Abstract
Dahl salt-sensitive (Dahl S) rats are prone to salt-dependent hypertension with severe organ damage, including stroke, cardiac failure and renal insufficiency. The mechanism for this susceptibility to kidney injury has not been elucidated. The present study proposed that an upregulation of intracellular signaling of angiotensin II (Ang-II) is responsible for the susceptibility to hypertensive kidney injury in Dahl S rats. Spontaneously hypertensive rats exhibited higher systolic blood pressure (SBP) and lower kidney damage than Dahl S rats fed a high-salt diet for 2 weeks. Ang-II infusion for 4 weeks significantly increased SBP in Dahl S and Dahl salt-resistant (Dahl R) rats fed a low-salt diet. The increase in SBP in Dahl S rats was associated with significant kidney injury with greater glomerular sclerosis (P<0.001). The expression of regulatory protein of Gαq signaling-2 (RGS2) mRNA in the aortic walls in response to Ang-II infusion was lower in Dahl S than Dahl R rats (P<0.05). Ang-II significantly increased RGS2 mRNA in the aorta in Dahl R rats, but the response was apparently blunted in Dahl S rats. These results suggest that Dahl S rats exhibit a blunted RGS2 response to Ang-II, and this blunted response may be partially responsible for the susceptibility to renal injury in Dahl S rats.
Similar content being viewed by others
Introduction
Recently, much attention has been given to the role of regulator of G-protein signaling 2 (RGS2), a member of the RGS family, in the pathogenesis of high blood pressure. RGS2 selectively inhibits the receptor-mediated signal transduction of vasoconstrictor substances, including angiotensin II (Ang-II), endothelin-1, and norepinephrine, via transformation of active GTP-Gαq to inactive GDP-coupled subunit by its GTPase activity.1, 2, 3 RGS2 also influences Gi- and Gs-mediated signal transduction, including bradykinin, serotonin and dopamine.4, 5 The expression of RGS2 protein is not widely investigated, but RGS2 mRNA expression is associated with changes in phenotype expression.6 Heximer et al.7 demonstrated that knockout of the RGS2 gene produced a hypertensive phenotype with prolonged vasoconstrictor signaling in an RGS2-deficient mouse line. Blood pressure elevation in RGS2−/− mice was due to an Ang-II-dependent increase in vascular tone. A series of studies on RGS2 mRNA expression strongly suggest that RGS2 has an important role in Ang-II receptor-mediated signal transduction and cardiovascular organ damage.8
Dahl salt-sensitive (Dahl S) rats represent a rat model of volume-dependent hypertension. Dahl S rats are more likely to develop severe arterial and renal injury when fed a high-salt diet compared with a genetic rat model of spontaneous hypertension (SHR). Our preliminary study demonstrated that Dahl S rats exhibited greater proteinuria and morphological damage in the kidney than SHR when blood pressure and age were matched. This susceptibility may be due to multiple factors, for example, increased shear stress following volume expansion, abnormal metabolism of vasoconstrictor substances, alterations of the renin–angiotensin system (RAS), and inflammatory processes with an overgeneration of oxygen radicals.9, 10, 11, 12, 13, 14
Angiotensin-converting enzyme inhibition attenuates blood pressure elevation in a RAS model, which should be suppressed.9 We also demonstrated that Dahl S rats with salt-induced hypertension have greater kidney injury in response to a continuous infusion of subpressor doses of Ang-II.11 These studies highly suggest that the signal transduction of Ang-II is upregulated in Dahl S rats, and this upregulation is partially responsible for the susceptibility of Dahl S to organ damage. Therefore, the present study highlighted the regulation of intracellular Ang-II signal transduction and proposed that RGS2, a modulator of the Ang-II-induced intracellular signal transduction system, has a role in the susceptibility of Dahl S rats to hypertensive renal injury. We investigated renal injury and RGS2 mRNA expression in low-salt Dahl S rats with Ang-II induced hypertension to test our hypothesis.
