Abstract
Hyperactivation of the sympathetic nervous system has an important role in the development and progression of arterial hypertension. This study evaluated the efficacy of etamicastat, a dopamine-β-hydroxylase (DβH) inhibitor, in controlling high blood pressure in the spontaneously hypertensive rat (SHR), either alone or in combination with other classes of antihypertensives. SHRs were administered with etamicastat by gavage, and its pharmacodynamic and pharmacokinetic properties were evaluated. Etamicastat induced a time-dependent decrease in noradrenaline-to-dopamine ratios in the heart and kidney, and had no effect on catecholamine levels in the frontal cortex of SHRs. Cardiovascular pharmacodynamic effects following administration of etamicastat alone or in combination with other classes of antihypertensive drugs were assessed by telemetry. Etamicastat was evaluated in combination with captopril, losartan, hydrochlorothiazide, metoprolol, prazosin and/or diltiazem. Etamicastat monotherapy induced a dose-dependent reduction in blood pressure without reflex tachycardia. Combination therapy amplified the antihypertensive effects of all tested drugs. In conclusion, inhibition of peripheral DβH with etamicastat, as a monotherapy or combination therapy, may constitute a valid alternative treatment for high blood pressure.
Similar content being viewed by others
Introduction
Hypertension is one of the most prevalent conditions worldwide with ~26.4% of the adult population affected in 2000, and it is projected that this will increase to 29.2%, affecting 1.5 billion people by 2025.1
Despite the availability of several pharmacologic agents from different classes to treat hypertension, ~50% of patients do not achieve ideal control of their blood pressure (BP).2 Thus, there remains an unmet clinical need for BP control, and this is of particular importance because hypertension constitutes one of the most important cardiovascular risk factors.3,4
Hyperactivity of the sympathetic nervous system (SNS), which involves increased spillover of noradrenaline (NA) in specific organs, such as heart, kidney and skeletal muscle vasculature, has a major role in the development and progression of hypertension.5, 6, 7 Congestive heart failure physiopathology8,9 has been associated with increased mortality.3,10,11 Recently, catheter-based renal sympathetic denervation (RDN) has been developed for treatment-resistant hypertension.12, 13, 14, 15 Although it has been shown to produce significant and sustained reduction in BP for up to 36 months after denervation,16 limitations to the procedure exist, such as patient eligibility criteria, restricting its use from a broader range of hypertensive patients.17,18
Therefore, alternative strategies to modulate sympathetic nerve function are attractive. Among them, the inhibition of dopamine-β-hydroxylase (DβH), the enzyme responsible for the conversion of dopamine (DA) to NA in sympathetic nerves, has emerged as the most promising.19 DβH inhibition has the advantage of dose adjustment, unlike RDN, and causes a gradual sympathetic slowdown instead of acute inhibition, such as with β-blockers,20 thus decreasing the negative hemodynamic impact.21 DβH inhibition also increases the availability of DA,22,23 which improves renal function by causing renal vasodilatation and inducing diuresis and natriuresis.24, 25, 26 Several DβH inhibitors have been reported thus far,27, 28, 29 but none have received regulatory approval because they were found to have weak potency, poor DβH selectivity and/or significant adverse effects.30 Etamicastat (also known as BIA 5-453; (R)-5-(2-aminoethyl)-1-(6,8-difluorochroman-3-yl)-1,3-dihydroimidazole-2-thione hydrochloride) is a novel reversible DβH inhibitor in development as a new putative drug therapy for cardiovascular disorders that acts by decreasing NA levels in sympathetically innervated tissues.31, 32, 33, 34, 35, 36, 37 Recently, etamicastat was demonstrated to have BP-lowering effects in hypertensive patients.38
A combination of two or more antihypertensive agents from different pharmacologic classes is often needed to achieve adequate BP control because of the multifactorial pathophysiology of hypertension. The current study was designed to evaluate the antihypertensive effects of etamicastat monotherapy, as well as dual combination therapy of etamicastat with six antihypertensive drugs belonging to different pharmacologic classes, in the spontaneously hypertensive rat (SHR), a model of genetic essential hypertension.
Methods
Animals and general procedures
Adult male SHRs (aged 12 weeks), purchased from Charles River Laboratories (Sulzfeld, Germany), were housed in macrolon cages on wood litter with free access to food and water under controlled environmental conditions in a colony room (12 h light/dark cycle, room temperature 22±1 °C and humidity 55±15%). Administrations were performed by single intragastric bolus at a volume of 4 ml kg−1. Carboxymethylcellulose of 0.5% was used as vehicle. All animal procedures conform with the guidelines from Directive 2010/63/EU of the European Parliament on the protection of animals used for scientific purposes and the Portuguese law on animal welfare (Decreto-Lei 113/2013). Etamicastat was synthesized in the Laboratory of Chemistry of BIAL-Portela & Cª, S.A. All other chemicals and materials were purchased from Sigma-Aldrich (St Louis, MO, USA), unless noted otherwise.
Pharmacokinetic evaluation
Pharmacokinetic evaluation was performed in SHRs administered with 30 mg kg−1 etamicastat. Blood was collected from the vena cava (S-Monovette, Sarstedt, Nümbrecht, Germany) of sodium pentobarbital-anesthetized animals (60 mg kg−1, intraperitoneally) at 1, 3, 6, 9, 24 and 48 h after dosing (n=5 per time point). Etamicastat was quantified in plasma by LC-MS/MS (tandem mass spectrometer), as previously described.39
Assay of catecholamines
Heart left ventricle, renal cortex, frontal cortex and parietal cortex from SHRs dosed with 30 mg kg−1 etamicastat were assayed for NA and DA content by high-pressure liquid chromatography coupled to electrochemical detection.40 Samples were collected from sodium pentobarbital-anesthetized animals at 1, 3, 6, 9, 15, 24 and 48 h after dosing (n=5 per time point).
