Abstract
Introduction
Cardiopulmonary resuscitation (CPR) is frequently performed in hospitalized patients after in-hospital cardiac arrest (IHCA), especially in the intensive care unit (ICU) (J Crit Care 24:408-414, 2009). Despite the fact that nearly half of the in-hospital cardiac arrests (IHCA) actually happen in intensive care units (ICUs) (N Engl J Med 367:1912-1920, 2012), intensive care unit cardiac arrest (ICU-CA) compared to IHCA or out-of-hospital cardiac arrests (OHCA) has received little attention, and data on ICU-CA remains scanty (Intensive Care Med 40:1853-1916, 2014).
Aim
We aimed to evaluate the clinical status and factors associated with the survival of patients subjected to cardiopulmonary resuscitation (CPR) after a witnessed cardiac arrest (CA) inside the medical intensive care unit (MICU).
Patients
The study included 110 patients, mean age of 60 ± 18 years, 69 (63%) males, and 41 (37%) females. Co-morbidities included diabetes mellitus was present in 46 (42%), hypertension 57 (52%), central nervous system (CNS) disease 31 (29%), cardiovascular (CVS) 76 (69%), respiratory 63 (57%), hepatic 16 (15%), shock 35 (32%), and renal 44 (40%). Mechanical ventilation was present in 97 (88%) of patients. SOFA score < 9 was present in 38%, MPM III score < 10 in 37%, and GCS > 7 in 66% of patients. Non-shockable rhythm occurred in 95 (86%) while shockable rhythm in 15 (14%) of patients.
Methods
Data were collected prospectively at the medical ICU of Cairo University from Jan. 2013 to Feb 2013. A resuscitation protocol was done according to the latest recommendation of the European Society of Cardiology at the time of patient inclusion. Clinical data were recorded and surviving patients were clinically followed daily until hospital discharge.
Results
Out of 110 witnessed cardiac arrests, CPR was initially successfully manifested by return of spontaneous circulation (ROSC) in 60 patients (55%), of whom 22 (20%) survived hospital discharge and only 9 patients (8%) were functionally independent. Compared to non-survivors, 60 patients (55%) with ROSC had a MPM III < 10 (p 0.015), EF ≥ 50% (p 0.001), and non-shocked patients (p 0.008). Other factors such as DC shocks < 3 (p 0.02), CPR cycles < 2 (p < 0.001), resuscitation duration < 10 min (p 0.03), time to start CPR < 1 min (p 0.001), maintained HCO3 (p 0.03), and PaCO2 (p 0.002) were found to improve ROSC. Mortality before discharge decreased with asystole (p < 0.01). Mortality before discharge increased with CNS (p < 0.02) and respiratory comorbidities (p 0.02), shock (p < 0.001) and mechanical ventilation (p < 0.0001), SOFA > 9 (p 0.001), MPM III > 10 (0.018), and time to start CPR > 1 min (p 0.001).
Conclusion
Not all ROSC reached long-term survival and hospital discharge. Several co-morbidities affect ROSC and short-term and long-term patient survival after witnessed MICU cardiac arrest.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiopulmonary resuscitation (CPR) is frequently performed in hospitalized patients after in-hospital cardiac arrest (IHCA), especially in the intensive care unit (ICU) after ICU cardiac arrest (ICU-CA) [1]. The incidence of cardiac arrest in the intensive care unit (ICU-CA) pooled rate across all studies was 2.27% and contemporary cohorts between 2014 and 2018 have not shown a clear reduction in the overall incidence compared to older studies which span a period of 30 years. Over time the disease severity has increased together with a significant advancement of critical care interventions, so that an unchanging incidence of ICU-CA in the face of an increased severity of illness could represent a management progress (Armstrong 2018) [2].
Despite the fact that nearly half of in-hospital cardiac arrests (IHCA) actually happen in intensive care units (ICUs) [3], intensive care unit cardiac arrest (ICU-CA) in comparison with IHCA or out-of-hospital cardiac arrests (OHCA) has received little attention, and data on ICU-CA remains scanty [4].
Information on survival after CPR for ICU patients might be of great value in facilitating future medical decisions and family discussions concerning CPR subjects.
