Abstract
Background
The aim of the present study was to observe the concomitant activation of nitric oxide (NO) and endothelium-derived hyperpolarizing factor (EDHF) pathways by TRPV4 channel agonist GSK1016790A in the rat pulmonary artery and explore the mechanism by which NO synthase inhibition attenuates EDHF-mediated relaxation in endothelium-intact rat pulmonary artery.
Methods
Tension experiments were conducted on the pulmonary artery from male Wistar rats.
Results
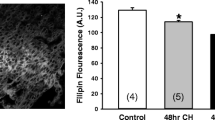
TRPV4 channel agonist GSK1016790A (GSK) caused concentration-dependent relaxation (Emax 86.9 ± 4.6%; pD2 8.7 ± 0.24) of the endothelium-intact rat pulmonary artery. Combined presence of apamin and TRAM-34 significantly attenuated the relaxation (Emax 61.1 ± 6.0%) to GSK. l-NAME (100 μM) significantly attenuated (8.2 ± 2.9%) the relaxation response to GSK that was resistant to apamin plus TRAM-34. However, presence of ICI192605 or furegrelate alongwith l-NAME revealed the GSK-mediated EDHF-response (Emax of 28.5 ± 5.2%; Emax 24.5 ± 4.3%) in this vessel, respectively. Further, these two TxA2 modulators (ICI/furegrelate) alongwith l-NAME had no effect on SNP-induced endothelium-independent relaxation in comparison to l-NAME alone. This EDHF-mediated relaxation was sensitive to inhibition by K+ channel blockers apamin and TRAM-34 or 60 mM K+ depolarizing solution. Further, combined presence of apamin and TRAM-34 in U46619 pre-contracted pulmonary arterial rings significantly reduced the maximal relaxation (Emax 71.6 ± 6.9%) elicited by GSK, but had no effect on the pD2 (8.1 ± 0.03) of the TRPV4 channel agonist in comparison to controls (Emax, 92.4 ± 4.3% and pD2, 8.3 ± 0.06).
Conclusion
The present study suggests that NO and EDHF are released concomitantly and NO synthase inhibition attenuates GSK-induced EDHF response through thromboxane pathway in the rat pulmonary artery.
Similar content being viewed by others
Abbreviations
- ACh:
-
acetylcholine
- ANOVA:
-
analysis of variance
- EDHF:
-
endothelium-derived hyperpolarizing factor
- GSK:
-
GSK1016790A
- ICI192605:
-
[4-(Z)-6-(2-0-chlrophenyl-4-Ohydroxyphenyl-1,3-dioxan-cis5-yl) hexenoic acid]
- IKCa (KCa 3.1):
-
intermediate conductance potassium channel
- l-NAME:
-
NG-nitro-l-arginine methyl ester
- MKHS:
-
modified Krebs-Henseleit solution
- NO:
-
nitric oxide
- NOS:
-
nitric oxide synthase
- PE:
-
phenylephrine
- PKG:
-
protein kinase G
- SKCa (KCa 2.3):
-
small conductance potassium channel
- SNP:
-
sodium nitroprusside
- TRAM-34:
-
1-[(2-chlorophenyl)diphenylmethyl]-1H-pyrazole
- TRPV4:
-
transient receptor potential vanilloid 4
- TP:
-
thromboxane/prostanoid receptor
References
Budhiraja R, Tuder RM, Hassoun PM. Endothelial dysfunction in pulmonary hypertension. Circulation 2004;109(2):159–65.
Edgaras S, Egidijus K, Enrikas V, Simonsen U. Role of nitric oxide and other endothelium-derived factors. Medicina 2003;39:333–41.
Chen G, Suzuki H, Weston AH. Acetylcholine releases endothelium-derived hyperpolarizing factor and EDRF from rat blood vessels. Br J Pharmacol 1988;95(4):1165–74.
Karamsetty MR, Nakashima JM, Ou LC, Klinger JR, Hill NS. EDHF contributes to strain-related differences in pulmonary arterial relaxation in rats. Am J Physiol Lung Cell Mol Physiol 2001;280(3):L458–64.
Subramani J, Marcus Leo MD, Kathirvel K, Arunadevi R, Singh TU, Prakash VR, et al. Essential role of nitric oxide in sepsis-induced impairment of endothelium-derived hyperpolarizing factor-mediated relaxation in rat pulmonary artery. Eur J Pharmacol 2010;630:84–91.
Sukumaran SV, Singh TU, Parida S, Reddy CEN, Thangamalai R, Kandasamy K, et al. TRPV4 channel activation leads to endothelium-dependent relaxation mediated by nitric oxide and endothelium-derived hyperpolarizing factor in rat pulmonary artery. Pharmacol Res 2013;78:18–27.
Zygmunt PM, Plane F, Paulsson M, Garland CJ, Högestätt ED. Interactions between endothelium-derived relaxing factors in the rat hepatic artery: focus on regulation of EDHF. Br J Pharmacol 1998;124:992–1000.
Feletou M, Vanhoutte PM. Endothelium-derived hyperpolarizing factor: where are we now. Arterioscler Thromb Vasc Biol 2006;26:1215–25.
McNeish AJ, Sandow SL, Neylon CB, Chen MX, Dora KA, Garland CJ. Evidence for involvement of both IKCa and SKCa channels in hyperpolarizing responses of the rat middle cerebral artery. Stroke 2006;37(5):1277–82.
