×2) or the low-dose (0.125 mg/kg ×2) Beta-PO4 given 24 h apart had increased diastolic and mean blood pressure, higher pH and lower pCO2 compared with control animals ( Table 2 ) (P < 0.05). There were no vital signs differences between the standard dose and the low-dose group. There was no difference in VT, PIP, or frequency in lung injury among groups.
Dynamic compliance, VEI and volume at 40 cmH2O were higher in animals treated with Beta-PO4 either standard or low-dose compared with controls (P < 0.05, Figure 1 ). On select t-test comparison between the standard and low-dose Beta-PO4 there were no differences in those variables.
mRNA quantitation
While the standard dose of Beta-PO4 increased the mRNA expression of SPA, SPB, SPC, AQP5, and ABCA3, low-dose Beta-PO4 only significantly increased the mRNA expression of AQP5 by ANOVA ( Figure 2 ). However, t-test comparison of mRNA expression between the standard and low-dose showed no differences between the groups for expression of the biochemical markers of lung maturation.
Low-dose Betamethasone treatment intervals
Vital signs, ventilatory results, and injury. Lambs treated with low-dose Beta-PO4 alone at 12 and 24 h intervals, but not at 6-h intervals, had higher diastolic and mean blood pressures compared with controls ( Table 2 ) (P < 0.05). All groups exposed to low-dose Beta-PO4 had higher pH and lower pCO2 at 30 min of ventilation compared with controls (P < 0.05), and those values were similar among the treated groups. There was no difference in the ventilation variables compared with the control group. ( Table 2 )
Dynamic compliance, VEI and volume at 40 cmH2O were higher in animals treated with Beta-PO4 + Beta-Ac and low-dose Beta-PO4 alone compared with controls (P < 0.05, Figure 3 ). Even though the mean for these variables were higher in animals that received Beta-PO4 + Beta-Ac compared with low-dose Beta-PO4 alone, the difference was not statistically significant. ( Figure 3 ).
Physiological data after 30 min of ventilation. (a) Dynamic compliance; (b) Ventilatory efficiency index (VEI) at 30 min of ventilation; (c) Volume at a pressure of 40 cmH2O (V40) after ventilation. Comparisons performed by ANOVA with corrected multiple comparisons. Standard and low-dose resulted in similar improvement in lung mechanics (*P < 0.05).
In the 6 and 12 h dosing interval groups two animals in each group (20%) had gross lung injury (one animal with air leak and one with subpleural dissection in each group) while only one of the animals in the 24 h dosing group (petechiae) had lung injury compared with one animal (11%) on the Beta-PO4 + Beta-Ac group and three (27%) of the animals in the control group. The differences among groups were not statistically significant.
mRNA Quantitation
Figure 4 gives the relative mRNA quantitation for the surfactant proteins, ABCA3 and AQP5 and also statistical significance by ANOVA. Low dose Beta-PO4 at 6-h interval, but not at 12 or 24-h intervals, significantly increased the mRNA of SPA and SPD compared with controls (P < 0.05). Low-dose Beta-PO4 at any dosing interval did not significantly change the expression of SPB, SPC, SPD, or ABCA3. Low-dose Beta-PO4 at 24-h interval, but not at 6 or 12-h intervals, increased the expression of AQP5 (P < 0.05).
mRNA quantitation in fold change relative to control for (a) surfactant protein A (SPA); (b) surfactant protein B (SPB); (c) surfactant protein C (SPC); (d) surfactant protein D (SPD); (e) ATP-binding cassette family A member 3 (ABCA3); (f) Aquaporin 5 (AQP5). Low-dose Beta-PO4 alone only changes the expression of SPA at 6 h interval and expression of AQP5 at 24 h interval on ANOVA.