Aim of the work
We aimed to evaluate the clinical status and factors associated with the survival of patients subjected to cardiopulmonary resuscitation (CPR) after a witnessed cardiac arrest (CA) inside the medical intensive care unit (MICU).
Patients and methods
Patients
Cardiopulmonary arrest was defined as sudden cessation of spontaneous respiration and circulation leading to loss of consciousness manifested by the absence of a palpable central pulse, apnea, and unresponsiveness (Paul et al., 2016) [5] which needs CPR, which is defined as the use of chest compressions and rescue breathing (Mark, and Anna- 2011) [6].
The study included 110 patients, mean age 60 ± 18 years, 69 (63%) males, 41 (37%) females Cardiopulmonary arrest was defined as sudden cessation of spontaneous respiration and circulation leading to loss of consciousness manifested by the absence of a palpable central pulse, apnea, and unresponsiveness (Paul et al., 2016) [5], whom need CPR which is defined as use of chest compressions and rescue breathing as per guidelines (Mark, and Anna- 2011) [6, 7].
Inclusion criteria
All adult MICU patients who suffered witnessed cardiac arrest and had CPR inside the MICU.
Exclusion criteria
-
1)
Patients who had a do-not-resuscitate (DNR) order.
-
2)
CPR that began outside of MICU.
Methods
Resuscitation protocols were evaluated at the time of analysis according to the latest recommendations of the European Society of Cardiology and the American Heart Association (2015) [8]. Clinical data were recorded and surviving patients were clinically followed daily until hospital discharge.
Data were analyzed according to following:
Pre-arrest clinical status:
-
Age, sex, comorbidities, clinical examination.
-
Electrocardiography (ECG) and echocardiography (Echo).
-
Arterial blood gas analysis (ABG) analysis.
-
Rapidly correctable causes (tension pneumothorax, tamponade cardiac, toxins, thrombosis coronary or pulmonary, trauma, hypovolemia, hypoxia, hydrogen ion acidosis, hyperkalemia or hypokalemia, hypothermia, hypoglycemia)
Scoring systems:
GCS (Glasgow coma scale) (motor examination, pupil response, corneal response): a neurological scale that aims to give an indication of the conscious state of a person with a score between 3 and 15 (Teasdale and Jennett-1974) [9].
MPM0-III score (Mortality Probability Model): assessed within 1 h of ICU admission to estimate mortality probability of hospital discharge (Higgins et al., 2007) [10].
SOFA Score (Sequential Organ Failure Assessment Score): quantifies the severity of the patient’s illness, based on the degree of organ dysfunction data on six organ failures, and is scored on a scale of 0–4. (Ferreira et al., 2001) [11].
CPR procedure assessment:
-
Drugs used (adrenaline, atropine, amiodarone, lidocaine, NaHco3, and Ca gluconate).
-
Cardiac rhythm (shockable (VF and pulseless VT), and non-shockable (asystole and PEA)).
-
Time of shift (morning or night).
-
Time to start management and duration of management.
-
ABG analysis.
-
CPR cycles (less than 2 cycles or more than 2 cycles).
-
Direct current (DC) shocks (less than 3 or more than 3 DC shocks).
Post-resuscitation outcome:
-
Initial survival manifested by the return of spontaneous circulation (ROSC): defined as restoration of a pulse for at least 20 min from cardiac arrest (Jacobs et al., 2004) [12].
-
Survival to hospital discharge, defined as the proportion of post-CPR ICU patients who were discharged alive.
-
Patient functionally dependent or independent on others. This was determined if the survivor needed a full-time companion to fulfill his activities.
Patient classification according to outcome is as follows:
-
I)
Short-term immediate outcome:
-
II)
Survivors: Patients with the return of spontaneous circulation (ROSC) after CPR (defined as a resumption of sustained perfusing cardiac activity more than 20 min associated with significant respiratory effort after cardiac arrest (Jacops et al., 2004) [12]
-
III)
Non-survivors: Patient who died after failed CPR procedure (no ROSC after CPR).
-
IV)
Long-term outcome:
-
V)
Survivors at discharge: patients with ROSC and survived to hospital discharge.
-
VI)
Non-survivors at discharge: patients who died after CPR failure or patients with ROSC but died before discharge.
