Abstract
Background:
Previous observations suggest suboptimal ‘real world’ survival outcomes for advanced pancreatic adenocarcinoma. We hypothesized that centralisation of advanced pancreatic adenocarcinoma management would improve chemotherapy treatment and survival from the disease.
Methods:
The data was prospectively collected on all cases of advanced pancreatic adenocarcinoma reviewed through Clatterbridge Cancer Centre according to two groups; 1 October 2009–31st Dec 2010 (devolved care) or 1 January 2013–31 March 2014 (centralised care). Analysis included treatment received, 30-day chemotherapy mortality rate and overall survival (OS).
Results:
More patients received chemotherapy with central care (67.0% (n=115) vs 43.0% (n=121); P=2.2 × 10−4) with no difference in 30-day mortality (20.8% vs 25%; P=0.573) but reduced time to commencement of chemotherapy (18 vs 28 days, P=1.0 × 10−3). More patients received second-line chemotherapy with central care (23.4% vs 1.9%, P=1.4 × 10−4), while OS was significantly increased with central care (median: Five vs three months, HR 0.785, P=0.045). Exploratory analysis suggested that it was those with a poorer performance status, elderly or with metastatic disease who benefited the most from transition to central care.
Conclusions:
A centralised clinic model for advanced pancreatic cancer management resulted in prompt, safe and higher use of chemotherapy compared with devolved care. This was associated with a modest survival benefit. Prospective studies are required to validate the findings reported and the basis for improved survival with centralised care.
Similar content being viewed by others
Main
With 9400 new diagnoses in the UK in 2013 and a 5-year survival rate of merely 3%, pancreas adenocarcinoma ranks among the most lethal of malignancies (Cancer Research UK, 2016). The vast majority of cases continued to be diagnosed at an advanced stage, for which recent reports suggest no significant improvement in survival over the past two decades (Sirri et al, 2016). Nevertheless, modest benefits in terms of longer survival and improved quality of life were demonstrated with palliative Gemcitabine chemotherapy for advanced pancreatic adenocarcinoma nearly two decades ago (Burris et al, 1997). More recently, longer median survival of between 8 and 11 months has been demonstrated with combination chemotherapy compared with 6 months on single agent Gemcitabine chemotherapy for metastatic disease (Garrido-Laguna and Hidalgo, 2015).
A review of the survival data for more than 20 000 patients with metastatic pancreatic adenocarcinoma in the US (1988–2008) by Worni et al (2013) suggested that there was only marginal improvement in the median survival from 2 to 3 months over that period. It was observed that only a minority of patients with advanced pancreatic adenocarcinoma received systemic chemotherapy, despite publication of the landmark trial, which established the role of Gemcitabine palliative chemotherapy mid-way through this period (Burris et al, 1997). The largest reported UK regional retrospective study (2002–2005) on outcomes for advanced pancreatic adenocarcinoma, also suggested a median survival of 7.2 and 2.8 months, respectively, for patients with locally advanced and metastatic disease (Mukherjee et al, 2008). This would suggest inadequate translation of the modest chemotherapy benefit from clinical trials to the ‘real-world’ patient population. While patients accrued to clinical trials may be fitter, the explanation for the discrepancy between trial and ‘real-world’ survival outcomes is uncertain. However, advanced pancreatic adenocarcinoma is known to be associated with significant morbidity and a poor prognosis. This introduces the necessity for optimal supportive care and complex judgement in the utilisation of chemotherapy treatment. Consequently, the relative contribution of patient fitness outwith the clinical trial population and practitioner attitude or limitations to suboptimal utilization of chemotherapy in routine practice is uncertain.
Centralised care has been demonstrated to improve the resection rate for early pancreatic adenocarcinoma (Gooiker et al, 2014). Furthermore, centralised care has been shown to reduce peri-operative mortality for patients with early pancreatic (Neoptolemos et al, 1997) and oesophageal cancer (van Lanschot et al, 2001). Increased surgeon specialization and peri-operative supportive care are factors, which have been hypothesized to contribute to the improved outcome for these malignancies treated by complex surgical procedures. In this respect, we hypothesized that centralisation of advanced pancreatic adenocarcinoma management could possibly improve supportive care, while improving oncology specialist input, thus increasing chemotherapy utilisation and potentially survival. Therefore, within the Merseyside and Cheshire Cancer Network (North West England), we adopted a transition from devolved to centralised pancreatic cancer management during 2011 and 2012. We now try to determine the impact of such modification in service delivery pattern by comparing patient chemotherapy treatment trends and survival outcomes astride the transition.
