Abstract
Apoptosis, an important innate immune mechanism that eliminates pathogen-infected cells, is primarily triggered by two signalling pathways: the death receptor pathway and the mitochondria-mediated pathway. However, many viruses have evolved various strategies to suppress apoptosis by encoding anti-apoptotic factors or regulating apoptotic signalling pathways, which promote viral propagation and evasion of the host defence. During its life cycle, α-herpesvirus utilizes an elegant multifarious anti-apoptotic strategy to suppress programmed cell death. This progress article primarily focuses on the current understanding of the apoptosis-inhibition mechanisms of α-herpesvirus anti-apoptotic genes and their expression products and discusses future directions, including how the anti-apoptotic function of herpesvirus could be targeted therapeutically.
Similar content being viewed by others
Facts
-
Apoptosis plays an important and critical role in host defence mechanisms against viral infection.
-
Viruses, including α-herpesviruses, encode anti-apoptotic virulence factors to evade elimination via apoptosis and to guarantee viral replication and propagation.
-
Multiple signalling pathways, including the intrinsic and extrinsic pathways, form a complicated network to modulate apoptosis.
-
Different viral anti-apoptotic genes have distinct mechanisms of mediating apoptosis.
Open Questions
-
In other evolving immune pathways, such as the autophagy and NF-κB signalling pathways, what is the role of viral anti-apoptotic genes, and how do they interact with established protein networks?
-
Can we properly exploit viral anti-apoptotic proteins as targets for antiviral drugs?
Herpesvirus
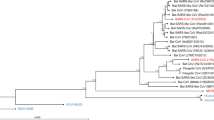
α-Herpesviruses are responsible for severe morbidity and mortality, and they are characterized by a complex enveloped virion and a double-stranded DNA genome. They typically lyse productively infected cells and establish a reactivatable, latent infection in their hosts. Furthermore, α-herpesviruses have a relatively broad host range.1 The human α-herpesviruses include herpes simplex virus types 1 and 2 (HSV-1 and HSV-2) and varicella zoster virus (VZV). Moreover, there are several veterinary α-herpesviruses, including bovine herpesvirus (BHV), pseudorabies virus (PRV) and duck plague virus.
Structure
The α-herpesvirus genomes range in size from approximately 120 to 180 kb, and their G+C nucleotide content ranges from 32 to 75%.2, 3, 4 The herpesvirus genomes are specified as type A, B, C, D or E genomes (Figure 1).5, 6, 7 Morphologically, herpesvirus virions share the similar strategy (Figure 1). The diameter of the virion is approximately 150–200 nm. The capsid consists of 162 capsomeres, containing 150 hexons of one protein species, 11 pentons of another protein and one portal vertex. There are three mature capsid forms A, B and C, which represent empty capsids, scaffold-containing capsids and viral DNA-containing capsids, respectively.8 The lipid envelope is derived from host cellular membranes and contains several viral membrane glycoproteins.5, 9 The glycoproteins have roles in adsorption, binding to the cell surface, and promoting fusion between the virion envelope and the cellular membrane.10
Overview of the types of herpesvirus genomes and the structure of virion. (I) The type A genomes (e.g., EHV-2) consist of a unique (U) region that is flanked by a direct terminal repeat (TR). The type B structure (e.g., Kaposi’s sarcoma-associated herpesvirus) also consists of a U region flanked by variable numbers of TRs. The type C genomes (e.g., Epstein-Barr virus) harbour variable numbers of terminal sequences and an internal direct repeat that is unrelated to the TR and splits the U region into two unique regions (UL and Us). The type D (e.g., PRV) and E (e.g., HSV-1) genomes contain UL and US regions that are each flanked by terminal and internal inverted repeats (TRL/IRL and IRS/TRS). The TRL/IRL regions are very short in some type D genomes (e.g., VZV), whereas they are longer in viruses with class E genomes. In the type E structure, there is also a terminal direct repeat of hundreds of base pairs that is known as the a sequence. Moreover, an inverted copy, known as the a’ sequence, is present internally. (II) The structure consists of four elements: (1) a core containing the viral dsDNA; (2) a T=16 icosahedral capsid encircling the core; (3) an amorphous protein layer called the tegument that surrounds the capsid; and (4) an outer lipid envelope (some inspiration came from these articles5, 6, 7, 9, 10)
Life cycle
The three subfamilies of herpesviruses share many strategies for replication. The two characteristic replication modes include a rapid, productive replication cycle and a life-long quiescent infection.
The lytic replication cycle
Understanding of the lytic replication cycle comes primarily from studies of HSV-1 and PRV.11, 12, 13 Consequently, this cycle includes (1) entry into the cell, (2) the transfer of the capsids to the nucleus and viral DNA replication, (3) capsid assembly and egress from the nucleus, (4) the maturation and envelopment of viral particles in the cytoplasm and (5) the exocytosis of mature virions (Figure 2).
The lytic replication cycle of herpesviruses: (1) entry into the cell, (2) transfer of the capsids to the nucleus, (3) viral DNA replication, (4) capsid assembly, (5) egress from the nucleus, (6) maturation and envelopment of viral particles in the cytoplasm and (7) exocytosis of mature virions (some inspiration came from these articles11, 12, 13, 14, 20, 23)
The α-herpesviruses attach to and then enter the cells of exposed mucosal surfaces to initiate infection. Depending on the cell type, virion entry can occur at either the plasma membrane or via endosomes after endocytosis.14, 15 In the primary mechanism, viral surface glycoproteins interact with cell-specific receptors to promote membrane fusion. Some of glycoproteins are involved in regulating apoptosis.16, 17
Upon fusion between the viral envelope and the cytomembrane, unenveloped virions enter the cytoplasm. Subsequently, capsids are transferred via microtubules to nuclear pores; motor proteins associated with microtubules are recruited through the exposure of inner tegument proteins, such as pUS3.18 Then, the viral genomes enter the nucleus through the nuclear pores and replicate. Herpesvirus gene expression can be divided into three types: immediate-early (IE or α), early (E or β) and late (L or γ). Functionally, IE genes, including ICP0, ICP4, ICP22 and ICP27, are the first genes transcribed; the transcription is stimulated by the viral tegument protein VP16 and uses the host transcriptional apparatus. The E gene-encoded proteins, independently of viral DNA replication, can be activated by IE gene expression. Based on the strictness of the DNA replication requirement, L genes are subdivided into leaky (γ1) late and true late (γ2).12, 19 Additionally, herpesviruses also produce some non-coding RNAs and microRNAs that regulate the stability of viral and cellular mRNAs.
Subsequently, the DNA circularizes rapidly, and replication proceeds though a rolling circle mechanism. After expressing capsid proteins, herpesviruses assemble capsids and package their genomes into them. Unlike other DNA viruses, herpesviruses cannot obliterate nuclear membranes for their release.20 The viral capsids are too large (at least 120 nm) to pass through nuclear pores. Therefore, for egress, capsids are wrapped in the inner nuclear membrane (INM) and bud into the perinuclear space where they form primary enveloped capsids. During this process, the α-herpesvirus kinase pUS3 can regulate capsid nuclear egress by phosphorylating lamin A/C, which composes the nuclear lamina.21 Next, the perinuclear-enveloped capsids fuse with the outer nuclear membrane (ONM), and unenveloped capsids are delivered into the cytoplasm in a process called de-envelopment. Although gD is required for fusion during viral entry and is found in the perinuclear particles at the INM/ONM, gD deletion has no detectable effect on egress.22
A few tegument proteins, such as VP16 and VP22, are packaged in the nucleus, and others are added in the cytoplasm. In the cytoplasm, tegument-coated capsids are budded into specialized vesicles derived from the Golgi and endosomes. In this secondary envelopment process, not only are mature viruses produced but also the transport vesicles that later fuse with the plasma membrane to release the viruses.23 In secondary envelopment, the assembly of tegument and envelope is a complex process that involves numerous protein-protein interactions.20, 23 Enveloped virions, packaged into transport vesicles, can promote cell-to-cell spread or transport into neuronal axons for transmission to peripheral tissues.
