Abstract
Background:
Eribulin mesylate is a synthetic microtubule inhibitor that showed cytotoxic synergy in combination with gemcitabine preclinically. This combination was assessed in a Phase I dose-finding trial in patients diagnosed with advanced solid tumours who had received up to two prior chemotherapy regimens for metastatic disease (CP cohort).
Methods:
Dose escalation was performed in a 3+3 design to identify the recommended phase II dose (RP2D). Two additional expansion cohorts in women with gynaecologic cancers at the RP2D (G), and further dose escalation of metastatic chemotherapy-naive patients (CN), were evaluated.
Results:
45 patients were treated: 21 (CP), 10 (G) and 14 (CN). The initial combination of eribulin and gemcitabine was administered on days 1, 8, and 15 of a 28-day cycle; however, due to 2 out of 6 dose-limiting haematological toxicities at the first dose level, a reduced dose-intense schedule was assessed. The RP2D was defined at 1.0 mg m−2 eribulin and 1000 mg m−2 gemcitabine day 1 and 8 q3 weeks. No other significant toxicities were observed in the G expansion cohort. Neutropenia prevented further dose escalation in the CN cohort. Objective responses were seen in all three cohorts – 2/21 (CP), 1/10 (G) and 2/14 (CN).
Conclusions:
The combination of eribulin and gemcitabine was well tolerated at the RP2D.
Similar content being viewed by others
Main
Eribulin mesylate is a non-taxane, synthetic microtubule inhibitor developed from halichondrin B, a natural marine product. Eribulin inhibits microtubule dynamics by binding to a unique site on tubulin (Dabydeen et al, 2006; Okouneva et al, 2008), resulting in the suppression of microtubule polymerisation, without effects on depolymerisation (Jordan et al, 2005). Eribulin exhibited in vitro and in vivo activities against a wide number of malignancies (Towle et al, 2001), particularly in disease models in which microtubule inhibitors have a therapeutic role such as in breast or ovarian cancers (Shablak, 2013). Eribulin has been recently approved as a third-line therapy for metastatic breast cancer patients, who have previously been treated with an anthracycline and a taxane (Swami et al, 2012). Eribulin monotherapy is administered as intravenous (IV) dose of 1.4 mg m−2 on days 1 and 8 of a 21-day cycle. The predominant toxicities are neutropenia and fatigue.
Preclinical studies show synergy when eribulin is combined with gemcitabine, inducing tumour regression in non-small cell lung cancer (NSCLC) xenografts (Towle et al, 2003; Kuznetsov et al, 2009). Gemcitabine is a cell cycle-dependent antineoplastic chemotherapeutic agent of the antimetabolite class. Gemcitabine exerts cytotoxicity through apoptosis following inhibition of DNA synthesis with incorporation of pyrimidine analogues into DNA (Plunkett et al, 1995). Gemcitabine is commonly used at a dose of 1000 mg m−2 IV in several malignancies such as advanced NSCLC (Abratt et al, 1944; Gatzemeier et al, 2004), pancreatic (Carmichael et al, 1996; Mattiucci et al, 2013), ovarian, breast (Lorusso et al, 2003) and bladder cancers (Von der Maase et al, 2000). Common toxicities of gemcitabine include myelosuppression, gastrointestinal toxicity such as nausea, vomiting and diarrhoea, rash, flu like symptoms and abnormalities in liver function tests (Aapro et al, 1998). A phase I clinical trial was conducted to determine the safety and tolerability of the combination of eribulin with gemcitabine in patients with refractory or advanced solid tumours. No pharmacokinetics data were done as this combination was not expected to be at risk for drug–drug interaction.