Methods
Salt-induced hypertensive Dahl S rats and SHR
Sixteen male Dahl S rats and SHR were fed a regular chow after weaning (Dahl S/Jr Sea, CLEA Japan, Tokyo, Japan). The rats were challenged with a high salt (8% NaCl, w/w) diet at 4 weeks of age and maintained on this diet for 2 weeks. Rats were given free access to water throughout the study. Urine was collected for 24 h using a metabolic cage prior to the high-salt loading (week 0) and at 2 weeks.
Ang-II-induced hypertension in Dahl S rats
Twenty-four male Dahl S and Dahl salt-resistant (Dahl R) rats were fed a low-salt (0.3% NaCl, w/w) diet immediately after weaning (Dahl S/Jr Sea and Dahl R/Jr Sea, CLEA Japan). The rats were given free access to water throughout the study.
Dahl S and Dahl R rats were divided into four experimental groups at the age of 6 weeks: (1) six Dahl S rats fed a low-salt diet and given a pressor dose of Ang-II (100 ng min−1 per kg body weight; Dahl S+Ang-II), (2) six Dahl S rats fed a low-salt diet and given saline solution (Dahl S Control), (3) six Dahl R rats fed a low-salt diet and given a pressor dose of Ang-II (100 ng min−1 per kg body weight; Dahl R+Ang-II), and (4) six Dahl R rats fed a low-salt diet and saline solution (Dahl R Control). Ang-II or the control saline solution was subcutaneously infused for 4 weeks using mini-osmotic pumps (model 1002; Alzet Corporation, Palo Alto, CA, USA).
Blood pressure determination and kidney processing
Systolic blood pressure (SBP) was determined weekly using a tail cuff and oscillometric method according to previous studies.12, 13, 14, 15 Blood samples and organs of interest were obtained under pentobarbital anesthesia (75 mg per kg body weight) at the end of the study. The left kidney and aorta were quickly plunged into liquid nitrogen for mRNA determination. The right kidney was used for morphological investigation. Separated blood samples and urine were stored at −80 °C until the assays were performed. Twenty-four hour urine was collected weekly using a metabolic cage.
Determination of renal function
Plasma and urinary creatinine concentrations were determined using an autoanalyzer (Model Hitachi 736, Hitachi, Tokyo, Japan). Urinary protein excretion was measured using a protein assay kit (Bio-Rad Laboratories, Hercules, CA, USA).
Histological investigation
Renal tissue was processed for light microscopy as follows: half of the left kidney was fixed in 3.5% formalin solution. Sagittal slices were cut, embedded and stained with hematoxylin and eosin, periodic acid-methenamine silver and periodic acid-Schiff stains.
An independent investigator who had no previous knowledge of the group to which each rat belonged evaluated all sections. At least 100 glomeruli in each specimen were examined, and the severity of lesions was graded 0 to 4+ according to the percentage of the glomerulus involved: 0 no lesions (group 1); 1+1–25% (group 2); 2+26–50% (group 3); 3+51–75% (group 4); and 4+76–100% (group 5).9, 10, 11, 12, 13, 14, 15 Each percentage of glomerular sclerosis in each category was multiplied by the corresponding grade, and the figures were summated to obtain glomerular sclerotic index.
RNA extraction
Kidney (20 mg) samples frozen in liquid nitrogen and stored under −80 °C were homogenized under −4 °C using a MagNA Lyser (Roche Diagnostics, Mannheim, Germany) at 6500 r.p.m. for 50 s. Total RNA was extracted from the kidney and aortic walls using a High Pure Tissue/Isolation kit (Roche Diagnostics) according to the manufacturer’s instructions. Total RNA concentrations and purity were determined using a spectrophotometer at 260/280 nm wavelengths. The ratio of OD260/OD280 was >1.90 in all extracted RNA samples. RNA (460 μg) was used for complementary DNA synthesis using a Transcriptor First Strand cDNA Synthesis Kit (Roche Diagnostics) according to the manufacturer’s protocol.
