Abstract
Background:
Cerebral visual impairment (CVI) is a major cause of visual impairment, with very preterm birth/very low birth weight (VP/VLBW) being a major risk factor. There is no generally accepted definition of CVI. This study aims to investigate the usefulness of an empirically-based functional definition of CVI.
Methods:
One-hundred-five VP/VLBW children and 67 controls participated. CVI was defined after comprehensive oculomotor, visual sensory and perceptive assessment, and validated against vision problems in daily life and in terms of intellectual, behavioral, emotional and social functioning, as well as use of therapeutic services.
Results:
Twenty-four per cent of the VP/VLBW children met criteria for CVI, compared to 7% of controls (P = 0.006, OR: 3.86, 95% CI: 1.40–10.70). VP/VLBW children with CVI had lower performance IQ, but not verbal IQ, than those without CVI. Visual problems in daily life were confirmed in VP/VLBW children classified with CVI. Additionally, difficulties in behavioral and social functioning were most prominent among VP/VLBW children with CVI.
Conclusion:
In VP/VLBW children, CVI defined in terms of visual function deficits is accompanied by intellectual, behavioral, and social impairments, validating our operational definition of CVI. CVI might act as a marker for developmental problems in VP/VLBW children.
Similar content being viewed by others
Main
Cerebral visual impairment (CVI) is among the principal causes of visual impairment in children in developed countries (1,2). Typically, CVI is referred to as visual impairment due to abnormalities in the visual brain system posterior to the optic chiasm (3), i.e., visual impairment without primarily ocular pathology. Several etiologies of CVI have been recognized, including hypoxic, ischemic, and inflammatory events that disturb cerebral white matter development (4). Because of its widespread architecture, the brain’s visual system is particularly vulnerable to white matter abnormalities that may result in CVI.
CVI can manifest as visual impairment ranging from severe visual deficits to subtle visual dysfunctions that adversely impact on daily functioning (5). However, definitions of CVI vary between research groups and generally accepted diagnostic criteria are still lacking. Some authors emphasize visual perceptive deficits as defining features of CVI (3). Others acknowledge visual sensory deficits may also result from cerebral pathology (4,6). Particularly dorsal stream functioning is found affected in children with visual dysfunctions in a range of developmental disorders (7), referring to disrupted functioning of occipital-parietal-frontal neural networks, that host motion and orientation processing (8). However, there exists continuous interaction between the dorsal stream and occipital-temporal networks (ventral stream) that serve object perception (7,8). Furthermore, also spatial attention relies on dorsal stream functioning and critically interferes with vision, indicating that attention deficits may frequently co-occur with visual perceptive dysfunctions and warrant accurate diagnostic differentiation (9).
Very preterm birth is a major risk factor for CVI (10). Visual sensory (11,12) and perceptive (13) dysfunctions are frequently observed in very preterm children, also in those without retinopathy of prematurity (14). These visual dysfunctions most likely result from widespread white matter pathology that also involves the visual system (15). However, routine imaging procedures do not allow to accurately differentiate between injury to visual and nonvisual cerebral structures. Defining and studying CVI in terms of functional measures opens opportunities for accurate diagnostic procedures.
In this study, we advocate a broad, empirically-based definition of CVI, capitalizing on any deficit arising from central as well as peripheral neural parts of the visual system. The aims of this study were to (i) define CVI in terms of deficits in visual functioning in a representative cohort of very preterm born children, (ii) investigate the validity of this definition against vision-related problems in daily life and in terms of intellectual, as well as behavioral and emotional functioning and therapeutic needs.