Materials and Methods
Patient eligibility
Adult patients (>18 years) with histologically confirmed metastatic or unresectable malignancy with no curative treatment options were eligible. Other eligibility criteria included the following: measurable disease, ECOG performance status 0 to 2, maximum of two prior chemotherapy regimens for metastatic disease, prior therapy completed at least 4 weeks prior to registration, adequate bone marrow and organ function (leukocytes >3 × 109 l−1, absolute neutrophil count (ANC) ⩾1.5 × 109 l−1, platelets ⩾100 × 109 l−1, total bilirubin within normal institutional limits, AST/ALT ⩽2.5 × institutional upper limit of normal, creatinine clearance ⩾60 ml min−1 1.73 m−2). Prior treatment with gemcitabine or eribulin was not allowed. Prior radiation could not have encompassed more than 40% of a patient’s bone marrow. Patients had to have recovered from any toxicity related to prior therapy at the time of registration. As CYP3A4 appears to be the major enzyme responsible for hepatic metabolism of eribulin, the concurrent use of inhibitors and inducers of CYP3A4 were prohibited. All patients gave informed written consent. The study was approved by the Ontario Cancer Research Ethics Board and registered on ClinicalTrials.gov (NCT00410553) and was conducted in accordance with Good Clinical Practice guidelines.
Trial design and procedures
This was an open-label, phase I, dose-escalation trial conducted by the Princess Margaret Phase II Consortium in conjunction with the US National Cancer Institute Cancer Therapy Evaluation Program, and was performed at two participating institutions, the Ottawa Hospital (Ottawa, ON, Canada) and Princess Margaret Cancer Centre (Toronto, ON, Canada). The primary objectives were to determine the dose-limiting toxicities (DLT) and recommended phase II dosing (RP2D) of the eribulin/gemcitabine combination. Secondary objectives included the assessment of treatment-related toxicities and preliminary assessment of clinical activity as measured by response rate and progression-free survival (PFS), defined as time from initiation of therapy to disease progression or death from any cause. Patients were treated with eribulin as an IV bolus and gemcitabine IV over 30 min, after completion of the eribulin infusion. The starting dose level (DL) 1 was eribulin 0.7 mg m−2 and gemcitabine 800 mg m−2, on day 1, 8, and 15 for the 28-day schedule (Q4W). This was switched to a 21-day cycle (Q3W) on day 1 and 8 after two DLT were seen in DL 1 on the 28-day schedule. Patients were premedicated with dexamethasone 10 mg IV plus additional antiemetics according to institutional guidelines before eribulin IV bolus. Dose escalation occurred in the standard 3+3 design. Treatment continued until disease progression, unacceptable toxicity or patient withdrawal. Dose escalation was continued until DLT was observed in two or more of the 3–6 patients. The RP2D was defined as the highest dose level with at least six patients where one or fewer patients experienced a DLT. Once RP2D was determined, two expansion cohorts of patients were planned in ovarian/endometrial cancer and in patients who were chemotherapy naive for the setting of metastatic disease. Patients remained on treatment until progression, unless they had unmanageable adverse events (AEs), or requested to discontinue therapy. In the first gynaecological cohort (limited to ovarian/endometrial cancer), patients received both drugs at the RP2D. In the second metastatic chemotherapy-naive cohort, patients were treated at dose levels above the RP2D on the 21-day cycle. It was felt that such patients would tolerate higher doses of the study regimen drugs.
Toxicity criteria and dose modifications
DLT was based on cycle 1 and defined as any grade 3 or 4 non-haematologic toxicity (with the exception of alopecia, or nausea/vomiting unless the latter occurs despite maximal supportive measures), any grade 4 haematologic toxicity lasting for more than 7 days, febrile neutropenia, inability to deliver days 8 and/or 15 in a 28-day cycle (during cycle 1) or day 8 in a 21-day cycle (during cycle 1), or the inability to initiate study drugs on day 1 of cycle 2 for more than 2 weeks from the scheduled date due to drug-related AEs. Toxicities were graded using the National Cancer Institute Common Toxicity Criteria for Adverse Events version 3.0 (DCTD, NCI, NIH, DHHS; http://ctep.cancer.gov). Doses of eribulin and gemcitabine were adjusted according to the set criteria based on the degree of haematologic and non-haematologic toxicities observed in the previous cycle. In order to be eligible to start the next cycle, patients were required to have adequate haematologic parameters: ANC ⩾1.5 × 109 l−1 and platelets ⩾100 × 109 l−1. In order to proceed with day 8 treatment (and day 15 treatment in the 28-day schedule), patients were required to have ANC ⩾1.0 × 109 l−1 and platelets ⩾50 × 109 l−1.