SHRs (n=6 per group) received a bolus of etamicastat (30 mg kg−1) and were placed in individual metabolic cages (Tecniplast, Varese, Italy) for 24 h urine collection. Urinary NA, DA, dihydroxyphenylacetic acid and homovanillic acid quantification was performed by high-pressure liquid chromatography coupled to electrochemical detection.40
Implantable telemetry
SHRs were instrumented with radiotelemeters (TA11PA-C40; DSI, St Paul, MN, USA) as described elsewhere.41 Briefly, rats were anesthetized with sodium pentobarbital, and a 5 cm midline abdominal incision was made. The abdominal aorta was dissected from its surroundings, and the pressure-sensing catheter was implanted into the vessel. For postoperative care, the incision site was covered with 2% lidocaine cream, and carprofen (5 mg kg−1 per day, subcutaneously) was administered for 3 days, two times daily. Animals were allowed to recover individually for 2 weeks before experiments.
Cardiovascular evaluation
Etamicastat monotherapy effect on BP, heart rate (HR) and activity was monitored in conscious telemetry-instrumented SHRs. Rats received an oral bolus of vehicle (0.5% carboxymethylcellulose) or 3, 30 or 100 mg kg−1 etamicastat (n=7).
The six antihypertensive drugs used in dual combination studies were as follows: captopril (an angiotensin-converting enzyme inhibitor, at 30 mg kg−1), losartan (an angiotensin II receptor blocker, at 30 mg kg−1), hydrochlorothiazide (a thiazide diuretic, at 30 mg kg−1), metoprolol (a β-blocker, at 30 mg kg−1), prazosin (an α-1 blocker, at 10 mg kg−1) and diltiazem (a calcium channel blocker, at 30 mg kg−1). Six independent experiments were performed, consisting of the following four groups: vehicle, etamicastat monotherapy, antihypertensive agent monotherapy and dual combination therapy. Drug dosages were the same in monotherapy and combination therapy. The dose of etamicastat was 30 mg kg−1, selected from the monotherapy study. The dose of the selected antihypertensive drugs was determined from the literature.42, 43, 44, 45, 46, 47 In combination therapy, drugs were delivered simultaneously as a single bolus. All experiments were performed in a crossover design with a washout period of 7 days between treatments. Data were recorded for 40 s every 10 min for 72 h and averaged in 6 h intervals using Dataquest A.R.T. acquisition and analysis system 4.0.
Evaluation of renal function
The effect of etamicastat on renal function was evaluated in SHRs (n=4–5 per group) that received a bolus of etamicastat (30 mg kg−1 per day) on three consecutive days and were placed in individual metabolic cages (Tecniplast, Buguggiate, Italy) for urine collection in the last 24 h period. The urine samples were collected in vials that were subsequently stored at −80 °C until assayed. After completion of this protocol, rats were anesthetized with sodium pentobarbital (60 mg kg−1, intraperitoneally). The animals were then killed by exsanguination using cardiac puncture, and the blood was collected into tubes containing K3 EDTA for later determination of plasma biochemical parameters. All biochemical assays were performed by Cobas Mira Plus analyzer (ABX Diagnostics for Cobas Mira, Geneva, Switzerland). Creatinine clearance was calculated using 24 h urine creatinine excretion in absolute values (ml min−1), as previously described.
Statistical analysis
Pharmacokinetic variables were derived by non-compartmental analysis using Prism 5 (GraphPad Software, San Diego, CA, USA) and Microsoft Office Excel 2007. The results are shown as the mean, range and median for tmax. The area under the plasma concentration–time curve (AUC0−t) values were calculated from time zero to the last sampling time at which the concentrations were detected, calculated by the linear trapezoidal rule, and extrapolated to infinity, according to the following equation: AUC0−inf=AUC0−t+Clast/λz, where Clast is the last measurable concentration, and λz is the elimination rate constant, calculated by log-linear regression of terminal segment of plasma concentration vs. time curve, using at least the three last quantifiable concentrations. The terminal half-life t1/2 was calculated from In(2)/λz.
Graphical data are presented as the mean±s.e.m. Data analyses were performed using Prism 5. Data were compared between vehicle and etamicastat (catecholamines) and between monotherapy and combination therapy (overall 72 h mean arterial pressure (MAP)) using Student’s t-test or between vehicle and etamicastat monotherapy, and where applicable, between vehicle, antihypertensive drug monotherapy and combined therapy by repeated-measures two-way analysis of variance followed by Holm–Sidak post hoc analysis for pairwise comparisons (telemetry studies). P-values <0.05 were considered statistically significant.
Results
Pharmacokinetic evaluation
Plasma etamicastat disposition was evaluated after oral administration to SHRs. As depicted in Figure 1, etamicastat was rapidly absorbed and reached the maximum concentration (Cmax) of 1.3 (1.1–1.4) μg ml−1 between 1 and 3 h following administration. Exposure to etamicastat declined rapidly until 8 h after dosing and then slowly decreased over the next time points. At 48 h after dosing, no etamicastat was observed in circulation. The half-life of etamicastat in plasma was 4.6 (1.6–7.2) h and the AUC0−t obtained was 10.2 (9.9–10.9) μg·h ml−1.