Results
CVI Classification
A sample of 105 VP/VLBW very preterm (<32 wk of gestation)/very-low-birth-weight children (birth weight <1,500 g; VP/VLBW) and 67 term born children participated in this study ( Table 1 ). Overall, 25 (24%) VP/VLBW children met criteria for CVI, compared to 5 term children (P = 0.006, OR: 3.86, 95% CI: 1.40–10.70), including deficits in oculomotor (7%), visual sensory (13%), and/or visual perceptive functioning (15%). Term children met CVI criteria based on cut-off criteria (weakest performing 5% of term controls) and were excluded from further analyses, leaving three groups: VP/VLBW children with CVI (n = 25), VP/VLBW (n = 80), and term children (n = 62) without CVI. These groups were not different in terms of age at assessment (P = 0.40), level of parental education (P = 0.38), and gender (P = 0.82). VP/VLBW children with CVI had a lower mean birth weight (P = 0.02, d = 0.61) than VP/VLBW children without CVI. In addition, VP/VLBW children with CVI more often tended to have had complicated neonatal histories including respiratory support, septic events, and oxygen dependence (P ≤ 0.10). VP/VLBW children with and without CVI did not differ in terms of mild and severe ultrasound abnormalities (28 vs. 30%, and 8 vs. 5%, respectively). Table 2 details criteria for visual deficits. Table 3 summarizes the visual deficits of VP/VLBW children with CVI and illustrates the variability in number and combinations of deficits across cases.
CVI Inventory
Table 4 depicts parent-reported vision-related problems on the CVI Inventory. The highest mean scores, indicating worse abilities, are reported for VP/VLBW children with CVI, whereas scores of VP/VLBW and term control children without CVI are comparable. Main effects of group were found for all scales and the total score of the CVI Inventory (P values < 0.05). Post hoc group comparisons revealed that VP/VLBW with CVI obtained higher mean CVI total scores (P = 0.015; d = 0.97), compared to VP/VLBW and term children without CVI. More difficulties in VP/VLBW children with CVI were found for visual field/attention (P = 0.017; d = 0.93), and recognition and navigation (P = 0.04; d = 0.86), compared to VP/VLBW without CVI. No differences were found between VP/VLBW and term children without CVI, suggesting that vision-related problems as captured by the CVI inventory are associated with CVI instead of VP/VLBW-status.
Association Between CVI and Visual Attention Functioning
For attention network efficiency, a main effect of group was found for the executive attention error rate only (P < 0.001). Post hoc group comparisons revealed higher mean error rates for executive attention in VP/VLBW children with and without CVI, relative to term controls (d = 0.93 and d = 0.54, respectively, P values < 0.01), but no difference between VP/VLBW children with and without CVI was found (d = 0.27, P = 0.46).
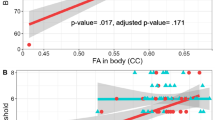
For the visual search task, a main effect of group was obtained for mean search time per target (P = 0.001) and error rate (P = 0.005). Post hoc group comparisons indicated an increased mean search time per target in VP/VLBW children with CVI, as compared to VP/VLBW children without CVI (d = 0.78, P = 0.001) and term controls (d = 0.92, P < 0.001). Mean error rate was increased in VP/VLBW children with CVI as compared to term controls only (d = 0.77, P = 0.01). Results for the two measures of attention functioning indicate that CVI-status is associated with deficits in selective attention, as indicated by the visual search task, but not with attention network efficiency ( Figure 1 ).
Intelligence (panel a), visual search performance (panel b), and attention network efficiency in terms of mean reaction time (panel c), and error rate (panel d) of very preterm birth/very low birth weight (VP/VLBW) children with cerebral visual impairment (CVI) (white bars), VP/VLBW children without CVI (black bars), and term children without CVI (gray bars). Results are shown as mean (SE) using normalized data; RT indicates reaction time; *P < 0.05, **P < 0.01, †P < 0.001.
After entering search time per target and error rate as covariates in the analyses investigating group differences on the CVI Inventory scales, the main effects of group for perception of movement (P = 0.07), visual search (P = 0.07), guidance of movement (P = 0.14), and attention (P = 0.15) disappeared. Across CVI inventory scales, however, differences in means between VP/VLBW children with and without CVI shifted from 0.58–0.97 SD to 0.41–0.82 SD, indicating that these differences were largely independent of attention functioning.
Intellectual, Behavioral, and Emotional Correlates of CVI
Table 4 depicts the IQ indices, as well as the results of the Strengths and Difficulties Questionnaire (SDQ) and the Children’s Social Behavior Questionnaire (CBSQ) measuring behavioral and emotional, as well as social functioning, respectively. Main effects of group were found for verbal as well as performance IQ (P values < 0.001). Post hoc group comparisons indicated that mean performance IQ was lower in VP/VLBW children with and without CVI as compared to controls (P values < 0.01), and was lower in VP/VLBW children with CVI, as compared to VP/VLBW without CVI (P = 0.027; d = 0.54). Mean verbal IQ was lower in VP/VLBW children with and without CVI compared to controls (P values < 0.01), but did not differ between VP/VLBW children with and without CVI (P = 0.38; d = 0.34).