Patients and methods
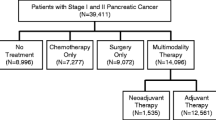
This study was retrospective in nature with baseline characteristics of patients, performance status and cause of death obtained from patient records. However, date of referral, diagnosis, hospital site of initial review, treatment records and the date of death had been prospectively charted on a database by statisticians of the Clinical Effectiveness team (CET). Ethical approval to review the database and patient case records for the study was obtained from the designated committee at the Centre. Patients with early pancreatic adenocarcinoma were excluded from the study. Patients with advanced pancreatic adenocarcinoma who fell into either of two groups were studied:
Early group (E)
Patients managed between 1 October 2009 and 31 December 2010.
Late group (L)
Patients managed between 1 January 2013 and 31 March 2014.
Patients in Group E were managed prior to, while patients in Group L were managed subsequent to, the centralisation of pancreatic adenocarcinoma management in Clatterbridge Cancer Centre. The groups were selected to cover similar intervals of time astride the transition to centralised care but prior to the introduction of Gemcitabine/Nab-Paclitaxel chemotherapy for the malignancy in our centre. Patients in group E could be seen by 5 different oncologists in any of five clinics distributed throughout the Mereyside and Cheshire region. These devolved clinics accommodated mostly patients with non-hepato-pancreatobiliary (non-HPB) malignancies. In contrast, patients in Group L were seen by two oncologists in two clinics dedicated to the management of HPB malignancies in two main hospitals. Liaison with HPB specialist nurses was available to the oncologists in Group E as required. In contrast, one HPB Specialist Nurse was regularly present for each of the clinics in Group L, while liaison with other HPB specialist nurses was available as required. Ad-hoc pathways for referral to dieticians, palliative care and other HPB medical specialists was available to both groups as required, but more direct referral pathways for such supportive care measures was set up for the clinics in Group L.
The data on demographics, smoking history, past medical history, histological diagnosis, cancer stage (locally advanced or metastatic), performance status, date and clinic of initial appointment at CCC, treatment received (one or two lines), date of death and cause of death were obtained. Smoking history was dichotomized (non-smoker vs current/ex-smoker), while the existence of a known diagnosis of diabetes mellitus or otherwise was noted from the past medical history. The histological diagnosis was recorded on the CET database but cross-checked with pathology results, while cancer stage was determined from radiology reports, which were updated by regional pancreatic cancer multi-disciplinary team (MDT) review. WHO performance status was that recorded at the time of review for commencement of chemotherapy for those who received such treatment or at the time of initial review in clinic for those who did not receive chemotherapy. Patients who did not receive chemotherapy were generally referred for community palliative care support and discharged from the oncology clinic. Given historical 12-month survival rates of <30% for advanced pancreatic adenocarcinoma, the database was frozen for survival analysis on 30 September 2015, permitting sufficient follow-up to calculate 12-month survival for all patients and enough events to compare survival between both groups in the study. Thirty-day mortality on chemotherapy was taken as an interval of 30 days or less between the date of the last dose of chemotherapy was received and the date of death. Furthermore, overall survival was taken as the interval between the date of the first visit to a CCC clinic and the date of death. We tested for any differences between groups in demographics, baseline characteristics, diagnosis of diabetes mellitus, type of treatment received and 30-day mortality on chemotherapy by χ2 analysis. Overall survival was computed by the Kaplan–Meier technique with log-rank analysis. Statistical analysis was performed by CET Statisticians CI and HW utilizing SPSS analytic software (version 20.0, IBM, New York, NY, USA).
Results
Baseline and treatment characteristics of patients
The baseline characteristics of patients in early (E) and late (L) groups (are displayed in Table 1A). In summary, similar numbers of patients referred from the regional MDT were managed for advanced pancreatic adenocarcinoma in both groups. There was no significant difference in the age and gender distribution of both the groups. However, there was significantly higher prevalence of diabetes mellitus in Group L. In addition, increased prevalence of metastatic disease in group L approached significance. Of note is that a significantly higher proportion of patients received chemotherapy in Group L. Further analysis in the metastatic subset of patients suggested that chemotherapy treatment was received by 36.1% (n=72) in Group E and 63.4% (n=82) in Group L. We also compared the time to commencement of chemotherapy after initial review between both groups and observed a reduced time to commencement of chemotherapy in group L (E: mean=28 days, 95% CI=21–34; L: mean=18 days, 95% CI=15–22; P=0.001). Therefore, patients treated in central clinics had increased likelihood of commencing chemotherapy and did so earlier than in the devolved clinics.