Catecholamine levels
DβH inhibition increases DA levels and reduces NA. Therefore, we determined the NA-to-DA ratios to evaluate the degree of DβH inhibition following oral etamicastat administration. As shown in Figure 2, etamicastat treatment induced a long-lasting reduction of the NA-to-DA ratios in the heart and kidney. Ratio values remained below 15% of vehicle values between 6 and 24 h after dosing. Maximal reduction of NA-to-DA ratios was 7.8±0.9% of vehicle values at 24 h after dosing and 7.8±0.6% of vehicle values at 9 h after dosing in heart left ventricle and renal cortex, respectively. By contrast, etamicastat treatment did not change the NA-to-DA ratios in the frontal cortex and had a limited effect in the parietal cortex (57.3±5.7% of vehicle values at 6 h after dosing).
Time course of noradrenaline (NA)-to-dopamine (DA) ratios in frontal cortex, parietal cortex, heart left ventricle and renal cortex of spontaneously hypertensive rats (SHRs) after oral administration of 30 mg kg−1 etamicastat. Significant differences are shown for vehicle corresponding values in vehicle-treated animals (*P<0.05). Data are the mean±s.e.m. (n=5 per time point).
The urinary excretion of catecholamines was evaluated as the 24 h cumulative amount of NA, DA, dihydroxyphenylacetic acid and homovanillic acid. As depicted in Figure 3, etamicastat treatment significantly increased the urinary levels of DA (vehicle: 17.6±1.6; etamicastat: 35.8±3.1 nmol; P=0.0004) as well as the levels of the DA metabolites dihydroxyphenylacetic acid (vehicle: 51.3±3.8; etamicastat: 141.3±12.0 nmol; P<0.0001) and homovanillic acid (vehicle: 154.1±12.4; etamicastat: 501.3±78.3 nmol; P=0.0014). The 24 h NA urinary excretion (vehicle: 4.4±0.9; etamicastat: 3.0±0.4 nmol; P=0.20) and volume output (vehicle: 6.3±0.8; etamicastat: 9.3±1.8 ml; P=0.16) were not different between vehicle- and etamicastat-treated animals. It should be noted that the catecholamine time-profile modulation showed a maximal reduction of the NA-to-DA ratios in renal tissue 9 h after dosing, which may explain why total 24 h urinary cumulative NA amount did not achieve statistical significance.
Effect of oral administration of 30 mg kg−1 etamicastat on 24 h urinary excretion of (a) noradrenaline, (b) dopamine, (c) dihydroxyphenylacetic acid (DOPAC) and (d) homovanillic acid (HVA) in spontaneously hypertensive rats (SHRs). Significantly different from vehicle corresponding values in vehicle-treated animals (*P<0.05). Data are the mean±s.e.m. (n=6 per group).
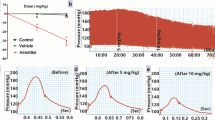
Etamicastat monotherapy dose-dependently decreases BP
The effect of etamicastat monotherapy upon systolic BP (SBP), diastolic BP (DBP), HR and home-cage activity was monitored in a crossover design during 72 h. SHRs (n=7) were orally administered with vehicle or etamicastat (3, 30 and 100 mg kg−1). As shown in Figure 4, over the 72 h observation period, etamicastat treatment produced a dose-dependent mean decrease in SBP of −6.2±3.2 mm Hg (P=0.0150), −9.5±1.6 mm Hg (P=0.0012) and −18.4±2.7 mm Hg (P<0.0001) from a vehicle baseline of 188.6±2.6 mm Hg for the 3, 30 and 100 mg kg−1 dose, respectively. In addition, etamicastat treatment led to a dose-dependent reduction in the SBP of −11.0±3.2 mm Hg at 9 h after dosing with 3 mg kg−1, −22.3±2.6 mm Hg at 15 h after dosing with 30 mg kg−1 and −29.4±4.2 mm Hg at 21 h after dosing with 100 mg kg−1.
Dose and time profile of (a) systolic blood pressure, (b) diastolic blood pressure, (c) heart rate and (d) home-cage activity of spontaneously hypertensive rats (SHRs) after oral administration of 3, 30 or 100 mg kg−1 etamicastat (Etam). Significantly different from vehicle corresponding values in vehicle-treated animals (*P<0.05). Data are shown as the mean±s.e.m. (n=7). The light gray areas indicate the 12 h dark cycle.
Etamicastat monotherapy also produced a significant average decrease in DBP of −8.5±4.1 mm Hg (P=0.0360) with 30 mg kg−1 dose and −13.9±4.5 mm Hg (P=0.0015) with 100 mg kg−1 dose from vehicle basal DBP of 133.7±5.1 mm Hg (Figure 4). The drop in DBP attained with the lowest dose of etamicastat was not different from vehicle-treated SHRs (−4.7±3.3 mm Hg, P=0.2). The peak effect on DBP was a reduction of −8.2±4.2 mm Hg at 9 h after dosing (3 mg kg−1), −18.8±4.4 mm Hg at 15 h after dosing (30 mg kg−1) and −23.4±6.4 mm Hg at 21 h after dosing (100 mg kg−1).
The overall (72 h) mean SBP and DBP decrease with increasing single administration of etamicastat (3, 30 and 100 mg kg−1) is depicted in Table 1.
No effect of etamicastat monotherapy on the 72 h mean HR or home-cage activity was observed (all P>0.05).
Effects of etamicastat on the renal function
Treatment with etamicastat (30 mg kg−1 per day) for three consecutive days had no effect on urinary Na+ and K+ levels (Table 2). Creatinine clearance did not differ between vehicle- and etamicastat-treated animals.
Combination therapy of etamicastat with antihypertensive drugs further decreases BP
Combination therapy was assessed in SHRs in a crossover design during a 72 h period, as described in the Methods section. As shown in Figure 5, combination studies evaluated the antihypertensive effect of etamicastat alone and in combination with captopril, losartan, hydrochlorothiazide, metoprolol, prazosin and/or diltiazem. The overall (72 h) MAP decrease with the different drugs and drug combinations is depicted in Table 3. In addition, the statistical analysis concerning the comparison between each antihypertensive drug monotherapy and the corresponding combination with etamicastat is provided in Table 3.
