Abstract
Study Design
Retrospective.
Objectives
The authors hypothesized that cervical lordosis (CL) would decrease with aging and increasing degeneration.
Summary of Background Data
It is theorized that with age and degeneration, the cervical spine loses lordosis and becomes progressively more kyphotic; however, no studies support these conclusions in patients with various spinal deformities.
Methods
The authors performed a radiographic analysis of asymptomatic adults (referring to their cervical spine) of varying ages, with differing forms of spinal deformity to the thoracic/lumbar spine to see how cervical lordosis changes with increasing age. A total of 104 total spine EOS X-rays of adult (aged > 18 years) spinal deformity patients without documented neck pain, prior neck surgery, or cervical deformity were reviewed. The researchers only reviewed EOS X-rays because they allow complete visualization from occiput to feet. Cervical lordosis, standard Cobb measurements, sagittal balance parameters, and cervical degeneration were quantified radiographically by the method previously described by Gore et al. Statistical analysis was performed with 1-way analysis of variance to compare significant differences between groups aged <40, 40—60 and >60 years as well as changes in sagittal balance. A p-value <.05 was considered significant.
Results
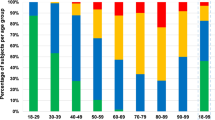
Average CL actually increased with increasing age (10.3 ± 14.7, 15.4 ± 15.1, and 23.3 ± 1.6.7 for age < 40, 40—60, and > 60 years, respectively; p <.05). Average cervical degeneration score increased at all disc space levels from C2 to C7 across age groups (0.7 ± 1.2, 9.9 ± 69, and 16.3 ± 8.9 for age <40, 40—60, and >60 years, respectively; p <.01), with the highest degeneration at the C5—6 and C6—7 disc spaces (3.7 ± 3.3 and 3.2 ± 2.9, respectively; p <.01). This increase did not correlate with the increase in CL seen with aging (r = 0.02; p =.84).
Conclusions
Cervical lordosis increased with aging in adult spinal deformity patients. There was no relationship between cervical degeneration and lordosis despite the strong relationship seen between increasing CL in older age groups.
Similar content being viewed by others
References
Gore DR, Sepic SB, Gardner GM. Roentgenographs findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976) 1986;11:521–4.
Ichihara D, Okada E, Chiba K, et al. Longitudinal magnetic resonance imaging study on whiplash injury patients: minimum 10-year follow-up. J Orthop Sci 2009;14:602–10.
Matsumoto M, Okada E, Ichihara D, et al. Age-related changes of thoracic and cervical intervertebral discs in asymptomatic subjects. Spine (Phila Pa 1976) 2010;35:1359–64.
Okada E, Matsumoto M, Ichihara D, et al. Does the sagittal alignment of the cervical spine have an impact on disk degeneration? Minimum 10-year follow-up of asymptomatic volunteers. Eur Spine J 2009;18:1644–51.
Doual JM, Ferri J, Laude M. The influence of senescence on craniofacial and cervical morphology in humans: surgical and radiologic anatomy. Surg Radiol Anat 1997;19:175–83.
Gore DR. Roentgenographic findings in the cervical spine in asymptomatic persons: a ten-year follow-up. Spine (Phila Pa 1976) 2001;26:2463–6.
Harrison DE, Harrison DD, Cailliet R, et al. Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine (Phila Pa 1976) 2000;25:2072–8.
Yukawa Y, Kato F, Suda K, et al. Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine. Part I: radiographic data from over 1,200 asymptomatic subjects. Eur Spine J 2012;21:1492–8.
Marchiori DM, Henderson CN. A cross-sectional study correlating cervical radiographic degenerative findings to pain and disability. Spine (Phila Pa 1976) 1996;21:2747–51.
Heller JG, Sasso RC, Papadopoulos SM, et al. Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine (Phila Pa 1976) 2009;34:101–7.
Coric D, Nunley PD, Guyer RD, et al. Prospective, randomized, multicenter study of cervical arthroplasty: 269 patients from the Kineflex|C artificial disc investigational device exemption study with a minimum 2-year follow-up: clinical article. J Neurosurg Spine 2011;15:348–58.
Murrey D, Janssen M, Delamarter R, et al. Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J 2009;9:275–86.
Upadhyaya CD, Wu JC, Trost G, et al. Analysis of the three United States Food and Drug Administration investigational device exemption cervical arthroplasty trials. J Neurosurg Spine 2012;16:216–28.
Mummaneni PV, Burkus JK, Haid RW, et al. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine 2007;6:198–209.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author disclosures: HJK (consultant on the Spine Innovation Advisory Board of Medtronic, Inc); LGL (patents from Medtronic [unpaid]; royalties from Medtronic and Quality Medical Publishing; travel reimbursement monies related to meetings/course from BroadWater, Medtronic, SRS); YO (none); TC (none); AM (none); SH (none); JLF (none); KDR (expert testimony; grants from Medtronic for IDE participation; royalties from Osprey, Medtronic, Biomet; stock/stock options with Osprey, Expanding Orthopedics, Spineology, Spinal Kinetics, Amedica, Nexgen Spine, Vertiflex, Benvenue, Paradigm Spine, PSD).
Rights and permissions
About this article
Cite this article
Kim, H.J., Lenke, L.G., Oshima, Y. et al. Cervical Lordosis Actually Increases With Aging and Progressive Degeneration in Spinal Deformity Patients. Spine Deform 2, 410–414 (2014). https://doi.org/10.1016/j.jspd.2014.05.007
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2014.05.007