Clinical activity
Clinical response was assessed by RECIST version 1.0 (Therasse et al, 2000). Imaging assessments were performed by CT scanner at baseline and every 2 cycles. Any partial or complete response required confirmatory imaging ⩾4 weeks after the initial imaging demonstrating response.
Results
The study was activated is November 2006 and was closed permanently to accrual on June 2012.
Patient characteristics
In the dose-escalation cohort (21- and 28-day schedule), 21 patients were enroled and all received at least one dose of the combination eribulin and gemcitabine. Baseline characteristics are presented in Table 1. After establishing RP2D, 10 women with gynaecologic malignancies were treated in an expansion cohort. Nine of these patients had ovarian cancer and one had endometrial cancer. All patients had been pretreated with systemic therapy for metastatic disease with a median number of two prior regimens. Fourteen chemo-naive patients were accrued and further dose escalation was attempted.
Dose escalation
Dose escalation and toxicities are shown on Table 2. Six patients were treated at DL 1 on the 28-day cycle schedule. At this DL 1, two DLTs occurred (grade 3 and 4 thrombocytopenia leading to reduced dose-intensity treatment on cycle 1 or delay in the initiation of cycle 2); subsequent patients were accrued to dose levels on the 21-day cycle regimen. Three patients were treated on the Q3W DL 1, 2 and 3 each with no DLT observed (Table 2). At DL 4, two patients developed DLT (grade 3 diarrhoea and grade 3 fatigue). Therefore, three more patients were treated on DL 3 and one patient developed DLT (grade 4 neutropenia with missing dose on cycle 1) over a total of six patients in this dose level. Thus, DL 3 defined by 1.0 mg m−2 eribulin with 1000 mg m−2 gemcitabine; both day 1 and 8 every 21 days, was considered as the RP2D. Haematologic toxicity was not dose-limiting when the chemotherapy regimen was given in a 21-day cycle; however, increasing dose of chemotherapy regimen from DL 1 to DL 3 was associated with a trend towards increasing myelosuppression, with a drop in the median nadir levels of haemoglobin, leukocyte and neutrophil counts (Supplementary Table 1A). A total of 77 cycles of treatment were administered to the 21 patients enroled, with a median number of 2 cycles (1–12). Sixteen and five patients discontinued study due to disease progression and toxicity respectively.
Expansion cohorts
Gynaecologic cohort
Ten patients treated at the RP2D received a total of 75 cycles of chemotherapy administered with a median number of 6 cycles (2–18). No DLT was observed. Eight and two patients discontinued study due to disease progression and toxicity, respectively. The toxicity profile was not significantly different from the patients in the dose-escalation cohort.
Metastatic chemotherapy-naive cohort
Fourteen patients were enroled from DL 4–6, these additional dose escalations were used for this cohort as patients were not exposed to previous chemotherapy in the metastatic setting (two patients received adjuvant chemotherapy). A total of 90 cycles of treatment were given with a median number of 5 cycles (1–16). Only two patients were enroled at DL 6 as the second patient experienced severe neutropenia G4. Ten and three patients discontinued due to progressive disease and toxicity, respectively. The major limitation beyond RP2D in the metastatic chemotherapy-naive cohort patients was myelosuppression in either the first cycle (Supplementary Table 1B) or later cycles. Based on the increased frequency of grade 3 and 4 neutropenia observed at DL 4, 5 or 6, the RP2D remained DL 3 even for the metastatic chemotherapy-naive patients.
Safety profile
The most common grade 3 or 4 toxicities were haematologic (Tables 3 and 4). The most common grade 3 or 4 biochemical toxicities were reversible elevation of liver transaminases. The main grade 3 or 4 non-hematolgic toxicities – observed in at least two cycles of therapy – were fatigue, diarrhoea, nausea and vomiting. There was no death attributable to chemotherapy-related toxicity.