Overall survival with chemotherapy treatment
Progressive cancer was the most commonly documented cause of death for patient in both groups (91.7% (Group E] vs 82.8% [Group L)). To determine if there was any difference in overall survival between both groups, we compared survival between Groups E and L and observed significantly increased survival for patients in Group L (Figure 1A). As there was a higher proportion of patients with metastatic disease in group L and the prognosis of metastatic disease is worse (Bilimoria et al, 2007), we combined Groups E and L, then determined if there was a difference in overall survival between patients with locally advanced (LA) and metastatic (M) disease (Figure 1B). We observed significantly increased survival for patients with locally advanced compared with metastatic disease. We then compared overall survival for patients with LA or metastatic disease between groups E and L. There was no difference in overall survival between groups E and L for LA disease (data not shown). In contrast, longer survival was observed for patients with metastatic disease in Group L (Figure 1C). Therefore, there was a 36% improvement in overall survival for the subgroup of patients with metastatic disease treated in centralised clinics.
Displays overall survival curves for patients with advanced pancreatic adenocarcinoma. (A) There was improved survival (HR: 0.785; P=0.045) for Group L (green; n=115) compared with Group E (blue; n=121). The median overall survival (and 12-month survival) were: 5 months (14.8%) for Group L compared with 3 months (11.6%) for Group E. (B) Combining Groups E and L showed improved survival (HR: 0.637; P=4.19 × 10−4) for LA (n=82) compared with metastatic disease (n=154). The median overall survival (and 12-month survival) was 7 months (17.1%) for patients with LA compared with 3 months (11.0%) for patients with metastatic disease. (C) For the patients with metastatic disease, there was improved survival (HR: 0.641; P=0.002) for Group L (green; n=82) compared with Group E (blue; n=72). The median overall survival (and 12-month survival) was 4 months (13.4%) for patients in Group L compared with 3 months (8.3%) for patients in Group E.
To assess survival with chemotherapy treatment in both groups, survival was compared between patients who received chemotherapy and those who did not in either group (Figures 2A and B). Patients who received chemotherapy had significantly improved survival in both groups with similar median overall survival. Therefore, despite the increased proportion of patients treated with chemotherapy in Group L, survival was similar for patients treated with chemotherapy between centralised and devolved clinics.
Displays survival curves for patients with advanced pancreatic adenocarcinoma with or without chemotherapy treatment. (A) Improved survival (HR: 0.307; P= <1 × 10−4) with chemotherapy (green; n=52) compared with no chemotherapy treatment (blue; n=69) in Group E. The median overall survival (and 12-month survival) was as follows: 7 months (23.1%) with chemotherapy compared with 2 months (2.9%) without chemotherapy. (B) Improved survival (HR: 0.229; P=<1 × 10−4) with chemotherapy (green; n=77) compared with no chemotherapy treatment (blue; n=38) in Group L. The median overall survival (and 12-month survival) was as follows: 7 months with chemotherapy (22.1%) compared with 2 months (0%) without chemotherapy.
Chemotherapy treatment received by patients
Analysis of chemotherapy regimens received by patients in Groups E and L is displayed in Table 1B: A Gemcitabine-containing regimen was the most common regimen received in the first-line setting in either group. More patients participated in clinical trials (based on Gemcitabine regimens) in Group E, while FOLFIRINOX chemotherapy (as a first-line regimen) was only available to patients in Group L. Significantly more patients received second-line chemotherapy in Group L compared with Group E (23.4% (n=18) vs 1.9% (n=1); P=1.4 × 10−4). Therefore, patients were more likely to receive second-line chemotherapy in the centralised clinics.
Thirty-day mortality and patient survival on chemotherapy
Thirty-day mortality on chemotherapy was compared between Groups E and L (Table 1B). There was no significant difference in 30-day mortality between both groups (E=25% vs L=20.8%, P=0.573). Furthermore, with the assumption of proportional hazards of death for a median survival of 2 months, 30-day mortality for patients who did not receive chemotherapy would be ∼25%.