Discussion
We identified differences among clinically used corticosteroid formulations in promoting fetal lung maturation. Specifically we report the new findings that betamethasone formulations are superior to dexamethasone in increasing the mRNA expression of surfactant proteins. Despite the lack of statistical significance in lung mechanics among the formulations tested with a small number of animals per group the trend toward higher dynamic compliance, volume at 40 cmH2O, and VEI in animals exposed to Beta-PO4 + Beta-Ac could be biologically relevant in preventing need to for mechanical ventilation and lung injury, especially considering the need for lower PIP in this group.
Clinical studies did not identify consistent differences in the outcomes of preterm newborns treated antenatally with dexamethasone compared with betamethasone (2). In our study, even though dexamethasone improved dynamic lung compliance and VEI comparable to Betamethasone ( Figure 1 ), lambs that received Beta-PO4 + Beta-Ac required significantly lower PIPs after 30 min of ventilation ( Table 2 ). In preterm lambs, ventilation with a VT of 8 ml/kg increases markers of lung injury (10). Therefore the decreased pressure requirement with Beta-PO4 + Beta-Ac treatment may be relevant in preventing lung injury in ventilated preterm infants. In our study the dexamethasone group had the highest number of animals with signs of gross lung injury (44%). Treatment with two doses of 0.25 mg/kg of Beta-PO4 alone resulted in improvements in the dynamic lung compliance and VEI comparable to dexamethasone and tended to be lower than Beta-PO4 + Beta-Ac although the difference was not significant. Similarly to dexamethasone, the PIP requirement in the Beta-PO4 alone group at 30 min of ventilation to maintain a VT of 8.5 ml/kg was not different from control. Even though paO2 was measured it is not an adequate marker of lung maturation due to the presence of an open ductus arteriosus with variation in size and directions of shunting among animals.
The fact that dexamethasone did not significantly increase the mRNA levels of the surfactant proteins or ABCA3 while a similar total steroid dose of Beta-PO4 + Beta-Ac or Beta-PO4 alone increased the mRNA levels by two to threefold may be of clinical significance. Since the regulation of surfactant proteins A and B is mostly pretranslational (11), the lack of increase in SPA and SPB mRNA by dexamethasone likely results in lower surfactant protein pool compared with treatment with betamethasone and contributes to the higher PIP requirement and trend toward lower dynamic and static compliance and VEI observed with dexamethasone. A similar dose of Beta-PO4 alone resulted in significant increases in the mRNA levels of SPA, SPB, SPC, and ABCA3 to levels similar to those observed with Beta-PO4 + Beta-Ac. This is particularly interesting given the fact that Dex-PO4 and Beta-PO4 have similar structure and pharmacological properties but different effects on the biochemical maturation of the fetal lung.
Besides inducing lung maturation, glucocorticoids affect multiple systems, which were not evaluated in this study. Studies comparing the side effects of antenatal dexamethasone vs. betamethasone have yielded conflicting results. Animal studies have suggested that antenatal dexamethasone was associated with developmental delay and altered neurobehavioral performance compared with betamethasone (12). In one retrospective study betamethasone has been associated with decreased risk of periventricular leukomalacia among very low birth weight infants (13), while in a randomized trial dexamethasone was associated with decreased incidence of IVH (5). While it is not clear whether one of the formulations is associated with decreased adverse effects, repeated doses have been associated with decreased birth weight (14) and decreased head circumference (15) and are likely not beneficial (16). Hence, limiting exposure to antenatal corticosteroids may prevent adverse growth and neurological outcomes.
Given the safety concerns with repeated exposures, we asked if a lower dose of Beta-PO4 alone that had the same amount of Beta-PO4 as in the Beta-PO4 + Beta-Ac combination would induce similar fetal lung maturation. Previous work has demonstrated that a single dose of 0.5 or 0.25 mg/kg of Beta-PO4 did not induce fetal lung maturation (17). Hence, we administered a two dose regimen of 0.125 mg/kg/dose for a total Beta-PO4 dose of 0.25 mg/kg at different dosing intervals. Low-dose Beta-PO4 given as 2 doses improved dynamic and static lung compliance, and VEI, compared with control. Interestingly, the compliance, VEI and V40 values observed with the low dose Beta-PO4 were essentially the same as the ones observed with the higher dose of Beta-PO4 alone. On the other hand the low dose Beta-PO4 did not change the expression of surfactant proteins at any dosing interval compared with controls. The fact that we observed an improvement in lung static and dynamic compliance without change in the mRNA for surfactant proteins in the low dose Beta-PO4 group suggests that the lung maturation observed during ventilation with the lower doses in our study may be more related to structural lung maturation rather than biochemical changes in surfactant production and tissue water balance.