Of the 45 patients in total (over all the investigated cohorts), 15 patients had dose reductions, 23 patients missed a dose and 28 patients had dose delays. All 45 patients experienced at least one treatment-related AE, with the most frequently occurring treatment-related AEs being haematological toxicities.
Clinical activity
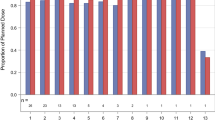
In the dose escalation cohort, among the RECIST-evaluable patients (17 of 21 patients), the best responses observed were two partial responses (PR) in one patient diagnosed with ovarian cancer and the second patient with head and neck carcinoma (10% of patients) and eight stable disease (SD; 38% of patients) with a median duration of 6.2 months (1.5–14.6). In the gynaecological expansion cohort, there was one PR (ovarian cancer) and seven SD (six SD in the ovarian subgroup and one SD with endometrial cancer) with a median SD duration of 6 months (2.9–15). In the chemotherapy-naive cohort, two PR (patients with unknown primary and pancreatic cancer) and eight SD with a median duration of 5.9 months (2.3–14.3) were observed (Table 5). Overall, the median PFS was 3.7 months (1.6–5.8). In the specific ovarian cancer subgroup, the median PFS was 4.5 months (1.6–15.2; Figure 1). No patients remain on treatment.
Discussion
This trial demonstrated a RP2D of the combination of eribulin 1.0 mg m−2 and gemcitabine 1000 mg m−2 on days 1 and 8 every 21 days. This combination was feasible and toxicity was generally manageable. Haematologic toxicity prevented further dose escalation. The RP2D was defined at the same dose level in the chemo-naive expansion cohort based on the myelosuppression observed beyond cycle 1. Myelosuppression, fatigue and biochemical liver enzyme changes were the most commonly observed AEs in this study, consistent with previously reported toxicities of these drugs. Haematological toxicities and fatigue, which have been observed with both eribulin and gemcitabine in single agent studies, may have been more prominent due to overlapping toxicity. Indeed, eribulin inhibits cancer cell growth via induction of irreversible complete mitotic block at G2–M (prometaphase blockage), disruption of mitotic spindles formation and initiation of apoptosis following prolonged mitotic blockage (Kuznetsov et al, 2004). Gemcitabine is an antimetabolite (incorporation of pyrimidine analogues into DNA) that primarily kills cells undergoing DNA synthesis (S phase) and blocks the progression of cells through the G1/S phase boundary (Bookman, 2005). The synergistic action on the cell cycle may explain the rate of haematological toxicities observed. Diarrhoea was infrequent and manageable with loperamide, although it was a defined DLT at DL 4 (grade 3 in one patient). The peripheral neuropathy appears to be lower with eribulin than other microtubule inhibitor agents (Shablak, 2013). Preliminary signs of activity were observed even in pretreated patients. As eribulin inhibits cancer cell proliferation via cell cycle arrest at G2–M phase (Towle et al, 2001; Jordan et al, 2005; Kuznetsov et al, 2009) and gemcitabine blocks the progression of cells through the G1/S phase (Plunkett et al, 1995; Mini et al, 2006), the drug combination may increase apoptosis by targeting two different checkpoints of the cell cycle, as demonstrated in preclinical models (Towle et al, 2003). Given the limited simple size and the dose-escalation nature of this trial, it is difficult to draw conclusions regarding the activity of this drug combination in patients. The lower incidence and grade of neuropathy with this combination and initial signal of activity may make this combination of interest in ovarian cancer given the efficacy of microtubule inhibitors in this disease such as paclitaxel but for which peripheral neuropathy is the main DLT (Gornstein and Schwarz, 2014); however, a dedicated phase II trial is needed to assess activity.