Overall survival by first-line chemotherapy regimen received is displayed in Figure 3A. Median overall survival was 8 months for FOLFIRINOX (n=9), 7 months for Gemcitabine (n=87) and 9 months for Gemcitabine trials (n=33). With patients on Gemcitabine (off trials) as reference, there was improved survival for patients who received Gemcitabine on trials but not with FOLFIRINOX treatment (Figure 3A). Twelve-month survival was 33.3% for FOLFIRINOX, 17.2% for Gemcitabine and 33.3% for Gemcitabine trials. Overall survival for the patients who received second-line chemotherapy is displayed in Figure 3B. Median overall survival for such patients (from time of diagnosis) was 11 months, with 42.1% alive at 12 months. In contrast, median overall survival from the time of commencement of second-line chemotherapy was 5 months (Figure 3C).
Displays overall survival curves for patients with advanced pancreatic adenocarcinoma who received chemotherapy. (A) Survival for patients who received different first-line chemotherapy regimens for advanced pancreatic adenocarcinoma; (Gemcitabine—green (n=87), Gemcitabine trials—grey (n=33) and FOLFIRINOX—blue (n=9)). The median overall survival (and 12-month survival) with the regimens were as follows: 7 months–Gemcitabine (17.2%); 9 months—Gemcitabine trials (33.3%); and 8 months—FOLFIRIONOX (33.3%). Patients on Gemcitabine trials had significantly improved survival compared with Gemcitabine off trials (P =0.02). In contrast, there was no significant difference in survival between those who received Gemcitabine off-trials and those who received FOLFIRINOX treatment (P=0.168). (B) Survival for patients who received second-line chemotherapy. The median overall survival was 11 months with a 12-month survival of 42.1% (n=19). (C) Survival for patients from commencement of second-line chemotherapy. The median overall survival was 5 months with no 12-month survivor (n=19).
Exploratory analysis of chemotherapy treatment by age
To determine if there was an age bias in selection of patients for chemotherapy, we analysed treatment in Groups E and L by age-group, comparing patients ⩽70 years of age with those >70 years of age. Significantly less patients >70 years of age were treated with chemotherapy in Group E (>70: 24.5% (n=53) vs ⩽70: 57.4% (n=48); P=3.0 × 10−4—Table 2A). We then compared chemotherapy treatment between patients up to and those >70 years of age in Group L. There was no significant difference in chemotherapy treatment by age in Group L (Table 2A). As there was no significant age bias in selection for chemotherapy in Group L, we compared survival between those up to or >70 years of age (Figure 4A), no significant difference in overall survival was observed. Similarly, no significant difference in 30-day mortality was observed (Table 2A). Finally, to determine the survival impact of increased utilization of chemotherapy in the older population of patients, we compared survival between groups E and L for patients >70 years of age (Figure 4B). Increased overall survival was observed for patients >70 years in Group L compared with E. Therefore, older patients (>70) were at least twice as likely to receive chemotherapy with centralised care. This translated to increased survival similar to that of younger patients who received chemotherapy.
Displays overall survival curves for sub-populations with advanced pancreatic adenocarcinoma. (A) There was no significant difference in survival (P=0.606) for patients treated with chemotherapy in Group L stratified by age (blue: >70 years; n=28) and (green ⩽ 70 years; n=49). The median overall survival (and 12- month survival) was as follows: 7 months (17.9%) for older patients compared with 8 months (24.5%) for younger patients. (B) There was improved survival (HR: 0.698; P=0.047) for older patients (>70 years of age) in Group L (green: n=48) compared with Group E (blue: n=53). The median overall survival (and 12-month survival) was as follows: 4 months (10.4%) for Group L compared with 3 months (7.5%) for Group E. (C) There was no significant difference in survival (P=0.324) for all patients of PS0 and 1 between Group E (blue; n=45) and Group L (green; n=71). The median overall survival (and 12-month survival) was as follows: 8 months for Group E (28.9%) compared with 6 months for Group L (18.3%). (D) There was improved survival for patients of PS2 (HR: 0.594; P=0.022) in Group L (green; n=30) compared with Group E (blue; n=40). The median overall survival (and 12-month survival) was 4 months (13.3%) for patients in Group L compared with 3 months (0%) for patients in Group E.