Latency and reactivation
Importantly, all α-herpesviruses establish a latent infection in the neurons of the peripheral nervous system, which establishes a high-density viral reservoir and evades host antiviral defences.24, 25, 26 After viral replication at the portal of entry, α-herpesviruses concurrently invade the nervous system via fusion with neuronal membranes at axonal termini. Once the viral DNA has entered the nuclei in a ganglion, α-herpesviruses are immediately silenced and assembled into a chromatin structure resembling heterochromatin, which favours virus survival and establishes latent infection.27 In latently infected neurons, latency-associated transcript (LAT), which can silence lytic gene expression and block apoptosis, is the only gene expressed in high abundance.28
However, these mechanisms have been studied primarily with HSV-1. Different stimuli, such as fever, UV light and menstruation, can reactivate α-herpesviruses. Biologically, α-herpesviruses are reactivated by one of the following two conditions: (a) infection with a high viral genome load to overcome repression or (b) the translocation of key tegument proteins, such as VP16, to the nucleus where it derepresses viral DNA.27 Once reactivation has occurred, viral capsids are transported to the distal axon, where virions are assembled.11, 29
Apoptosis
Apoptosis, also called programmed cell death, is a process that is common to all multicellular organisms for eliminating cells via a complex but highly defined programme. Apoptotic cells are characterized by nuclear fragmentation, cell shrinkage and the formation of apoptotic bodies.30 Virus-induced apoptosis can limit viral replication and transmission. Although apoptosis contributes to the prevention of pathogenesis, it is a potentially costly and even vainly attempted self-sacrifice.31, 32
Notably, viruses have evolved anti-apoptotic mechanisms to maintain their replication and propagation.33 To escape elimination via apoptosis, viruses target and regulate key regulatory steps in the apoptotic pathway; they can inhibit death receptor-mediated apoptotic signals, regulate mitochondrial permeability and suppress the caspase cascade.34, 35, 36 Moreover, viruses can inhibit apoptosis by regulating the pro-apoptotic tumour suppressor p53.37
α-Herpesvirus can encode anti-apoptotic viral proteins, such as US3, gJ and LAT, to interfere with the apoptosis pathway.36 Understanding the mechanisms by which α-herpesvirus regulates apoptosis is useful for future research. In this article, we focus on reviewing the roles played by α-herpesvirus proteins in suppressing apoptosis.
The apoptotic pathway
Apoptosis is modulated by two signalling pathways – the intrinsic and the extrinsic pathways. The extrinsic pathway, also called the death receptor pathway, is regulated by membrane death receptors, which are activated by binding between a ligand and its receptor.38 Conversely, the intrinsic pathway is modulated by intracellular stimuli, such as oxidative stress, hypoxia and nutrient deprivation, which lead to mitochondrial outer membrane permeabilization (MOMP). Subsequently, cytochrome C is released into the cytoplasm.39, 40 Both pathways can activate the enzymatic cysteine-specific aspartate protease (caspase) cascade, triggering numerous proteolytic events that mediate the apoptotic cell death programme.40 The underlying mechanisms of apoptosis are now being unravelled. We will review the intrinsic and extrinsic signalling pathways to better understand the mechanisms by which α-herpesvirus perturbs apoptosis.
The extrinsic pathway
The extrinsic apoptotic pathway is a process in which specific ligands or apoptotic signals bind to membrane death receptors (DRs) to initiate apoptosis (Figure 3). These DRs belong to the TNF superfamily. To date, the eight TNF superfamily receptors CDl20a (p55/TNFR1), CDl20b (TNFR2), CD95 (Fas/ApoI), DR3, DR4 (TRAILR1), DR5 (TRAILR2), NGFR and EDAR have been identified in this process.41 Fas and TNFR1, the representative receptors, can bind with Fas ligand (FasL) and tumour necrosis factor-related apoptosis-inducing ligand (TRAIL), respectively, to form a death-inducing signalling complex (DISC) and activate a caspase cascade.42, 43
The extrinsic apoptosis pathway. (a) Fas and DR4/5 are activated by the binding of their respective ligands FasL and TRAIL; the receptors then bind to FADD via the death domain (DD). Then, the death effector domain (DED) of FADD binds to procaspase-8/10, forming the death-inducing signalling complex (DISC) to facilitate the autoproteolytic cleavage of procaspase-8/10, which induces the activation of the caspase cascade and ultimately results in apoptosis. (b) In particular cells, activated caspase-8 cleaves the pro-apoptotic protein Bid to create truncated Bid (tBid), and this results in the activation of the mitochondria-mediated apoptotic signalling pathway. (c) TNFR1, EDAR and DR3/6 are activated by the binding of their respective ligands. TNFR1 recruits TRADD, an adaptor protein that binds to TNF receptor-associated factors (TRAFs), receptor-interacting protein kinase (RIP1) and cellular inhibitor of apoptosis (cIAPs), forming the initial membrane pro-survival complex (complex I), which stimulates the MAPK/JNK and NF-κB pathways to facilitate cell survival or apoptosis. (d) Complex I forms two types of cytoplasmic apoptotic complexes, TRADD-dependent complex IIA and RIP1-dependent complex IIB, which activate caspase-8, thus initiating apoptosis (some inspiration came from these articles47, 48, 49, 50, 51, 52)
Mediated by FADD
Fas-associated protein with death domain (FADD), an apoptosis-related adaptor protein, is composed of a death domain (DD) and a death effector domain (DED).44 Fas, DR4 and DR5 are activated by specific ligands and bind to FADD through the DD domain. Then, the DED of FADD binds to procaspase-8/10 to construct the DISC. The DISC promotes the autoproteolytic cleavage of procaspase-8/10.45 The activation of caspase-8/10, which have enzymatic activity, can hydrolyse caspase-3/6/7 to induce apoptotic conditions, including cell shrinkage, nuclear fragmentation, apoptotic DNA fragmentation and ultimate cell death.44, 46, 47, 48, 49
Mediated by TRADD
TNFR1-associated death domain protein (TRADD), an adaptor molecule, transduces the signal downstream of TNFR1, and TRADD contains a DD. Other death receptors, including TNFR1, DR3, DR6 and EDAR, recruit TRADD, which links DRs to TRAF2 (TNF receptor-associated factor 2), RIP (receptor-interacting protein kinase) and cIAPs (cellular inhibitor of apoptosis), forming a signalling complex named complex I.41, 49 TRADD interacts with TRAF2 via its N-terminal TRAF2-binding domain and with RIP via the DD. The initial formation of the membrane pro-survival TRADD–RIP1–TRAF2 complex I is followed by the assembly of a cytoplasmic apoptotic complex (complex II). There are two types of cytosolic complex II. FADD and caspase-8 are recruited by TRADD to form TRADD-dependent complex IIA, and RIP1 recruits FADD and caspase-8 into complex IIB, which can be negatively regulated by cIAPs. Both complex IIA and IIB can initiate apoptosis by activating caspase-8.44, 50, 51 Additionally, complex I stimulates the mitogen-activated protein kinase/c-Jun N-terminal kinase (MAPK/JNK) pathway to induce cell survival, proliferation or apoptosis, and it modulates the nuclear factor kappa B (NF-κB) pathway, which facilitates cell survival, inflammatory signalling and apoptosis.50, 52
The intrinsic pathway
The intrinsic pathway, or the mitochondria-mediated apoptotic pathway (Figure 4), is initiated by intracellular stimuli that trigger MOMP, which allows the release of cytochrome C from mitochondria and is closely regulated by the Bcl-2 family.53 Bcl-2 family proteins are divided into pro-apoptotic proteins (Bax, Bid, Bak, Bad) and anti-apoptotic proteins (Bcl-2, Bcl-xl, Mcl-1, A1). A slight change in the dynamic balance of these proteins leads to apoptosis or apoptosis inhibition.54, 55, 56
The intrinsic apoptosis pathway. The intrinsic apoptotic pathway is triggered by intracellular stimuli. (a) Intracellular apoptotic stimuli upregulate the pro-apoptotic Bcl-2 family of proteins, such as Bax, Bid, Bak and Bad, leading to the mitochondrial release of cytochrome C, which binds to Apaf-1. The replacement of ADP by dATP/ATP in Apaf-1 triggers the formation of a heptameric apoptosome, which assembles with procaspase-9 to form the holo-apoptosome. The Apaf-1 apoptosome catalyses the cleavage and activation of procaspase-9, which triggers the caspase cascade, and the activation of caspase-3 and caspase-7 leads to eventual apoptosis. (b) Under ER stress, three upstream signalling proteins – IRE1, PERK and ATF6 – are activated, thus leading to a cascade of activity that induces apoptosis. (b1) The ER releases Ca2+ from the ER lumen into the cytoplasm, which triggers apoptosis by activating the calcium-sensing kinase CaMKII. Then, CaMKII activates procaspase, which in turn triggers caspase cascade activation. (b2) The prolonged activation of IRE1 can promote apoptosis. Phosphorylated IRE1 recruits TRAF2 (TNF receptor-associated factor 2) and triggers a cascade of phosphorylation events, such as the activation of ASK1 (apoptosis signalling kinase 1), which ultimately phosphorylates and activates JNK. Then, JNK phosphorylation activates pro-apoptotic Bim and blocks anti-apoptotic Bcl-2. (b3) The homomultimerization and autophosphorylation of PERK leads to eIF-2α (eukaryotic translation initiation factor 2α) phosphorylation, which increases the translation of ATF4 (activating transcription factor-4). Then, ATF4 upregulates the expression of CHOP (C/EBP-homologous protein), which promotes apoptosis through two of the major cell death pathways – the IP3R–Ca2+–CaMKII pathway and the Bcl-2 family member pathway (some inspiration came from these articles56, 57, 58, 59, 60, 61)
Pro-apoptotic Bcl-2 family members respond to a variety of intracellular apoptotic stimuli and then form pores in the outer mitochondrial membrane through which cytochrome C, which is normally bound to the inner mitochondrial membrane, is released into the cytoplasm.57 The released cytochrome C binds to Apaf-1 via β-propellers, and it then triggers nucleotide exchange and the gradual assembly of the apoptosome.58 The Apaf-1 and procaspase-9 caspase recruitment domains (CARDs) co-assemble to form a CARD–CARD disk, thus assembling the holo-apoptosome, which creates an asymmetric proteolysis machine. Each holo-apoptosome can recruit five to seven procaspase-9 molecules by interacting with the N-terminal CARDs of Apaf-1.59 The tethered catalytic domains of multiple procapase-9 molecules result in the activation of zymogen, which cleaves procaspase-9. Subsequently, caspase-9 triggers the caspase cascade, and then the activation of caspase-3/7 executes apoptosis.53, 58
Furthermore, chronic or unresolved endoplasmic reticulum (ER) stress, which can be caused by increased protein synthesis or misfolding rates and alterations in Ca2+ stores, is involved in the mitochondrial apoptotic pathway.60 Under ER stress, the ER-specific unfolded protein response is triggered through IRE1 (inositol requiring protein-1), PERK (protein kinase RNA-like ER kinase) and ATF6 (activating transcription factor-6) apoptotic pathways, which are connected to the mitochondria-mediated apoptotic pathway.61
The Anti-apoptotic Genes of α-herpesvirus
To evade elimination, α-herpesviruses have gradually evolved various host immune modulation strategies to promote their fitness and pathogenesis. Although cells infected with viruses can be eliminated by cellular apoptosis, viruses can also suppress this apoptosis by encoding anti-apoptotic virulence factors. Here, we review the current understanding of the apoptosis-inhibiting mechanisms of the α-herpesvirus anti-apoptotic genes and their expression products (Table 1).