Real-time PCR of RGS2 mRNA
RGS2 and GAPDH mRNA were quantified using a LightCycler 1.5 real-time PCR (Roche Diagnostics) and LightCycler TaqMan Master (Roche Diagnostics). Nihon Gene Research Laboratories, Tokyo, Japan, designed the primers.
Primer of RGS2 (forward), 5′-GTTGGGTAGTGAATCAGGAAGC-3′
Primer of RGS2 (reverse), 5′-GACCACCTATTCCCTTCTTGC-3′
Primer of GAPDH (forward), 5′-AATGTATCCGTTGTGGATCTGA-3′
Primer of GAPDH (reverse), 5′-GCTTCACCACCTTCTTGATGT-3′
The probes were selected from Universal Probe Library Probes 1–165 for LightCycler (Roche Diagnostics). The reaction mixture (20 μl) was composed of a 5 × concentration of LightCycler TaqMan Master, 100 nmol l−1 Universal Probe Library probe, 100 nmol l−1 forward primer, 200 nmol l−1 reverse primer and 5 μl of the template. Times and temperatures for the real-time PCR configuration using the TaqMan probe and the LightCycler were 10 s at 95 °C for denaturation, 20 s at 62 °C for annealing and 10 s at 72 °C for amplification (45 cycles).
Statistical analysis
Data are expressed as the means±s.e.m. Differences were analyzed using one-way analysis of variance followed by post hoc analysis, and multiple regression analysis was performed using STATISTICA software (StatSoft, Tulsa, OK, USA). P<0.05 was considered statistically significant.
Guidelines for the handling of rats for experiments
The rats used in the studies were handled according to the University guideline for animal husbandry and the management of experimental animals.
Results
Salt-induced hypertensive Dahl S rats and SHR
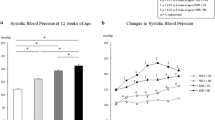
A high-salt diet challenge significantly increased SBP in Dahl S rats over 2 weeks, and SHR fed a high-salt diet also exhibited an increased SBP, but this increase was significantly smaller in Dahl S rats than SHR (Figure 1a). Challenge with a high-salt diet and the subsequent increase in blood pressure were associated with more than a 20-fold increase in urinary protein excretion in Dahl S rats (Figure 1b). These excretions were not altered in hypertensive SHR, and the difference between the two strains was marked (P<0.001). Glomerular sclerotic lesions significantly progressed in Dahl S rats challenged by a high-salt diet, but few glomerular sclerotic lesions were observed in SHR, even SHR with higher SBP than Dahl S rats (Figure 1c).
Hypertension and kidney injury in Dahl salt-sensitive (Dahl S) rats and spontaneously hypertensive rats (SHR). We demonstrated the effects of a high-salt diet on systolic blood pressure (SBP) (a) and renal biomarkers, including urinary protein excretion (b) and glomerular sclerosing score (c), in SHR and Dahl S rats (DS). SHR_0W, SHR aged 4 weeks old and fed a low-salt (0.3%) NaCl diet after weaning; SHR_2W, 6-week-old SHR fed a 8% NaCl (w/w) diet for 2 weeks; DS_0W, Dahl S rats aged 4 weeks and fed a low-salt diet after weaning; DS_2W, 6-week-old Dahl S rats fed a 8% NaCl diet for 2 weeks. Values are expressed as means±s.e.m. Differences between the four groups were assessed using a one-way analysis of variance. NS, not significant.
These data strongly suggested that the Dahl S rat strain was prone to hypertensive renal damage in contrast to the SHR strain. Volume expansion in Dahl S rats following a high-salt diet may contribute to the difference between the two strains. We attempted to minimize the effects of volume expansion using a low-salt (0.3% NaCl, w/w) diet and investigated the role of Ang-II in organ injury in Dahl S and Dahl R rats on a low-salt diet.
