Abstract
Nonsynonymous TP53 exon 4 single-nucleotide polymorphism (SNP), R72P, is linked to cancer and mutagen susceptibility. R72P associations with specific cancer risk, particularly hematological malignancies, have been conflicting. Myelodysplastic syndrome (MDS) with chromosome 5q deletion is characterized by erythroid hypoplasia arising from lineage-specific p53 accumulation resulting from ribosomal insufficiency. We hypothesized that apoptotically diminished R72P C-allele may influence predisposition to del(5q) MDS. Bone marrow and blood DNA was sequenced from 705 MDS cases (333 del(5q), 372 non-del(5q)) and 157 controls. Genotype distribution did not significantly differ between del(5q) cases (12.6% CC, 38.1% CG, 49.2% GG), non-del(5q) cases (9.7% CC, 44.6% CG, 45.7% GG) and controls (7.6% CC, 37.6% CG, 54.8% GG) (P=0.13). Allele frequency did not differ between non-del(5q) and del(5q) cases (P=0.91) but trended towards increased C-allele frequency comparing non-del(5q) (P=0.08) and del(5q) (P=0.10) cases with controls. Median lenalidomide response duration increased proportionate to C-allele dosage in del(5q) patients (2.2 (CC), 1.3 (CG) and 0.89 years (GG)). Furthermore, C-allele homozygosity in del(5q) was associated with prolonged overall and progression-free survival and non-terminal interstitial deletions that excluded 5q34, whereas G-allele homozygozity was associated with inferior outcome and terminal deletions involving 5q34 (P=0.05). These findings comprise the largest MDS R72P SNP analysis.
Similar content being viewed by others
Introduction
Risk for development of myelodysplastic syndromes (MDS) is senescence dependent and modified by lifetime exposure to potential leukemogens or other modifiers. The most common chromosome abnormality in de novo or therapy-related MDS is an interstitial deletion involving the long arm of chromosome 5 (del(5q)). Patients with isolated del(5q) MDS present with clinically and pathologically distinct features that include severe hypoplastic anemia, megakaryocyte dysplasia, low risk for leukemia transformation and a high rate of response to lenalidomide.1, 2 Although haploinsufficiency of several genes in the commonly deleted region contribute to the disease phenotype, allelic deletion of the ribosomal processing gene RPS14, a component of the 40S ribosomal subunit, is a key determinant of ineffective erythropoiesis. Nucleolar stress arising from disruption of ribosome assembly triggers p53 activation, a key effector of erythroid hypoplasia in both del(5q) MDS and congenital ribosomopathies. A murine model of the human 5q− syndrome generated by allelic deletion of the syntenic genes within the commonly deleted region showed that p53 inactivation is alone sufficient to rescue the hematologic phenotype, indicating that the hypoplastic anemia of the 5q− syndrome is p53-dependent.3, 4, 5, 6, 7, 8 Furthermore, we recently reported that acquired resistance to lenalidomide is associated with restoration of p53 expression.9, 10
P53 is a key regulator of stem cell homeostasis that impacts an array of cellular functions including genomic surveillance, cell-cycle regulation and apoptotic and inflammatory response. TP53 mutations are well described in human malignancies with up to 50% of all cancers harboring a mutation in the DNA-binding domain or in one of its regulators affecting p53 function.11, 12 In MDS, TP53 gene mutations are found almost exclusively in patients with chromosome 5q deletion or a complex karyotype, and have been associated with lower probability of response to lenalidomide.13, 14, 15 Genome-wide association studies have shown linkage between single-nucleotide polymorphisms (SNPs) that alter p53 function and select malignancies. One of the most well-studied nonsynonymous SNPs, rs1042522 (R72P), located within codon 72 has been implicated in susceptibility and predisposition to solid tumors. The R72P TP53 SNP in exon 4 lies proximal to the DNA-binding domain and adjacent to the proline-rich, proapoptotic domain of the protein.12, 16, 17 Substitution of a cytosine (C allele) for the more common guanine (G allele) results in translation of a proline (P) rather than arginine (R) residue at position 72. The amino-acid variants affect the tertiary structure of the putative p53 Src homology 3-binding domain resulting in discernible functional differences. The R/R homozygous genotype has greater apoptosis-promoting potential than the P/P genotype, arising in part from intrinsically greater mitochondrial localization triggering cytosolic release of cytochrome c.16, 18 The homozygous P/P genotype displays greater transcriptional efficiency, inducing a higher level of G1 arrest than the R/R genotype in a tissue- and context-specific manner.16, 19, 20, 21, 22, 23
Previous studies of the R72P variants in hematologic malignancies have shown conflicting results. Patients with chronic lymphocytic leukemia harboring a homozygous C allele displayed inferior clinical outcome irrespective of immunoglobulin heavy-chain variable (IGHV) gene mutation status,24 whereas no similar relationship was observed in patients with acute myeloid leukemia (AML).25 In chronic myelogenous leukemia, however, C-allele homozygozity was associated with decreased overall survival (OS) and progression-free survival (PFS).26 A meta-analysis of TP53 R72P association with hematologic malignancy risk validated an association of R72P with lymphoma risk, but not leukemia. Previous reports of R72P in MDS involved only small patient cohorts and did not examine the relationship to chromosome 5q deletion.27 Given the pathogenetic importance of p53 in del(5q) MDS, we investigated the distribution of this SNP in patients with MDS vs controls, and explored the relationship to TP53 mutations, chromosome 5q deletion, disease features and outcome.