LAT and its mechanism of apoptosis regulation
During the latent stage, LAT is the only highly transcribed viral gene. LAT enhances the establishment of latency, reactivates the virus from latency and protects the host cells from apoptosis.62, 63 Moreover, HSV-1 LAT can inhibit capase-8/9-mediated apoptosis stimulated through either the intrinsic or extrinsic pathway.64, 65, 66, 67
The anti-apoptotic mechanisms of LAT are being unravelled (Figure 5). Stable cell lines expressing LAT can block caspase-3 activation, thus confirming that LAT can suppress apoptosis even in the absence of other HSV-1 genes.28 HSV-1 LAT can stabilize the levels of total and phosphorylated AKT protein, which phosphorylates and inactivates the pro-apoptotic proteins Bad, Bax and caspase-9, to regulate caspase-3 activation and ultimately block apoptosis.68, 69 In addition, a stable cell line expressing LAT can recover from cold-shock-induced apoptosis, which supports the notion that LAT can inhibit the dephosphorylation of pAKT and stabilize phosphorylated AKT.70 Furthermore, the inhibition of pAKT dephosphorylation by LAT promotes cell survival and virus latency by protecting against the cleavage of caspase-2/3/9 and increasing the ratio of Bcl-2/Bcl-xl (or Bcl-2/tBid).70
The anti-apoptotic pathway of LAT. The main domain of the LAT gene is contained in the first 1.5 kb. LAT can inhibit apoptosis by interacting with the following pathways: (a) LAT stabilizes the levels of total and phosphorylated AKT protein, which phosphorylates and inactivates the pro-apoptotic proteins Bad, Bax and caspase-9 to ultimately regulate caspase-3 activation and block apoptosis; (b) LAT cooperates with RIG-1 to promote NF-κB-dependent transcription to interfere with apoptosis and benefit cell survival; and (c) LAT substitutes for the function of c-FLIP, which is an inhibitor of caspase-8-mediated apoptosis
Additionally, LAT inhibits apoptosis by blocking GrB- and Fas-mediated caspase-3 cleavage, which protects Neuro2A and C1300 cells against cytotoxic CD8 T-cell-mediated death.71 The cellular FLICE-like inhibitory protein (c-FLIP), an inhibitor of caspase-8-mediated apoptosis, can substitute for LAT to enhance the reactivation phenotype.72 Furthermore, downregulating c-FLIP expression via small interfering RNA markedly promoted apoptosis in uninfected immature dendritic cells, and its function could be replaced by LAT.73 Thus, LAT either inhibits multiple steps in apoptotic cascades or regulates AKT and pAKT levels to promote cell survival.
HSV-1 LAT is an 8.3-kb gene, and splicing yields two forms – a stable 2-kb LAT and an unstable 6.3-kb LAT. The first 1.5 kb of the primary 8.3-kb LAT has anti-apoptotic activity,66 and it contains eight open reading frames (ORFs) based on sequence analysis. Point mutation of six ATGs in the intron reduces the anti-apoptotic effect on caspase-9 but not on caspase-8, whereas mutating the two ATGs in the exon does not completely eliminate the anti-apoptotic activity that affects caspase-8/9.74 The first 1.5 kb of LAT encodes two small RNAs (sRNA1 and sRNA2) of 62 nt and 36 nt, respectively, and they cooperate to block apoptosis.75 They also cooperate with RIG-1 to promote NF-κB-dependent transcription to inhibit apoptosis and benefit cell survival.76
Notably, HSV-2 LAT also shows anti-apoptotic activity. ORF1, ORF2, and ORF3 of HSV-2 LAT protect Vero cells from apoptosis induced by actinomycin D (ActD), 5-FU and cisplatin, respectively,77, 78, 79, 80 but the underlying mechanism remains elusive. Similarly, BHV-1 latency-related RNA (LR-RNA) encodes two microRNAs and a protein (ORF2) that can protect cells from stress-induced apoptosis by stimulating NF κB and activating AKT.81
ICP22 and its mechanism of apoptosis regulation
Infection cell protein 22 (ICP22), an IE protein, is required for efficient replication in restrictive cells and the conventional expression of viral late proteins. HSV-1 US1 encodes the 420-amino-acid protein ICP22 and produces an in-frame, N-terminally truncated form of ICP22 called US1.5, which contains 273 amino acids.48, 82 US1.5 becomes detectable and accumulates only at a later time point after infection.83 It is generally believed that ICP22 not only promotes apoptosis but also inhibits apoptosis. The pro-apoptotic function is thought to be regulated by US1.5, which activates caspase-3.83
The ICP22-deleted HSV-1 induces more apoptotic cells, demonstrating that ICP22 can block apoptosis.67 Moreover, ActD-induced apoptosis can be blocked by transfecting a pEGFP-ICP22 plasmid.84 Nevertheless, the anti-apoptotic activity of ICP22 is not strong. Thus, ICP22-mediated anti-apoptosis is not likely acting directly on apoptotic signalling but instead precisely regulates the expression of viral early and late genes, including anti-apoptotic genes. For example, in the absence of ICP22, the expression of US5 is delayed.85
Additionally, cells infected with HSV-1 d120 (an apoptosis inducer), which blocks the ICP4 and US3 genes, show an additional product known as Mr 37 500, which results from the proteolytic cleavage of ICP22 by caspase-3. Furthermore, this process is suppressed by over-expressing Bcl-2, transfecting US3 or adding caspase-3 inhibitor.86 During viral infection, viral protein cleavage by caspases leads to a variety of consequences, such as the counteraction of apoptosis, the enhancement or weakening of replication and the spread of the virus.87 Furthermore, ICP22 can antagonize p53. p53 is a master factor in the cell that modulates various cellular pathways and controls apoptosis by activating Bax or inhibiting Bcl-2.88 p53 has dual effects on HSV-1 replication; it plays a positive role by enhancing ICP27 expression and a negative role by inhibiting ICP0 expression. The negative effect of p53 is suppressed through interaction with ICP22, which promotes cell survival and efficient replication.89 However, it remains unclear whether ICP22 can directly regulate apoptosis by interacting with p53.
VZV causes diseases of the skin or mucosa in a similar fashion as HSV-1. Moreover, VZV ORF63, which encodes the immediate-early protein 63 (IE63) and shares homology with HSV-1 ICP22, can also block apoptosis.90, 91 VZV ORF63-deleted VZV-infected human neurons demonstrate significantly increased apoptosis compared with neurons infected with the parental VZV. Furthermore, expressing ORF63 alone can inhibit apoptosis, showing that VZV can encode an anti-apoptotic gene.92 Compared with parental virus, ORF63-deleted VZV has higher levels of phosphorylated eIF-2α to promote apoptosis. Meanwhile, the expression of IE63 alone can be sufficient to block eIF-2α phosphorylation.93 Thus, like its homologue HSV-1 ICP22, VZV ORF63 can inhibit apoptosis, but it acts through exceedingly different mechanisms.