Effect of etamicastat in combination with six antihypertensive drugs in spontaneously hypertensive rats (SHRs) on change from vehicle values (Δ) of mean arterial pressure and heart rate. (a) Etamicastat/captopril (n=4), (b) etamicastat/losartan (n=4), (c) etamicastat/hydrochlorothiazide (n=4), (d) etamicastat/metoprolol (n=8), (e) etamicastat/prazosin (n=8) and (f) etamicastat/diltiazem (n=5). The doses used were (mg kg−1, per os) etamicastat, 30; captopril, 30; losartan, 30; hydrochlorothiazide, 30; metoprolol, 30; prazosin, 10; and diltiazem, 30. Data are shown as the mean±s.e.m. The light gray areas indicate the 12 h dark cycle.
Etamicastat/captopril combination
The antihypertensive effect of the ACE inhibitor captopril was tested alone and in combination with etamicastat. As shown in Figure 5a, captopril alone produced a decrease in the 72 h average MAP of −9.0±5.5 mm Hg from a baseline value of 147.5±4.2 mm Hg without effects on HR (P=0.7). Owing to the prompt antihypertensive effect of captopril, the overall 72 h MAP was not different from vehicle-treated rats (P=0.1). The maximal reduction in MAP was −17.6±7.3 mm Hg at 3 h after dosing (P<0.0001). Combination therapy induced a superior reduction in the 72 h average MAP of −14.3±3.2 mm Hg (P=0.0253), with a maximum drop in MAP of −21.3±6.1 mm Hg at 15 h after treatment (P<0.0001). There was no effect of etamicastat/captopril treatment in the 72 h mean HR (P=0.7).
Etamicastat/losartan combination
The effect of losartan on MAP and HR is depicted in Figure 5b. Losartan produced a 72 h mean reduction in MAP of −17.3±1.5 mm Hg (P<0.0001) compared with vehicle MAP of 148.4±3.6 mm Hg, without effects on HR (P=0.2). The maximal drop in MAP of −24.5±2.5 mm Hg (P<0.0001) was observed at 33 h after dosing. Administration of etamicastat plus losartan led to a marked drop in 72 h MAP of −25.7±2.9 mm Hg (P<0.0001), with a major BP decreasing effect of −35.6±4.8 mm Hg (P<0.0001) at 27 h after administration without effects on HR (P=0.4).
Etamicastat/hydrochlorothiazide combination
The effect of hydrochlorothiazide on MAP and HR is shown in Figure 5c. The 72 h MAP after the administration of hydrochlorothiazide was not different (−4.6±3.9 mm Hg, P=0.3) from corresponding values in vehicle-treated animals (153.1±4.8 mm Hg). No effect upon HR was observed (P=0.6). The maximal MAP reduction in hydrochlorothiazide-treated SHRs was −11.1±4.8 mm Hg (P=0.0042) at 21 h after dosing. Etamicastat amplified the antihypertensive effect of hydrochlorothiazide, with a 72 h period drop in MAP of −15.6±2.2 mm Hg (P=0.0083). The peak antihypertensive effect was observed at 21 h after dosing and produced a drop in MAP of −27.5±3.5 mm Hg (P<0.0001). Combination therapy had no further effect on HR (P=0.9).
Etamicastat/metoprolol combination
The antihypertensive effect of the β-blocker metoprolol is shown in Figure 5d. The 72 h MAP reduction was −1.1±2.0 mm Hg (P=0.6), with a peak effect of −10.5 mm Hg (P<0.0001) 3 h after dosing, compared with the vehicle value of 147.1±2.4 mm Hg. No effects on HR were observed (P=0.6). The combination of etamicastat plus metoprolol produced a significant drop in the 72 h MAP of −9.7±2.3 mm Hg (P=0.0017). The etamicastat/metoprolol combination produced a maximal reduction in MAP of −18.1±4.7 (P<0.0001) at 3 h after dosing (Figure 5d) without effects on 72 h mean HR (P=0.4).
Etamicastat/prazosin combination
The α-1 blocker prazosin produced a significant reduction in 72 h MAP (−3.1±0.6 mm Hg, P=0.0012) and an increase in HR (17.8±2.3 b.p.m., P<0.0001). Vehicle MAP and HR were 153.4±2.8 mm Hg and 310.1±4.2 b.p.m., respectively. The maximal effect on MAP was observed at 9 h after dosing (−16.5±0.9 mm Hg, P<0.0001). Prazosin transiently increased heart rate, with a peak effect at 3 h after dosing (63.2±6.4 b.p.m., P<0.0001). The combination of etamicastat plus prazosin produced a further drop in the 72 h MAP (−11.9±1.2, P<0.0001), with a maximal effect of −26.1±1.7 mm Hg at 9 h after dosing. Nevertheless, the combination therapy effect on HR was similar to the one observed with prazosin alone (17.0±3.9 b.p.m., P<0.0001), with a maximal increase of 55.9±9.6 b.p.m. at 3 h after treatment (Figure 5e).
Etamicastat/diltiazem combination
The calcium channel blocker diltiazem induced a very short reduction in MAP with a maximal effect 1 h after treatment of −15.6±9.3 mm Hg (P=0.0018) and no effect on overall MAP (1.5±1.9 mm Hg, P=0.3) or HR (P=0.6). Conversely, combination of etamicastat plus diltiazem produced a significant 72 h mean decrease in MAP of −7.9±1.4 mm Hg (P=0.0006) from a vehicle MAP of 154.6±5.7 mm Hg. The combination therapy peak drop in MAP was of −13.8±3.4 mm Hg (P<0.0001) at 21 h after dosing (Figure 5f). No effect on HR was observed (P=0.3).