For the behavioral and emotional measures, higher mean scores, indicating more problems, are more prominent among VP/VLBW children with CVI, than in VP/VLBW children and term controls without CVI ( Table 4 ). For the SDQ, main effects of group were found for total difficulties, emotional symptoms, hyperactivity/inattention, and prosocial behavior scores (P values < 0.05). Post hoc group comparisons revealed higher mean scores on SDQ total difficulties in VP/VLBW children with CVI than in term controls (P = 0.017; d = 0.86) and less prosocial behavior among VP/VLBW children with CVI than in VP/VLBW children without CVI (P = 0.01, d = 0.76), indicating worse social skills in VP/VLBW children with CVI, compared to VP/VLBW and term children without CVI.
Main effects of group were found for the Children’s Social Behavior Questionnaire (CSBQ) Total Score and the scales reduced contact/social interest, understanding social information, stereotyped behavior, and fear of and resistance to change (P values <0.05). Post hoc group comparisons revealed higher mean scores on the scales reduced contact/social interest and fear of and resistance to change among VP/VLBW children with CVI than among VP/VLBW children without CVI (P = 0.04, d = 0.74 and P = 0.03, d = 0.84, respectively). Stereotyped behavior was more prevalent among VP/VLBW with and without CVI, compared to term controls (P = .008, d = 0.98 and P = 0.02, d = 0.48, respectively). These results indicate that adapting to and interacting with the social environment, but not displaying stereotyped behavior, are associated with CVI-status instead of VP/VLBW-status.
Use of Therapeutic Services
Ten (40%) VP/VLBW with CVI and 26 (33%) VP/VLBW children without CVI were supported by or were referred to therapeutic services (P = 0.49). These 36 children needed additional support in regular education or attending special education (13%), physiotherapy (20%), speech therapy (19%), occupational therapy (8%), and/or psychotherapy (3%). Remarkably, none of the participating children was referred to visual rehabilitation.
Uncorrected Refractive Errors and Nesting Effects
All analyses were repeated without children suspected of uncorrected refractive errors, and were repeated with only one, randomly selected multiplet member. These corrections for potential biases left the results essentially unchanged.
Discussion
Since generally accepted diagnostic criteria for CVI are still lacking, this study set out to classify CVI according to empirically-based operational criteria and aimed to investigate its concurrent validity against a commonly used CVI questionnaire. As expected, CVI was found more frequently among VP/VLBW children than among controls. CVI-status was specifically accompanied by medium to large sized increases in parent-reported vision-related problems on the CVI Inventory, supporting the concurrent validity of our CVI concept. Other studies using different approaches found similar results in very preterm born children and among children referred to a CVI clinic (16,17). In addition, parent-reported vision-related problems in VP/VLBW children with CVI remained largely present irrespective of selective and executive attention abilities, indicating that these visual problems exist independent of attention problems of very preterm born children (18).
The criterion validity of the CVI classification was evaluated against measures for attention, intellectual, behavioral and emotional functioning, and therapeutic needs. CVI-status was associated with attention dysfunctions in terms of impaired visual search performance. Performance IQ, but not verbal IQ, was lower in VP/VLBW children with CVI, consistent with previous analyses in our sample that showed that visual perceptive functioning is especially associated with Performance IQ (19). In addition, CVI-status was associated with medium to large sized increases in behavioral (SDQ total difficulties) and social (CSBQ total score) difficulties, suggesting that the frequently reported increased susceptibility of VP/VLBW children for autism spectrum disorders (20) may specifically coincide with CVI. In contrast, no differences in referrals to therapeutic services between VP/VLBW children with and without CVI were found, including no referrals to visual rehabilitation services. To summarize, CVI-status seems a sensitive indicator for lower performance IQ and atypical behavioral and social development of VP/VLBW children.