ICP27 and its mechanism of apoptosis regulation
Infection cell protein 27 (ICP27) is an IE protein that is indispensable for viral replication. Interestingly, ICP27 is the only IE protein that has homologues in all of the herpesviruses. ICP27 is a multifunctional protein that performs various activities during the viral life cycle,94, 95 such as shutting down host protein synthesis,96 promoting viral DNA synthesis and expression,97, 98 orchestrating all stages of viral mRNA biogenesis,99, 100 activating stress signalling pathways101 and blocking apoptosis.102
Based on studies comparing an HSV-1 ICP27-deletion virus with a wild-type virus, ICP27 was shown to block apoptosis.102, 103, 104 Moreover, ICP27-null virus-induced apoptosis in HEp-2 cells is closely associated with the activation of caspase-3.104 A succession of viral ICP27 mutants revealed that encompassing 20–65 amino acids near the N-terminus are required for p38 and modest JNK signalling activation.105, 106 However, the C-terminus can indirectly inhibit apoptosis by increasing the expression of anti-apoptotic genes, such as, gJ and gD.85, 105, 107
Moreover, expressing ICP27 can directly activate p38 signalling and partially activate JNK signalling.108 Additionally, ICP27-mediated JNK signalling during HSV-1 infection induces the activation of NF-κB, which is associated with the inhibition of apoptosis.109, 110 Interestingly, the region from amino acids 21 to 63 is also required for IκBα stabilization.109 ICP27 suppresses the phosphorylation and ubiquitination of IκBα, thus stabilizing IκBα and inhibiting NF-κB activity, which progressively blocks apoptosis.101
Furthermore, as a multifunctional protein, ICP27 is not only an inhibitor of apoptosis but is also capable of triggering cell death. Using chemical inhibitors, it was shown that the ICP27-mediated activation of p38 signalling can stimulate the apoptotic pathways.108 However, during a viral infection, p38 also mediates the destabilization of Bcl-2 to prevent apoptosis; this process also requires ICP27 expression.111 ICP27 might alternate between pro- and anti-apoptotic activity by changing the Bax/Bcl-2 ratio in the course of reactivation from a latent state.112 To summarize, ICP27 is an important regulator of host cell fate. It promotes maximum viral replication in the early phase of infection and greatly enhances viral release in the late stage.
US3 and its mechanism of apoptosis regulation
US3 is represented by ORF3 in the US region of the herpesvirus genome, and it encodes a serine/threonine protein kinase that is highly conserved throughout the α-herpesvirus subfamily. US3-encoded proteins have an ATP binding domain and a catalytic active site in the kinase domain.113 Although the US3 protein kinase (PK) is not required for viral replication, it can regulate the biological functions of the virus and the host cells. For example, US3 PK is involved in the egress of nucleocapsids,114 the maturation of virions,21, 115 enhancing viral spread,116 rearranging the actin cytoskeleton117 and evading antiviral responses.118 US3 PK can block apoptosis induced by viral infection, the overexpression of Bcl-2 family proteins, cytochrome C release and Fas/UV-mediated apoptosis.119, 120, 121, 122, 123
US3 regulation of the intrinsic pathway
Expressing US3 suppresses the release of cytochrome C and the activation of procaspase-3 in HEp-2 cells infected with HSV-1 d120 mutant, thus blocking apoptosis at the pre-mitochondrial stage.124, 125 Furthermore, active US3 PK also phosphorylates procaspase-3 to enhance apoptosis resistance.125 These studies indicate that US3 PK may target specific molecules in the cellular pro-apoptotic pathway to block apoptosis and promote viral replication.
US3 PK also inhibits apoptosis induced by the overexpression of Bad and Bid, which are parallel signalling proteins in the mitochondria-mediated apoptotic pathway. Thus, US3 also prevents apoptosis by affecting downstream effectors of the mitochondria-mediated pathway.122, 126 Specifically, US3 blocks apoptosis by phosphorylating Bad and inactivating caspases that cleave Bad to render the protein more pro-apoptotic.123 PRV US3 prevents apoptosis with the same efficiency as HSV-1 US3.127 Point mutation in the putative ATP binding site of the PRV US3 gene removes its ability to resist apoptosis, and it does not phosphorylate pre-apoptotic Bad.128 Furthermore, transiently transfected PRV US3 can induce Bad serine-112 and serine-136 phosphorylation, the downregulation of pro-apoptotic Bax, and the upregulation of anti-apoptotic Bcl-2 to regulate apoptosis.129 Both HSV-1 US3 and PRV US3 can prevent apoptosis induced by Bcl-2 family proteins, demonstrating the conserved anti-apoptotic role of US3.122
US3 regulation of the extrinsic pathway
Accordingly, α-herpesvirus-encoded proteins such as US3 PK and ICP27 can modulate the NF-κB signalling pathway, which can mediate cytokine production and virus-driven apoptosis.101, 130 Furthermore, the kinase activity of US3 can inhibit NF-κB activation and NF-κB-mediated cytokine production.131, 132 The NF-κB signalling pathway can be activated by TLR-dependent signalling. Additionally, US3 can block TLR2 signalling by interacting with proteins downstream of MyD88 and upstream of p65, and it can reduce TRAF6 polyubiquitination.131 Moreover, US3 interacts with endogenous p65 to lead to the hyperphosphorylation of p65 at serine 75, which sufficiently prevents the translocation of p65 and blocks the nuclear accumulation of NF-κB.132
Likewise, PRV US3 PK also regulates the NF-κB pathway to suppress apoptosis. US3a and US3b, two isoforms of PRV US3, both upregulate anti-apoptotic signalling through transient overexpression, but the anti-apoptosis effect of US3a is greater than that of US3b. Similar to HSV-1 US3, the kinase activity of PRV US3 is indispensable for its anti-apoptotic activity.129 In the presence of US3, phosphorylated IκBα increases in the early stage of infection to suppress apoptosis. In addition, transiently transfecting US3a or US3b can produce more phosphorylated AKT, an anti-apoptotic protein, and its activator molecule PDK-1, which is responsible for the PI3K-dependent phosphorylation of AKT serine 473. Comparatively, HSV-1 US3 can activate AKT substrate phosphorylation by targeting the downstream AKT signalling molecules.133 HSV-1 US3 masquerades as AKT, even though it does not look like AKT, and it phosphorylates tuberous sclerosis complex 2 (TSC2) on the same residues phosphorylated by AKT (T1462/S939134), indicating that phylogenetically related viruses have different mechanisms of modulating the same signalling pathways.
Additionally, US3 can bind and phosphorylate group A p21-activated kinases (PAKs), thus regulating Cdc42/Rac GTPase signalling, which is involved in US3-mediated cytoskeletal rearrangements.135 Interestingly, activated PAK1 phosphorylates the pro-apoptotic protein Bad, and activated PAK2 also regulates the activity of Bad.136, 137, 138 Investigating the involvement between PAKs and US3 showed that PAK2 has no effect on US3-mediated anti-apoptosis, whereas PAK1 has a significant, yet limited, effect. Interestingly, human immunodeficiency virus (HIV)-associated anti-apoptotic protein targets PAKs to induce anti-apoptotic signalling. This mechanism is similar to that of the US3 PK of α-herpesvirus,139 indicating that viruses of different genera share some common strategies to evade host immunity.
cAMP-dependent protein kinase (PKA) is similar to the substrate specificity of US3 PK, which can regulate apoptosis.140 US3 can phosphorylate the regulatory subunit of PKA, such as the autophosphorylation site of RIIα, to promote a redundancy of anti-apoptotic events.140, 141 In addition, programmed cell death protein 4 (PDCD4), a tumour suppressor, interacts with HSV-1 US3 PK to regulate apoptosis.142
Viral glycoproteins and their apoptosis regulation mechanisms
Herpesvirus glycoproteins are critical for viral entry and for transmission between host cells, and they can undermine host defences, including apoptosis, thus helping viruses persist for a lifetime.143 Some viral glycoproteins, such as gD, gE and gJ, have been shown to play roles in the suppression of apoptosis.
US5, a poorly conserved gene, is represented by ORF5 in the US region; it is a late gene that encodes glycoprotein J and is unnecessary for viral replication. Thus, the US5 gene of herpesvirus has been much less carefully studied, except with respect to its function of blocking apoptosis. The deletion of US5 from HSV-1 markedly abrogated protection from Fas-mediated apoptosis and partially reduced the protection from UV radiation by suppressing the activation of caspase-3/8.120 Transfecting US5 inhibits Fas/UV-induced apoptosis and weakens the activation of caspases.144 In sum, gJ is sufficient to establish an anti-apoptotic phenotype. US5-deleted HSV-1 shows weakened protection from cytotoxic T lymphocyte-induced apoptosis, and gJ is sufficient to inhibit F0F1 ATP synthase activity and reactive oxygen species creation to suppress apoptosis.85, 145 However, the mechanism by which gJ blocks apoptosis remains elusive.
US6, encoding glycoprotein D, is represented by ORF6 in the US region. US6 is the main component of the envelope and is essential for virus dissemination. gD of HSV-1 and BHV-1 can inhibit apoptosis.146, 147, 148 Compared with gJ, gD blocks apoptosis at different stages of the viral life cycle.17 The binding of HSV-1 gD to herpesvirus entry mediators, such as mannose-6 phosphate receptor, can suppress premature apoptosis, distinguishing gD from other anti-apoptotic genes.146, 149 Additionally, gD can inhibit Fas-mediated apoptosis, which involves the activation of NF κB.150 Furthermore, with the inactivation of NF κB, HSV-1-driven apoptosis increases and is accompanied by high gD expression.151 However, the molecular signalling involved in the anti-apoptotic activity of gD remains poorly understood.