Materials and methods
Study population, tissue specimens and DNA isolation
Peripheral blood and/or bone marrow were collected from patients (n=705, 372 non-del(5q) and 333 del(5q)) and healthy controls (n=157) who provided written consent according to Institutional Review Board (IRB)-approved protocols. Controls were not biologically related to cases and were either Florida blood bank donors or recruited on Moffitt Cancer Center clinical trials with IRB consent. All controls were healthy individuals. MDS cases were collected from hospitals in the United States (Moffitt Cancer Center (DER and AFL), Cleveland Clinic (JPM) and Arizona Cancer Center (AFL)), Canada (British Columbia Cancer Center (AK)), Spain (Hospital de Mar, ICO-Hospital Germans Trias I Pujol, Hospital Universitario La Fe and Hospital Clinico Universitario Santiago de Compostela (FS)), Germany (MLL Munich Leukemia Laboratory (TH)) and London (King’s College Hospital (GM)). DNA was isolated using Qiagen (Valencia, CA, USA) DNA isolation kits according to the manufacturer’s instructions. Median follow-up for all patients was 34.7 months for OS and 43.2 months for PFS.
PCR and TP53 genotyping
DNA was amplified using GoTaq Green (Promega Cooperation, Madison, WI, USA) according to the manufacturer’s protocol. Up to 100ng of DNA was used to amplify TP53 exon 4 using primers F-5′-CCTGGTCCTCTGACTGCTCTTTTCACCCA-3′ and R-5′-GGCCAGGCATTGAAGTCTCAT-3′ under the following conditions: 94°C for 2 min, 35 cycles of 94 °C for 30 s, 58 °C for 30 s and then 72 °C for 30 s, followed by a final 5 min extension at 72 °C, and held at 4 °C. PCR products were resolved on a 2% agarose gel, and the exon 4 356 bp fragment was excised and purified using Wizard SV Gel and PCR Cleanup Kit (Promega Cooperation). The purified DNA was sequenced by the Sanger method using BigDye Terminator v.3.1 Cycle Sequencing Kit (Applied Biosystems, Carlsbad, CA, USA) and a 3130xl Genetic Analyzer (Applied Biosystems). Genotypes were identified by sequencing in both forward and reverse directions. German samples were sequenced by next-generation deep sequencing of the exons 4–11 of the TP53 gene using the 454 GS FLX amplicon chemistry (Roche Applied Science, Indianapolis, IN, USA) as described previously.28 For London samples, 14 amplicons across the entire TP53 coding region, including untranslated exon 1, were sequenced using the Roche GS FLX sequencing platform (Roche, Indianapolis, IN, USA) as described previously.29
Variable description
Clinical data on all patients was collected through March 2011, and disease-specific features analyzed were limited to the date of diagnosis. Genotype frequency did not differ across races among del(5q) MDS cases (P=0.54) or controls (P=1.0); however, there was a significant difference in R72P genotype between Caucasian and non-Caucasian among non-del(5q) MDS informative cases, or in those of which these data were available (P=0.05). As the proportion of non-Caucasian patients within each subgroup was <10% (3.6% for del(5q), 10% for non-del(5q) and 3.6% for controls), and we found no significant difference in R72P genotype by race (P=0.21) in the total population, all analyses included all patients and controls regardless of race. Cytogenetic risk was defined according to the following criteria: low/good: normal, −Y and isolated 5q or 20q deletion as single anomaly; intermediate (Int): 5q deletion plus one, or one abnormality; and high/poor: any chromosome 7 abnormality or 2+ abnormalities. R72P genotype among World Health Organization (WHO) subtypes was assessed by comparing genotype distribution across the following categories: isolated del(5q), refractory anemia with excess blasts-1 (RAEB-1), RAEB-2, RAEB-transformed (RAEB-T) and ‘other’, which included refractory anemia (RA), RA with ring sideroblasts (RARS), refractory cytopenia with multilineage dysplasia (RCMD) and RCMD with ring sideroblasts; MDS/myeloproliferative neoplasm (MPN), AML and the non-proliferative MDS/MPN chronic myelomonocytic leukemia (CMML).