Statistical analysis
Data were statistically described in terms of mean, standard deviation (SD), median and range, or frequencies (number of cases) and percentages when appropriate. Comparison of numerical variables between the study groups was done using Student’s t test for independent samples for normally distributed data and the Mann–Whitney test for non-normal data.
For comparing categorical data, a chi-square test was performed. The exact test was used instead when the expected frequency was less than 5. Correlation to mortality was done using the Spearman rank correlation equation.
p values less than 0.05 were considered statistically significant.
All statistical calculations were done using the computer program SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA) release 15 for Microsoft Windows (2006).
Results
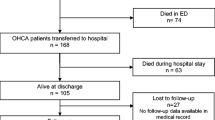
We studied a total of 110 (100%) MICU patients with a mean age 60 ± 18 years CPR was initially successfully manifested by ROSC in 60 (55%), 22 (20%) survived to hospital discharge, and only 9 (8% of total patients, 41% of survivors to discharge) were functionally independent; however, 14 (59% of survivors to discharge) were dependent on an assisting companion.
Male gender 69 (63%), out of whom 36 (52%) exhibited ROSC and 16 (23%) survived to hospital discharge. Gender was not associated with a statistically significant difference neither for initial ROSC (p 0.65) nor for survival to discharge [p 0.40].
Age > 50 was present in 84 (76%), out of whom 44(52%) exhibited ROSC and 15(18%) survived hospital discharge vs. 40 (48%) failed CPR and 69 (82%) did not survive hospital discharge. Age was not associated with a statistically significant difference neither for initial ROSC (p 0.55) nor for with survival to discharge (p 0.47) (Table 1, Fig. 1).
Clinical comorbidities clinical severity scores
-
Diabetes mellitus was present in 46 (42%), hypertension 57 (52%), CNS 31 (29%), cardiovascular (CVS) 76 (69%), respiratory 63 (57%), hepatic 16 (15%), shock 35 (32%), and renal 44 (40%). Mechanical ventilation was present in 97 (88%) of patients.
-
CNS comorbidities were associated with increased initial ROSC (p 0.05) but a decreased survival to discharge (p 0.02).
-
Respiratory comorbidities were associated with survival to discharge (p 0.02).
-
Shock was associated with a decreased ROSC (p 0.008) and a decreased survival to discharge (p < 0.001).
-
Mechanical ventilation was associated with decreased survival to discharge (p < 0.0001)
-
Other comorbidities such as diabetes (DM)s, hypertension (HTN), cardiovascular (CVS), and hepatic or renal comorbidities were not associated with any significant associations with outcome survival (p > 0.05) (Table 1, Figs. 1 and 2).
Clinical severity scores
SOFA score < 9 was present in 38%, MPM III score < 10 in 37%, and GCS > 7 in 66% of patients.
MPM III score < 10 was associated with initial ROSC (p 0.015) and survival to hospital discharge (p 0.018).
SOFA score < 9 was not associated with initial ROSC (p 0.07) but was associated with survival to hospital discharge (p < 0.001).
GCS > 7 was not associated with a statistically significant difference neither for initial ROSC (p 0.28) nor for survival to hospital discharge (p 0.07) (Table 2).
Rapidly correctable causes were not associated with any significant survival outcome (p > 0.05).
Echo evaluation pre-arrest (Table 3)
EF < 50% was significantly associated with decreased initial ROSC (p 0.01).
Evaluation of CPR procedure
Cardiac rhythm at the time of cardiac arrest (Table 4 , Fig. 3 )
Non-shockable rhythm (asystole or pulseless electrical activity (PEA)) were encountered in 95 (86%) of patients, out of who 51 (54%) exhibited ROSC and 20 (21%) survived to long-term discharge vs. 44 (46%) failed CPR and a total of 75 (79%) did not survive to hospital discharge (p > 0.05).
Asystole occurred in 88 patients (86%), out of who 48 (55%) exhibited ROSC and 13 (15%) survived hospital discharge vs. 40 (45%) failed CPR and 75 (85%) did not survive hospital discharge. PEA occurred in 7 patients (7%), 3 out of 7 (43%) exhibited ROSC and 2 out of 7 (29%) survived to hospital discharge vs. 4 out of 7 (57%) failed CPR and 5 out of 7 (71%) did not survive to hospital discharge (p > 0.05).
Asystole was associated with survival to hospital discharge (p 0.01).