Exploratory analysis of chemotherapy treatment by performance status in older patients
To determine if poorer performance status (>2) in patients >70 years of age explains reduced utilization of chemotherapy treatment in Group E, we analysed patient distribution for performance status by age in Groups E and L (Table 2A). A significantly reduced proportion was estimated to be of PS 0–2 among patients >70 compared with patients up to 70 years of age in Group E (⩽70: 80.9% (n=68) vs >70: 56.6% (n=53); P=0.004). In contrast, while there was a trend towards higher performance status in general in Group L, there was no significant difference in the proportion of patients estimated to be of PS 0–2 by age in Group L (⩽70: 91.0% (n=67) vs >70: 83.3% (n=48); P=0.21). Therefore, there was a trend to a poorer performance status estimate for older patients with devolved care associated with non-reception of chemotherapy.
Exploratory analysis of chemotherapy treatment and survival by performance status in the entire population
To determine if there was any difference in chemotherapy treatment between Groups E and L at a given performance status estimate, we summarized chemotherapy treatment by performances status in both groups (Table 2B). There was no significant difference in the proportion of patients who received chemotherapy at a given performance status. However, the proportion of ‘fit’ patients (PS 0 and 1) in Group E was 36.9% (n=121) compared with 61.8% (n=115) in Group L. Therefore, while reception of chemotherapy treatment was not significantly different at a given PS in both groups, patients in Group E were generally estimated to be of lower performance status than those in Group L.
Given the difference in PS distribution between both groups, we then compared overall survival for ‘fit’ patients (PS0/1—Figure 4C) and for relatively ‘frail’ patients (PS2—Figure 4D) between Groups E and L. Overall survival was similar for PS0/1 patients between Groups E and L. In contrast, patients of PS2 had significantly improved survival in Group L compared with Group E (HR: 0.594, P=0.022). Furthermore, 12-month survival for the PS2 population was 13.3% for Group L while there were no 12-month survivors for Group E. Therefore, similar survival to devolved care was observed for the proportionately larger PS0/1 population with centralised care. In contrast, longer survival was observed for the PS2 population with centralised care. Given the lead-time bias to initial clinic review in Group L, for the small but frailer PS2 population, we compared time to commencement of chemotherapy and survival between Groups E and L (from the time of commencement of chemotherapy). Improved survival for PS2 patients from the time of commencement of chemotherapy was observed in Group L (HR: 0.41, P=0.012—Supplementary Figure 1).
Exploratory analysis of chemotherapy regimen by age and performance status
Patients who received FOLFIRINOX (median age=53.2; n=9) were younger than those who received Gemcitabine (median age=68.8; n=87) or participated in Gemcitabine trials (median age=66.9; n=33). Furthermore, patients who received FOLFIRINOX were entirely of PS 0 and 1, while patients who received Gemcitabine were mostly of PS 1 and 2 (Supplementary Table 1). There was no significant difference in 30-day mortality between the regimens. Therefore, there was a trend to FOLFIRIONOX been given to younger, fitter patients. Notably, all those who received FOLFIRINOX also received second-line chemotherapy, while only a minority (11.5%) of those who received Gemcitabine received second-line chemotherapy.
Discussion
The crucial findings in this study on advanced pancreatic adenocarcinoma management are that transition to centralised care tended to increase performance status overall (possibly by improved supportive care), associated with increased utilization of systemic chemotherapy and longer survival. Noteworthy is that the proportion of patient treated with chemotherapy prior to centralisation of care in our centre and the median survival for patients with metastatic disease prior to centralisation were very similar to that of the previously reported UK retrospective study (Mukherjee et al, 2008). The increment in survival with centralised care for this poor prognosis malignancy was modest, but reassuringly, the increased utilisation of chemotherapy with centralisation was achieved without delayed clinical review or a rise in the proportion of deaths within 30 days of chemotherapy treatment. Unfortunately, we did not have the serial PS data collected to determine if earlier initial clinic review or improved supportive care in centralised clinics explained improved overall PS in central clinics. However, the improved detection of diabetes with centralised care may reflect improved screening for purposes such as a supportive care measure. Furthermore, there was no objective way to correlate quality of life with the clinic journey times and survival differences observed in this study.