Statistical analysis
Participants’ demographic features, R72P genotype and allele frequency among controls and MDS (non-del(5q) and del(5q)) cases were compared using the analysis of variance test for continuous variables and the χ2 test using the exact method with Monte Carlo estimation for categorical variables. The association between R72P genotype and disease features was evaluated using the Fisher’s exact test. OS was defined as the interval from the date of diagnosis until the date of death from any cause or until the last date of follow-up. PFS was defined as the time from diagnosis to development of AML or to date of death due to any cause, whichever came first. The OS, PFS and lenalidomide transfusion independence response duration were estimated using the time-to-event approach. For the lenalidomide transfusion independence response duration, the data were truncated at 4 years because only five patients had a response beyond 4 years. The Kaplan–Meier curves by genotype were generated and compared using the log-rank test. The genotype frequencies between del(5q) MDS patients with deletions resolved by metaphase cytogenetics were analyzed using the χ2 test using the exact method with Monte Carlo estimation. All P-values ⩽0.05 were considered statistically significant. All analyses were conducted using SAS (Version 9.2; SAS Institute Inc., Cary, NC, USA).
Results
Subject characteristics
A total of 705 MDS cases were analyzed (372 non-del(5q) and 333 del(5q)), as well as 157 healthy controls. The mean age in controls was 53.3 years and ranged from 18 to 89 years (Table 1). Among informative non-del(5q) MDS, the mean age was 68.5 years with a range of 16–94 years, and for del(5q) patients mean age was 68.7 years and ranged from 23 to 93 years. The percentage of females in each population was 52.8%, 32.2% and 66.5% in controls, non-del(5q) and del(5q) MDS, respectively, as isolated 5q− is more frequent in females; however, there were no genotype differences by sex. WHO MDS subtype was available for 348 non-del(5q) cases, which included 50 (14.4%) refractory anemia with excess blasts-1 (RAEB-1), 32 (9.2%) RAEB-2, 4 (1.1%) AML, 10 (2.9%) non-proliferative MDS/MPN category of CMML, 4 (1.1%) MDS/MPN-unclassified and 248 (71.3) ‘others’, which included the non-blastic, morphologic subtypes of refractory anemia (RA), RARS, RCMD and RCMD with ring sideroblasts. Within the del(5q) cohort, WHO subtype was available for 309 cases, which included 179 (57.9%) patients with isolated del(5q) MDS, 28 (9.1%) with RAEB-1, 17 (5.5%) with RAEB-2, 5 (1.6%) with RAEB-T, 15 (4.9%) with AML, 2 (0.6%) with CMML and 63 (20.4%) with ‘other’ diagnoses (Table 1). Of the 321 non-del(5q) cases with International Prognostic Scoring System (IPSS) data, 254 (79.1%) were grouped as lower risk, which included both low-risk and intermediate-1 IPSS values, whereas 67 (20.9%) were grouped as higher risk, which included intermediate-2 and high-risk patients. Of the 164 del(5q) cases informative for IPSS, 72% were lower-risk and 28% were higher-risk patients by IPSS. Distribution of low, intermediate and high cytogenetic risk among 357 non-del(5q) patients was 265 (74.2%), 52 (14.6%) and 40 (11.2%), respectively, and 213 (68.9%), 21 (6.8%) and 75 (24.3%), respectively, among 309 del(5q) cases.