Dahl S rats with Ang-II-induced hypertension
Figure 2a shows that a 100 ng min−1 infusion of Ang-II significantly increased SBP in Dahl S and Dahl R rats in a time-dependent manner. SBP was greater in Dahl S than Dahl R rats at the end of the study. Basal blood pressure was higher in Dahl S than Dahl R rats, but there was no difference in SBP changes in response to Ang-II infusion between the two strains (Figure 2b).
Blood pressure in angiotensin II (Ang-II)-induced hypertension. We demonstrated the effects of Ang-II infusion on systolic blood pressure in Dahl salt-sensitive (Dahl S) and Dahl salt-resistant (Dahl R) rats (a). The absolute changes in SBP are also shown in b. Open squares, Dahl S rats fed a low-salt diet (Dahl S); closed squares, Dahl S rats fed a low-salt diet and given Ang-II (100 ng min−1 per kg body weight (BW); Dahl S+AII); open triangles, Dahl R rats fed a low-salt diet (Dahl R) and; closed triangles, Dahl R rats fed a low-salt diet and given Ang-II (100 ng min−1 per kg BW; Dahl R+AII). Values are expressed as means±s.e.m. Differences between the four groups were assessed using a one-way analysis of variance. *P<0.01 versus value at the same week in Dahl R+AII rats. NS, not significant.
Characterization of renal injury
Figure 3a shows that urinary protein excretions were greater in Dahl S rats given a saline solution (Dahl S Control) than Dahl R Control. Ang-II infusion significantly increased urinary protein excretion in Dahl S rats, but protein excretions were unchanged in Dahl R rats. Ang-II infusion decreased the creatinine clearance rate in Dahl S rats, and the creatinine clearance rate was unchanged in Dahl R rats (Figure 3b).
Renal impairment in angiotensin II (Ang-II)-induced hypertension. The alterations in urinary excretions of protein and creatinine clearance rate are shown in a and b, respectively. Dahl salt-resistant (Dahl R) rats, Dahl R rats fed a low-salt diet; Dahl R+AII, Dahl R rats fed a low-salt diet and given Ang-II (100 ng min−1 per kg body weight (BW)). Dahl salt-sensitive (Dahl S) rats, Dahl S rats fed a low-salt diet and; Dahl S+AII, Dahl S rats fed a low-salt diet and given Ang-II (100 ng min−1 per kg BW). Values are expressed as means±s.e.m. Differences between the four groups were assessed using a one-way analysis of variance. NS, not significant.
We morphologically investigated renal impairment. Figure 4 shows that various degrees of kidney injury, from almost intact to completely sclerotic glomeruli, were observed. We determined the percentage of glomeruli that exhibited each degree of glomerular sclerosis and estimated the sclerosis index, as described in the Methods section. Glomerular sclerotic lesions were higher in control Dahl S rats than control Dahl R rats. Ang-II infusion significantly increased glomerular sclerotic lesions in Dahl S rats, but it did not influence lesions in Dahl R rats (Figure 5).
Representative glomerular lesions in Dahl salt-resistant (Dahl R) and Dahl salt-sensitive (Dahl S) rats. A large number of glomeruli were almost normal in appearance in Dahl R rats fed a low-salt diet (a) (0% sclerosis). In Dahl S rats, sclerosis of the glomeruli was greater than Dahl R rats (b) (25–50% sclerosis). Angiotensin II (Ang-II) infusion enhanced the glomerular sclerosis in Dahl R rats (c) (0–25% sclerosis) and Dahl S rats (d) (50–75% sclerosis). However, glomerular sclerosis was apparently greater in Dahl S rats than Dahl R rats. Periodic acid Schiff stain, original magnification × 400.
Morphological assessment of renal injury. Alterations in glomerular sclerosis following angiotensin II (Ang-II) infusion in Dahl salt-resistant (Dahl R) and Dahl salt-sensitive (Dahl S) rats. Dahl R, Dahl R fed a low-salt diet; Dahl R+AII, Dahl R rats fed a low-salt diet and given Ang-II (100 ng min−1 per kg body weight (BW)). Dahl S, Dahl S rats fed a low-salt diet and; Dahl S+AII, Dahl S rats fed a low salt-diet and given Ang-II infusion (100 ng min−1 per BW). Values are expressed as means±s.e.m. Differences between the four groups were assessed using one-way analysis of variance. NS, not significant.
