Abstract
Purpose
To evaluate safety and long-term recurrence rate of entropion in patients having everting sutures (ES) for involutional entropion by ophthalmic nurses in a real clinical setting.
Patients and methods
Retrospective notes review of all patients who had an outpatient ES by our trained ophthalmic nurses over 2 year’s time period. Outcome measures were complication and recurrence rates. Those with less than 3 years' recorded follow-up were contacted by paper questionnaire.
Results
90 lids of 82 patients analysed. Mean age was 78 (range 54–97). In total, 82% had no entropion surgery before, whereas 13% had previous ES and 5% one or more other procedures. Questionnaires were sent to 38, with return rate of 81%. Recurrence rate was 21.1% after 36–60 months follow up from nurse-performed ES, with mean time to recurrence of 15 months (SD 13 months). A total of 32% of patients died during the follow-up period. Mean time between the procedure and death is 20.5 months. When ES were repeated twice (11 patients), recurrence rate was still 20%. No patients had any complications.
Conclusion
ES can be safely performed by ophthalmic nurses, with success rate comparable to the same technique performed by ophthalmologists.
Similar content being viewed by others
Introduction
Involutional entropion represents a significant proportion of the oculoplastic work-load. Its prevalence in the community is thought to be around 2.4% in those above 60 years old.1 Previous studies have established that surgical methods that address horizontal lid laxity provide longer-lasting entropion correction than everting sutures (ES) alone.2, 3 Various techniques have been described and all of them are more complex than ES and utilise more theatre time. ES is a low cost and simple method that is reproducible in the hands of operators with different surgical experience.4 It can be provided in the outpatient clinic on patients’ first visit and does not require stopping antiplatelet medication. Allowing appropriately trained ophthalmic nurses to deliver this service could reduce costs provided safety and efficacy can be demonstrated and patients informed of alternatives to permit informed consent. This service was introduced in our unit in 2007 with the aim of improving treatment for entropion patients in a catchment region of around 650 000 population with only one oculoplastic surgeon. Three senior nurses were trained by a single consultant to perform ES under a local anaesthetic. Patients referred with entropion were then triaged into nurse-led minor operations clinics run in parallel to a consultant-led oculoplastic clinic; these nurses were then able to perform same day ES in a procedure room. The nurse performed a history and examination, and the diagnosis of entropion confirmed by the oculoplastic consultant or registrar before the nurse proceeded to obtain informed consent and perform the ES. The nurses usually performed one to two ES procedures per clinic, alongside other minor operations such as incision and curettage of chalazia. No other scrub nurse was utilised, but a health care assistant supported the clinic. In this paper we aim to establish the safety and long-term outcome of this procedure performed by our ophthalmic nurses.
Subjects and methods
Retrospective notes review of all patients having outpatient ES by our ophthalmic nurses in Aberdeen Royal Infirmary, UK, from 2007–2008 inclusive. Permission and support obtained from NHS Grampian Clinical Effectiveness Team. Total procedures recorded in the minor operations room logbook were 98 eyes for 88 patients. One patient was treated twice due to a recurrence, so was counted only once. Medical notes for five patients (seven lids) who had died were destroyed therefore inaccessible; since it was not possible to confirm any clinical details, the patients were excluded. After excluding those with inaccessible notes/ duplication 90 eyes for 82 patients remained and were analysed. The outcome measures were complications and recurrence rates. Case notes of all patients were reviewed and for those who had been seen by an ophthalmology doctor in the clinic for any reason (for example, cataract) within the 36-month minimum requirement, the last recorded examination of the lid was taken. Those who had not had this minimum follow-up, and were still alive, were sent a questionnaire to ask them if they had recurrence of symptoms, and those with recurrent symptoms were invited to clinic for examination.
In total, 44 of the 82 patients analysed (54%) either had 3 years’ recorded follow-up or were confirmed to have died; thus 38 (46%) patients (41 lid procedures) were identified as having insufficient clinical follow-up and were sent a postal questionnaire enquiring whether they were aware of any recurrence of entropion and whether they had relevant symptoms. The response rate was 81.5% (31 of 38 patients). Four recurrences were identified in this way, three of which had already been recognised as having recurrence from reviewing the notes. One patient thought she had a recurrence and was keen to be seen in the clinic. When seen in the clinic, the recurrence was excluded and her symptoms were due to blepharitis/ dry eyes. One patient was not sure if there was a recurrence but declined to re-attend clinic.
