Abstract
Background:
Roux-en-Y gastric bypass (RYGBP) is the most widely used bariatric surgery procedure, which induces profound metabolic and physiological effects, such as substantial improvements in obesity, type 2 diabetes and their comorbidities. Increasing evidence identifies bile acids (BAs) as signaling molecules that contribute to the metabolic improvement after RYGBP. However, how and to what extent BAs mediate the metabolic effects of RYGBP still remains unclear and requires mechanism of action studies using preclinical models. In this study, we compared plasma BA profiles before and after RYGBP in two animal models, rats and pigs, with humans to evaluate their translational potential.
Methods:
Plasma BAs were profiled in rats, pigs and humans by liquid chromatography coupled with tandem mass spectrometry before and after RYGBP.
Results:
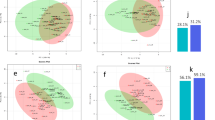
RYGBP increased baseline plasma total BA concentrations in humans and in the two animal models to a similar extent (∼3-fold increase), despite differences in presurgery BA levels and profiles between the models. However, qualitatively, RYGBP differently affected individual plasma BA species, with similar increases in some free species (cholic acid (CA), chenodeoxycholic acid (CDCA) and deoxycholic acid (DCA)), different increases in glyco-conjugated species depending on the model and globally no increase in tauro-conjugated species whatever the model.
Conclusions:
The tested animal models share similar quantitative RYGBP-induced increases in peripheral blood BAs as humans, which render them useful for mechanistic studies. However, they also present qualitative differences in BA profiles, which may result in different signaling responses. Such differences need to be taken into account when translating results to humans.





Similar content being viewed by others
References
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014; 384: 766–781.
Cummings DE, Overduin J, Foster-Schubert KE . Gastric bypass for obesity: mechanisms of weight loss and diabetes resolution. J Clin Endocrinol Metab 2004; 89: 2608–2615.
Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, Pories WJ et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med 2009; 122: 248–256.
Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg 1995; 222: 339–350.
Mummadi RR, Kasturi KS, Chennareddygari S, Sood GK . Effect of bariatric surgery on nonalcoholic fatty liver disease: systematic review and meta-analysis. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 2008; 6: 1396–1402.
Caiazzo R, Lassailly G, Leteurtre E, Baud G, Verkindt H, Raverdy V et al. Roux-en-Y gastric bypass versus adjustable gastric banding to reduce nonalcoholic fatty liver disease: a 5-year controlled longitudinal study. Ann Surg 2014; 260: 893–898.
Ricci C, Gaeta M, Rausa E, Macchitella Y, Bonavina L . Early impact of bariatric surgery on type II diabetes, hypertension, and hyperlipidemia: a systematic review, meta-analysis and meta-regression on 6,587 patients. Obes Surg 2014; 24: 522–528.
Tailleux A, Rouskas K, Pattou F, Staels B . Bariatric surgery, lipoprotein metabolism and cardiovascular risk. Curr Opin Lipidol 2015; 26: 317–324.
Lindqvist A, Spégel P, Ekelund M, Mulder H, Groop L, Hedenbro J et al. Effects of ingestion routes on hormonal and metabolic profiles in gastric-bypassed humans. J Clin Endocrinol Metab 2013; 98: E856–E861.
Wu Q, Xiao Z, Cheng Z, Tian H . Changes of blood glucose and gastrointestinal hormones 4 months after Roux-en-Y gastric bypass surgery in Chinese obese type 2 diabetes patients with lower body mass index. J Diabetes Invest 2013; 4: 214–221.
Sweeney TE, Morton JM . The human gut microbiome: a review of the effect of obesity and surgically induced weight loss. JAMA Surg 2013; 148: 563–569.
Ryan KK, Tremaroli V, Clemmensen C, Kovatcheva-Datchary P, Myronovych A, Karns R et al. FXR is a molecular target for the effects of vertical sleeve gastrectomy. Nature 2014; 509: 183–188.
Penney NC, Kinross JM, Newton RC, Purkayastha S . The role of bile acids in reducing the metabolic complications of obesity after bariatric surgery: a systematic review. Int J Obes 2015; 191: 127–139.
Russell DW . The enzymes, regulation, and genetics of bile acid synthesis. Annu Rev Biochem 2003; 72: 137–174.
Lefebvre P, Cariou B, Lien F, Kuipers F, Staels B . Role of bile acids and bile acid receptors in metabolic regulation. Physiol Rev 2009; 89: 147–191.
