Abstract
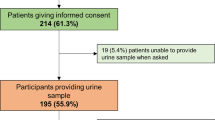
Poor adherence with pharmacotherapy is well recognised as one of the main barriers to achieving satisfactory blood pressure control, although accurately measuring patient adherence has historically been very challenging. Urine analysis by high-performance liquid chromatography-tandem mass spectrometry has recently become routinely available as a method of screening for non-adherence. In addition to measuring rates of adherence in hypertensive patients, this study aimed to investigate the reasons for non-adherence given by patients and how patients react when they are informed of their results. This was a retrospective observational study looking at results from the routine use of this assay in a specialist hypertension clinic in Birmingham, UK, in patients with uncontrolled hypertension and those under consideration for renal denervation. Out of the 131 patients analysed, only 67 (51%) were taking all their medications as prescribed. Forty-three patients (33%) were taking some of their medications, whilst 21 patients (16%) were completely non-adherent. The most common reasons cited for non-adherence were adverse effects of medication and forgetfulness. Adherence rates for thiazide/thiazide-like diuretics and spironolactone were lower than for other classes of antihypertensive drug. Despite the objective nature and high sensitivity of the test, 36% of non-adherent patients disputed the results. A minority of patients did not attend follow-up. Further research investigating the implications of a ‘non-adherence’ result on the patient-clinician relationship is required.



Similar content being viewed by others
References
Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD et al. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension 2008; 51: 1403–1419.
Yiannakopoulou ECh, Papdopulos JS, Cokkinos DV, Mountokalakis TD . Adherence to antihypertensive treatment: a critical factor for blood pressure control. Eur J Cardiovasc Prev Rehabil 2005; 12: 243–249.
Naderi SH, Bestwick JP, Wald DS . Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376 162 patients. Am J Med 2012; 125: 882–887.
Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M . Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ 2008; 336 (7653): 1114–1117.
Horne R, Weinman J, Barber N. Concordance, adherence and compliance in medicine taking. Report for the national co-ordinating centre for NHS service delivery and organisation research and development. 2005. Available from http://www.nets.nihr.ac.uk/__data/assets/pdf_file/0009/64494/FR-08-1412-076.pdf Accessed on January 2016.
Feinstein AR . On white-coat effects and the electronic monitoring of compliance. Arch Intern Med 1990; 150: 1377–1378.
Chobanian AV . Impact of nonadherence to antihypertensive therapy. Circulation 2009; 120 (16): 1558–1560.
Burnier M, Wuerzner G, Struijker-Boudier H, Urquhart J . Measuring, analyzing, and managing drug adherence in resistant hypertension. Hypertension 2013; 62: 218–225.
Tomaszewski M, White C, Patel P, Masca N, Damani R, Hepworth J et al. High rates of non-adherence to antihypertensive treatment revealed by high-pressure liquid chromatography-tandem mass spectrometry (HPLC-MS/MS) urine analysis. Heart 2014; 100 (11): 855–861.
Jung O, Gechter JL, Wunder C, Paulke A, Bartel C, Geiger H et al. Resistant hypertension? Assessment of adherence by toxicological urine analysis. J Hypertens 2013; 31 (4): 766–774.
Wright JM, Lee C, Chambers GK . Real-world effectiveness of antihypertensive drugs. CMAJ 2000; 162: 190–191.
Anderson JL, Dodman S, Kopelman M . Patient information recall in a rheumatology clinic. Rheumatol Rehabil 1979; 18 (1): 18–22.
Osterberg L, Blaschke T . Adherence to medication. N Eng J Med 2005; 353: 487–497.
Myers MG . Compliance in hypertension: why don’t patients take their pills? CMAJ 1999; 160: 64–65.
Claxton AJ, Cramer J, Pierce C . A systematic review of the associations between dose regimens and medication compliance. Clin Ther 2001; 23 (8): 1296–1310.
Schroeder K, Fahey T, Ebrahim S . Interventions for improving adherence to treatment in patients with high blood pressure in ambulatory settings. Cochrane Databse Syst Rev 2004; (2): CD004804.
Leenen FH, Wilson TW, Bolli P, Larochelle P, Myers M, Handa SP et al. Patterns of compliance with once versus twice daily antihypertensive drug therapy in primary care: a randomized clinical trial using electronic monitoring. Can J Cardiol 1997; 13 (10): 914–920.
Thom S, Poulter N, Field J, Patel A, Prabhakaran D, Stanton A et al. Effects of a fixed-dose combination strategy on adherence and risk factors in patients with or at high risk of CVD. The UMPIRE randomized clinical trial. JAMA 2013; 310 (9): 918–929.
van Servellen G, Chang B, Garcia L, Lombardi E . Individual and system level factors associated with treatment nonadherence in human immunodeficiency virus-infected men and women. AIDS Patient Care STDS 2002; 16: 269–281.
Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV . Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of the literature. J Clin Psychiatry 2002; 63: 892–909.
Pound P, Britten N, Morgan M, Yardley L, Pope C, Daker-White G et al. Resisting medicines: a synthesis of qualitative studies of medicine taking. Soc Sci Med 2005; 61 (1): 133–155.
Adams A, Uratsu C, Dyer W, Magid D, O’Connor P, Beck A et al. Health system factors and antihypertensive adherence in a racially and ethnically diverse cohort of new users. JAMA 2013; 173 (1): 54–61.
Acknowledgements
We would like to acknowledge the University of Leicester group responsible for developing the assay (Tomaszewski et al,9). We would also like to acknowledge the National Institute for Health Research (NIHR)/Wellcome Trust Birmingham Clinical Research Facility. The views expressed are those of the authors(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Journal of Human Hypertension website .
Supplementary information
Rights and permissions
About this article
Cite this article
Pucci, M., Martin, U. Detecting non-adherence by urine analysis in patients with uncontrolled hypertension: rates, reasons and reactions. J Hum Hypertens 31, 253–257 (2017). https://doi.org/10.1038/jhh.2016.69
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2016.69
- Springer Nature Limited
This article is cited by
-
The effect of combining therapeutic drug monitoring of antihypertensive drugs with personalised feedback on adherence and resistant hypertension: the (RHYME-RCT) trial protocol of a multi-centre randomised controlled trial
BMC Cardiovascular Disorders (2023)
-
Perioperative use of renin-angiotensin system inhibitors and outcomes in patients undergoing cardiac surgery
Nature Communications (2019)
-
Antihypertensive Treatment Patterns and Blood Pressure Control in Older Adults: Results from the Berlin Aging Study II
Drugs & Aging (2018)