Overall, as depicted in Figure 6, coadministration of etamicastat with captopril, losartan, hydrochlorothiazide, metoprolol, prazosin and/or diltiazem in SHRs potentiated the antihypertensive effects of all classes of antihypertensive test drugs.
Etamicastat-potentiated antihypertensive effects of captopril, losartan, hydrochlorothiazide, metoprolol, prazosin and/or diltiazem in spontaneously hypertensive rats. The doses used were (mg kg−1, per os) etamicastat, 30; captopril, 30; losartan, 30; hydrochlorothiazide (HCTZ), 30; metoprolol, 30; prazosin, 10; and diltiazem, 30. The X axis represents the change in mean arterial pressure induced by the combination, expressed as a percentage of the sum of changes induced by each drug in the 72 h mean period after administration; n=4–8 for each point.
Discussion
In the present study, we addressed the antihypertensive effect of etamicastat, a new reversible long-acting DβH inhibitor, with limited access to the brain and improved potency and selectivity compared with other DβH inhibitors thus far reported in the literature.19,36 Etamicastat acts mainly at the periphery by decreasing NA-to-DA ratios in sympathetically innervated tissues (Figures 2 and 3). Furthermore, etamicastat-dependent peripheral sympathetic downregulation results in decreases in BP without significant reflex tachycardia (Figure 4) and renal function (Table 2) in the SHR. It is interesting to highlight the finding that despite marked increases in urinary dopamine, etamicastat failed to affect renal function, and its BP-decreasing effects were not accompanied by natriuresis in the SHR. However, this is in line with the view that the SHR is a genetic model of hypertension characterized by the resistance to the natriuretic effect of dopamine and D1-like receptor agonists, as a result of a defective transduction of the D1 receptor signal in renal proximal tubules.26,48 However, the BP-decreasing effect of etamicastat in the SHR correlates well with the NA time-profile modulation in peripheral sympathetically innervated tissues.
The etamicastat sympatholytic and antihypertensive effects were assessed following a single intragastric bolus dose. Nonetheless, data presented here are in agreement with previous work from our laboratory showing that chronic etamicastat treatment (in drinking water) produces a sustained peripheral sympatholytic effect and decreases BP in SHRs for up to 8 months with no adverse effects and devoid of reflex tachycardia.49
Recently, catheter-based renal denervation for treatment-resistant hypertension has been developed. RDN produces significant and sustained reduction of BP for up to 36 months after denervation.16 Nevertheless, limitations to the procedure exist, such as patient eligibility criteria, restricting its use from a broader range of hypertensive patients.17,18 Etamicastat treatment, like RDN, is able to decrease BP through a downregulation of the SNS; however, DβH inhibition has the additional benefit of dose modulation and reversibility upon discontinuation. Moreover, it should be noted that RDN has a target-specific effect on renal sympathetic nerves,50 whereas DβH inhibition by etamicastat has a more widespread effect on peripheral SNS.
Despite the availability of generalized effective antihypertensive drugs, nearly half of hypertensive patients do not achieve goal BP, most often because of SBP persistent elevation.2 Although antihypertensive therapies decrease both SBP and DBP, drugs targeting the renin–angiotensin system, diuretics and α-1 blockers act primarily through a decrease in systemic vascular resistance, either by a decrease in body fluid volume or an increase in peripheral vasodilatation. This mechanism-of-action may partially explain the difficulty to achieve optimal SBP. Therefore, the use of DβH inhibitors may constitute a new tool against hypertension because it gradually decreases NA release from sympathetic nerves with a subsequent decline in both α- and β-adrenergic receptor activation. Indeed, the use of adrenoceptor blockers to inhibit the sympathetic drive proved to be a valuable therapeutic approach. However, the abrupt withdrawal of sympathetic tone may cause hemodynamic deterioration in some patients, particularly those with some degree of heart failure.51 Furthermore, DβH inhibition may show additional benefits by increasing dopamine availability,22,23 which improves renal function by causing renal vasodilatation, diuresis and natriuresis.24, 25, 26
According to the 2013 ESH/ESC guidelines for the management of arterial hypertension, monotherapy can effectively reduce BP in only a limited number of hypertensive patients, and most patients require the combination of at least two drugs to achieve BP control. Furthermore, combining two agents from any two classes of antihypertensive drugs increases BP reduction much more than increasing the dose of one agent.4 Therefore, in the present study we evaluated the antihypertensive efficacy of etamicastat in combination with six antihypertensive drugs belonging to different pharmacologic classes. The results presented here showed that combination therapy amplified the antihypertensive effect over monotherapy in SHRs (Figures 5 and 6). Captopril and losartan provide a partial blockade of renin–angiotensin system that, together with an SNS modulator, operates cooperatively in regulating cardiovascular disorders.52 Increasing renin–angiotensin system activity contributes to vasoconstriction, sodium and water retention, increasing cardiac contractility, cardiomyocyte hypertrophy, aldosterone synthesis, NA release, oxidative stress and inflammation. Because both renin–angiotensin system and SNS are implicated in the pathophysiology of hypertension, it is reasonable to assume that coadministration of drugs that selectively inhibit each of these systems (e.g., etamicastat and captopril or losartan) may further improve the antihypertensive effects. Indeed, here, we showed that etamicastat potentiates the antihypertensive effects of captopril and losartan.