RGS2 mRNA expression
The renal impairment demonstrated in Dahl S rats with Ang-II-induced hypertension was the result of the increased sensitivity to mechanical stress from hypertension or Ang-II-mediated events. We investigated alterations in mRNA levels of a regulator of intracellular Ang-II signal transduction, RGS2, in the kidney and aorta. Dahl S rats tended to exhibit decreased RGS2 mRNA expression compared with Dahl R rats. However, Ang-II infusion increased mRNA expression in Dahl R rats (Dahl R+AII in Figure 6a), but this trend of RGS2 mRNA expression was blunted in Dahl S rats. A significant difference between Dahl R and Dahl S rats was observed (Dahl R+AII and Dahl S+AII in Figure 6a).
Regulators of G-protein signaling (RGS2) mRNA expression in the kidney (a) and aortic walls (b). Dahl R, Dahl R rats fed a low-salt diet; Dahl R+AII, Dahl R rats fed a low-salt diet and given angiotensin II (Ang-II; 100 ng min−1 per kg body weight (BW)); Dahl S, Dahl S rats fed a low-salt diet and; Dahl S+AII, Dahl S rats fed a low-salt diet and given Ang-II (100 ng min−1 per kg BW). Values are expressed as means±s.e.m. Differences between the four groups were assessed using one-way analysis of variance followed by post hoc analysis. mRNA was extracted as described in the Methods section, and mRNA expression analysis was performed using real-time PCR. NS, not significant.
This difference was more clearly demonstrated in RGS2 mRNA expression in aortic walls (Figure 6b). RGS2 mRNA expression increased by ~150% in response to Ang-II infusion, which strongly suggests a downregulation of Ang-II receptor-mediated signal transduction. In contrast, the response of RGS2 mRNA expression to Ang-II infusion was completely blunted in Dahl S rats, which suggests that Ang-II receptor-mediated signal transduction more likely occurred downstream.
Discussion
The present study demonstrated that Dahl S rats are likely to develop kidney injury compared with SHR with similar high blood pressure. This result may be due to an increased shear or mechanical stress from salt retention and/or intrinsic susceptibility to hypertensive injury. We investigated the inherent mechanisms for this hypersensitivity. We demonstrated that inhibition of the (RAS) by angiotensin-converting enzyme inhibitors attenuated blood pressure elevation in salt-dependent hypertension in Dahl S rats, and this effect was associated with reduced glomerular sclerosis.9 In addition to shear or mechanical stress, RAS likely participates in the susceptibility to renal injury in salt-induced hypertension.16, 17, 18 An increase in body fluid generally suppresses RAS activity. Therefore, the contribution of RAS to the renal injury in volume-dependent hypertension should be investigated.
We examined the effects of Ang-II on renal injury when the influence of volume expansion was minimized to understand the mechanisms of this susceptibility in Dahl S rats. The present study demonstrated that Ang-II infusion induced hypertension in Dahl S and Dahl R rats fed a low-salt diet. The blood pressure was higher in Dahl S than Dahl R rats, but the absolute changes during Ang-II infusion were nearly equivalent between Dahl S and Dahl R rats (Figure 2b).
However, there was a marked difference in renal injury between Dahl S and Dahl R rats. Urinary protein excretions were much greater in Dahl S than Dahl R rats. Plasma creatinine concentrations were increased in Dahl S rats, which decreased the creatinine clearance rate. The morphological findings were consistent with changes in biomarkers that indicate renal function. Ang-II-induced hypertension of Dahl S rats was associated with worsening of glomerulosclerotic lesions, compared with Dahl R rats. We could not neglect the possibility that Dahl S rats were more sensitive to the mechanical stress due to hypertension. However, if the pathophysiological implications of RAS are considered, then we may presume that intracellular Ang-II signal transduction was upregulated in Dahl S rats.