Claus SP, Ellero SL, Berger B, Krause L, Bruttin A, Molina J et al. Colonization-induced host–gut microbial metabolic interaction. mBio 2011; 2: e00271–00210.
de Aguiar Vallim TQ, Tarling EJ, Edwards PA . Pleiotropic roles of bile acids in metabolism. Cell Metab 2013; 17: 657–669.
Osto E, Doytcheva P, Corteville C, Bueter M, Dörig C, Stivala S et al. Rapid and body weight-independent improvement of endothelial and high-density lipoprotein function after Roux-en-Y gastric bypass: role of glucagon-like peptide-1. Circulation 2015; 131: 871–881.
Bruinsma BG, Uygun K, Yarmush ML, Saeidi N . Surgical models of Roux-en-Y gastric bypass surgery and sleeve gastrectomy in rats and mice. Nat Protoc 2015; 10: 495–507.
Arble DM, Sandoval DA, Seeley RJ . Mechanisms underlying weight loss and metabolic improvements in rodent models of bariatric surgery. Diabetologia 2015; 58: 211–220.
Seyfried F, le Roux CW, Bueter M . Lessons learned from gastric bypass operations in rats. Obes Facts 2011; 4 (Suppl 1): 3–12.
Shin AC, Zheng H, Townsend RL, Sigalet DL, Berthoud H-R . Meal-induced hormone responses in a rat model of Roux-en-Y gastric bypass surgery. Endocrinology 2010; 151: 1588–1597.
Bhutta HY, Rajpal N, White W, Freudenberg JM, Liu Y, Way J et al. Effect of Roux-en-Y gastric bypass surgery on bile acid metabolism in normal and obese diabetic rats. PLoS One 2015; 10: e0122273–e0122290.
Potvin M, Gagner M, Pomp A . Laparoscopic Roux-en-Y gastric bypass for morbid obesity: a feasibility study in pigs. Surg Laparosc Endosc 1997; 7: 294–297.
Cagigas JC, Martino E, Escalante CF, Ingelmo A, Estefanía R, Gutierrez JM et al. Technical alternatives in laparoscopic distal gastric bypass for morbid obesity in a porcine model. Obes Surg 1999; 9: 166–170.
Scott DJ, Provost DA, Tesfay ST, Jones DB . Laparoscopic Roux-en-Y gastric bypass using the porcine model. Obes Surg 2001; 11: 46–53.
Gentileschi P, Gagner M, Milone L, Kini S, Fukuyama S . Histologic studies of the bypassed stomach after Roux-en-Y gastric bypass in a porcine model. Obes Surg 2006; 16: 886–890.
Flum DR, Devlin A, Wright AS, Figueredo E, Alyea E, Hanley PW et al. Development of a porcine Roux-en-Y gastric bypass survival model for the study of post-surgical physiology. Obes Surg 2007; 17: 1332–1339.
Sham JG, Simianu VV, Wright AS, Stewart SD, Alloosh M, Sturek M et al. Evaluating the mechanisms of improved glucose homeostasis after bariatric surgery in Ossabaw miniature swine. J Diabetes Res 2014; 2014: 526972–526979.
Lindqvist A, Spégel P, Ekelund M, Garcia Vaz E, Pierzynowski S, Gomez MF et al. Gastric bypass improves β-cell function and increases β-cell mass in a porcine model. Diabetes 2014; 63: 1665–1671.
Verhaeghe R, Zerrweck C, Hubert T, Tréchot B, Gmyr V, D’Herbomez M et al. Gastric bypass increases postprandial insulin and GLP-1 in nonobese minipigs. Eur Surg Res 2014; 52: 41–49.
Laville M, Romon M, Chavrier G, Guy-Grand B, Krempf M, Chevallier JM et al. Recommendations regarding obesity surgery. Obes Surg 2005; 15: 1476–1480.
García-Cañaveras JC, Donato MT, Castell JV, Lahoz A . Targeted profiling of circulating and hepatic bile acids in human, mouse, and rat using a UPLC-MRM-MS-validated method. J Lipid Res 2012; 53: 2231–2241.
Ahlberg J, Angelin B, Björkhem I, Einarsson K . Individual bile acids in portal venous and systemic blood serum of fasting man. Gastroenterology 1977; 73: 1377–1382.
McRae M, Rezk NL, Bridges AS, Corbett AH, Tien H-C, Brouwer KLR et al. Plasma bile acid concentrations in patients with human immunodeficiency virus infection receiving protease inhibitor therapy: possible implications for hepatotoxicity. Pharmacotherapy 2010; 30: 17–24.
Kasbo J, Saleem M, Perwaiz S, Mignault D, Lamireau T, Tuchweber B et al. Biliary, fecal and plasma deoxycholic acid in rabbit, hamster, guinea pig, and rat: comparative study and implication in colon cancer. Biol Pharm Bull 2002; 25: 1381–1384.