The majority of currently available fixed-dose combinations are based on the use of diuretic therapies.53 In the present work, hydrochlorothiazide, a thiazide-type diuretic, was used in combination with etamicastat. Hydrochlorothiazide inhibits the renal NaCl cotransporter, leading to sodium and water excretion and reduced plasma volume. In the SHR, etamicastat increased the BP-lowering effect of hydrochlorothiazide. Interestingly, etamicastat gradually decreased BP, whereas metoprolol had immediate BP-lowering effects, most likely due to their distinct mechanisms of sympathoinhibition. In contrast to etamicastat, β-blockers produce immediate occupation of adrenoceptors, leading to abrupt withdrawal of sympathetic tone with a complete recovery to baseline over 24 h in SHRs. Likewise, a similar effect on BP was observed for the α-1 blocker prazosin. Furthermore, prazosin produced a significant transient reflex tachycardia in the first 24 h after administration. Although etamicastat could not prevent the transient increase in pulse rate induced by prazosin, it did not intensify the tachycardia, even if it amplified the antihypertensive effects. Diltiazem targets the L-type voltage-dependent calcium channel, stopping the influx of calcium into the cells. In vascular smooth muscle cells, this causes vasodilatation and a resultant decrease in BP. The antihypertensive effect of diltiazem in the SHR was prompt, occurring in the first hours after dosing. Nonetheless, coadministration of etamicastat with diltiazem further enhanced the lowering effect on BP.
Overactive SNS has been implicated in the development and progression of several cardiovascular diseases through increased sympathetic outflow to the heart, kidney and skeletal muscle vasculature. This study supports the use of peripheral DβH inhibitors as a promising approach for the treatment of cardiovascular disorders, such as hypertension and chronic heart failure, for which a reduction in NA levels may be of therapeutic benefit.
Recently, etamicastat was demonstrated in hypertensive patients to have very promising BP-lowering effects with no clinically or statistically relevant changes in HR.38 Despite the relatively small sample size (5 or 6 patients in each dose group) and the short treatment period (10 days), a dose-dependent decrease in both SBP and DBP was apparent after 10 days of treatment. The observed decrease attained statistical significance vs. placebo in nighttime SBP for all etamicastat doses (50, 100 and 200 mg per day). The results of a detailed meta-analysis of 147 randomized trials of BP reduction showed that, regardless of BP before treatment, lowering SBP by 10 mm Hg or DBP by 5 mm Hg significantly reduces coronary events and stroke without increases in nonvascular mortality.54 However, it should be underscored that nighttime BP is a better predictor than daytime BP, and nocturnal BP may be a target to reduce cardiovascular morbidity and mortality in hypertensive patients.55
References
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J . Global burden of hypertension: analysis of worldwide data. Lancet 2005; 365: 217–223.
Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, White A, Cushman WC, White W, Sica D, Ferdinand K, Giles TD, Falkner B, Carey RM . Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension 2008; 51: 1403–1419.
Malpas SC . Sympathetic nervous system overactivity and its role in the development of cardiovascular disease. Physiol Rev 2010; 90: 513–557.
Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F Task Force Members. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31: 1281–1357.
Grassi G . Sympathetic neural activity in hypertension and related diseases. Am J Hypertens 2010; 23: 1052–1060.
Grassi G, Seravalle G, Quarti-Trevano F . The 'neuroadrenergic hypothesis' in hypertension: current evidence. Exp Physiol 2010; 95: 581–586.
Esler M, Kaye D . Sympathetic nervous system activation in essential hypertension, cardiac failure and psychosomatic heart disease. J Cardiovasc Pharmacol 2000; 35 (Suppl 4): S1–S7.
Parati G, Esler M . The human sympathetic nervous system: its relevance in hypertension and heart failure. Eur Heart J 2012; 33: 1058–1066.
Grassi G, Bolla G, Quarti-Trevano F, Arenare F, Brambilla G, Mancia G . Sympathetic activation in congestive heart failure: reproducibility of neuroadrenergic markers. Eur J Heart Fail 2008; 10: 1186–1191.
Lee CS, Tkacs NC . Current concepts of neurohormonal activation in heart failure: mediators and mechanisms. AACN Adv Crit Care 2008; 19: 364–385.
Mancia G, Grassi G, Giannattasio C, Seravalle G . Sympathetic activation in the pathogenesis of hypertension and progression of organ damage. Hypertension 1999; 34 (Pt 2): 724–728.
Krum H, Schlaich M, Whitbourn R, Sobotka PA, Sadowski J, Bartus K, Kapelak B, Walton A, Sievert H, Thambar S, Abraham WT, Esler M . Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet 2009; 373: 1275–1281.
Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, Bohm M . Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet 2010; 376: 1903–1909.
Worthley SG, Tsioufis CP, Worthley MI, Sinhal A, Chew DP, Meredith IT, Malaiapan Y, Papademetriou V . Safety and efficacy of a multi-electrode renal sympathetic denervation system in resistant hypertension: the EnligHTN I trial. Eur Heart J 2013; 34: 2132–2140.
Mahfoud F, Ukena C, Schmieder RE, Cremers B, Rump LC, Vonend O, Weil J, Schmidt M, Hoppe UC, Zeller T, Bauer A, Ott C, Blessing E, Sobotka PA, Krum H, Schlaich M, Esler M, Böhm M . Ambulatory blood pressure changes after renal sympathetic denervation in patients with resistant hypertension. Circulation 2013; 128: 132–140.
Krum H, Schlaich MP, Sobotka PA, Bohm M, Mahfoud F, Rocha-Singh K, Katholi R, Esler MD . Percutaneous renal denervation in patients with treatment-resistant hypertension: final 3-year report of the Symplicity HTN-1 study. Lancet 2013; 383: 622–629.