Intracellular RGS2 regulates Ang-II signal transduction, and RGS2 knockout mice exhibit an increase in blood pressure of ~50 mm Hg.7 Reduced RGS2 expression in peripheral blood mononuclear cells of hypertensive patients increases calcium mobilization and Ang-II-induced ERK1/2 phosphorylation.19 Notably, Freson et al.20 demonstrated that −391 C to G substitution in the RGS2 promoter increased the susceptibility to metabolic syndrome in white European men.
Therefore, we hypothesized that the kidney injury in Dahl S rats with Ang-II-induced hypertension is partially due to RGS2 function. This study first investigated RGS2 mRNA expression in aortic homogenates and found that RGS2 expression was upregulated in Dahl R rats with Ang-II induced hypertension, which suggests a downregulation of Ang-II signal transduction. This effect likely minimizes Ang-II-mediated untoward influence, and it is consistent with previous data on RGS2 upregulation following Ang-II stimulation in vascular smooth muscle cells in culture.21, 22, 23
We also demonstrated that the basal levels of RGS2 mRNA tended to be decreased in Dahl S rats compared with Dahl R rats. Notably, the upregulation of RGS2 mRNA in response to Ang-II infusion was almost completely abolished in the arterial vessels of Dahl S rats. This result strongly suggests that the intracellular signal transduction of Ang-II is enhanced in Dahl S rats. However, our preliminary study found that RGS2 mRNA levels in the aortic walls from young SHR was greater than those in Wistar Kyoto rats (1.89±0.47 (n=6) vs 1.12±0.11 (n=6), P<0.05; unpublished data). These data suggested that the blunted upregulation of RGS2 mRNA following Ang-II infusion contributed to the susceptibility of Dahl S rats to organ and vascular damage.
In the present study, we examined RGS2 mRNA levels, but we could not determine the expression of RGS2 protein because the tissue concentration of RGS2 protein was too low to detect using a commercially available antibody and western blot analysis. This problem was observed in many previous studies from other laboratories as noted by Ross et al.2 However, RGS2 mRNA is associated with changes in its downstream signaling pathways, and it is highly possible that changes in RGS2 mRNA expression observed in the present study were related to the susceptibility of Dahl S rats to hypertensive organ damage.
Heximer and associates clearly demonstrated that RGS2 is an important regulatory element that decreases Gαq-coupled receptor signaling in vivo.7 These receptors are critical to the pathogenesis of hypertension and target organ damage. Ang-II activates G-protein-coupled angiotensin II subtype-1 receptors (AT1R) via conformational changes, with transformation from GDP to GTP on the Gαq subunit. The Gαq-GTP and Gβγ subunits dissociate, which frees their activation of downstream effector proteins and results in physiological actions, such as vasoconstriction and MAP kinase activation. RGS2 enhances the Gαq-catalyzed hydrolysis of GTP to GDP, which terminates signal transduction between the Gα-system and the subsequent effects. If the regulator dysfunction demonstrated in the present study is a gene-related event, then we may hypothesize that some alterations occur in the promotor area of RGS2 gene in Dahl S rats. Our next step is to disclose the possible hypersensitivity to Ang-II events in Dahl S rats.
The present data suggest that Ang-II-mediated signal transduction must be completely abolished in salt-sensitive hypertension because only a slight change in Ang-II may promote post-receptor signal transduction. We found that the AT1R-specific antagonist olmesartan completely abolishes Ang-II-induced RGS2 mRNA expression in vascular smooth muscle cells in culture (unpublished data). This mechanism may support the rationale for the requirement for a total RAS inhibition strategy in clinical settings. If ARB antagonism with RGS2 upregulation is available, then it is likely very helpful as an antihypertension strategy. We are now searching for these types of drugs in ARBs.