Patti M-E, Houten SM, Bianco AC, Bernier R, Larsen PR, Holst JJ et al. Serum bile acids are higher in humans with prior gastric bypass: potential contribution to improved glucose and lipid metabolism. Obesity (Silver Spring, MD) 2009; 17: 1671–1677.
Nakatani H, Kasama K, Oshiro T, Watanabe M, Hirose H, Itoh H . Serum bile acid along with plasma incretins and serum high-molecular weight adiponectin levels are increased after bariatric surgery. Metabolism 2009; 58: 1400–1407.
Pournaras DJ, Glicksman C, Vincent RP, Kuganolipava S, Alaghband-Zadeh J, Mahon D et al. The role of bile after Roux-en-Y gastric bypass in promoting weight loss and improving glycaemic control. Endocrinology 2012; 153: 3613–3619.
Simonen M, Dali-Youcef N, Kaminska D, Venesmaa S, Käkelä P, Pääkkönen M et al. Conjugated bile acids associate with altered rates of glucose and lipid oxidation after Roux-en-Y gastric bypass. Obes Surg 2012; 22: 1473–1480.
De Giorgi S, Campos V, Egli L, Toepel U, Carrel G, Cariou B et al. Long-term effects of Roux-en-Y gastric bypass on postprandial plasma lipid and bile acids kinetics in female non diabetic subjects: a cross-sectional pilot study. Clin Nutr 2014; 34: 911–917.
Scholtz S, Miras AD, Chhina N, Prechtl CG, Sleeth ML, Daud NM et al. Obese patients after gastric bypass surgery have lower brain-hedonic responses to food than after gastric banding. Gut 2014; 63: 891–902.
Werling M, Vincent RP, Cross GF, Marschall H-U, Fändriks L, Lönroth H et al. Enhanced fasting and post-prandial plasma bile acid responses after Roux-en-Y gastric bypass surgery. Scand J Gastroenterol 2013; 48: 1257–1264.
Jansen PLM, van Werven J, Aarts E, Berends F, Janssen I, Stoker J et al. Alterations of hormonally active fibroblast growth factors after Roux-en-Y gastric bypass surgery. Dig Dis (Basel, Switzerland) 2011; 29: 48–51.
Steinert RE, Peterli R, Keller S, Meyer-Gerspach AC, Drewe J, Peters T et al. Bile acids and gut peptide secretion after bariatric surgery: a 1-year prospective randomized pilot trial. Obesity (Silver Spring, MD) 2013; 21: E660–E668.
Jørgensen NB, Dirksen C, Bojsen-Møller KN, Kristiansen VB, Wulff BS, Rainteau D et al. Improvements in glucose metabolism early after gastric bypass surgery are not explained by increases in total bile acids and fibroblast growth factor 19 concentrations. J Clin Endocrinol Metab 2015; 100: E396–E406.
Dutia R, Embrey M, O’Brien S, Haeusler RA, Agénor KK, Homel P et al. Temporal changes in bile acid levels and 12α-hydroxylation after Roux-en-Y gastric bypass surgery in type 2 diabetes. Int J Obes 2015; 39: 806–813.
Albaugh VL, Flynn CR, Cai S, Xiao Y, Tamboli RA, Abumrad NN . Early increases in bile acids post Roux-en-Y gastric bypass are driven by insulin-sensitizing, secondary bile acids. J Clin Endocrinol Metab 2015; 100: E1225–E1233.
Gerhard GS, Styer AM, Wood GC, Roesch SL, Petrick AT, Gabrielsen J et al. A role for fibroblast growth factor 19 and bile acids in diabetes remission after Roux-en-Y gastric bypass. Diabetes Care 2013; 36: 1859–1864.
Zhou D, Jiang X, Ding W, Zhang D, Yang L, Zhen C et al. Impact of bariatric surgery on ghrelin and obestatin levels in obesity or type 2 diabetes mellitus rat model. J Diabetes Res 2014; 2014: 569435.
Kohli R, Bradley D, Setchell KD, Eagon JC, Abumrad N, Klein S . Weight loss induced by Roux-en-Y gastric bypass but not laparoscopic adjustable gastric banding increases circulating bile acids. J Clin Endocrinol Metab 2013; 98: E708–E712.
Kohli R, Kirby M, Setchell KDR, Jha P, Klustaitis K, Woollett LA et al. Intestinal adaptation after ileal interposition surgery increases bile acid recycling and protects against obesity-related comorbidities. Am J Physiol Gastrointest Liver Physiol 2010; 299: G652–G660.