US8 is represented by ORF8 in the US region and encodes glycoprotein E, which is also a late gene (γ) and an important α-herpesvirus virulence factor. PRV gE activated ERK1/2 in T lymphocytes and epithelial cells, and this was associated with the degradation of the pro-apoptotic protein Bim.152 Notably, this is the first time that gE was associated with the apoptosis signalling pathway.
Future Perspective
Viruses must evade host defence mechanisms to proliferate and be transmitted. Apoptosis, a critically important host defence mechanism, contributes to the elimination of pathogen-infected cells. To oppose the immune and inflammatory responses induced by infection, many viral proteins interact with apoptotic signals to regulate apoptosis. Apoptosis inhibition is essential for the maintenance of latent infection by herpesvirus. Understanding the anti-apoptotic mechanisms of herpesvirus will greatly improve the ability to develop new drugs and vaccines for treatment and prevention; these drugs could inhibit virus release, adjust latency to reduce viral infection or promote the death of infected cells in the early stage of infection.
Disrupting apoptosis is an effective strategy for virus replication and dissemination, but the apoptotic signalling pathway of the host cells is not isolated; interplay exists with other cellular defence mechanisms. Because of the co-evolution of the virus and the host, viral anti-apoptotic factors have evolved to exploit multiple immune pathways, including the autophagy, IFN and NF κB signalling pathways.153, 154 Interestingly, target diversity does not depend on the anti-apoptotic properties of the virus.155 Therefore, studies that specifically clarify how viruses inhibit apoptosis or interact with other signalling networks to promote replication will potentially lead to improved herpesvirus treatment.
References
Pellett P, Roizman B . Herpesviridae. In: Knipe DM, Howley PM (eds). Fields Virology. 6th edn. Lippincott, Williams & Wilkins: Philadelphia, PA, USA, 2013, pp 1802–1822.
Gray WL, Starnes B, White MW, Mahalingam R . The DNA sequence of the simian varicella virus genome. Virology 2001; 284: 123–130.
Waltzek TB, Kelley GO, Stone DM, Way K, Hanson L, Fukuda H et al. Koi herpesvirus represents a third cyprinid herpesvirus (CyHV-3) in the family Herpesviridae. J Gen Virol 2005; 86: 1659–1667.
Szpara ML, Gatherer D, Ochoa A, Greenbaum B, Dolan A, Bowden RJ et al. Evolution and diversity in human herpes simplex virus genomes. J Virol 2014; 88: 1209–1227.
Davison AJ . Herpesviruses: general features. In Encyclopedia of Virology. 3rd edn. Brian WJ Mahy, Marc HV Van (eds). Regenmortel, Academic Press: Oxford, 2008, p 430–436.
Osterrieder N, Wallaschek N, Kaufer BB . Herpesvirus genome integration into telomeric repeats of host cell chromosomes. Annu Rev Virol 2014; 1: 215–235.
Wagner MJ, Summers WC . Structure of the joint region and the termini of the DNA of herpes simplex virus type 1. J Virol 1978; 27: 374–387.
Tandon R, Mocarski ES, Conway JF . The A, B, Cs of herpesvirus capsids. Viruses 2015; 7: 899–914.
Zaichick SV, Bohannon KP, Smith GA . Alphaherpesviruses and the cytoskeleton in neuronal infections. Viruses 2011; 3: 941–981.
Krummenacher C, Carfí A, Eisenberg RJ, Cohen GH . Entry of herpesviruses into cells: the enigma variations Pöhlmann S, Simmons G Viral Entry into Host Cells. Springer: New York, 2013, pp 178–195.
Zeev-Ben-Mordehai T, Hagen C, Grünewald K . A cool hybrid approach to the herpesvirus ‘life’cycle. Curr Opin Virol 2014; 5: 42–49.
Kukhanova M, Korovina A, Kochetkov S . Human herpes simplex virus: life cycle and development of inhibitors. Biochemistry (Moscow) 2014; 79: 1635–1652.
Kramer T, Greco T, Enquist L, Cristea I . Proteomic characterization of pseudorabies virus extracellular virions. J Virol 2011; 85: 6427–6441.
Campadelli-Fiume G, Menotti L, Avitabile E, Gianni T . Viral and cellular contributions to herpes simplex virus entry into the cell. Curr Opin Virol 2012; 2: 28–36.
Karasneh GA, Shukla D . Herpes simplex virus infects most cell types in vitro: clues to its success. Virol J 2011; 8: 481.
Agelidis AM, Shukla D . Cell entry mechanisms of HSV: what we have learned in recent years. Future Virol 2015; 10: 1145–1154.
Zhou G, Galvan V, Campadelli-Fiume G, Roizman B . Glycoprotein D or J delivered in trans blocks apoptosis in SK-N-SH cells induced by a herpes simplex virus 1 mutant lacking intact genes expressing both glycoproteins. J Virol 2000; 74: 11782–11791.
Radtke K, Kieneke D, Wolfstein A, Michael K, Steffen W, Scholz T et al. Plus-and minus-end directed microtubule motors bind simultaneously to herpes simplex virus capsids using different inner tegument structures. PLoS Pathogens 2010; 6: e1000991.
Roizman B, Zhou G . The 3 facets of regulation of herpes simplex virus gene expression: a critical inquiry. Virology 2015; 479: 562–567.
Johnson DC, Baines JD . Herpesviruses remodel host membranes for virus egress. Nat Rev Microbiol 2011; 9: 382–394.
Mou F, Forest T, Baines JD . US3 of herpes simplex virus type 1 encodes a promiscuous protein kinase that phosphorylates and alters localization of lamin A/C in infected cells. J Virol 2007; 81: 6459–6470.
Klupp B, Altenschmidt J, Granzow H, Fuchs W, Mettenleiter TC . Glycoproteins required for entry are not necessary for egress of pseudorabies virus. J Virol 2008; 82: 6299–6309.
Owen D, Crump C, Graham S . Tegument assembly and secondary envelopment of alphaherpesviruses. Viruses 2015; 7: 5084–5114.
Steiner I, Benninger F . Update on herpes virus infections of the nervous system. Curr Neurol Neurosci Rep 2013; 13: 1–7.
Knipe DM, Cliffe A . Chromatin control of herpes simplex virus lytic and latent infection. Nat Rev Microbiol 2008; 6: 211–221.
Curanovic D, Enquist L . Directional transneuronal spread of α-herpesvirus infection. Future Virol 2009; 4: 591–603.
Roizman B, Whitley RJ . An inquiry into the molecular basis of HSV latency and reactivation. Annu Rev Microbiol 2013; 67: 355–374.
Carpenter D, Hsiang C, Brown DJ, Jin L, Osorio N, BenMohamed L et al. Stable cell lines expressing high levels of the herpes simplex virus type 1 LAT are refractory to caspase 3 activation and DNA laddering following cold shock induced apoptosis. Virology 2007; 369: 12–18.
Ibiricu I, Huiskonen JT, Döhner K, Bradke F, Sodeik B, Grünewald K . Cryo electron tomography of herpes simplex virus during axonal transport and secondary envelopment in primary neurons. PLoS Pathog 2011; 7: e1002406.
Wyllie A . Apoptosis: an overview. Br Med Bull 1997; 53: 451–465.
Kennedy PG . Viruses, apoptosis, and neuroinflammation – a double-edged sword. J Neurovirol 2015; 21: 1–7.
Benedict CA, Norris PS, Ware CF . To kill or be killed: viral evasion of apoptosis. Nat Immunol 2002; 3: 1013–1018.
Mossman KL, Weller SK . HSV cheats the executioner. Cell Host Microbe 2015; 17: 148–151.
Ashkenazi A, Salvesen G . Regulated cell death: signaling and mechanisms. Annu Rev Cell Dev Biol 2014; 30: 337–356.
Postigo A, Way M . The vaccinia virus-encoded Bcl-2 homologues do not act as direct Bax inhibitors. J Virol 2012; 86: 203–213.
Papaianni E, El Maadidi S, Schejtman A, Neumann S, Maurer U, Marino-Merlo F et al. Phylogenetically distant viruses use the same BH3-only protein Puma to trigger Bax/Bak-dependent apoptosis of infected mouse and human cells. PLoS ONE 2015; 10: e0126645.
Giorgi C, Bonora M, Sorrentino G, Missiroli S, Poletti F, Suski JM et al. p53 at the endoplasmic reticulum regulates apoptosis in a Ca2+-dependent manner. Proc Natl Acad Sci USA 2015; 112: 1779–1784.
Lamkanfi M, Festjens N, Declercq W, Berghe TV, Vandenabeele P . Caspases in cell survival, proliferation and differentiation. Cell Death Differ 2007; 14: 44–55.