Surgical method
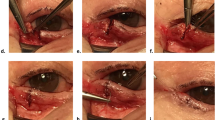
Anaesthesia was performed with topical oxybuprocaine 0.4% and subcutaneous injections of 2–3 ml of lidocaine with 1:200 000 adrenaline. The technique used was essentially the same as described by Wright et al,4 with substitution of vicryl for catgut (which is no longer available in the UK). Three double-ended 4/0 vicryl sutures were used. This suture was chosen as it was relatively easy to handle for nurses with limited previous experience in microsurgical suturing. Each needle was passed through the conjunctival fornix in a mattress fashion, picking up the inferior retractors before rotating antero-superiorly in front of the lower tarsus to exit the skin just below the lash line. The knot was tightened to create a very slight initial over correction (a small lid margin ectropion). Sutures were only placed in the lateral three quarters of the lower lid to avoid punctal ectropion, and spaced evenly in this part of the lid. Sutures were left to dissolve. Topical chloramphenicol was prescribed three times a day for 1 week. Patients were offered 6 weeks' follow-up appointment in the nurse-led minor ops clinic at which time any residual sutures were removed only if there was related irritation or over correction.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Results
Baseline characteristics of the study population summarised in Table 1.
In total, 18 out of 90 entropion recurred giving a recurrence rate from all patients’ records alone of 20%. Those who died in the follow-up period were analysed according to their last recorded examination. Questionnaires sent to surviving patients with <3 years of recorded follow-up identified one extra case of recurrence, giving a total recurrence rate of 21.1% (Figure 1) with a follow-up period of 36–60 months. The mean time to recurrence was 15 months (SD 13; range 6 weeks–3 years). There were no complications and no identified ectropion.
A total of 29 patients (32%) died during the follow-up period with mean time between procedure and death of 20.5 months (SD14; Range 3–59 months).
Patients who had had ES for recurrent entropion (11 lids with sufficient follow-up were treated following recurrence after previous ES and patients opted to have repeat ES) also showed a recurrence rate of 20%. However, 50% of those who had ES twice died within the follow-up period. It should be noted that patients with recurrent entropion were offered more formal entropion repair in theatre but opted for further ES due to factors such as unwillingness to wait for treatment or to make further journeys to the hospital, and as such might represent a more frail group than those opting for other surgical treatments.
Of patients within the study period who had recurrence, nine chose to have further outpatient ES, two went on to have lateral tarsal strip (LTS), two had Jones procedure, one had Wedge resection, one had hard palate graft, one became unfit for surgery due to severe dementia, two been referred to surgery but died in the interim and one was not interested in further follow up.
Discussion
Most of the evidence we have on entropion surgery comes from case series. A Cochrane review published in 20115 and a more recent review6 identified only one high level study that compares ES with a more modern technique, and the methodology of even this study was assessed by the Cochrane group as containing some risk of bias.5 The high level study was that of Scheepers et al2 who performed a randomised controlled trial comparing ES alone with LTS combined with ES. Doctors performed all treatments in their study. Their recurrence rate was 21 and 0% respectively. Therefore their recurrence rate for ES performed by doctors was the same as ours for ES performed by Ophthalmic nurses. Table 2 list some of the later published studies that looked at success rate of ES compared with other procedures or alone.
In all of the above studies, ophthalmologists at various levels of training performed ES. Our study evaluated ES performed by ophthalmic nurses. The success rate in our study is comparable to most other studies, with only Wright et al4 having a higher success rate. Another study in China showed a recurrence rate of 11% however it was not included in the table as it excluded patients with horizontal Lid laxity and the mean follow up was 9 months only.7 The low complications rate of the procedure noted in previous studies was also demonstrable in our results.
Involutional entropion is a disease of older people therefore it is reasonable to consider life expectancy and patients’ preferences when counselling patients prior to their surgery. Almost one third of patients in our study died during the follow-up period. Wright et al4 made a similar observation.