Eribulin is the only ‘classical’ cytotoxic agent approved for the treatment of breast cancer in the last 7 years over the new era of molecularly targeted agents. Eribulin was responsible for prolonging overall survival (OS) of heavily pretreated metastatic breast cancer patients in a large Phase III trial (Cortes et al, 2011) and is now under clinical development in earlier settings such as neoadjuvant and adjuvant settings. Furthermore, its unique mechanism of action and the absence of cross-resistance with taxanes have led to the design of clinical trials in multiple indications including: bladder, lung and prostate cancers (Polastro et al, 2014; Swami et al, 2015). On the basis of the promising results from the phase II (Schöffski et al, 2011), a randomised, open-label, multicenter phase III trial of eribulin mesylate in patients with locally advanced or recurrent and/or metastatic adipocytic sarcoma or leiomyosarcoma was conducted (NCT01327885). This trial enroled 452 patients who had disease progression following two standard therapies, which must have included an anthracycline and at least one additional regimen after anthracycline failure. Eribulin was given on day 1 and 8 of a 21-day cycle vs dacarbazine given on day 1, every 21 days. The primary endpoint of the study was to compare OS between treatment arms. Recent data showed that the primary endpoint in this trial was met, demonstrating a statistically significant improvement in OS in patients treated with eribulin vs Dacarbazine (Schöffski et al, 2015).
On the basis of scientific rationale, the combination of eribulin and gemcitabine is under investigation in several different ongoing clinical trials. For example, based on the RP2D defined in our phase I trial, a randomised phase II trial is open to accrual comparing eribulin and gemcitabine chemotherapy with paclitaxel and gemcitabine chemotherapy for patients with HER-2-negative metastatic breast cancer as first-line chemotherapy (NCT02263495). The combination of gemcitabine and eribulin is also under investigation in a phase II trial for patients with bladder cancer that is advanced or cannot be removed by surgery (NCT02178241).
Further development of eribulin is assessed in combination with other agents. A phase I trial showed that on the 21-day cycle, eribulin mesylate 1.2 mg m−2, administered on days 1 and 8, in combination with cisplatin 75 mg m−2, administered on day 1 is well tolerated and showed preliminary anticancer activity (Koczywas et al, 2014). Eribulin combined with standard gemcitabine/cisplatin chemotherapy was also shown to be feasible with encouraging clinical activity for locally advanced or metastatic bladder cancer with haematologic toxicity remaining the main limiting factor (Vogelzang et al, 2012). The RP2D of eribulin in combination with standard doses of gemcitabine (1000 mg m−2, days 1 and 8 every 21 days) and cisplatin (70 mg m−2, day 1) was also established at 1.0 mg m−2 on the same schedule at day 1 and 8 every 21 days. These findings corroborate our findings and the RP2D.
Conclusion
The RP2D of eribulin and gemcitabine combination is 1.0 mg m−2 of eribulin and 1000 mg m−2 of gemcitabine at day 1 and 8 every 21 days. Clinical benefits were reported with manageable toxicity.
Change history
01 December 2015
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Aapro MS, Martin C, Hatty S (1998) Gemcitabine--a safety review. Anticancer Drugs 9 (3): 191–201.
Abratt RP, Bezwoda WR, Falkson G, Goedhals L, Hacking D, Rugg TA (1944) Efficacy and safety profile of gemcitabine in non-small-cell lung cancer: a phase II study. J Clin Oncol 12 (8): 1535–1540.
Bookman MA (2005) Gemcitabine monotherapy in recurrent ovarian cancer: from the bench to the clinic. Int J Gynecol Cancer 15 (Suppl 1): 12–17.
Carmichael J, Fink U, Russell RC, Spittle MF, Harris AL, Spiessi G, Blatter J (1996) Phase II study of gemcitabine in patients with advanced pancreatic cancer. Br J Cancer 73 (1): 101–105.
Cortes J, O'Shaughnessy J, Loesch D, Blum JL, Vahdat LT, Petrakova K, Chollet P, Manikas A, Diéras V, Delozier T, Vladimirov V, Cardoso F, Koh H, Bougnoux P, Dutcus CE, Seegobin S, Mir D, Meneses N, Wanders J, Twelves C EMBRACE (Eisai Metastatic Breast Cancer Study Assessing Physician's Choice Versus E7389) investigators (2011) Eribulin monotherapy versus treatment of physician's choice in patients with metastatic breast cancer (EMBRACE): a phase 3 open-label randomised study. Lancet 377 (9769): 914–923.