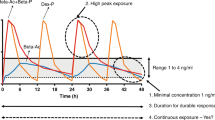
Pharmacokinetics studies can contribute to our understanding of the differences among glucocorticoid formulations in inducing lung maturation. In pregnant sheep, a 0.17 mg/kg dose of i.m. Beta-PO4 + Beta-Ac or Beta-PO4 result in a fetal plasma peak of 12 ng/ml at 3–4 h with detectable betamethasone levels for up to 12 h (18). In a previous study, we demonstrated that after a single maternal dose of 0.5 mg/kg of Beta-PO4 + Beta-Ac, the peak of Beta in the fetal plasma is ~15 ng/ml at 1.5 h which becomes undetectable after 24 h. On the other hand, a 0.25 mg/kg i.m. dose of Beta-Ac alone results in a maternal peak of 6–9 h and very low (2.4 μg/ml) to undetectable fetal levels of Beta (9).
Despite the undetectable fetal levels, a single 0.5 mg/kg dose of Beta-Ac improves lung compliance and surfactant protein mRNA expression. On the other hand, a single 0.5 mg/kg dose of Beta-PO4, which produces a higher fetal peak level than Beta-Ac, does not improve lung compliance or surfactant mRNA expression (9). In this study, we demonstrated that two doses of 0.25 mg/kg of either Beta-PO4 or Dex-PO4 improves lung compliance, albeit not to the same degree as the Beta-PO4 + Beta-Ac formulation, and are less effective in increased surfactant mRNA expression. These data suggest that a lower and prolonged fetal exposure to corticosteroids is more effective in inducing fetal lung maturation than higher peaks with a shorter exposure. This strategy may also result in a decreased total dose of antenatal corticosteroids, thereby limiting possible side effects.
In summary, the combination of Beta-PO4 + Beta-Ac was superior to DexPO4 or Beta-PO4 alone at promoting biochemical and mechanical fetal lung maturation. These results are relevant since the 0.25 mg/kg dose of Dex-PO4 and of Beta-PO4 alone result in similar total corticosteroid exposure of the fetus as treatment with Beta-PO4+Beta-Ac (4). However, the short acting steroids cause high fetal blood levels of free Beta or Dex that have no physiological benefit. In fact the lower PIP requirement and trend toward better compliance and VEI, as well the increased expression of surfactant proteins in lambs exposed to Beta-PO4+Beta-Ac suggest an advantage of this treatment over the soluble steroids alone.
Statement of Financial Support
This work was funded by the Division of Neonatology and Pulmonary Biology, Cincinnati Children’s Hospital Medical Center.
Disclosure
The authors have no conflicts of interest.
References
Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev 2006; 3:CD004454.
Brownfoot FC, Gagliardi DI, Bain E, Middleton P, Crowther CA. Different corticosteroids and regimens for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev 2013; 8:CD006764.
Gilstrap LC, Christensen R, Clewell WH, et al. Effect of corticosteroids for fetal maturation on perinatal outcomes: NIH consensus development panel on the effect of corticosteroids for fetal maturation on perinatal outcomes. JAMA 1995; 273:413–418.
Jobe AH, Soll RF. Choice and dose of corticosteroid for antenatal treatments. Am J Obstet Gynecol 2004;190:878–81.
Elimian A, Garry D, Figueroa R, et al. ‘Betacode Trial’ antenatal betamethasone compared to dexamethasone: a randomized controlled trial. Obstet Gynecol 2007;110:26–30.