R72P genotype and disease status
To assess potential differences in allele distribution and frequency, we first compared SNP genotype among controls and cases of non-del(5q) and del(5q) MDS and found no significant differences in R72P genotype (P=0.13), including no significant difference between the del(5q) vs non-del(5q) cases (P=0.17). The frequency of CC, CG and GG among controls, non-del(5q) and del(5q) samples were 7.6%, 37.6% and 54.8%; 9.7%, 44.6% and 45.7%; and 12.6%, 38.1% and 49.2%, respectively (Table 1). There was no significant difference in allele frequency in del(5q) MDS vs non-del(5q) MDS cases (P=0.91); however, differences between non-del(5q) allele frequency and controls approached significance (P=0.08), as well as del(5q) cases, compared with controls (P=0.10). C-allele frequency for controls, non-del(5q) MDS and del(5q) MDS was 26.4%, 32.0% and 31.7%, respectively (Table 1). These findings suggest that there may be greater C-allele frequency among MDS cases compared with controls.
R72P genotype and clinical characteristics
We next investigated whether R72P genotype was associated with differences in disease features in del(5q) or non-del(5q) MDS cases (Table 2). There was no correlation between IPSS category and R72P in non-del(5q) patients (P=0.42) with corresponding frequencies for CC, CG and GG of 9.4%, 46.1% and 44.5% for lower-risk and 11.9%, 37.3% and 50.7% for higher-risk MDS, respectively. In del(5q) MDS, the frequencies of CC, CG and GG were 16.9%, 48.3% and 34.7% for lower-risk and 13%, 34.8% and 52.2% for higher-risk IPSS patients, respectively, with no correlation between IPSS and genotype (P=0.12) (Table 2). There was a difference in R72P genotype distribution by WHO classification in non-del(5q) MDS cases with an increasing frequency of the CC genotype corresponding to increased bone marrow blast percentage (P=0.04); however, this represents only a small proportion of patients in our study. There was no relationship between WHO classification and R72P genotype in del(5q) MDS (P=0.37). We next examined the relationship between R72P genotype and age of disease onset among MDS cases. We found no significant difference in age at diagnosis according to R72P genotype among patients with either non-del(5q) (mean±s.d. was 65.3±11.2, 65.4±12.9 and 62.5±13.5, for CC, CG and GG, respectively) or del(5q) MDS (66.6±10.5, 64.1±13.8 and 65.9±11.6, for CC, CG and GG, respectively) (P=0.08 and P=0.69, respectively). Age at diagnosis did decrease with G-allele homozygozity in non-del(5q) MDS and approached significance when comparing the age at diagnosis in patients harboring the GG genotype between non-del(5q) and del(5q) MDS patients (P=0.07).
R72P genotype and disease natural history
To investigate possible differences in outcome by R72P genotype, we assessed OS and PFS. There was no significant difference in OS by genotype among all MDS cases (log-rank test, P=0.64), where 5-year OS was 0.46, 0.56 and 0.49 for CC, CG and GG, respectively (Figure 1). Among non-del(5q) cases, median survival by genotype was 4.5 years for CC, 10.2 years for CG and 5.3 years for GG (P=0.39). However, 1-year survival increased in a G-allele dosage manner with survival estimates of 0.83, 0.96 and 0.98 for CC, CG and GG. Among del(5q) MDS patients, the median OS was 4.9 years for CC, 5.1 years for CG and 4.0 years for GG (P=0.52) with >1-year survival associated with the C-allele (0.82, 0.77 and 0.73 for CC, CG and GG, respectively). Although there was no significant differences in PFS in del(5q) MDS by R72P genotype (P=0.53) or non-del(5q) MDS (P=0.61), the CC genotype showed a trend of overall improved PFS than G-allele-containing genotypes in del(5q) MDS, whereas G-allele-containing genotypes were associated with improved PFS and OS in non-del(5q) MDS (Figure 2). When comparing the interaction of the R72P genotype with other prognostic variables (i.e., age at diagnosis, cytogenetics, blast percentage and gender) by multivariate analysis, only IPSS retained prognostic significance for OS and PFS.