Mahfoud F, Luscher TF, Andersson B, Baumgartner I, Cifkova R, Dimario C, Doevendans P, Fagard R, Fajadet J, Komajda M, Lefèvre T, Lotan C, Sievert H, Volpe M, Widimsky P, Wijns W, Williams B, Windecker S, Witkowski A, Zeller T, Böhm M European Society of Cardiology. Expert consensus document from the European Society of Cardiology on catheter-based renal denervation. Eur Heart J 2013; 34: 2149–2157.
Hayek SS, Abdou MH, Demoss BD, Legaspi JM, Veledar E, Deka A, Krishnan SK, Wilmot KA, Patel AD, Kumar VR, Devireddy CM . Prevalence of resistant hypertension and eligibility for catheter-based renal denervation in hypertensive outpatients. Am J Hypertens 2013, 1452–1458.
Stanley WC, Li B, Bonhaus DW, Johnson LG, Lee K, Porter S, Walker K, Martinez G, Eglen RM, Whiting RL, Hegde SS . Catecholamine modulatory effects of nepicastat (RS-25560-197), a novel, potent and selective inhibitor of dopamine-beta-hydroxylase. Br J Pharmacol 1997; 121: 1803–1809.
Bertera FM, Del Mauro JS, Lovera V, Chiappetta D, Polizio AH, Taira CA, Höcht C . Acute effects of third generation beta-blockers on short-term and beat-to-beat blood pressure variability in sinoaortic-denervated rats. Hypertens Res 2013; 36: 349–355.
Hegde SS, Friday KF . Dopamine-beta-hydroxylase inhibition: a novel sympatho-modulatory approach for the treatment of congestive heart failure. Curr Pharm Des 1998; 4: 469–479.
Soares-da-Silva P . Evidence for a non-precursor dopamine pool in noradrenergic neurones of the dog mesenteric artery. Naunyn Schmiedebergs Arch Pharmacol 1986; 333: 219–223.
Soares-da-Silva P . A comparison between the pattern of dopamine and noradrenaline release from sympathetic neurones of the dog mesenteric artery. Br J Pharmacol 1987; 90: 91–98.
Gomes P, Soares-da-Silva P . Dopamine. In Michael Bader (ed.). Cardiovascular Hormone Systems: From Molecular Mechanisms to Novel Therapeutics. Wiley-Blackwell: Weinheim, Germany. 2008, pp 251–293.
Jose PA, Eisner GM, Felder RA . Role of dopamine receptors in the kidney in the regulation of blood pressure. Curr Opin Nephrol Hypertens 2002; 11: 87–92.
Jose PA, Soares-da-Silva P, Eisner GM, Felder RA . Dopamine and G protein-coupled receptor kinase 4 in the kidney: role in blood pressure regulation. Biochim Biophys Acta 2010; 1802: 1259–1267.
Ishii Y, Fujii Y, Mimura C, Umezawa H . Pharmacological action of FD-008, a new dopamine beta-hydroxylase inhibitor. I. Effects on blood pressure in rats and dogs. Arzneimittelforschung 1975; 25: 55–59.
Kruse LI, Kaiser C, DeWolf WE Jr, Frazee JS, Ross ST, Wawro J, Wise M, Flaim KE, Sawyer JL, Erickson RW . Multisubstrate inhibitors of dopamine beta-hydroxylase. 2. Structure-activity relationships at the phenethylamine binding site. J Med Chem 1987; 30: 486–494.
Ohlstein EH, Kruse LI, Ezekiel M, Sherman SS, Erickson R, DeWolf WE Jr, Berkowitz BA . Cardiovascular effects of a new potent dopamine beta-hydroxylase inhibitor in spontaneously hypertensive rats. J Pharmacol Exp Ther 1987; 241 (2): 554–559.
Kruse LI, Kaiser C, DeWolf WE Jr, Frazee JS, Erickson RW, Ezekiel M, Ohlstein EH, Ruffolo RR Jr, Berkowitz BA . Substituted 1-benzylimidazole-2-thiols as potent and orally active inhibitors of dopamine beta-hydroxylase. J Med Chem 1986; 29: 887–889.
Falcao A, Nunes T, Rocha JF, Almeida L, Soares-da-Silva P . Comparative bioavailability study of etamicastat (BIA 5-453) under fasted and fed conditions. J Clin Pharmacol 2009; 49: 1095 (abstract).
Nunes T, Rocha JF, Vaz-da-Silva M, Falcao A, Almeida L, Soares-da-Silva P . Pharmacokinetics and tolerability of etamicastat following single and repeated administration in elderly versus young healthy male subjects: an open-label, single-center, parallel-group study. Clin Ther 2011; 33: 776–791.
Nunes T, Rocha JF, Vaz-da-Silva M, Igreja B, Wright LC, Falcão A, Almeida L, Soares-da-Silva P . Safety, tolerability, and pharmacokinetics of etamicastat, a novel dopamine-beta-hydroxylase inhibitor, in a rising multiple-dose study in young healthy subjects. Drugs R D 2010; 10: 225–242.
Rocha JF, Vaz-da-Silva M, Nunes T, Igreja B, Loureiro AI, Bonifácio MJ, Wright LC, Falcão A, Almeida L, Soares-da-Silva P . Single-dose tolerability, pharmacokinetics, and pharmacodynamics of etamicastat (BIA 5-453), a new dopamine {beta}-hydroxylase inhibitor, in healthy subjects. J Clin Pharmacol 2012; 52: 156–170.
Vaz-da-Silva M, Nunes T, Rocha JF, Falcao A, Almeida L, Soares-da-Silva P . Effect of food on the pharmacokinetic profile of etamicastat (BIA 5-453). Drugs R D 2011; 11: 127–136.