Kroemer G, Galluzzi L, Brenner C . Mitochondrial membrane permeabilization in cell death. Physiol Rev 2007; 87: 99–163.
Galluzzi L, Kepp O, Kroemer G . Mitochondria: master regulators of danger signalling. Nat Rev Mol Cell Biol 2012; 13: 780–788.
Lavrik I, Golks A, Krammer PH . Death receptor signaling. J Cell Sci 2005; 118: 265–267.
Bodmer J-L, Schneider P, Tschopp J . The molecular architecture of the TNF superfamily. Trends Biochem Sci 2002; 27: 19–26.
Mathew SJ, Haubert D, Krönke M, Leptin M . Looking beyond death: a morphogenetic role for the TNF signalling pathway. J Cell Sci 2009; 122: 1939–1946.
Lee EW, Jeong MH, Song JW . The roles of FADD in extrinsic apoptosis and necroptosis. Biochem Mol Biol Rep 2012; 45: 496–508.
Pennarun B, Meijer A, de Vries EG, Kleibeuker JH, Kruyt F, de Jong S . Playing the DISC: turning on TRAIL death receptor-mediated apoptosis in cancer. Biochim Biophys Acta 2010; 1805: 123–140.
Chowdhury I, Tharakan B, Bhat GK . Caspases—an update. Comp Biochem Physiol B Biochem Mol Biol 2008; 151: 10–27.
Ashkenazi A . Targeting the extrinsic apoptosis pathway in cancer. Cytokine Growth Factor Rev 2008; 19: 325–331.
Carter KL, Roizman B . The promoter and transcriptional unit of a novel herpes simplex virus 1 alpha gene are contained in, and encode a protein in frame with, the open reading frame of the alpha 22 gene. J Virol 1996; 70: 172–178.
Mahmood Z, Shukla Y . Death receptors: targets for cancer therapy. Exp Cell Res 2010; 316: 887–899.
Pobezinskaya YL, Liu Z . The role of TRADD in death receptor signaling. Cell Cycle 2012; 11: 871–876.
Declercq W, Berghe TV, Vandenabeele P . RIP kinases at the crossroads of cell death and survival. Cell 2009; 138: 229–232.
Wilson NS, Dixit V, Ashkenazi A . Death receptor signal transducers: nodes of coordination in immune signaling networks. Nat Immunol 2009; 10: 348–355.
Jiang X . The intrinsic apoptotic pathway. In: Wu H (ed.). Cell Death. Springer: New York, 2014, pp 15–40.
Borner C, Andrews D . The apoptotic pore on mitochondria: are we breaking through or still stuck&quest. Cell Death Differ 2014; 21: 187–191.
Wong W, Puthalakath H . Bcl‐2 family proteins: the sentinels of the mitochondrial apoptosis pathway. IUBMB Life 2008; 60: 390–397.
Kilbride S, Prehn J . Central roles of apoptotic proteins in mitochondrial function. Oncogene 2013; 32: 2703–2711.
Tait SW, Green DR . Mitochondria and cell death: outer membrane permeabilization and beyond. Nat Rev Mol Cell Biol 2010; 11: 621–632.
Yuan S, Akey CW . Apoptosome structure, assembly, and procaspase activation. Structure 2013; 21: 501–515.
Yuan S, Topf M, Reubold TF, Eschenburg S, Akey CW . Changes in Apaf-1 conformation that drive apoptosome assembly. Biochemistry 2013; 52: 2319–2327.
Shore GC, Papa FR, Oakes SA . Signaling cell death from the endoplasmic reticulum stress response. Curr Opin Cell Biol 2011; 23: 143–149.
Verma G, Datta M . The critical role of JNK in the ER‐mitochondrial crosstalk during apoptotic cell death. J Cell Physiol 2012; 227: 1791–1795.
Jones C . Herpes simplex virus type 1 and bovine herpesvirus 1 latency. Clin Microbiol Rev 2003; 16: 79–95.
Bloom DC, Kwiatkowski DL . HSV-1 latency and the roles of LATs. In: Weller SK. (ed.). Alphaherpesviruses. Molecular Virology. Caister Academic Press: Norfolk, UK, 2011, pp 295–316.
Henderson G, Peng W, Jin L, Perng G-C, Nesburn AB, Wechsler SL et al. Regulation of caspase 8-and caspase 9-induced apoptosis by the herpes simplex virus type 1 latency-associated transcript. J Neurovirol 2002; 8: 103–111.
Jin L, Peng W, Perng G-C, Brick DJ, Nesburn AB, Jones C et al. Identification of herpes simplex virus type 1 latency-associated transcript sequences that both inhibit apoptosis and enhance the spontaneous reactivation phenotype. J Virol 2003; 77: 6556–6561.
Peng W, Jin L, Henderson G, Perng G, Brick D, Nesburn A et al. Mapping herpes simplex virus type 1 latency-associated transcript sequences that protect from apoptosis mediated by a plasmid expressing caspase-8. J Neurovirol 2004; 10: 260–265.
Nguyen ML, Blaho JA . Apoptosis during herpes simplex virus infection. Adv Virus Res 2006; 69: 67–97.
Liu X, Cohen JI . The role of PI3K/Akt in human herpesvirus infection: From the bench to the bedside. Virology 2015; 479: 568–577.
Li S, Carpenter D, Hsiang C, Wechsler SL, Jones C . Herpes simplex virus type 1 latency-associated transcript inhibits apoptosis and promotes neurite sprouting in neuroblastoma cells following serum starvation by maintaining protein kinase B (AKT) levels. J Gen Virol 2010; 91: 858–866.
Carpenter D, Hsiang C, Jiang X, Osorio N, BenMohamed L, Jones C et al. The herpes simplex virus type 1 (HSV-1) latency-associated transcript (LAT) protects cells against cold-shock-induced apoptosis by maintaining phosphorylation of protein kinase B (AKT). J Neurovirol 2015; 21: 568–575.
Jiang X, Chentoufi AA, Hsiang C, Carpenter D, Osorio N, BenMohamed L et al. The herpes simplex virus type 1 latency-associated transcript can protect neuron-derived C1300 and Neuro2A cells from granzyme B-induced apoptosis and CD8 T-cell killing. J Virol 2011; 85: 2325–2332.
Jin L, Carpenter D, Moerdyk-Schauwecker M, Vanarsdall AL, Osorio N, Hsiang C et al. Cellular FLIP can substitute for the herpes simplex virus type 1 latency-associated transcript gene to support a wild-type virus reactivation phenotype in mice. J Neurovirol 2008; 14: 389–400.
Kather A, Raftery MJ, Devi-Rao G, Lippmann J, Giese T, Sandri-Goldin RM et al. Herpes simplex virus type 1 (HSV-1)-induced apoptosis in human dendritic cells as a result of downregulation of cellular FLICE-inhibitory protein and reduced expression of HSV-1 antiapoptotic latency-associated transcript sequences. J Virol 2010; 84: 1034–1046.
Carpenter D, Henderson G, Hsiang C, Osorio N, BenMohamed L, Jones C et al. Introducing point mutations into the ATGs of the putative open reading frames of the HSV-1 gene encoding the latency associated transcript (LAT) reduces its anti-apoptosis activity. Microb Pathog 2008; 44: 98–102.
Shen W, E Silva MS, Jaber T, Vitvitskaia O, Li S, Henderson G et al. Two small RNAs encoded within the first 1.5 kilobases of the herpes simplex virus type 1 latency-associated transcript can inhibit productive infection and cooperate to inhibit apoptosis. J Virol 2009; 83: 9131–9139.
da Silva LF, Jones C . Small non-coding RNAs encoded within the herpes simplex virus type 1 latency associated transcript (LAT) cooperate with the retinoic acid inducible gene I (RIG-I) to induce beta-interferon promoter activity and promote cell survival. Virus Res 2013; 175: 101–109.
Lv F, Yang H, Zhong F, Fan J, Liu Y, Gao R . Expression of herpes simplex virus type 2 latency associated transcript ORF1 and its anti-apoptotic function. Chin J Biotechnol 2013; 29: 1776–1785.
Ruidi G, Huilan Y, Feifei Z, Fangbiao L . The expression and anti-apoptotic function of herpes simplex virus type 2 latency associated transcript-RL1. Biotechnol Bull 2014; 3: 032.
Yang H, Bai L . The expression and Anti-apoptotic Function of HSV-2 LAT ORF2. Microbiolgy 2010; 37: 389–393.
Yang H, Xue L, Fan J, Zhang F, Long C, Zhang L . Effects of herpes simplex virus 2 latency-associated transcript open reading frame 3 on the apoptosis in Vero cells. Chin J Dermatology 2012; 45: 186–190.
Jones C . Bovine herpes virus 1 (BHV-1) and herpes simplex virus type 1 (HsV-1) promote survival of latently infected sensory neurons, in part by inhibiting apoptosis. J Cell Death 2013; 6: 1–16.
Bowman JJ, Schaffer PA . Origin of expression of the herpes simplex virus type 1 protein US1. 5. J Virol 2009; 83: 9183–9194.