R72P genotype and lenalidomide response duration
We previously reported that lenalidomide modifies p53 stability, which facilitates G1 escape and transition to G2 arrest in del(5q) progenitors.30, 31 To determine if TP53 R72P SNP genotype influences lenalidomide response or duration, we explored the relationship between R72P genotype and duration of erythroid response to lenalidomide treatment in del(5q) patients. Erythroid response was defined using the previously described criteria.1, 2, 32 Although we found no significant difference in response rates by genotype (P=0.75) (73.5% overall response rate, 71.4% for CC, 77.5% for CG and 69.0% for GG), comparison of response duration by genotype showed a trend for increased duration of transfusion independence with C-allele dosage; however, this did not reach statistical significance (P=0.51) (Figure 3). Median response durations according to genotype were 2.2, 1.3 and 0.89 years for CC, CG and GG genotypes, respectively. Interestingly, the 2-year estimate for lenalidomide response duration was more than doubled for CC (0.50) compared with both CG (0.21) and GG (0.13) (P=0.09).
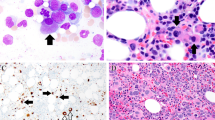
Chromosome 5q deletion size, TP53 mutation and R72P genotype
Size of the deletion on chromosome 5q varies from microdeletions to large terminal deletions. The larger, more terminal lesions, particularly those including or extending telomeric to 5q34, have been linked to higher-risk MDS and AML, and unfavorable prognosis. To ascertain the relationship between R72P genotype and extended terminal chromosome deletions, we investigated genotype distribution by deletion inclusion of chromosome 5q34 deletion (Figure 4a). Using a cohort of 190 del(5q) patient specimens, chromosome 5 deletion location was assessed by diagnostic metaphase cytogenetics. We found that the GG genotype was significantly associated with those patients harboring a deletion involving 5q34 (P=0.05) compared with those patients with a C-allele-containing genotype. The frequency of a 5q34 deletion in either CC or CG samples was 50%; however, this increased to 71% for those with a GG genotype. Jerez et al.33 recently reported an association between larger chromosome 5 deletions and TP53 mutations;33 therefore, we next examined the relationship between R72P genotype and TP53 DNA-binding domain mutation. Among the 211 del(5q) cases with TP53 mutation analysis, 30.3% contained a DNA-binding domain mutation; however, there was no association with R72P genotype (CC, 45.5, CG, 23.9 and GG, 31.4%). Among those patients harboring the 5q34 deletion, we found no association with TP53 mutation (P=0.33) (Figure 4b). Lastly, we found no association between GG genotype and TP53 mutation in the del(5q) cases (P=0.38) (Figure 4c). There was no association with TP53 mutation and any R72P genotype in either del(5q) MDS (P=0.15) or non-del(5q) MDS (P=1.0).
Discussion
Gene deletion studies indicate that the p53 polyproline domain is essential to mount an effective apoptotic response to stress and inhibit tumorigenesis.34,35,36,37 P53-P72 binds more weakly than p53-R72 to the positive regulatory protein PIN1, a prolyl isomerase,38 yet interacts more readily with the inhibitory protein iASPP (inhibitor of ASPP).39 We found no differences in age of MDS onset by R72P genotype; however, germline gene mutations implicated in the development of familial MDS, such as the Runt-related transcription factor-1 (RUNX1), similarly show no consistent association with earlier onset of disease, suggesting that secondary events necessary for MDS development are age-dependent.40, 41, 42
A significant finding in this study was the association of the G-allele and GG homozygous genotype with more terminal 5q34 deletions (P=0.05). Previous studies reported that patients with larger terminal deletions have a less favorable prognosis and higher frequency of TP53 mutation.33 Although we did not discern a relationship to gene mutation status, the overall frequency of TP53 gene mutation was relatively low. Nonetheless, the precise mechanisms driving the differences in deletion loci by R72P genotype remain unclear. The P72 (CC) variant is reported to be more efficient in inducing cell-cycle arrest and DNA repair than the R72 variant, which may account for the longer OS and PFS in del(5q) patients harboring the C-allele or CC genotype.23, 43 By contrast, in patients with non-del(5q) MDS, we found that OS and PFS were reduced in those individuals harboring the CC genotype. We hypothesize that in non-del(5q) MDS in which the hematologic phenotype is not p53-dependent, the attenuated apoptotic activity of the C-allele/P72 variant may facilitate emergence and survival of clones with greater AML potential.