In conclusion, we demonstrated that Dahl S rats were prone to hypertensive renal injury because of hypersensitivity to mechanical stress and/or an upregulation of Ang-II signal transduction via a blunted response of RGS2 mRNA expression. The alterations in the RGS2 mRNA response to Ang-II infusion in Dahl S rats were strikingly different from Dahl R rats. The difference may be due to alterations in the expression of the RGS2 gene, particularly in its promotor region. This hypothesis appears very promising, and a direct gene analysis will provide the answer to this important question.
References
Kehrl JH, Sinnarajah S . RGS2: a multifunctional regulator of G-protein signaling. Int J Biochem Cell Biol 2002; 34: 432–438.
Ross EM, Thomas M, Wilkie TM . GTPase-activating proteins for heterotrimeric G proteins: regulators of G protein signaling (RGS) and RGS-like proteins. Annu Rev Biochem 2000; 69: 795–827.
Heng BC, Aubel D, Fussenegger MG . Protein-coupled receptors revisited: therapeutic applications inspired by synthetic biology. Annu Rev Pharmacol Toxicol 2014; 54: 227–249.
Ingi T, Krumins AM, Chidiac P, Brothers GM, Chung S, Snow BE, Barnes CA, Lanahan AA, Siderovski DP, Ross EM, Gilman AG, Worley PF . Dynamic regulation of RGS2 suggests a novel mechanism in G-protein signaling and neuronal plasticity. J Neurosci 1998; 18: 7178–7188.
Sinnarajah S, Dessauer CW, Srikumar D, Chen J, Yuen J, Yilma S, Dennis JC, Morrison EE, Vodyanoy V, Kehrl JH . RGS2 regulates signal transduction in olfactory neurons by attenuating activation of adenylyl cyclase III. Nature 2001; 409: 1051–1055.
Wolff DW, Xie Y, Deng C, Gatalica Z, Yang M, Wang B, Wang J, Lin MF, Abel PW, Tu Y . Epigenetic repression of regulator of G-protein signaling 2 promotes androgen-independent prostate cancer cell growth. Int J Cancer 2012; 130: 1521–1531.
Heximer SP, Russell RH, Sun X, Kaltenbronn KM, Rhee MH, Peng N, Oliveira-dos-Santos A, Penninger JM, Muslin AJ, Steinberg TH, Wyss JM, Mecham RP, Blumer KJ . Hypertension and prolonged vasoconstrictor signaling in RGS2-deficient mice. J Clin Invest 2003; 111: 445–452.
Le TH, Coffman TM . RGS2: a “turn-off” in hypertension. J Clin Invest 2003; 111: 441–443.
Hirawa N, Uehara Y, Kawabata Y, Ohshima N, Ono H, Nagata T, Gomi T, Ikeda T, Goto A, Yagi S, Omata M . Mechanistic analysis of renal protection by angiotensin converting enzyme inhibitor in Dahl salt-sensitive rats. J Hypertens 1994; 12: 909–918.
Uehara Y, Numabe A, Hirawa N, Kawabata Y, Iwai J, Ono H, Matsuoka H, Takabatake Y, Yagi S, Sugimoto T . Antihypertensive effects of cicletanine and renal protection in Dahl salt-sensitive rats. J Hypertens 1991; 9: 719–728.
Hirawa N, Uehara Y, Kawabata Y, Numabe A, Ohshima N, Ono H, Gomi T, Ikeda T, Yagi S, Toyo-oka T . Subpresor dose of angiotensin II increases susceptibility to the haemodynamic injury of blood pressure in Dahl salt-sensitive rats. J Hypertens 1995; 13: 81–90.
Ishimitsu T, Uehara Y, Numabe A, Tsukada H, Ogawa Y, Iwai J, Ikeda T, Matsuoka H, Sugimoto T, Yagi S . Interferon gamma attenuates hypertensive renal injury in salt-sensitive Dahl rats. Hypertension 1992; 19: 804–808.