Shockable rhythm (ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT)) was encountered in 15 patients (14%), out of whom 9 (60%) exhibited ROSC and 2 (13%) survived to hospital discharge vs. 6 (40%) failed CPR and 13 (87%) did not survive to hospital discharge. VF occurred in 4 patients (4%), out of who 2 (50%) exhibited ROSC and 2 (50%) survived hospital discharge vs. 2 (50%) failed CPR and 2 (50%) did not survive hospital discharge. Pulseless VT occurred in 12 patients (11%), out of who 7 (64%) exhibited ROSC and 5 (45%) survived hospital discharge vs. 4 (36%) failed CPR and 6 (55%) did not survive hospital discharge.
Shockable rhythms at the time of cardiac arrest were not associated with any significant association with outcome (p > 0.05).
CPR performance (Table 5 , Fig. 4 )
-
Duration of CPR < 10 min was associated with increased initial ROSC (p 0.03).
-
Number of CPR cycles < 2 were associated with increased initial ROSC (p < 0.001).
-
Number of DC shocks < 3 were associated with increased initial ROSC (p 0.02).
-
Adrenaline doses were not associated with any significant difference neither with initial ROSC (p 0.120 nor with survival to hospital discharge (p 0.07).
-
Time of shift whether morning or night at the time of CPR was not associated with a statistically significant difference neither for initial ROSC (p 0.98) nor for survival to hospital discharge (p 0.35).
Arterial blood gas analysis (Table 6 )
-
Higher PaCO2 was associated with an increase in initial ROSC (p 0.01)
-
Higher HCO3 was associated with an increase in initial ROSC (p 0.009). Rapidly correctable causes were not associated with any significant impact on outcome ( p > 0.05)
Drugs used (Table 3 )
The use of noradrenaline, adrenaline, atropine, amiodarone, lidocaine, sodium bicarbonate, and calcium gluconate did not show any significant associations with outcome survival (p > 0.05).
Discussion
The available data on intensive care cardiac arrest (ICU-CA) are quite limited and mostly were retrospective studies [1]. Cardiac arrest has been suggested to be a hidden epidemic that is associated with poorer outcomes for the sickest hospital patients. Prospective data collection would better define its scale and prognostic implications as it may offer an opportunity to intervene to improve patient outcomes. (Richard A Armstrong 2018) [2]. Our study provides a prospective clinical assessment of the outcome of patients who witnessed cardiac arrest inside the ICU and received CPR.
Studies of ICU-CA showed a high initial success and ROSC (24–100%), but the survival to discharge remained low (0% to 47%) [13,14,15,16,17].
Our initial survival rate manifested by ROSC was 55%. We adopted a ROSC definition to be the resumption of sustained perfusing cardiac activity > 20 min associated with significant respiratory effort after cardiac arrest [18, 19]. On the other hand, other authors defined successful CPR in numerous ways, such as the presence of pulse [20] or survival > 30 s [1, 21], restoration of cardiac function ≥ 5 min [22], or survival 24 h [13]. These variable definitions may be the cause of variability in outcomes among those studies. Studies on mixed-popularity general ICU patients documented a lower ROSC rate than other sites in the hospital [23]. Patients from mixed ICUs probably have multiple factors contributing to the occurrence of cardiac arrest and complete physiological failure [4].
Our study showed that 20% survived to hospital discharge. Previous studies on a majority of shocked patients showed a 16% survival to hospital discharge [15]. Cardiovascular and surgical patients with good prognosis showed the highest survival-to-discharge rate [13], while cancer patients with bad prognosis showed a very low 2% survival-to-discharge rate [24]. The different underlying illness is definitely associated with a different survival outcome and plays an important role in determining the prognosis.
Our study was in concordance with other studies [1, 21, 23, 25] showing no significant association between age and outcome. Some older studies have shown that patient’s aged > 60 years can predict poor outcomes [26, 27].
The effect of age on survival may be confounded by a selection bias as older patients (> 70 years) are less likely to receive CPR than younger patients [28]. This is explained by healthcare providers showing the trend for less aggressive care and less effective CPR in old patients during cardiac arrest compared to young patients [29].
We also showed similarity with other studies which proved that long-term survival had no specific association with gender [23, 30]. Conversely, some older studies reported a better female survival to discharge [31, 32].