The functional empirical approach of this study, defining CVI in terms of visual deficits, was taken to advance definition and extend understanding of CVI. Interestingly, the criterion-related validity indicates that our CVI classification identifies VP/VLBW children that also display a range of intellectual, behavioral as well as social communication and interaction disadvantages, that are frequently found in VP/VLBW children (21). Similarly, the clustering of intellectual and behavioral disadvantages in our VP/VLBW children with CVI confirms the finding indicating that neurodevelopmental disadvantages in VP/VLBW children often occur across multiple domains of functioning (22). In addition, lower birth weight and increases in respiratory and septic adversities of the VP/VLBW children with CVI suggests that these children appear the subgroup that survived the most serious perinatal complications. No evidence was found, however, for increased use of therapeutic services at this age, but VP/VLBW children classified as CVI may be those children at risk for future difficulties in behavioral functioning or academic achievement. Notably, none of the VP/VLBW children with CVI was referred for visual rehabilitation. Most likely, CVI in our sample was not the principal dysfunction in these children’s neurodevelopmental weaknesses, illustrating that VP/VLBW children typically show developmental disadvantages across multiple domains of functioning (22). In addition, with advances in medicine, white matter abnormalities have become less widespread and severe (23), which in turn might have resulted in a concomitant decrease of (severe) CVI. Our finding contrasts assumed visual rehabilitation needs for VP/VLBW children with CVI (16). Although the lack of visual service use might also reflect unmet needs, referrals to visual rehabilitation were not restricted by narrow acceptance criteria.
Our functional approach to defining CVI included any oculomotor, visual sensory, and perceptive deficit arising from cerebral abnormalities, thereby extending the range of deficits in conventional definitions of CVI (3,5,6). Our approach incorporates recent insights indicating that also “sensory” functions of binocular vision such as stereopsis have their cerebral underpinnings (24). Consequently, CVI becomes a broad umbrella term that includes a wide range of visual deficits. The large variety of deficits and combinations of deficits observed in our sample, emphasizes the need to distinguish subgroups of children with CVI that respond to different forms of treatment. Furthermore, our approach does not exclude neuroimaging techniques as future diagnostic tools for CVI. Diffusion tensor imaging studies illustrate the role of integrity of the optic tract in visual functioning in very preterm infants’ visual fixation ability (25), oculomotor functioning and visual acuity (26), as well as the role of optic radiation integrity in visual acuity and visual perceptive functioning in childhood (27), and the role of callosal and frontal white matter integrity in visual acuity during adolescence (28). However, studies have not tapped into the role of specific other tracts of the neural network underlying vision in very preterm children so far, and, given the comorbidity of CVI and intellectual and behavioral dysfunctions, advances in diagnostic neuroimaging procedures are warranted to successfully identify CVI.
This study has some limitations. Our CVI classification was primarily established to study its utility. Although this approach proved fruitful in differentiating VP/VLBW children with and without neurodevelopmental adversities, results should, at this point, not be taken as a diagnostic guideline. Next, although our and earlier findings (16) may support the concurrent validity of the CVI Inventory, it should be noted that its validity has not been studied so far. However, the CVI Inventory is the first and best described questionnaire to gather behavioral evidence of CVI. Referrals for therapeutic services were based on multidisciplinary clinical decision making without a standardized procedure. Furthermore, although our approach provides clear-cut criteria for CVI, differentiating between neurological and non-neurological causes of visual deficits remains difficult in some cases. No cerebral imaging data at follow-up were available that would have enabled us to elucidate the neural correlates of CVI in our sample.
In conclusion, we found evidence that CVI in terms of visual function deficits is specifically associated with vision-related problems in daily life, largely independent of attention functioning. In addition, CVI was associated with poorer performance IQ, and with behavioral and emotional problems, highlighting their comorbidity and calling for differential diagnostic guidelines. Clinicians should be aware that CVI, as well as its behavioral characteristics, emerge within a wider cluster of neurocognitive and behavioral problems and, therefore, should follow adequate differential diagnostic procedures in order to select sensible treatment options. Longitudinal studies of CVI are necessary to investigate whether CVI in early childhood is a general precursor of adverse developmental outcome, or identifies those children with lasting visual deficits and needs for visual rehabilitation, thereby also addressing the question whether visual training programs would be beneficial to VP/VLBW children with CVI.