Hagglund R, Munger J, Poon AP, Roizman B . US3 protein kinase of herpes simplex virus 1 blocks caspase 3 activation induced by the products of US1.5 and UL13 genes and modulates expression of transduced US1.5 open reading frame in a cell type-specific manner. J Virol 2002; 76: 743–754.
You S, Liu Y, Fan J, Yang H . Effects of herpes slmplex virus 2 Infection Cell protein 22 and its apoptosis function in Vero cells. J Pract Med 2014; 30: 364–366.
Aubert M, Chen Z, Lang R, Dang CH, Fowler C, Sloan DD et al. The antiapoptotic herpes simplex virus glycoprotein J localizes to multiple cellular organelles and induces reactive oxygen species formation. J Virol 2008; 82: 617–629.
Munger J, Hagglund R, Roizman B . Infected cell protein no. 22 is subject to proteolytic cleavage by caspases activated by a mutant that induces apoptosis. Virology 2003; 305: 364–370.
Richard A, Tulasne D . Caspase cleavage of viral proteins, another way for viruses to make the best of apoptosis. Cell Death Dis 2012; 3: e277.
Pietsch EC, Sykes SM, McMahon SB, Murphy ME . The p53 family and programmed cell death. Oncogene 2008; 27: 6507–6521.
Maruzuru Y, Fujii H, Oyama M, Kozuka-Hata H, Kato A, Kawaguchi Y . Roles of p53 in herpes simplex virus 1 replication. J Virol 2013; 87: 9323–9332.
Kinchington PR, Leger A, Guedon J, Hendricks RL . Herpes simplex virus and varicella zoster virus, the house guests who never leave. Herpesviridae 2012; 3: 5.
James SF, Mahalingam R, Gilden D . Does apoptosis play a role in varicella zoster virus latency and reactivation? Viruses 2012; 4: 1509–1514.
Hood C, Cunningham AL, Slobedman B, Arvin AM, Sommer MH, Kinchington PR et al. Varicella-zoster virus ORF63 inhibits apoptosis of primary human neurons. J Virol 2006; 80: 1025–1031.
Ambagala AP, Cohen JI . Varicella-zoster virus IE63, a major viral latency protein, is required to inhibit the alpha interferon-induced antiviral response. J Virol 2007; 81: 7844–7851.
Sandri-Goldin MR . The many roles of the highly interactive HSV protein ICP27, a key regulator of infection. Future Microbiol 2011; 6: 1261–1277.
Sandri-Goldin RM . The many roles of the regulatory protein ICP27 during herpes simplex virus infection. Front Biosci 2008; 13: 5241–5256.
Amor S, Strassheim S, Dambrine G, Remy S, Rasschaert D, Laurent S . ICP27 protein of Marek’s disease virus interacts with SR proteins and inhibits the splicing of cellular telomerase chTERT and viral vIL8 transcripts. J Gen Virol 2011; 92: 1273–1278.
Sedlackova L, Perkins KD, Lengyel J, Strain AK, van Santen VL, Rice SA . Herpes simplex virus type 1 ICP27 regulates expression of a variant, secreted form of glycoprotein C by an intron retention mechanism. J Virol 2008; 82: 7443–7455.
Olesky M, McNamee EE, Zhou C, Taylor TJ, Knipe DM . Evidence for a direct interaction between HSV-1 ICP27 and ICP8 proteins. Virology 2005; 331: 94–105.
Majerciak V, Yamanegi K, Allemand E, Kruhlak M, Krainer AR, Zheng ZM . Kaposi's sarcoma-associated herpesvirus ORF57 functions as a viral splicing factor and promotes expression of intron-containing viral lytic genes in spliceosome-mediated RNA splicing. J Virol 2008; 82: 2792–2801.
Tunnicliffe RB, Hautbergue GM, Kalra P, Jackson BR, Whitehouse A, Wilson SA et al. Structural basis for the recognition of cellular mRNA export factor REF by herpes viral proteins HSV-1 ICP27 and HVS ORF57. PLoS Pathog 2011; 7: e1001244.
Kim JC, Lee SY, Kim SY, Kim JK, Kim HJ, Lee HM et al. HSV-1 ICP27 suppresses NF-κB activity by stabilizing IκBα. FEBS Lett 2008; 582: 2371–2376.
Pradhan P, Nguyen ML . Early passage neonatal and adult keratinocytes are sensitive to apoptosis induced by infection with an ICP27-null mutant of herpes simplex virus 1. Apoptosis 2013; 18: 160–170.
Aubert M, Blaho JA . The herpes simplex virus type 1 regulatory protein ICP27 is required for the prevention of apoptosis in infected human cells. J Virol 1999; 73: 2803–2813.
Aubert M, O’Toole J, Blaho JA . Induction and prevention of apoptosis in human HEp-2 cells by herpes simplex virus type 1. J Virol 1999; 73: 10359–10370.
Aubert M, Rice SA, Blaho JA . Accumulation of herpes simplex virus type 1 early and leaky-late proteins correlates with apoptosis prevention in infected human HEp-2 cells. J Virol 2001; 75: 1013–1030.
Hargett D, McLean T, Bachenheimer SL . Herpes simplex virus ICP27 activation of stress kinases JNK and p38. J Virol 2005; 79: 8348–8360.
Fontaine-Rodriguez EC, Knipe DM . Herpes simplex virus ICP27 increases translation of a subset of viral late mRNAs. J Virol 2008; 82: 3538–3545.
Gillis PA, Okagaki LH, Rice SA . Herpes simplex virus type 1 ICP27 induces p38 mitogen-activated protein kinase signaling and apoptosis in HeLa cells. J Virol 2009; 83: 1767–1777.
Hargett D, Rice S, Bachenheimer SL . Herpes simplex virus type 1 ICP27-dependent activation of NF-κB. J Virol 2006; 80: 10565–10578.
Gilmore TD . Introduction to NF-κB: players, pathways, perspectives. Oncogene 2006; 25: 6680–6684.
Zachos G, Koffa M, Preston CM, Clements JB, Conner J . Herpes simplex virus type 1 blocks the apoptotic host cell defense mechanisms that target Bcl-2 and manipulates activation of p38 mitogen-activated protein kinase to improve viral replication. J Virol 2001; 75: 2710–2728.
Long C, Yang H, Zhang F, Xue L, Du H . Investigation of Vero cell apoptosis caused by the herpes simplex virus type 2 ICP27. Int J Virol 2013; 20: 160–165.
Deruelle MJ, Favoreel HW . Keep it in the subfamily: the conserved alphaherpesvirus US3 protein kinase. J Gen Virol 2011; 92: 18–30.
Wild P, Leisinger S, de Oliveira AP, Schraner EM, Kaech A, Ackermann M et al. Herpes simplex virus 1 Us3 deletion mutant is infective despite impaired capsid translocation to the cytoplasm. Viruses 2015; 7: 52–71.
Wisner TW, Wright CC, Kato A, Kawaguchi Y, Mou F, Baines JD et al. Herpesvirus gB-induced fusion between the virion envelope and outer nuclear membrane during virus egress is regulated by the viral US3 kinase. J Virol 2009; 83: 3115–3126.
Demmin GL, Clase AC, Randall JA, Enquist L, Banfield BW . Insertions in the gG gene of pseudorabies virus reduce expression of the upstream Us3 protein and inhibit cell-to-cell spread of virus infection. J Virol 2001; 75: 10856–10869.
Jacob T, Van den Broeke C, Favoreel HW . Viral serine/threonine protein kinases. J Virol 2011; 85: 1158–1173.
Wang S, Wang K, Lin R, Zheng C . Herpes simplex virus 1 serine/threonine kinase US3 hyperphosphorylates IRF3 and inhibits beta interferon production. J Virol 2013; 87: 12814–12827.
Asano S, Honda T, Goshima F, Nishiyama Y, Sugiura Y . US3 protein kinase of herpes simplex virus protects primary afferent neurons from virus-induced apoptosis in ICR mice. Neurosci Lett 2000; 294: 105–108.
Jerome KR, Fox R, Chen Z, Sears AE, Lee H, Corey L . Herpes simplex virus inhibits apoptosis through the action of two genes, Us5 and Us3. J Virol 1999; 73: 8950–8957.
Hata S, Koyama AH, Shiota H, Adachi A, Goshima F, Nishiyama Y . Antiapoptotic activity of herpes simplex virus type 2: the role of US3 protein kinase gene. Microbes Infect 1999; 1: 601–607.
Ogg PD, McDonell PJ, Ryckman BJ, Knudson CM, Roller RJ . The HSV-1 Us3 protein kinase is sufficient to block apoptosis induced by overexpression of a variety of Bcl-2 family members. Virology 2004; 319: 212–224.
Benetti L, Munger J, Roizman B . The herpes simplex virus 1 US3 protein kinase blocks caspase-dependent double cleavage and activation of the proapoptotic protein BAD. J Virol 2003; 77: 6567–6573.