Horibe M, Ogawa K, Sohn JT, Murray PA. Propofol attenuates acetylcholine-induced pulmonary vasorelaxation: role of nitric oxide and endothelium-derived hyperpolarizing factors. Anesthesiology 2000;93(2):447–55.
Tracey A, Bunton D, Irvine J, MacDonald A, Shaw AM. Relaxation to bradykinin in bovine pulmonary supernumerary arteries can be mediated by both a nitric oxide-dependent and -independent mechanism. Br J Pharmacol 2002;137(4):538–44.
Aschner JL, Smith TK, Kovacs N, Pinheiro JMB, Fuloria M. Mechanisms of bradykinin-mediated dilation in newborn piglet pulmonary conducting and resistance vessels. Am J Physiol Lung Cell Mol Physiol 2002;283:L373–82.
Kroigaard C, Dalsgaard T, Simonsen U. Mechanisms underlying epithelium-dependent relaxation in rat bronchioles: analogy to EDHF-type relaxation in rat pulmonary arteries. Am J Physiol Lung Cell Mol Physiol 2010;298(4):L531–42.
Bauersachs J, Popp R, Hecker M, Sauer E, Fleming I, Busse R. Nitric oxide attenuates the release of endothelium-derived hyperpolarizing factor. Circulation 1996;94:3341–7.
McNeish AJ, Garland CJ. Thromboxane A2 inhibition of SKCa after NO synthase block in rat middle cerebral artery. Br J Pharmacol 2007;151:441–9.
Crane GJ, Garland CJ. Thromboxane receptor stimulation associated with loss of SKCa activity and reduced EDHF responses in the rat isolated mesenteric artery. Br J Pharmacol 2004;142:43–50.
Wade ML, Fitzpatrick FA. Nitric oxide modulates the activity of the hemoproteins prostaglandin I2 synthase and thromboxane A2 synthase. Arch Biochem Biophys 1997;347:174–80.
Reid HM, Kinsella BT. The {alpha}, but not the ta, isoform of the human thromboxane A2 receptor is a target for nitric oxide-mediated desensitization: independent modulation of TP{alpha} signaling by nitric oxide and prostacyclin. J Biol Chem 2003;278:51190–202.
Kroigaard C, Dalsgaard T, Nielsen G, Laursen BE, Pilegaard H, Kohler R, et al. Activation of endothelial and epithelial KCa2.3 calcium-activated potassium channels by NS309 relaxes human small pulmonary arteries and bronchioles. Br J Pharmacol 2012;167:37–47.
Randriamboavonjy V, Kiss L, Falck JR, Busse R, Fleming I. The synthesis of 20-HETE in small porcine coronary arteries antagonizes EDHF-mediated relaxation. Cardiovas Res 2005;65:487–94.
Benyo Z, Gorlach C, Wahl M. Involvement of thromboxane A2 in the mediation of the contractile effect induced by inhibition of nitric oxide synthesis in isolated rat middle cerebral arteries. J Cereb Blood Flow Metab 1998;18: 616–618.
Lacza Z, Herman P, Gorlach C, Hortobagyi T, Sandor P, Wahl M, et al. NO synthase blockade induces chaotic cerebral vasomotion via activation of thromboxane receptors. Stroke 2001;32:2609–14.
Pankey EA, Zsombok A, Lasker GF, Kadowitz PJ. Analysis of responses to the TRPV4 agonist GSK1016790A in the pulmonary vascular bed of the intact-chest rat. Am J Physiol Heart Circ Physiol 2014;306:H33–40.
Busse R, Edwards G, Feletou M, Fleming I, Vanhoutte PM, Weston AH. EDHF: bringing the concepts together. Trends Pharmacol Sci 2002;23:374–80.
Gupta PK, Subramani J, Singh TU, Leo MDM, Sikarwar AS, Prakash VR, et al. Role of protein kinase G in nitric oxide deficiency-induced supersensitivity to nitrovasodilator in rat pulmonary artery. J Cardiovasc Pharmacol 2008;51(5): 450–456.
Gerber RT, Anwar MA, Poston L. Enhanced acetylcholine induced relaxation in small mesenteric arteries from pregnant rats: an important role for endothelium-derived hyperpolarizing factor (EDHF). Br J Pharmacol 1998;125: 455–460.
Bagher P, Beleznai T, Kansui Y, Mitchell R, Garland CJ, Dora KA. Low intravascular pressure activates endothelial cell TRPV4 channels, local Ca2+ events, and IKCa channels, reducing arteriolar tone. PNAS 2012;109:18174–79.
Saifeddine M, El-Daly M, Mihara K, Bunnett NW, McIntyre P, Altier C, et al. GPCR-mediated EGF receptor transactivation regulates TRPV4 action in the vasculature. Br J Pharmacol 2015;172:2493–506.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Addison, M.P., Singh, T.U., Parida, S. et al. NO synthase inhibition attenuates EDHF-mediated relaxation induced by TRPV4 channel agonist GSK1016790A in the rat pulmonary artery: Role of TxA2. Pharmacol. Rep 68, 620–626 (2016). https://doi.org/10.1016/j.pharep.2016.01.003
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.pharep.2016.01.003