Methods
Participants
All VP/VLBW children originally participated in a multicenter randomized controlled trial comparing a home-based intervention and care as usual (29). Exclusion criteria at study entry were severe congenital abnormalities, severe maternal physical or mental conditions, not mastering the Dutch language and unavailability of an interpreter, and participation in other trials on postdischarge management (29). At 5.5 y corrected age 160 of 176 children participating in the trial were available for follow-up, of whom 136 (77%) agreed to participate and 105 successfully completed the assessments. Of the 31 children excluded, data were (partially) missing due to developmental delay or behavioral problems that crucially interfered with task execution (n = 8), declined participation in the second assessment day (n = 5), time constraints (n = 12), and technical problems (n = 6). Participating (n = 105) and nonparticipating children (n = 71) did not differ in terms of characteristics at discharge (P values > 0.05), except that nonparticipating children more often lived in single parent households (9 and 21%, respectively, P = 0.02) and families speaking a non-Dutch primary language (10 and 33%, respectively, P = 0.02). No differences on any dependent variable were found between VP/VLBW intervention (n = 57) and VP/VLBW care as usual children (n = 48), P values > 0.05, except for small sized differences on the CVI Inventory scales visual field/attention and guidance of movement, and the CSBQ scale stereotyped behavior (P values < 0.05, d < 0.43), favoring VP/VLBW intervention compared to VP/VLBW care as usual children. Because no intervention-status by CVI-status interactions were present (p values > 0.15) and because repeating all other analyses without VP/VLBW intervention children left the results essentially unchanged, the total VP/VLBW sample was analyzed regardless of intervention status in all analyses.
Term born controls (n = 67) were recruited from regular schools attended by the VP/VLBW children (n = 29) and additional schools located in the same geographical area (n = 38). Controls were included if they had a GA >37 wk and BW >2,500 g. Exclusion criteria were parent reported severe perinatal complications or illnesses that might interfere with normal brain development, and learning difficulties. Perinatal risk factors were taken from the medical records at discharge for VP/VLBW children and reported by parents for term controls. Socio-demographic data were obtained using a custom made questionnaire at the 5.5-y assessment. The measure of parental education was derived from the number of years postelementary education of both parents and classified as high (either parent >8 y), middle (both parents 6–8 y) or low (either parent <6 y) (22).
Measures
Measures used to define CVI
Visual assessment. Comprehensive assessment of visual functioning included measures of refraction, oculomotor functioning (eye alignment, motility, convergence, nystagmus, torticollis), visual sensory functioning (visual acuity, visual field, contrast sensitivity, stereovision, color vision), and perceptive functioning (static and motion visual coherence, position in space, figure-ground, visual closure, form constancy, and face recognition) and has been described in detail elsewhere (19). Criteria for oculomotor and visual sensory deficits were derived from large and representative samples of typically developing children (30,31,32,33). Visual perceptive deficits were defined as performance equaling the weakest 5% performing term controls, for measures that differentiated between VP/VLBW and control children (detailed in Table 2 ). Deficits on any measure of the visual assessment were classified as CVI, excluding those deficits that were likely due to uncorrected refractive errors. Children with deficient eye alignment, visual acuity, and/or stereovision accompanied by uncorrected refractive errors were not classified as CVI, to minimize the possibility that CVI would result from nonretinal ocular conditions.
Measures used to validate CVI
CVI inventory. The CVI inventory identifies typical behavioral features of CVI and comprises seven scales and allows calculation of a total score (34). The scales refer to problems in activities involving visual field/attention, perception of movement, visual search, guidance of movement, attention, crowded scenes, and recognition and navigation, with higher scores indicating worse visual abilities.
Visual attention assessment. Visual attention functioning was assessed using a child friendly adaptation of the Attention Network Test and a visual search task, and has been described in detail elsewhere (35). Briefly, the Attention Network Test required children to respond to a target image that was presented on a computer screen by pressing the left or right button, corresponding to the target location. There were four types of trials: trials with no cues, neutral cues, directional cues, or incongruent cues. Attention network indices were calculated as differences in mean reaction time and error rate between no cue and neutral cue trials (assessing alerting attention), neutral and directional cue trials (assessing orienting attention) and neutral and incongruent cue trials (assessing executive attention). Differences in mean reaction time and error rate for each attention network index were used as dependent variables in the analyses, with larger differences indicating higher efficiency of alerting and orienting networks and lower executive network efficiency. The visual search task required children to point to target images, presented among distractor images, on a touch screen monitor. Search time per target (total search time divided by the number of correctly identified targets) and error rate (percentage of incorrectly identified and missed targets) were used as dependent variables in the analyses, with longer search time and higher error rate reflecting worse performance.