Notably, older patients, less fit patients (PS2) and those with metastatic disease who instinctively would be more likely to be recommended to the convenience of devolved care, benefitted the most from centralised care. However, increased utilisation of supportive input such as from the HPB-specialist nurses/dieticians/palliative care and more rapid access to HPB-specialist medical support through the centralised clinics would be the most plausible explanation. Furthermore, given the subjectivity of PS assessment, underestimation of patient fitness for initiation and continuation of chemotherapy in the devolved care setting is possible. Particularly, when patients with advanced pancreatic adenocarcinoma are seen in joint clinics dominated by patients with less morbid malignancies. However, with respect to fitness, the assessment of PS at the time of initial review (for untreated patients) but the time of commencement of chemotherapy (for treated patients) may have introduced bias. This would have favoured patients who received centralised care, given the greater proportion of patients who received chemotherapy in that group. Nevertheless, the improved fitness and longer overall survival with the centralised care approach would be desirable, irrespective of a less nihilistic chemotherapy fitness assessment or frailer populations benefitting from a more proactive management pathway being the explanation. However, distinction between these two possibilities would be crucial to guide service design, particularly as regards to the possibility of improving outcomes with better supportive care in the devolved care setting. Similar to observations with devolved care in this study (on advanced disease), a retrospective study in the US observed overall less treatment for older patients with early pancreatic adenocarcinoma (Amin et al, 2013).
While 30-day mortality on chemotherapy may have appeared nominally high at 20–25%, the mortality was not significantly different with centralisation and estimated not to be higher than that for advanced pancreatic cancer patients off chemotherapy. Patients treated with first-line Gemcitabine achieved median and 12-month survival comparable to patients treated with Gemcitabine on the control arm of the largest of the most recent first-line clinical trials (von Hoff et al, 2013). Therefore, given that >95% of our patients on chemotherapy were on first-line Gemcitabine regimens, this would suggest safe translation of the modest benefit from previous first-line Gemcitabine trials to the treated ‘real-world’ patient population in this study. While there was no significant difference in survival for the PS0/1 population between centralised and devolved clinics, longer survival for the ‘relatively frail PS2 sub-set’ in centralised clinics may reflect increased willingness to persist with systemic treatment in the less fit PS2 population in conjunction with better supportive care. The fact that first-line trials were open throughout the period of devolved care covered by this study, but only for part of the period covered by centralised care, probably explains the increased recruitment to first-line trials with devolved care.
The median overall survival of 5 months on second-line chemotherapy compares favourably with recent fluoropyrimidine-based second-line clinical trials (Pelzer et al, 2011; Oettle et al, 2014). In the central clinics, utilization of second-line chemotherapy was nominally higher than the UK average of 15% (Smyth et al, 2015). However, definitive clinical trial evidence of the benefit of second-line chemotherapy emerged during the period of transition from devolved to centralised care in this study. While increased utilization of second-line chemotherapy and the introduction of FOLFIRINOX with centralised care are potential confounding factors in survival analysis here, some observations would argue against their significance. The patients on FOLFIRINOX who comprised half of the populations that received second-line chemotherapy in central clinics had no discernible survival benefit.
The observation of comparable overall survival between FOLFIRINOX and Gemcitabine treatment was possibly due to median overall survival for our patients on FOLFIRINOX at 8 months being inferior to 11 months in the Conroy study (Conroy et al, 2011). This was despite all our patients on FOLFIRINOX receiving second-line Gemcitabine compared with ∼50% of those on the Conroy study. However, given its recent introduction as at that point in time and concerns about regimen toxicity, the FOLFIRINOX-treated population appeared very highly selected (comprising only 9 patients) and treatment was given without the 5-FU bolus. We cannot exclude the possibility that efficacy of the FOLFIRIONOX regimen may have been compromised by omission of the 5-FU bolus. The only published trial of equivalent efficacy of an attenuated FOLFIRIONX regimen to date, modified the regimen in a different way but retained the 5-FU bolus component. However, it reported that efficacy was similar despite the modification (Stein et al, 2016). Furthermore, the young population treated may have different disease biology and thus be unrepresentative of typical survival outcomes with the regimen. These possibilities require further evaluation. Survival for patients on first-line Gemcitabine trials was longer than that for Gemcitabine off-trial in this study. However, there was no survival benefit on the intervention arm of the first-line trial, which ran for most of the period of the study (Middleton et al, 2014), while the results of the second trial are yet to be published. The longer survival on trials may just reflect better overall care on clinical trial protocols, which has previously been reported to be associated with improved survival (Stead et al, 2011).