Central nervous system comorbidities in our study were more associated with ROSC than with CPR failure. Unfortunately, this was not extended to a longer-term benefit; in fact, cerebrovascular comorbidities were more associated with a decrease in survivors to discharge. In concordance with previous studies, CNS comorbidities have been shown to be predictive of unfavorable long-term outcomes [33], and lower CNS SOFA sub-scores were associated with a lower survival to discharge [30].
Renal comorbidities in our study did not show any association with outcome, in concordance with Tian et al. (2010) [15]. Other studies emphasized renal failure as a more significant determinant of outcome than other comorbidities [30].
Our study in concordance with Tian (2010) showed that respiratory comorbidities were associated with decreased survivors to discharge [15]. We also proved that mechanical ventilation pre-arrest was associated with a decrease survival to discharge. The ICON registry (2016) [30] showed that mechanical ventilation on admission was one of the predictors of unfavorable neurological outcomes.
Cardiac comorbidities in our study did not show a significant association with outcome; however, we showed that shock was associated with both a decreased initial ROSC (p 0.008) and decreased survival to discharge (p < 0.001). Other studies concluded that CVS SOFA sub-score was lower in survivors [30] and that patients had a better survival if they were not on vasopressors at the moment of cardiac arrest or immediately previously to that [15, 30, 34]. The presence of shock and the need for vasopressors reflect a worse state of hypo-perfusion of vital organs with more liability of tissue damage and a possible decreased chance of survival.
The pH post-arrest has been previously shown to be associated with higher ROSC [29]; however, we did not show any significant association of PH with outcome. In our study, higher levels of PaCO2 and HCO3 were associated with a higher ROSC. The consumption of HCO3 may be pronounced in prolonged hypoperfusion and anaerobic metabolism, which has a bad prognostic value.
We documented that a higher MPM0-III score was associated with failed CPR and non-survival to discharge and that a higher SOFA score was associated with non-survival to discharge. Efendijev et al. (2014) showed that higher SOFA and APACHE II scores were predictive of long-term worse outcomes [4]. The ICON registry showed that SOFA scores on admission were higher in non-survivors [30]. Kutsogiannis et al. (2011) showed that the APACHE II score was not an independent predictor of ROSC [13]. Similarly, Skrifvars et al., in 2012, showed that the APACHE score did not have a good prognostic value in cardiac arrest [35].
Our study showed that non-shockable rhythms (asystole or PEA) were the most common cardiac arrest rhythms 86% compared to only 14% shockable rhythms (VT/VF). This ratio is similar to the majority of studies of in-hospital cardiac arrests (IHCA) demonstrating that non-shockable rhythms were the dominant initially observed rhythms, ranging from 61.5 to 89.7% with a profit rate of 76.8% [2, 15, 18, 21, 36, 37]. IHCA is frequently precipitated by hypoxia or hypotension, which more likely manifests by asystole, while out-of-hospital cardiac arrests (OHCA) are more commonly precipitated by ischemia which often manifests by shockable rhythms (VT, VF) [38]. In similarity to our study, some studies have shown that asystole was associated with lower survival to discharge [39, 40]. Conversely, other studies observed a favorable outcome with non-shockable rhythms [6, 16]. Asystole may be reversible as it is frequently precipitated by rapidly correctable causes (such as hemorrhage, cardiac tamponade, hypoxia, or hypotension [21].
Our study showed that ICU-CA in early morning shifts was more common than night shifts which may be attributed to cortisol-catecholamine surge upon awakening [13]. The time of arrest had no significant association with the outcome which is similar to Kutsogiannis et al. (2011) [13]. Conversely, Peberly et al. (2008) showed a higher ROSC [41] and Brindely et al. (2002) showed greater survivors to discharge in early morning shifts than in night shifts [42]. A possible explanation is the presence of more staff and expert physicians during morning shifts in some ICUs.
Our study was similar to that of Shih et al. (2004) who showed that the duration of resuscitation longer than 10 min was associated with decreased ROSC [1]. Conversely, Goldberger et al., in 2012, showed that resuscitation time longer than 25 min was predictive of higher ROSC [43]. Previous studies proved that a resuscitation time longer than 15 min has been associated with a decrease in survival to discharge [21, 36, 44], and that a longer duration of resuscitation is associated with higher mortality [45]. The longer duration for resuscitation is probably coupled with longer vital tissue hypo-perfusion and damage [46].