Goncalves D, Barataud A, De Vadder F, Vinera J, Zitoun C, Duchampt A et al. Bile routing modification reproduces key features of gastric bypass in rat. Ann Surg 2015; 262: 1006–1015.
Lutz TA, Bueter M . Physiological mechanisms behind Roux-en-Y gastric bypass surgery. Dig Surg 2014; 31: 13–24.
Birck MM, Vegge A, Støckel M, Gögenur I, Thymann T, Hammelev KP et al. Laparoscopic Roux-en-Y gastric bypass in super obese Göttingen minipigs. Am J Transl Res 2013; 5: 643–653.
Parks DJ, Blanchard SG, Bledsoe RK, Chandra G, Consler TG, Kliewer SA et al. Bile acids: natural ligands for an orphan nuclear receptor. Science 1999; 284: 1365–1368.
Kawamata Y, Fujii R, Hosoya M, Harada M, Yoshida H, Miwa M et al. A G protein-coupled receptor responsive to bile acids. J Biol Chem 2003; 278: 9435–9440.
Sayin SI, Wahlström A, Felin J, Jäntti S, Marschall H-U, Bamberg K et al. Gut microbiota regulates bile acid metabolism by reducing the levels of tauro-beta-muricholic acid, a naturally occurring FXR antagonist. Cell Metab 2013; 17: 225–235.
Makishima M, Okamoto AY, Repa JJ, Tu H, Learned RM, Luk A et al. Identification of a nuclear receptor for bile acids. Science 1999; 284: 1362–1365.
Cui J, Heard TS, Yu J, Lo J-L, Huang L, Li Y et al. The amino acid residues asparagine 354 and isoleucine 372 of human farnesoid X receptor confer the receptor with high sensitivity to chenodeoxycholate. J Biol Chem 2002; 277: 25963–25969.
Midtvedt T . Microbial bile acid transformation. Am J Clin Nutr 1974; 27: 1341–1347.
Ridlon JM, Kang D-J, Hylemon PB . Bile salt biotransformations by human intestinal bacteria. J Lipid Res 2006; 47: 241–259.
Swann JR, Want EJ, Geier FM, Spagou K, Wilson ID, Sidaway JE et al. Systemic gut microbial modulation of bile acid metabolism in host tissue compartments. Proc Natl Acad Sci USA 2011; 108 (Suppl 1): 4523–4530.
Mueller M, Thorell A, Claudel T, Jha P, Koefeler H, Lackner C et al. Ursodeoxycholic acid exerts farnesoid X receptor-antagonistic effects on bile acid and lipid metabolism in morbid obesity. J Hepatol 2015; 62: 1398–1404.
Song P, Rockwell CE, Cui JY, Klaassen CD . Individual bile acids have differential effects on bile acid signaling in mice. Toxicol Appl Pharmacol 2015; 283: 57–64.
Acknowledgements
We thank C Corteville for technical support in rat surgery. VS was supported by a grant from the Fondation pour la Recherche Médicale (FRM) Grant FDT20140930804. This work was supported by grants from ‘European Genomic Institute for Diabetes’ (EGID, ANR-10-LABX-46), European Commission, Région Nord-Pas de Calais, FEDER, INSERM, A.N.R. (FXREn), Université Lille and Université Lille Nord de France. BS is a member of the Institut Universitaire de France.
Note added in proof
Since submission, it was observed that the free and conjugated UDCA peaks in the LC-MS/MS measurement contain UDCA plus HDCA. The analyzed human and rat samples contain solely HDCA, whereas in pigs HDCA is the major BA in this peak. These findings do not impact the conclusions of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Spinelli, V., Lalloyer, F., Baud, G. et al. Influence of Roux-en-Y gastric bypass on plasma bile acid profiles: a comparative study between rats, pigs and humans. Int J Obes 40, 1260–1267 (2016). https://doi.org/10.1038/ijo.2016.46
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2016.46
- Springer Nature Limited
This article is cited by
-
Intrahepatic cholestasis of pregnancy: insights into pathogenesis and advances in omics studies
Hepatology International (2024)
-
Hyodeoxycholic acid ameliorates nonalcoholic fatty liver disease by inhibiting RAN-mediated PPARα nucleus-cytoplasm shuttling
Nature Communications (2023)
-
Hyocholic acid species as novel biomarkers for metabolic disorders
Nature Communications (2021)
-
Metabolomics in Bariatric Surgery: Towards Identification of Mechanisms and Biomarkers of Metabolic Outcomes
Obesity Surgery (2021)
-
Metabolic characteristics of plasma bile acids in patients with intrahepatic cholestasis of pregnancy-mass spectrometric study
Metabolomics (2021)