The pathophysiology of involutional entropion classically described as a triad of lower lid retractors dehiscence, horizontal lid laxity and overriding of the orbicularis oculi.6 Numerous studies demonstrate that techniques addressing all these anatomical problems especially horizontal lid laxity (for example, through LTS, Quickert method which includes horizontal lid shortening or Lower Eyelid Retractor Advancement with or without LTS) have a higher success rate than ES alone2, 3, 5, 6, 8, 9, 10, 11 and we do not dispute this finding. However, demands on theatre time and oculoplastic expertise are high and resources limited in many NHS ophthalmology services. Patients with entropion are usually elderly and in discomfort, and desire rapid resolution of the problem. Nurse-led ES can therefore save valuable resources and provide a faster and safe service to patients. We found that providing this service in parallel to the oculoplastic clinic allowed exclusion of non-involutional types of entropion, and the offer of ES as first-line treatment at the initial visit for patients with uncomplicated involutional entropion was an option that most of our patients chose to take even when counselled about the higher recurrence rate compared with other entropion procedures that we could offer in day-case theatres.
In conclusion, ES can be safely performed by ophthalmic nurses, with success rates comparable to the same technique performed by ophthalmologists. A nurse-led ES service can benefit patients and save resources such as operating theatre time.

References
Damasceno RW, Osaki MH, Dantas PE, Belfort R Jr . Involutional entropion and ectropion of the lower eyelid: prevalence and associated risk factors in the elderly population. Ophthal Plast Reconstr Surg 2011; 27 (5): 317–320.
Scheepers MA, Singh R, Ng J, Zuercher D, Gibson A, Bunce C et al. A randomized controlled trial comparing everting sutures with everting sutures and a lateral tarsal strip for involutional entropion. Ophthalmology 2010; 117 (2): 352–355.
Rougraff PM, Tse DT, Johnson TE, Feuer W . Involutional entropion repair with fornix sutures and lateral tarsal strip procedure. Ophthal Plast Reconstr Surg 2001; 17 (4): 281–287.
Wright M . Everting suture correction of lower lid involutional entropion. Br J Ophthalmol 1999; 83 (9): 1060–1063.
Boboridis KG, Bunce C . Interventions for involutional lower lid entropion. Cochrane Database Syst Rev 2011; (12): CD002221.
Marcet MM, Phelps PO, Lai JSM . Involutional entropion: risk factors and surgical remedies. Curr Opin Ophthalmol 2015; 26: 416–421.
Tsang S, Yau GS, Lee JW, Chu AT, Yuen CY . Surgical outcome of involutional lower eyelid entropion correction using transcutaneous everting sutures in Chinese patients. Int Ophthalmol 2014; 34 (4): 865–868.
Boboridis K, Bunce C, Rose GE . A comparative study of two procedures for repair of involutional lower lid entropion. Ophthalmology 2000; 107 (5): 959–961.
Danks JJ, Rose GE . Involutional lower lid entropion: to shorten or not to shorten? Ophthalmology 1998; 105 (11): 2065–2067.
Lance SE, Wilkins RB . Involutional entropion: a retrospective analysis of the Wies procedure alone or combined with a horizontal shortening procedure. Ophthal Plast Reconstr Surg 1991; 7 (4): 273–277.
Barnes JA, Bunce C, Olver JM . Simple effective surgery for involutional entropion suitable for the general ophthalmologist. Ophthalmology 2006; 113 (1): 92–96.
Meadows AE, Reck AC, Gaston H, Tyers AG . Everting sutures in involutional entropion. Orbit 1999; 18 (3): 177–181.
Jang SY, Choi SR, Jang JW, Kim SJ, Choi HS . Long-term surgical outcomes of Quickert sutures for involutional lower eyelid entropion. J Craniomaxillofac Surg 2014; 42: 1629–1631.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Mohammed, B., Ford, R. Success rate of nurse-led everting sutures for involutional lower lid entropion. Eye 31, 732–735 (2017). https://doi.org/10.1038/eye.2016.314
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2016.314
- Springer Nature Limited
This article is cited by
-
Pretarsal orbicularis oculi muscle tightening with skin flap excision in the treatment of lower eyelid involutional entropion
BMC Ophthalmology (2021)
-
Randomized Controlled Trial Comparing Everting Sutures with a Lateral Tarsal Strip for Involutional Lower Eyelid Entropion
Ophthalmology and Therapy (2019)