CPR Outcome and its effects on functional dependency
In our study 13 (59%) of 22 survivors to discharge were functionally dependent on a companion while only 9 (41%) of the 22 survivors to discharge were functionally independent. In concordance with our results, Hayley et al. (2012) demonstrated that 80% of survivors to discharge remained functionally dependent [17]. Enohuma et al. (2006) showed that 44% were discharged to rehabilitation centers or to another hospital [21].
Favorable outcomes may be expected if the CPR procedure was done inside rather than outside the hospital owing to a possibly earlier initiation of CPR, proximity of CPR equipment, and the availability trained personnel, especially in the ICU. On the other hand, ICU patients have a higher severity of illness and are more susceptible to cardiac arrests due to the presence of associated multiple comorbidities which have a definite impact on the outcome of their own. The variability in outcomes may be due to the heterogeneity of the underlying severity of comorbidities, patient demographics, and arrest etiologies.
Cardiopulmonary resuscitation for intensive care unit cardiac arrests (ICU-CA) has the privilege of being continuously monitored in the presence of highly qualified personnel and, therefore, may theoretically be expected to have a higher successful rate than CPR performed outside the ICU. On the other hand, the severity of the critical illness may disturb these expectations [1, 47].
CPR for cardiac arrest inside the ICU show variable rates of short- and long-term survival which were associated with the underlying clinical comorbidities. Our finding may aid physicians in further understanding of the prognosis of patients who receive CPR in the ICU and possibly aid in modifying future management strategies and improving ICU care.
Study limitations
We included only two ICUs with relatively small sample sizes. There was no long-term follow-up after hospital discharge.
Conclusions
-
Initially, successful CPR and ROSC occurred in 60 patients (55%) with MICU-CA. Witnessed cardiac arrest, in-hospital versus outside the hospital cardiac arrest, as well as co-morbidities, do impact the success of CPR and ROSC
-
After a witnessed MICU CA, a non-shockable rhythm was present in 86% while a shockable rhythm in 14% of patients. CPR was initially successfully manifested by ROSC in 55% of cases while 20% survived to hospital discharge. Only 8% of total patients survived to discharge and were functionally independent.
-
ROSC increased with MPM III < 10, EF ≥ 50%, non-shocked state, maintained HCO3 and PaCO2, DC shocks < 3, CPR cycles < 2, resuscitation duration < 10 min, and time to start CPR < 1 min.
-
Mortality before discharge was higher with CNS and respiratory comorbidities, shocked and mechanically ventilated patients, SOFA > 9, MPM III > 10, and time to start CPR > 1 min. Mortality before discharge was less with asystole.
-
Unsuccessful CPR and mortality before discharge were both higher in patients with MPM III > 10 and shock.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- CPR:
-
Cardiopulmonary resuscitation
- ICU-CA:
-
Intensive care unit cardiac arrest
- IHCA:
-
In-hospital cardiac arrest
- OHCA:
-
Out-of-hospital cardiac arrest
- ROSC:
-
Return of spontaneous circulation
References
Chang S, Huang C, Shih C, et al. Who survives cardiac arrest in the intensive care units. J Crit Care. 2009;24:408–14.
Armstrong RA, Kane C, Oglesby F, Barnard K, Soar J, Thomas M. The incidence of cardiac arrest in the intensive care unit: A systematic review and meta-analysis. J Intensive Care Soc. 2019;20(2):144–54.
Girotra S, Nallamothu BK, Spertus JA, et al. Trends in survival after inhospital cardiac arrest. N Engl J Med. 2012;367:1912–20.
Efendijev I, Raj R, Reinikainen M, et al. Temporal trends in cardiac arrest incidence and outcome in Finnish intensive care units from 2003 to 2013. Intensive Care Med. 2014;40(12):1853–916.
Chan PS, et al. Resuscitation Practices Associated With Survival after In Hospital Cardiac Arrest A Nationwide Survey. JAMA Cardiol. 2016;1(2):189–97.
Ebell MH, Afonso AM. Pre-arrest predictors of failure to survive after in-hospital cardiopulmonary resuscitation: a meta-analysis. Fam Pract. 2011;28(5):505–15.