Intelligence. Intellectual functioning was measured using a short form of the Wechsler Preschool and Primary Scale of Intelligence (WPPSI-III), comprising an estimated Verbal IQ (subtests Information and Vocabulary) and Performance IQ (subtests Block Design and Matrix Reasoning) (36). These estimates correlate >.90 with Verbal and Performance IQ obtained from the full scale assessment in VP/VLBW children (37).
Behavioral and emotional functioning. The SDQ measures emotional symptoms, conduct problems, hyperactivitiy/inattention, peer problems, prosocial behavior, and calculates a Total Difficulties score (38). Higher ratings correspond to more behavioral or emotional problems, except for the Prosocial Behavior scale, where higher scores indicate more prosocial behavior.
The CSBQ captures problems in social communication and interaction (39). The CSBQ comprises 6 factors: Tuned to Social Situation, Reduced Contact/Social Interest, Orientation Problems, Understanding Social Information, Stereotyped Behavior, Fear of and Resistance to Change, and a Total Score. Higher scores indicate more social behavioral problems.
Therapeutic services. The use of therapeutic services was defined as any treatment by a physiotherapist, speech therapist, occupational therapist, child psychologist/psychiatrist, including current therapies and referrals for treatment based on a comprehensive assessment, of which the current study was part. Educational support included remedial teaching or in-class support by a teaching assistant in regular education, and attending special education.
Procedure
All VP/VLBW children were invited for follow-up assessment at 5.5 y corrected age. Teachers were asked to distribute invitation letters to parents of all term control children. All tasks were performed in one of two counterbalanced fixed orders (randomly assigned to participating children) and were completed on 2 separate days to avoid fatigue. Questionnaires were completed by parents during the assessments, or at home.
Tests were administered by trained researchers using standardized instructions. Refractive status, oculomotor and visual sensory functioning was assessed by trained orthopthists. Computerized tasks were performed on a Dell Optiplex 2.8 GHz desktop computer using E-Prime 2.0 software (Psychology Software Tools, Pittsburgh, PA). The study protocol was approved by the Medical Ethics Committee of the Academic Medical Center Amsterdam, and all parents signed informed consent.
Statistical Analyses
All analyses were performed using SPSS 21.0 (IBM, Armonk, NY). Prior to analyzing the VP/VLBW sample collectively, possible effects of the postdischarge intervention on all dependent variables were assessed using independent samples t-tests, and by repeating all analyses without VP/VLBW intervention children. Dependent variables derived from the CVI Inventory, Attention Network Test, visual search task, IQ measures, SDQ and CSBQ were subjected to Analyses of Variance with group (three levels: VP/VLBW children with CVI, and VP/VLBW and term children without CVI) as between-subject factor. When a main effect of group was obtained, group differences were assessed using Games-Howell post hoc comparisons, controlling the overall α at 0.05 and adjusting for unequal variances and sample sizes across groups. Visual attention measures that differed between groups were inserted as covariates in the analyses studying group differences on the CVI Inventory to investigate if attention abilities could account for these group differences. The association between CVI-status and therapeutic services was investigated using χ2 tests. Because there were 12 twins and two sets of triplets in the VP/VLBW group, analyses were repeated with only one, randomly selected, multiplet member. In all analyses, α was set at 0.05 and significance testing was two-sided. Effect sizes were calculated in terms of standardized mean differences (Cohen’s d) with 0.20, 0.50, and 0.80 referring to small, medium and large effects, respectively (40).
Statement of Financial Support
This research was supported by a grant from the Novum Foundation, Huizen, The Netherlands, a non-profit organization providing financial support to (research) projects that improve the quality of life of individuals with visual impairment (www.stichtingnovum.org). The study sponsor had no involvement study design, data collection and analysis, manuscript preparation, and the decision to submit the paper for publication.
Disclosure
None of the authors has an interest that might be perceived as posing a conflict or bias.
References
Hatton DD, Schwietz E, Boyer B, Rychwalski P. Babies Count: the national registry for children with visual impairments, birth to 3 years. J AAPOS 2007;11:351–5.