Dabydeen DA, Burnett JC, Bai R, Verdier-Pinard P, Hickford SJ, Pettit GR, Blunt JW, Munro MH, Gussio R, Hamel E (2006) Comparison of the activities of the truncated halichondrin B analog NSC 707389 (E7389) with those of the parent compound and a proposed binding site on tubulin. Mol Pharmacol 70 (6): 1866–1875.
Gatzemeier U, Groth G, Butts C, Van Zandwijk N, Shepherd F, Ardizzoni A, Barton C, Ghahramani P, Hirsh V (2004) Randomized phase II trial of gemcitabine-cisplatin with or without trastuzumab in HER2-positive non-small-cell lung cancer. Ann Oncol 15 (1): 19–27.
Gornstein E, Schwarz TL (2014) The paradox of paclitaxel neurotoxicity: Mechanisms and unanswered questions. Neuropharmacology 76 (Pt A): 175–183.
Jordan MA, Kamath K, Manna T, Okouneva T, Miller HP, Davis C, Littlefield BA, Wilson L (2005) The primary antimitotic mechanism of action of the synthetic halichondrin E7389 is suppression of microtubule growth. Mol Cancer Ther 4 (7): 1086–1095.
Koczywas M, Frankel PH, Synold TW, Lenz HJ, Mortimer JE, El-Khoueiry AB, Gandara DR, Cristea MC, Chung VM, Lim D, Reckamp KL, Lau DH, Doyle LA, Ruel C, Carroll MI, Newman EM (2014) Phase I study of the halichondrin B analogue eribulin mesylate in combination with cisplatin in advanced solid tumors. Br J Cancer 111 (12): 2268–2274.
Kuznetsov G, Towle MJ, Cheng H, Kawamura T, TenDyke K, Liu D, Kishi Y, Yu MJ, Littlefield BA (2004) Induction of morphological and biochemical apoptosis following prolonged mitotic blockage by halichondrin B macrocyclic ketone analog E7389. Cancer Res 64 (16): 5760–5766.
Kuznetsov G, Xu Q, Rudolph-Owen L, Tendyke K, Liu J, Towle M, Zhao N, Marsh J, Agoulnik S, Twine N, Parent L, Chen Z, Shie JL, Jiang Y, Zhang H, Du H, Boivin R, Wang Y, Romo D, Littlefield BA (2009) Potent in vitro and in vivo anticancer activities of des-methyl, des-amino pateamine A, a synthetic analogue of marine natural product pateamine A. Mol Cancer Ther 8 (5): 1250–1260.
Lorusso V, Crucitta E, Silvestris N, Catino A, Caporusso L, Mazzei A, Guida M, Latorre A, Sambiasi D, D'Amico C, Schittulli F, Calabrese P, De Lena M (2003) Phase I/II study of gemcitabine plus mitoxantrone as salvage chemotherapy in metastatic breast cancer. Br J Cancer 88 (4): 491–495.
Mattiucci GC, Ippolito E, D'Agostino GR, Alfieri S, Antinori A, Crucitti A, Balducci M, Deodato F, Luzi S, Macchia G, Smaniotto D, Morganti AG, Valentini V (2013) Long-term analysis of gemcitabine-based chemoradiation after surgical resection for pancreatic adenocarcinoma. Ann Surg Oncol 20 (2): 423–429.
Mini E, Nobili S, Caciagli B, Landini I, Mazzei T (2006) Cellular pharmacology of gemcitabine. Ann Oncol 17 (Suppl 5): v7–12.
Okouneva T, Azarenko O, Wilson L, Littlefield BA, Jordan MA (2008) Inhibition of centromere dynamics by eribulin (E7389) during mitotic metaphase. Mol Cancer Ther 7 (7): 2003–2011.
Plunkett W, Huang P, Xu YZ, Heinemann V, Grunewald R, Gandhi V (1995) Gemcitabine: metabolism, mechanisms of action, and self-potentiation. Semin Oncol 22 (4 Suppl 11): 3–10.
Polastro L, Aftimos PG, Awada A (2014) Eribulin Mesylate in the management of metastatic breast cancer and other solid cancers: a drug review. Expert Rev Anticancer Ther 14 (6): 649–665.