Subtil D, Tiberghien P, Devos P, et al. Immediate and delayed effects of antenatal corticosteroids on fetal heart rate: a randomized trial that compares betamethasone acetate and phosphate, betamethasone phosphate, and dexamethasone. Am J Obstet Gynecol 2003;188:524–31.
Crowther CA, Harding JE, Middleton PF, Andersen CC, Ashwood P, Robinson JS ; A*STEROID Study Group. Australasian randomised trial to evaluate the role of maternal intramuscular dexamethasone versus betamethasone prior to preterm birth to increase survival free of childhood neurosensory disability (A*STEROID): study protocol. BMC Pregnancy Childbirth 2013;13:104.
Althabe F, Belizan JM, McClure EM, et al. A population-based, multifaceted strategy to implement antenatal corticosteroid treatment versus standard care for reduction of neonatal mortality due to preterm birth in low-income and middle-income countries: the ACT cluster-randomised trial. Lancet 2015;385:400–412.
Jobe AH, Nitsos I, Pillow JJ, Polglase GR, Kallapur SG, Newnham JP. Betamethasone dose and formulation for induced lung maturation in fetal sheep. Am J Obstet Gynecol 2009;201:611.e1–7.
Polglase GR, Hillman NH, Pillow JJ, et al. Positive end-expiratory pressure and tidal volume during initial ventilation of preterm lambs. Pediatr Res 2008;64:517–22.
Tan RC, Ikegami M, Jobe AH, Yao LY, Possmayer F, Ballard PL. Developmental and glucocorticoid regulation of surfactant protein mRNAs in preterm lambs. Am J Physiol 1999;277(6 Pt 1):L1142–8.
Rayburn WF, Christensen HD, Gonzalez CL. A placebo-controlled comparison between betamethasone and dexamethasone for fetal maturation: differences in neurobehavioral development of mice offspring. Am J Obstet Gynecol 1997;176:842–50; discussion 850–1.
Baud O, Foix-L’Helias L, Kaminski M, et al. Antenatal glucocorticoid treatment and cystic periventricular leukomalacia in very premature infants. N Engl J Med 1999;341:1190–6.
Crowther CA, McKinlay CJ, Middleton P, Harding JE. Repeat doses of prenatal corticosteroids for women at risk of preterm birth for improving neonatal health outcomes. Cochrane Database Syst Rev 2015;CD003935.
Hagan R, French N, Evans S. et al. Repeated antenatal corticosteroids: growth and early childhood outcomes. Pediatr Res 1997;41:405.
Guinn DA, Atkinson MW, Sullivan L, et al. Single vs weekly courses of antenatal corticosteroids for women at risk of preterm delivery: A randomized controlled trial. JAMA 2001;286:1581–7.
Jobe AH, Moss TJ, Nitsos I, Ikegami M, Kallapur SG, Newnham JP. Betamethasone for lung maturation: testing dose and formulation in fetal sheep. Am J Obstet Gynecol 2007;197:523.e1–6.
Schwab M, Coksaygan T, Samtani MN, Jusko WJ, Nathanielsz PW. Kinetics of betamethasone and fetal cardiovascular adverse effects in pregnant sheep after different doses. Obstet Gynecol 2006;108(3 Pt 1):617–25.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schmidt, A., Kemp, M., Kannan, P. et al. Antenatal dexamethasone vs. betamethasone dosing for lung maturation in fetal sheep. Pediatr Res 81, 496–503 (2017). https://doi.org/10.1038/pr.2016.249
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2016.249
- Springer Nature America, Inc.
This article is cited by
-
Antenatal corticosteroids: a reappraisal of the drug formulation and dose
Pediatric Research (2021)
-
Dosing and formulation of antenatal corticosteroids for fetal lung maturation and gene expression in rhesus macaques
Scientific Reports (2019)
-
Contemporary Challenges and Developments: Antenatal Corticosteroid Therapy
Current Obstetrics and Gynecology Reports (2019)