Although we were unable to discern significant differences in the duration of transfusion independence to lenalidomide according to genotype in del(5q) MDS patients, there was a trend favoring longer response duration in patients with a C allele that appears allele dosage dependent. As lenalidomide suppresses del(5q) MDS clones by inhibiting the dual specificity phosphatases CDC25C and PP2Acα encoded within or adjacent to the 5q31 commonly deleted region to arrest progenitors in G2/M, we questioned whether the diminished apoptotic capacity of the homozygous CC phenotype might foster transition from G0/G1 and sustained G2/M arrest to account for the more prolonged response duration. Furthermore, given that approximately half of lenalidomide-treated patients become resistant to treatment within 3 years, the lack of significant differences in 5-year response duration is not surprising.1
These data underscore the distribution of R72P in MDS and highlight differences between del(5q) and non-del(5q) subtypes by gene polymorphism and the relationship to lenalidomide response. The potential interaction of R72P variants with germline variants in other key regulators or effectors of the p53 pathway that may modify MDS risk and lenalidomide response merit further investigation in a larger cohort of patients.
References
List A, Dewald G, Bennett J, Giagounidis A, Raza A, Feldman E et al. Lenalidomide in the myelodysplastic syndrome with chromosome 5q deletion. N Engl J Med 2006; 355: 1456–1465.
List A, Kurtin S, Roe DJ, Buresh A, Mahadevan D, Fuchs D et al. Efficacy of lenalidomide in myelodysplastic syndromes. N Engl J Med 2005; 352: 549–557.
Barlow JL, Drynan LF, Hewett DR, Holmes LR, Lorenzo-Abalde S, Lane AL et al. A p53-dependent mechanism underlies macrocytic anemia in a mouse model of human 5q− syndrome. Nat Med 2010; 16: 59–66.
Deisenroth C, Zhang Y . Ribosome biogenesis surveillance: probing the ribosomal protein-Mdm2-p53 pathway. Oncogene 2010; 29: 4253–4260.
Ebert BL, Pretz J, Bosco J, Chang CY, Tamayo P, Galili N et al. Identification of RPS14 as a 5qFunding syndrome gene by RNA interference screen. Nature 2008; 451: 335–339.
Gotlib J . Ribosomes and beone marrow failure syndromes: convergence with p53. Hematologist 2010; 7: 12.
Dutt S, Narla A, Lin K, Mullally A, Abayasekara N, Megerdichian C et al. Haploinsufficiency for ribosomal protein genes causes selective activation of p53 in human erythroid progenitor cells. Blood 2011; 117: 2567–2576.
Starczynowski DT, Morin R, McPherson A, Lam J, Chari R, Wegrzyn J et al. Genome-wide identification of human microRNAs located in leukemia-associated genomic alterations. Blood 2011; 117: 595–607.
Wei S, Chen X, McGraw K, Zhang L, Komrokji R, Clark J et al. Lenalidomide promotes p53 degradation by inhibiting MDM2 auto-ubiquitination in myelodysplastic syndrome with chromosome 5q deletion. Oncogene 2012; 32: 1110–1120.
Caceres G, McGraw K, Yip BH, Pellagatti A, Johnson J, Zhang L et al. TP53 suppression promotes erythropoiesis in del(5q) MDS, suggesting a targeted therapeutic strategy in lenalidomide-resistant patients. Proc Natl Acad Sci USA 2013; 110: 16127–16132.
Soussi T, Wiman KG . Shaping genetic alterations in human cancer: the p53 mutation paradigm. Cancer Cell 2007; 12: 303–312.
Bode AM, Dong Z . Post-translational modification of p53 in tumorigenesis. Nat Rev Cancer 2004; 4: 793–805.
Kulasekararaj AG, Smith AE, Mian SA, Mohamedali AM, Krishnamurthy P, Lea NC et al. TP53 mutations in myelodysplastic syndrome are strongly correlated with aberrations of chromosome 5, and correlate with adverse prognosis. Br J Haematol 2013; 160: 660–672.
Mallo M, Del Rey M, Ibanez M, Calasanz MJ, Arenillas L, Larrayoz MJ et al. Response to lenalidomide in myelodysplastic syndromes with del(5q): influence of cytogenetics and mutations. Br J Haematol 2013; 162: 74–86.