Beliaev A, Learmonth DA, Soares-da-Silva P . Synthesis and biological evaluation of novel, peripherally selective chromanyl imidazolethione-based inhibitors of dopamine beta-hydroxylase. J Med Chem 2006; 49: 1191–1197.
Bonifácio MJ, Igreja B, Wright L, Soares-da-Silva P . Kinetic studies on the inhibition of dopamine-ß-hydroxylase by BIA 5-453. pA2 Online 2009; 7: 050P (abstract).
Almeida L, Nunes T, Costa R, Rocha JF, Vaz-da-Silva M, Soares-da-Silva P . Etamicastat, a novel dopamine beta-hydroxylase inhibitor: tolerability, pharmacokinetics, and pharmacodynamics in patients with hypertension. Clin Ther 2013; 35: 1983–1996.
Loureiro AI, Fernandes-Lopes C, Bonifacio MJ, Wright LC, Soares-da-Silva P . N-acetylation of etamicastat, a reversible dopamine-beta-hydroxylase inhibitor. Drug Metab Dispos 2013; 41: 2081–2086.
Soares-da-Silva P, Pestana M, Vieira-Coelho MA, Fernandes MH, Albino-Teixeira A . Assessment of renal dopaminergic system activity in the nitric oxide-deprived hypertensive rat model. Br J Pharmacol 1995; 114: 1403–1413.
Huetteman DA, Bogie H . Direct blood pressure monitoring in laboratory rodents via implantable radio telemetry. Methods Mol Biol 2009; 573: 57–73.
Clough DP, Hatton R, Keddie JR, Collis MG . Hypotensive action of captopril in spontaneously hypertensive and normotensive rats. Interference with neurogenic vasoconstriction. Hypertension 1982; 4: 764–772.
Narita H, Nagao T, Yabana H, Yamaguchi I . Hypotensive and diuretic actions of diltiazem in spontaneously hypertensive and Wistar Kyoto rats. J Pharmacol Exp Ther 1983; 227: 472–477.
Wada T, Sanada T, Ojima M, Kanagawa R, Nishikawa K, Inada Y . Combined effects of the angiotensin II antagonist candesartan cilexetil (TCV-116) and other classes of antihypertensive drugs in spontaneously hypertensive rats. Hypertens Res 1996; 19: 247–254.
DePasquale MJ, Fossa AA, Holt WF, Mangiapane ML . Central DuP 753 does not lower blood pressure in spontaneously hypertensive rats. Hypertension 1992; 19 (Part 2): 668–671.
Antonaccio MJ, High J, DeForrest JM, Sybertz E . Antihypertensive effects of 12 beta adrenoceptor antagonists in conscious spontaneously hypertensive rats: relationship to changes in plasma renin activity, heart rate and sympathetic nerve function. J Pharmacol Exp Ther 1986; 238: 378–387.
Ryan MJ, Bjork FA, Cohen DM, Coughenour LL, Major TC, Mathias NP, Mertz TE, Olszewski BJ, Singer RM, Evans DB CI-926 (3-[4-[4-(3-methylphenyl)-1-piperazinyl]butyl]-2,4-imidazolinedione): antihypertensive profile and pharmacology. J Pharmacol Exp Ther 1986; 238: 473–479.
Jose PA, Eisner GM, Felder RA . Dopamine and the kidney: a role in hypertension? Curr Opin Nephrol Hypertens 2003; 12: 189–194.
Igreja B, Wright L, Soares-da-Silva P . Sustained antihypertensive effects of a selective peripheral dopamine-ß-hydroxylase inhibitor. Hypertension 2007; 50: E133 (abstract).
Foss JD, Fink GD, Osborn JW . Reversal of genetic salt-sensitive hypertension by targeted sympathetic ablation. Hypertension 2013; 61: 806–811.
Pfeffer MA, Stevenson LW . Beta-adrenergic blockers and survival in heart failure. New Engl J Med 1996; 334: 1396–1397.
Goldsmith SR . Interactions between the sympathetic nervous system and the RAAS in heart failure. Curr Heart Fail Rep 2004; 1: 45–50.
Kalra S, Kalra B, Agrawal N . Combination therapy in hypertension: an update. Diabetol Metab Syndr 2010; 2: 44.
Law MR, Morris JK, Wald NJ . Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009; 338: b1665.
Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML, De Bacquer DA . Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension 2008; 51: 55–61.
Acknowledgements
This work was supported by BIAL—Portela & Cª, S.A.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
BI, NMP, MJB, AIL, CF-L, LCW and PS-d-S are or were employees of BIAL—Portela & Cª, S.A. (the sponsor of the study) at the time of the study.
Rights and permissions
About this article
Cite this article
Igreja, B., Pires, N., Bonifácio, M. et al. Blood pressure-decreasing effect of etamicastat alone and in combination with antihypertensive drugs in the spontaneously hypertensive rat. Hypertens Res 38, 30–38 (2015). https://doi.org/10.1038/hr.2014.143
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.143
- Springer Nature Singapore Pte Ltd.
Keywords
This article is cited by
-
Acute salt loading induces sympathetic nervous system overdrive in mice lacking salt-inducible kinase 1 (SIK1)
Hypertension Research (2019)
-
New Molecules for Treating Resistant Hypertension: a Clinical Perspective
Current Hypertension Reports (2019)
-
Emerging Therapy in Hypertension
Current Hypertension Reports (2019)
-
Antihypertensive effect of etamicastat in dopamine D2 receptor-deficient mice
Hypertension Research (2018)
-
Blood pressure decrease in spontaneously hypertensive rats folowing renal denervation or dopamine β-hydroxylase inhibition with etamicastat
Hypertension Research (2015)