Our study has several limitations. The populations compared were sequential rather than in parallel, meaning that improvements, in general, such as in medical/oncology care, introduction of Acute Oncology teams/patient management pathways could have improved outcome in Group L. Furthermore, there were also differences in chemotherapy regimen utilisation with centralised care. The inadvertent difference in managing oncologists between devolved and centralised care is also another potential confounder. Consequently, the contribution of any or a combination of these to survival differences is uncertain.
In conclusion, following transition to a centralised clinic model in a tertiary cancer centre, we show safely increased utilization of chemotherapy with a modest increase in overall survival for patients with advanced pancreatic adenocarcinoma. Additionally, we show that survival with first and second line chemotherapy was similar to observations in clinical trials except for the limited number of patients treated with FOLFIRIONOX. Counter-intuitively, the benefits of centralised care were greatest for older patients, those with metastatic disease and less fit patients. Further prospective studies are required to validate the findings reported from this exploratory study, to facilitate harnessing the modest but increasing benefit of treatment for this poor prognostic malignancy. However, to inform service design, such studies will need to be appropriately designed to make the distinction between inadequate resourcing for supportive care and nihilism in the devolved care setting.
Change history
14 February 2017
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Amin S, Lucas AL, Frucht H (2013) Evidence for treatment and survival disparities by age in pancreatic adenocarcinoma: a population-based analysis. Pancreas 42 (2): 249–253.
Bilimoria KY, Bentrem DJ, Ko CY, Ritchey J, Stewart AK, Winchester DP, Talamonti MS (2007) Validation of the 6th edition AJCC pancreatic cancer staging system: report from the National Cancer Database. Cancer 110 (4): 738–744.
Burris HA 3rd, Moore MJ, Andersen J, Green MR, Rothenberg ML, Modiano MR, Cripps MC, Portenoy RK, Storniolo AM, Tarassoff P, Nelson R, Dorr FA, Stephens CD, Von Hoff DD (1997) Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol 15 (6): 2403–2413.
Cancer Research UK (2016) http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/pancreatic-cancer (accessed on 30 April 2016).
Conroy T, Desseigne F, Ychou M, Bouché O, Guimbaud R, Bécouarn Y, Adenis A, Raoul JL, Gourgou-Bourgade S, de la Fouchardière C, Bennouna J, Bachet JB, Khemissa-Akouz F, Péré-Vergé D, Delbaldo C, Assenat E, Chauffert B, Michel P, Montoto-Grillot C, Ducreux M Groupe Tumeurs Digestives of Unicancer; PRODIGE Intergroup (2011) FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med 364 (19): 1817–1825.
Sirri E, Castro FA, Kieschke J, Jansen L, Emrich K, Gondos A, Holleczek B, Katalinic A, Urbschat I, Vohmann C, Brenner H (2016) Recent trends in survival of patients with pancreatic cancer in Germany and the United States. Pancreas 45 (6): 908–914.
Garrido-Laguna I, Hidalgo M (2015) Pancreatic cancer: from state-of-the-art treatments to promising novel therapies. Nat Rev Clin Oncol 12 (6): 319–334.
Gooiker GA, Lemmens VE, Besselink MG, Busch OR, Bonsing BA, Molenaar IQ, Tollenaar RA, de Hingh IH, Wouters MW (2014) Impact of centralization of pancreatic cancer surgery on resection rates and survival. Br J Surg 101 (8): 1000–1005.
Middleton G, Silcocks P, Cox T, Valle J, Wadsley J, Propper D, Coxon F, Ross P, Madhusudan S, Roques T, Cunningham D, Falk S, Wadd N, Harrison M, Corrie P, Iveson T, Robinson A, McAdam K, Eatock M, Evans J, Archer C, Hickish T, Garcia-Alonso A, Nicolson M, Steward W, Anthoney A, Greenhalf W, Shaw V, Costello E, Naisbitt D, Rawcliffe C, Nanson G, Neoptolemos J (2014) Gemcitabine and capecitabine with or without telomerase peptide vaccine GV1001 in patients with locally advanced or metastatic pancreatic cancer (TeloVac): an open-label, randomised, phase 3 trial. Lancet Oncol 15 (8): 829–840.