Bally C, Ades L, Renneville A, Preudhomme C, Raynaud S, Cluzeau T et al. P-023 Incidence and prognostic value of TP53 mutations in IPSS low and INT 1 (lower risk) MDS with del 5q. Leuk Res 37: S32–S33.
Dumont P, Leu JI, Della Pietra AC 3rd, George DL, Murphy M . The codon 72 polymorphic variants of p53 have markedly different apoptotic potential. Nat Genet 2003; 33: 357–365.
Joerger AC, Fersht AR . The tumor suppressor p53: from structures to drug discovery. Cold Spring Harbor Perspect Biol 2010; 2: a000919.
Vietri MT, Riegler G, Ursillo A, Caserta L, Cioffi M, Molinari AM . P53 codon 72 polymorphism in patients affected with ulcerative colitis. J Gastroenterol 2007; 42: 456–460.
Frank AK, Leu JI, Zhou Y, Devarajan K, Nedelko T, Klein-Szanto A et al. The codon 72 polymorphism of p53 regulates interaction with NF-{kappa}B and transactivation of genes involved in immunity and inflammation. Mol Cell Biol 2011; 31: 1201–1213.
Zhu F, Dolle ME, Berton TR, Kuiper RV, Capps C, Espejo A et al. Mouse models for the p53 R72P polymorphism mimic human phenotypes. Cancer Res 2010; 70: 5851–5859.
Thomas M, Kalita A, Labrecque S, Pim D, Banks L, Matlashewski G . Two polymorphic variants of wild-type p53 differ biochemically and biologically. Mol Cell Biol 1999; 19: 1092–1100.
Sullivan A, Syed N, Gasco M, Bergamaschi D, Trigiante G, Attard M et al. Polymorphism in wild-type p53 modulates response to chemotherapy in vitro and in vivo. Oncogene 2004; 23: 3328–3337.
Pim D, Banks L . P53 polymorphic variants at codon 72 exert different effects on cell cycle progression. Int J Cancer 2004; 108: 196–199.
Majid A, Richards T, Dusanjh P, Kennedy DB, Miall F, Gesk S et al. TP53 codon 72 polymorphism in patients with chronic lymphocytic leukaemia: identification of a subgroup with mutated IGHV genes and poor clinical outcome. Br J Haematol 2011; 153: 533–535.
Nakano Y, Naoe T, Kiyoi H, Kunishima S, Minami S, Miyawaki S et al. Poor clinical significance of p53 gene polymorphism in acute myeloid leukemia. Leuk Res 2000; 24: 349–352.
Bergamaschi G, Merante S, Orlandi E, Galli A, Bernasconi P, Cazzola M . TP53 codon 72 polymorphism in patients with chronic myeloid leukemia. Haematologica 2004; 89: 868–869.
Machado-Neto JA, Traina F, De Melo Campos P, Andreoli-Risso MF, Costa FF, Olalla Saad ST . Lack of association between MDM2 SNP309 and TP53 Arg72Pro polymorphisms with clinical outcomes in myelodysplastic syndrome. Neoplasma 2012; 59: 530–535.
Grossmann V, Roller A, Klein HU, Weissmann S, Kern W, Haferlach C et al. Robustness of amplicon deep sequencing underlines its utility in clinical applications. J Mol Diagn 2013; 15: 473–484.
Jadersten M, Saft L, Smith A, Kulasekararaj A, Pomplun S, Gohring G et al. TP53 mutations in low-risk myelodysplastic syndromes with del(5q) predict disease progression. J Clin Oncol 2011; 29: 1971–1979.
List A, Rocha K, Zhang L, Komrokji R, Clark J, Caceres G et al. Secondary resistance to lenalidomide in Del(5q) MDS is associated with CDC25C & PP2A overexpression. Blood 2009; 114: 123.
Wei S, Chen X, Rocha K, Epling-Burnette PK, Djeu JY, Liu Q et al. A critical role for phosphatase haplodeficiency in the selective suppression of deletion 5q MDS by lenalidomide. Proc Natl Acad Sci USA 2009; 106: 12974–12979.
Komrokji RS, List AF . Role of lenalidomide in the treatment of myelodysplastic syndromes. Semin Oncol 2011; 38: 648–657.