Munger J, Chee AV, Roizman B . The US3 protein kinase blocks apoptosis induced by the d120 mutant of herpes simplex virus 1 at a premitochondrial stage. J Virol 2001; 75: 5491–5497.
Benetti L, Roizman B . In transduced cells, the US3 protein kinase of herpes simplex virus 1 precludes activation and induction of apoptosis by transfected procaspase 3. J Virol 2007; 81: 10242–10248.
Munger J, Roizman B . The US3 protein kinase of herpes simplex virus 1 mediates the posttranslational modification of BAD and prevents BAD-induced programmed cell death in the absence of other viral proteins. Proc Natl Acad Sci 2001; 98: 10410–10415.
Geenen K, Favoreel HW, Olsen L, Enquist LW, Nauwynck HJ . The pseudorabies virus US3 protein kinase possesses anti-apoptotic activity that protects cells from apoptosis during infection and after treatment with sorbitol or staurosporine. Virology 2005; 331: 144–150.
Deruelle M, Geenen K, Nauwynck HJ, Favoreel HW . A point mutation in the putative ATP binding site of the pseudorabies virus US3 protein kinase prevents Bad phosphorylation and cell survival following apoptosis induction. Virus Res 2007; 128: 65–70.
Chang C-D, Lin P-Y, Liao M-H, Chang C-I, Hsu J-L, Yu F-L et al. Suppression of apoptosis by pseudorabies virus Us3 protein kinase through the activation of PI3-K/Akt and NF-κB pathways. Res Vet Sci 2013; 95: 764–774.
Hayden MS, Ghosh S . NF-κB in immunobiology. Cell Res 2011; 21: 223–244.
Sen J, Liu X, Roller R, Knipe DM . Herpes simplex virus US3 tegument protein inhibits Toll-like receptor 2 signaling at or before TRAF6 ubiquitination. Virology 2013; 439: 65–73.
Wang K, Ni L, Wang S, Zheng C . Herpes simplex virus 1 protein kinase US3 hyperphosphorylates p65/RelA and dampens NF-κB activation. J Virol 2014; 88: 7941–7951.
Chuluunbaatar U, Roller R, Feldman ME, Brown S, Shokat KM, Mohr I . Constitutive mTORC1 activation by a herpesvirus Akt surrogate stimulates mRNA translation and viral replication. Genes Dev 2010; 24: 2627–2639.
Chuluunbaatar U, Mohr I . A herpesvirus kinase that masquerades as Akt: you don’t have to look like Akt, to act like it. Cell Cycle 2011; 10: 2064–2068.
Van den Broeke C, Radu M, Deruelle M, Nauwynck H, Hofmann C, Jaffer ZM et al. Alphaherpesvirus US3-mediated reorganization of the actin cytoskeleton is mediated by group A p21-activated kinases. Proc Natl Acad Sci USA 2009; 106: 8707–8712.
Jakobi R, Moertl E, Koeppel MA . p21-activated protein kinase γ-PAK suppresses programmed cell death of BALB3T3 fibroblasts. J Biol Chem 2001; 276: 16624–16634.
Schürmann A, Mooney A, Sanders L, Sells M, Wang H, Reed J et al. p21-activated kinase 1 phosphorylates the death agonist bad and protects cells from apoptosis. Mol Cell Biol 2000; 20: 453–461.
Pacheco A, Chernoff J . Group I p21-activated kinases: emerging roles in immune function and viral pathogenesis. Int J Biochem Cell Biol 2010; 42: 13–16.
Wolf D, Witte V, Laffert B, Blume K, Stromer E, Trapp S et al. HIV-1 Nef associated PAK and PI3-kinases stimulate Akt-independent Bad-phosphorylation to induce anti-apoptotic signals. Nat Med 2001; 7: 1217–1224.
Benetti L, Roizman B . Herpes simplex virus protein kinase US3 activates and functionally overlaps protein kinase A to block apoptosis. Proc Natl Acad Sci USA 2004; 101: 9411–9416.
Roizman B, Taddeo B. The strategy of herpes simplex virus replication and takeover of the host cell. In: Arvin A, Campadelli-Fiume G, Mocarski E et al. (eds). Human Herpesviruses: Biology, Therapy, and Immunoprophylaxis. Cambridge University Press: Cambridge, UK, 2007, p 163–173..
Wang X, Patenode C, Roizman B . US3 protein kinase of HSV-1 cycles between the cytoplasm and nucleus and interacts with programmed cell death protein 4 (PDCD4) to block apoptosis. Proc Natl Acad Sci 2011; 108: 14632–14636.
Antoine TE, Park PJ, Shukla D . Glycoprotein targeted therapeutics: a new era of anti‐herpes simplex virus‐1 therapeutics. Rev Med Virol 2013; 23: 194–208.
Jerome KR, Chen Z, Lang R, Torres MR, Hofmeister J, Smith S et al. HSV and glycoprotein J inhibit caspase activation and apoptosis induced by granzyme B or Fas. J Immunol 2001; 167: 3928–3935.
Aubert M, Krantz EM, Jerome KR . Herpes simplex virus genes Us3, Us5, and Us12 differentially regulate cytotoxic T lymphocyte-induced cytotoxicity. Viral Immunol 2006; 19: 391–408.
Zhou G, Avitabile E, Campadelli-Fiume G, Roizman B . The domains of glycoprotein D required to block apoptosis induced by herpes simplex virus 1 are largely distinct from those involved in cell-cell fusion and binding to nectin1. J Virol 2003; 77: 3759–3767.
Hanon E, Keil G, Griebel P, Vanderplasschen A, Rijsewijk FA, Babiuk L et al. Bovine herpesvirus 1-induced apoptotic cell death: role of glycoprotein D. Virology 1999; 257: 191–197.
Zhou G, Galvan V, Campadelli-Fiume G, Roizman B . Glycoprotein D or J delivered in transblocks apoptosis in SK-N-SH cells induced by a herpes simplex virus 1 mutant lacking intact genes expressing both glycoproteins. J Virol 2000; 74: 11782–11791.
Sciortino MT, Medici MA, Marino-Merlo F, Zaccaria D, Giuffre-Cuculletto M, Venuti A et al. Involvement of gD/HVEM interaction in NF-kB-dependent inhibition of apoptosis by HSV-1 gD. Biochem Pharmacol 2008; 76: 1522–1532.
Medici MA, Sciortino MT, Perri D, Amici C, Avitabile E, Ciotti M et al. Protection by herpes simplex virus glycoprotein D against Fas-mediated apoptosis: role of nuclear factor kappaB. J Biol Chem 2003; 278: 36059–36067.
Marino-Merlo F, Papaianni E, Medici MA, Macchi B, Grelli S, Mosca C et al. HSV-1-induced activation of NF-κB protects U937 monocytic cells against both virus replication and apoptosis. Cell Death Dis 2016; 7: e2354.
Pontes MS, Van Waesberghe C, Nauwynck H, Verhasselt B, Favoreel HW . Pseudorabies virus glycoprotein gE triggers ERK1/2 phosphorylation and degradation of the pro-apoptotic protein Bim in epithelial cells. Virus Res 2016; 213: 214–218.
Liang C, Oh B-H, Jung J . Novel functions of viral anti-apoptotic factors. Nat Rev Microbiol 2015; 13: 7–12.
Mariño G, Niso-Santano M, Baehrecke EH, Kroemer G . Self-consumption: the interplay of autophagy and apoptosis. Nat Rev Mol Cell Biol 2014; 15: 81–94.
Seo J-Y, Yaneva R, Hinson ER, Cresswell P . Human cytomegalovirus directly induces the antiviral protein viperin to enhance infectivity. Science 2011; 332: 1093–1097.
Acknowledgements
This work was supported by grants from National Natural Science Foundation of China (31272545), National Science and Technology Support Program (No. 2015BAD12B05), China Agricultural Research System (CARS-43-8) and Special Fund for Key Laboratory of Animal Disease and Human Health of Sichuan Province (2016JPT0004).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by M Agostini
Rights and permissions
Cell Death and Disease is an open-access journal published by Nature Publishing Group. This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
You, Y., Cheng, AC., Wang, MS. et al. The suppression of apoptosis by α-herpesvirus. Cell Death Dis 8, e2749 (2017). https://doi.org/10.1038/cddis.2017.139
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2017.139
- Springer Nature Limited
This article is cited by
-
Construction of a pathological model of skin lesions in acute herpes zoster virus infection and its molecular mechanism
Mammalian Genome (2024)
-
Apoptosis is mediated by FeHV-1 through the intrinsic pathway and interacts with the autophagic process
Virology Journal (2023)
-
Duck plague virus UL41 protein inhibits RIG-I/MDA5-mediated duck IFN-β production via mRNA degradation activity
Veterinary Research (2022)
-
Regulation of alphaherpesvirus protein via post-translational phosphorylation
Veterinary Research (2022)
-
Dual inhibition of innate immunity and apoptosis by human cytomegalovirus protein UL37x1 enables efficient virus replication
Nature Microbiology (2022)