Mukherjee S, Hudson E, Reza S, Thomas M, Crosby T, Maughan T (2008) Pancreatic cancer within a UK cancer network with special emphasis on locally advanced non-metastatic pancreatic cancer. Clin Oncol (R Coll Radiol) 20 (7): 535–540.
Neoptolemos JP, Russell RC, Bramhall S, Theis B (1997) Low mortality following resection for pancreatic and periampullary tumours in 1026 patients: UK survey of specialist pancreatic units. UK Pancreatic Cancer Group. Br J Surg 84 (10): 1370–1376.
Oettle H, Riess H, Stieler JM, Heil G, Schwaner I, Seraphin J, Görner M, Mölle M, Greten TF, Lakner V, Bischoff S, Sinn M, Dörken B, Pelzer U (2014) Second-line oxaliplatin, folinic acid, and fluorouracil versus folinic acid and fluorouracil alone for gemcitabine-refractory pancreatic cancer: outcomes from the CONKO-003 trial. J Clin Oncol 32 (23): 2423–2429.
Pelzer U, Schwaner I, Stieler J, Adler M, Seraphin J, Dörken B, Riess H, Oettle H (2011) Best supportive care (BSC) versus oxaliplatin, folinic acid and 5-fluorouracil (OFF) plus BSC in patients for second-line advanced pancreatic cancer: a phase III-study from the German CONKO-study group. Eur J Cancer 47 (11): 1676–1681.
Smyth EN, Bapat B, Ball DE, André T, Kaye JA (2015) Metastatic Pancreatic Adenocarcinoma treatment patterns, health care resource use, and outcomes in France and the United Kingdom between 2009 and 2012: a retrospective study. Clin Ther 37 (6): 1301–1316.
Stead M, Cameron D, Lester N, Parmar M, Haward R, Kaplan R, Maughan T, Wilson R, Campbell H, Hamilton R, Stewart D, O'Toole L, Kerr D, Potts V, Moser R, Darbyshire J, Selby P National Cancer Research Networks across the UK (2011) Strengthening clinical cancer research in the United Kingdom. Br J Cancer 104 (10): 1529–1534.
Stein SM, James ES, Deng Y, Cong X, Kortmansky JS, Li J, Staugaard C, Indukala D, Boustani AM, Patel V, Cha CH, Salem RR, Chang B, Hochster HS, Lacy J (2016) Final analysis of a phase II study of modified FOLFIRINOX in locally advanced and metastatic pancreatic cancer. Br J Cancer 114 (7): 809–812.
van Lanschot JJ, Hulscher JB, Buskens CJ, Tilanus HW, ten Kate FJ, Obertop H (2001) Hospital volume and hospital mortality for esophagectomy. Cancer 91 (8): 1574–1578.
von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, Seay T, Tjulandin SA, Ma WW, Saleh MN, Harris M, Reni M, Dowden S, Laheru D, Bahary N, Ramanathan RK, Tabernero J, Hidalgo M, Goldstein D, Van Cutsem E, Wei X, Iglesias J, Renschler MF (2013) Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med 369 (18): 1691–1703.
Worni M, Guller U, White RR, Castleberry AW, Pietrobon R, Cerny T, Gloor B, Koeberle D (2013) Modest improvement in overall survival for patients with metastatic pancreatic cancer: a trend analysis using the surveillance, epidemiology, and end results registry from 1988 to 2008. Pancreas 42 (7): 1157–1163.
Acknowledgements
This study was supported by Clinical Effectiveness team CCC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Faluyi, O., Connor, J., Chatterjee, M. et al. Advanced pancreatic adenocarcinoma outcomes with transition from devolved to centralised care in a regional Cancer Centre. Br J Cancer 116, 424–431 (2017). https://doi.org/10.1038/bjc.2016.406
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2016.406
- Springer Nature Limited
Keywords
This article is cited by
-
Initial treatment is associated with improved survival and end-of-life outcomes for patients with pancreatic cancer: a cohort study
BMC Cancer (2022)
-
Prolonged time to treatment initiation in advanced pancreatic cancer patients has no major effect on treatment outcome: a retrospective cohort study controlled for lead time bias and waiting time paradox
Journal of Cancer Research and Clinical Oncology (2020)
-
Economic Evaluation for the UK of Systemic Chemotherapies as First-Line Treatment of Metastatic Pancreatic Cancer
PharmacoEconomics (2018)