Jerez A, Gondek LP, Jankowska AM, Makishima H, Przychodzen B, Tiu RV et al. Topography, clinical, and genomic correlates of 5q myeloid malignancies revisited. J Clin Oncol 2012; 30: 1343–1349.
Sakamuro D, Sabbatini P, White E, Prendergast GC . The polyproline region of p53 is required to activate apoptosis but not growth arrest. Oncogene 1997; 15: 887–898.
Walker KK, Levine AJ . Identification of a novel p53 functional domain that is necessary for efficient growth suppression. Proc Natl Acad Sci USA 1996; 93: 15335–15340.
Toledo F, Lee CJ, Krummel KA, Rodewald LW, Liu CW, Wahl GM . Mouse mutants reveal that putative protein interaction sites in the p53 proline-rich domain are dispensable for tumor suppression. Mol Cell Biol 2007; 27: 1425–1432.
Roth J, Koch P, Contente A, Dobbelstein M . Tumor-derived mutations within the DNA-binding domain of p53 that phenotypically resemble the deletion of the proline-rich domain. Oncogene 2000; 19: 1834–1842.
Mantovani F, Tocco F, Girardini J, Smith P, Gasco M, Lu X et al. The prolyl isomerase Pin1 orchestrates p53 acetylation and dissociation from the apoptosis inhibitor iASPP. Nat Struct Mol Biol 2007; 14: 912–920.
Bergamaschi D, Samuels Y, Sullivan A, Zvelebil M, Breyssens H, Bisso A et al. iASPP preferentially binds p53 proline-rich region and modulates apoptotic function of codon 72-polymorphic p53. Nat Genet 2006; 38: 1133–1141.
Chen CY, Lin LI, Tang JL, Ko BS, Tsay W, Chou WC et al. RUNX1 gene mutation in primary myelodysplastic syndrome—the mutation can be detected early at diagnosis or acquired during disease progression and is associated with poor outcome. Br J Haematol 2007; 139: 405–414.
Owen C, Barnett M, Fitzgibbon J . Familial myelodysplasia and acute myeloid leukaemia—a review. Br J Haematol 2008; 140: 123–132.
Liew E, Owen C . Familial myelodysplastic syndromes: a review of the literature. Haematologica 2011; 96: 1536–1542.
Siddique MM, Balram C, Fiszer-Maliszewska L, Aggarwal A, Tan A, Tan P et al. Evidence for selective expression of the p53 codon 72 polymorphs: implications in cancer development. Cancer Epidemiol Biomarkers Prev 2005; 14: 2245–2252.
Acknowledgements
This work was funded, in part, by the National Cancer Institute/National Institute of Health (5 R01 CA131076-04); by a grant from the Instituto de Salud Carlos III, Ministerio de Sanidad y Consumo, Spain (PI 11/02010); by the Red Temática de Investigación Cooperativa en Cáncer (RTICC, FEDER) (RD12/0036/0044 and RD12/0036/0014); 2014 SGR225 (GRE) Generalitat de Catalunya; economical support from Fundació Internacional Josep Carreras i de la Obra Social 'la Caixa'; from Celgene Spain; and generous support provided by Martin Schaffel.
Author Contributions
KLM designed and performed research, collected and analyzed data, and wrote the manuscript; LMZ performed research and collected data; DER, AJ, WF, YZ and HYL performed statistical analysis and analyzed and interpreted data; AAB, DLB, SEK, SY, KG, TJN, MJC, JC, ES, TG, AES, AK and SS collected data; LS, PE, MM, AK, FS, TH, GM and JPM collected, analyzed and interpreted data. AFL designed research, analyzed and interpreted data and wrote the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
AFL was a consultant for, and DB is employed by, Celgene Corporation. There are no other conflicts of interest to declare.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
McGraw, K., Zhang, L., Rollison, D. et al. The relationship of TP53 R72P polymorphism to disease outcome and TP53 mutation in myelodysplastic syndromes. Blood Cancer Journal 5, e291 (2015). https://doi.org/10.1038/bcj.2015.11
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bcj.2015.11
- Springer Nature Limited
This article is cited by
-
Association of TP53 gene polymorphisms with the risk of acute lymphoblastic leukemia in Moroccan children
Molecular Biology Reports (2022)
-
Presence of new mutations in the TP53 gene in patients with low-risk myelodysplastic syndrome: two case reports
Journal of Medical Case Reports (2017)