Schöffski P, Maki RG, Italiano A, Gelderblom H, Grignani G, Pires De Camargo V, Bauer S, Young Rha S, Chawla SP, Blay JY, Hohenberger P, D'Adamo DR, Wang B, Chmielowski B, Le Cesne A, Demetri GD, Patel S (2015) Randomized, open-label, multicenter, phase III study of eribulin versus dacarbazine in patients (pts) with leiomyosarcoma (LMS) and adipocytic sarcoma (ADI). J Clin Oncol 33 (Suppl): Abstr LBA10502.
Schöffski P, Ray-Coquard IL, Cioffi A, Bui NB, Bauer S, Hartmann JT, Krarup-Hansen A, Grünwald V, Sciot R, Dumez H, Blay JY, Le Cesne A, Wanders J, Hayward C, Marreaud S, Ouali M, Hohenberger P European Organisation for Research and Treatment of Cancer (EORTC) Soft Tissue and Bone Sarcoma Group (STBSG) (2011) Activity of eribulin mesylate in patients with soft-tissue sarcoma: a phase 2 study in four independent histological subtypes. Lancet Oncol 12 (11): 1045–1052.
Shablak A (2013) Eribulin for advanced breast cancer: a drug evaluation. J Breast Cancer 16 (1): 12–15.
Swami U, Chaudhary I, Ghalib MH, Goel S (2012) Eribulin -a review of preclinical and clinical studies. Crit Rev Oncol Hematol 81 (2): 163–184.
Swami U, Shah U, Goel S (2015) Eribulin in cancer treatment. Mar Drugs 13 (8): 5016–5058.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92 (3): 205–216.
Towle MJ, Agoulnik S, Kuznetsov G, TenDyke K, Reardon C, Cheng H, Zheng W, Seletsky BM, Palme MH, Kishi Y, Lewis MD, Yu MJ, Littlefield BA (2003) In vivo efficacy of E7389, a synthetic analogue of the marine sponge antitubulin agent halichondrin B, against human tumor xenografts under monotherapy and combination therapy conditions. Proc Am Assoc Cancer Res (AACR) 44 (2nd ed.) Abstract 2749.
Towle MJ, Salvato KA, Budrow J, Wels BF, Kuznetsov G, Aalfs KK, Welsh S, Zheng W, Seletsky BM, Palme MH, Habgood GJ, Singer LA, Dipietro LV, Wang Y, Chen JJ, Quincy DA, Davis A, Yoshimatsu K, Kishi Y, Yu MJ, Littlefield BA (2001) In vitro and in vivo anticancer activities of synthetic macrocyclic ketone analogues of halichondrin B. Cancer Res 61 (3): 1013–1021.
Vogelzang N, Conkling P, Duran I, Maroto J, Modiano M, De Leonardis P, Hodge JP, Lieberman R (2012) Phase Ib/II study of eribulin mesylate administered in combination with gemcitabine/cisplatin as first-line therapy for locally advanced or metastatic bladder cancer: Phase Ib results. J Clin Oncol 30 (suppl 5): Abstract 273.
Von der Maase H, Hansen SW, Roberts JT, Dogliotti L, Oliver T, Moore MJ, Bodrogi I, Albers P, Knuth A, Lippert CM, Kerbrat P, Sanchez Rovira P, Wersall P, Cleall SP, Roychowdhury DF, Tomlin I, Visseren-Grul CM, Conte PF (2000) Gemcitabine and cisplatin versus methotrexate, vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: results of a large, randomized, multinational, multicenter, phase III study. J Clin Oncol 18 (17): 3068–3077.
Acknowledgements
We acknowledge the NCI US grant; Contract # HHSN261201100032C.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Lheureux, S., Oza, A., Laurie, S. et al. A phase I combination dose-escalation study of eribulin mesylate and gemcitabine in patients with advanced solid tumours: a study of the Princess Margaret Consortium. Br J Cancer 113, 1534–1540 (2015). https://doi.org/10.1038/bjc.2015.343
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2015.343
- Springer Nature Limited