Rahi JS, Cable N ; British Childhood Visual Impairment Study Group. Severe visual impairment and blindness in children in the UK. Lancet 2003;362:1359–65.
Good WV, Jan JE, DeSa L, Barkovich AJ, Groenveld M, Hoyt CS. Cortical visual impairment in children. Surv Ophthalmol 1994;38:351–64.
Dutton GN, Jacobson LK. Cerebral visual impairment in children. Semin Neonatol 2001;6:477–85.
Edmond JC, Foroozan R. Cortical visual impairment in children. Curr Opin Ophthalmol 2006;17:509–12.
Fazzi E, Signorini SG, Bova SM, et al. Spectrum of visual disorders in children with cerebral visual impairment. J Child Neurol 2007;22:294–301.
Braddick O, Atkinson J, Wattam-Bell J. Normal and anomalous development of visual motion processing: motion coherence and ‘dorsal-stream vulnerability’. Neuropsychologia 2003;41:1769–84.
Kravitz DJ, Saleem KS, Baker CI, Mishkin M. A new neural framework for visuospatial processing. Nat Rev Neurosci 2011;12:217–30.
Atkinson J, Braddick O. Visual attention in the first years: typical development and developmental disorders. Dev Med Child Neurol 2012;54:589–95.
Khetpal V, Donahue SP. Cortical visual impairment: etiology, associated findings, and prognosis in a tertiary care setting. J AAPOS 2007;11:235–9.
Cooke RW, Foulder-Hughes L, Newsham D, Clarke D. Ophthalmic impairment at 7 years of age in children born very preterm. Arch Dis Child Fetal Neonatal Ed 2004;89:F249–53.
Jongmans M, Mercuri E, Henderson S, de Vries L, Sonksen P, Dubowitz L. Visual function of prematurely born children with and without perceptual-motor difficulties. Early Hum Dev 1996;45:73–82.
Geldof CJ, van Wassenaer AG, de Kieviet JF, Kok JH, Oosterlaan J. Visual perception and visual-motor integration in very preterm and/or very low birth weight children: a meta-analysis. Res Dev Disabil 2012;33:726–36.
O’Connor AR, Stephenson T, Johnson A, et al. Long-term ophthalmic outcome of low birth weight children with and without retinopathy of prematurity. Pediatrics 2002;109:12–8.
Volpe JJ. Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol 2009;8:110–24.
Macintyre-Béon C, Young D, Dutton GN, et al. Cerebral visual dysfunction in prematurely born children attending mainstream school. Doc Ophthalmol 2013;127:89–102.
Ortibus E, Laenen A, Verhoeven J, et al. Screening for cerebral visual impairment: value of a CVI questionnaire. Neuropediatrics 2011;42:138–47.
de Kieviet JF, van Elburg RM, Lafeber HN, Oosterlaan J. Attention problems of very preterm children compared with age-matched term controls at school-age. J Pediatr 2012;161:824–9.
Geldof CJ, Oosterlaan J, Vuijk PJ, de Vries MJ, Kok JH, van Wassenaer-Leemhuis AG. Visual sensory and perceptive functioning in 5-year-old very preterm/very-low-birthweight children. Dev Med Child Neurol 2014;56:862–8.
Leavey A, Zwaigenbaum L, Heavner K, Burstyn I. Gestational age at birth and risk of autism spectrum disorders in Alberta, Canada. J Pediatr 2013;162:361–8.
Aarnoudse-Moens CS, Weisglas-Kuperus N, van Goudoever JB, Oosterlaan J. Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics 2009;124:717–28.
Potharst ES, van Wassenaer AG, Houtzager BA, van Hus JW, Last BF, Kok JH. High incidence of multi-domain disabilities in very preterm children at five years of age. J Pediatr 2011;159:79–85.
van Haastert IC, Groenendaal F, Uiterwaal CS, et al. Decreasing incidence and severity of cerebral palsy in prematurely born children. J Pediatr 2011;159:86–91.e1.
Joly O, Frankó E. Neuroimaging of amblyopia and binocular vision: a review. Front Integr Neurosci 2014;8:62.
Berman JI, Glass HC, Miller SP, et al. Quantitative fiber tracking analysis of the optic radiation correlated with visual performance in premature newborns. AJNR Am J Neuroradiol 2009;30:120–4.