Uehara Y, Tobian L, Iwai J, Ishii M, Sugimoto T . Alterations of vascular prostacyclin and thromboxane A2 in Dahl genetical strain susceptible to salt-induced hypertension. Prostaglandins 1987; 33: 727–738.
Uehara Y, Kawabata Y, Hirawa N, Takada S, Nagata T, Numabe A, Iwai J, Sugimoto T . Possible radical scavenging properties of cicletanine and renal protection in Dahl salt sensitive rats. Am J Hypertens 1993; 6 (6 Pt 1): 463–472.
Hirawa N, Uehara Y, Kawabata Y, Numabe A, Ogawa N, Gomi T, Ikeda T, Goto A, Toyoka T, Omata M . High salt intake potentiates the renal vascular and glomerular damage caused by low doses of angiotensin II in uni-nephrectomized rats. J Hypertens 1999; 17: 923–932.
Anderso PW, Do YS, Hsueh WA . Angiotensin II causes mesangial cell hypertrophy. Hypertension 1993; 21: 29–35.
Raij L, Learne WF . Glomerular mesangium: its function and relationship to angiotensin II. Am J Med 1985; 79: 24–30.
Hirawa N, Uehara Y, Numabe A, Kawabata Y, Gomi T, Ikeda T, Ohnishi T, Ishii M, Omata M . The implication of renin-angiotensin system on renal injury seen in Dahl salt-sensitive rats. Am J Hypertens 1997; 10: 102S–106S.
Semplicini A, Lenzini L, Sartori M, Papparella I, Calò LA, Pagnin E, Strapazzon G, Benna C, Costa R, Avogaro A, Ceolotto G, Pessina AC . Reduced expression of regulator of G-protein signaling 2 (RGS2) in hypertensive patients increases calcium mobilization and ERK1/2 phosphorylation induced by angiotensin II. J Hypertens 2006; 24: 1115–1124.
Freson K, Stolarz K, Aerts R, Brand E, Brand-Herrmann SM, Kawecka-Jaszcz K, Kuznetsova T, Tikhonoff V, Thijs L, Vermylen J, Staessen JA, Van Geet C . European Project on Genes in Hypertension Investigators. -391 C to G substitution in the regulator of G-protein signalling-2 promoter increases susceptibility to the metabolic syndrome in white European men. J Hypertens 2007; 25: 117–125.
Grant SL, Lasseque B, Griendling KK, Ushio-Fukai M, Lyons PR, Alexander RW . Specific regulation of RGS2 messenger RNA by angiotensin II in cultured vascular smooth muscle cells. Mol Pharmacol 2000; 57: 460–467.
Wang X, Adams LD, Pabon LM, Mahoney WM Jr, Beaudry D, Gunaje J, Geary RL, Deblois D, Schwartz SM . RGS5, RGS4, and RGS2 expression and aortic contractibility are dynamically co-regulated during aortic banding-induced hypertrophy. J Mol Cell Cardiol 2008; 44: 539–550.
Xie Z, Gong MC, Su W, Turk J, Guo Z . Group VIA phospholipase A2 (iPLA2β) participates in angiotensin II-induced transcriptional up-regulation of regulator of G-protein signaling-2 in vascular smooth muscle cells. J Biol Chem 2007; 282: 25278–25289.
Acknowledgements
We acknowledge Yukari Kawabata for technical assistance and animal maintenance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Wu, Y., Takahashi, H., Suzuki, E. et al. Impaired response of regulator of Gαq signaling-2 mRNA to angiotensin II and hypertensive renal injury in Dahl salt-sensitive rats. Hypertens Res 39, 210–216 (2016). https://doi.org/10.1038/hr.2015.132
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.132
- Springer Nature Singapore Pte Ltd.
Keywords
This article is cited by
-
A high-salt diet enhances leukocyte adhesion in association with kidney injury in young dahl salt-sensitive rats
Hypertension Research (2017)
-
The angiotensin II receptor antagonist, losartan, enhances regulator of G protein signaling 2 mRNA expression in vascular smooth muscle cells of Wistar rats
Hypertension Research (2016)