Groppo M, Ricci D, Bassi L, et al. Development of the optic radiations and visual function after premature birth. Cortex 2014;56:30–7.
Thompson DK, Thai D, Kelly CE, et al. Alterations in the optic radiations of very preterm children-Perinatal predictors and relationships with visual outcomes. Neuroimage Clin 2014;4:145–53.
Lindqvist S, Skranes J, Eikenes L, et al. Visual function and white matter microstructure in very-low-birth-weight (VLBW) adolescents–a DTI study. Vision Res 2011;51:2063–70.
Koldewijn K, Wolf MJ, van Wassenaer A, et al. The Infant Behavioral Assessment and Intervention Program for very low birth weight infants at 6 months corrected age. J Pediatr 2009;154:33–38.e2.
Robaei D, Rose K, Ojaimi E, Kifley A, Huynh S, Mitchell P. Visual acuity and the causes of visual loss in a population-based sample of 6-year-old Australian children. Ophthalmology 2005;112:1275–82.
Junghans B, Kiely PM, Crewther DP, Crewther SG. Referral rates for a functional vision screening among a large cosmopolitan sample of Australian children. Ophthalmic Physiol Opt 2002;22:10–25.
Hargadon DD, Wood J, Twelker JD, Harvey EM, Dobson V. Recognition acuity, grating acuity, contrast sensitivity, and visual fields in 6-year-old children. Arch Ophthalmol 2010;128:70–4.
Aring E, Grönlund MA, Andersson S, Hård AL, Ygge J, Hellström A. Strabismus and binocular functions in a sample of Swedish children aged 4-15 years. Strabismus 2005;13:55–61.
Macintyre-Beon C, Young D, Calvert J, Ibrahim H, Dutton GN, Bowman R. Reliability of a question inventory for structured history taking in children with cerebral visual impairment. Eye (Lond) 2012;26:1393.
Geldof CJ, de Kieviet JF, Dik M, Kok JH, van Wassenaer-Leemhuis AG, Oosterlaan J. Visual search and attention in five-year-old very preterm/very low birth weight children. Early Hum Dev 2013;89:983–8.
Sattler JM. Assessment of Children: Cognitive Applications. 4th edn. San Diego, CA: Jerome M. Sattler, Publisher, 2001.
Groth-Marnat G. Handbook of Psychological Assessment. Hoboken, NJ: John Wiley & Sons, 1997.
Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581–6.
Hartman CA, Luteijn E, Serra M, Minderaa R. Refinement of the Children’s Social Behavior Questionnaire (CSBQ): an instrument that describes the diverse problems seen in milder forms of PDD. J Autism Dev Disord 2006;36:325–42.
Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd edn. Hillsdale, NJ: Lawrence Erlbaum Associates, 1988.
Acknowledgements
We are most grateful to J Atkinson, O Braddick, and J Wattam-Bell for sharing the static and motion coherence tasks, and to GN Dutton for sharing the CVI inventory. We thank M Apeldoorn, M Meijer, and S van der Zwet-Slotemaker for conducting the orthoptic assessments. This paper builds on previously published results obtained from the same sample as the sample described in the current manuscript. Previous published results concern outcomes of the assessments of visual as well as attention functioning, which has been clearly indicated in the manuscript. The current paper reports the consequences of visual deficits in other domains of functioning. Previously published results can be found here: Geldof CJA, Oosterlaan J, de Vries MJ, Kok JH, van Wassenaer-Leemhuis AG 2014 Visual Sensory and Perceptive Functioning in Five-Year-Old Very Low Birth Weight Children. Dev Med Child Neurol 56:862–8. Geldof CJA, de Kieviet JF, Dik M, Kok JH, van Wassenaer-Leemhuis AG, Oosterlaan J 2013 Visual search and attention in five-year-old very preterm/very low birth weight children. Early Hum Dev 89:983–8.
Author information
Authors and Affiliations
Corresponding author
PowerPoint slides
Rights and permissions
About this article
Cite this article
Geldof, C., van Wassenaer-Leemhuis, A., Dik, M. et al. A functional approach to cerebral visual impairments in very preterm/very-low-birth-weight children. Pediatr Res 78, 190–197 (2015). https://doi.org/10.1038/pr.2015.83
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2015.83
- Springer Nature America, Inc.