Nolan JP, Sandroni C, Böttiger BW, et al. European Resuscitation Council and European Society of Intensive Care Medicine guidelines 2021: post-resuscitation care. Intensive Care Med. 2021;47:369–421.
American Heart Association. (2015): Web-based Integrated Guidelines for CPR & ECC. Available at https:// eccguidelines. heart. org/ index. php/ circulation/ cpr-ecc- guidelines- 2/. October 15, 2015.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness: A practical scale. The Lancet. 1974;2(7872):81–4.
Higgins TL, Teres D, et al. Assessing contemporary intensive care unit outcome: an updated Mortality Probability Admission Model (MPM0-III). Crit Care Med. 2007;35:827–35.
Ferreira FL, Bota DP, et al. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286:1754–8.
Jacobs I, Nadkarni V, Bahr J, et al. "Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries. Circulation. 2004;110(21):3385–97.
Kutsogiannis DJ, Bagshaw SM, Laing B, Brindley PG. Predictors of survival after cardiac or respiratory arrest in critical care units. CMAJ. 2011;183:1589–95.
Lee HK, Lee H, No JM, et al. Factors influencing outcome in patients with cardiacarrest in the ICU. Acta Anaesthesiol Scand. 2013;57:784–92.
Tian J, Kaufman DA, Zarich S, et al. Outcomes of critically ill patients who received cardiopulmonary resuscitation. Am J Respir Crit Care Med. 2010;182:501–6.
Rabinstein AA, McClelland RL, Wijdicks EF, et al. Cardiopulmonary resuscitation in critically ill neurologic neurosurgical patients. Mayo Clin Proc. 2004;79:1391–5.
Gershengorn HB, Li G, et al. Survival and functional outcomes after cardiopulmonary resuscitation in the intensive care unit. J Crit Care. 2012;27(4):421.e9-17.
Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14,720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308.
Suraseranivongse S, Chawaruechai T, Saengsung P, Komoltri C. Outcome of cardiopulmonary resuscitation in a 2300-bed hospital in a developing country. Resuscitation. 2006;71:188–93.
Brindley PG, Markland DM, Mayers I, et al. Predictors of survival following in-hospital adult cardiopulmonary resuscitation. CMAJ. 2002;167:343–8.
Enohumah KO, Moerer O, Kirmse C, et al. Outcome of cardiopulmonary resuscitation in intensive care units in a university hospital. Resuscitation. 2006;71:161–70.
Myrianthefs P, Kalafati M, Lemonidou C, et al. Efficacy of CPR in a general, adult ICU. Resuscitation. 2003;57:43–8.
Rasheed AM, Amera MF, Parameaswari PJ, et al. The Initial Success Rate of Cardiopulmonary Resuscitation and It’s Associated Factors among Intensive Care Unit Patients in a Tertiary Hospital in Saudi Arabia. J Intensive & Crit Care. 2016;2:2.
Wallace S, Ewer MS, Price KJ, Feeley TW. Outcome and cost implications of cardiopulmonary resuscitation in the medical intensive care unit of a comprehensive cancer center. Support Care Cancer. 2002;10:425–9.
Van Den Noortgate N, Vogelaers D, Afschrif TM, et al. Intensive care for very elderly patient: Outcome and risk factors for in-hospital mortality. Age Ageing. 1999;28:253–6.
Schultz SC, Cullinane DC, et al. Predicting in-hospital mortality during cardiopulmonary Resuscitation. Resuscitation. 1996;33:13–7.
Herlitz J, Bang A, Gunnarsson J, et al. Factors associated with survival to hospital discharge among patients hospitalized alive after out of hospital cardiac arrest: Change in outcome over 20 years in the community of Göteborg, Sweden. Heart. 2003;89:25–30.
Schwenzer KJ, Smith WT, Durbin CG Jr. Selective application of cardiopulmonary resuscitation improves survival rates. Anesthesia Analgesia. 1993;76:478–84.
Hamel MB, Lynn J, Teno JM, Covinsky KE, Wu AW, et al. Age-related differences in care preferences, treatment decisions, and clinical outcomes of seriously ill hospitalized adults: Lessons from SUPPORT. Journal of American Geriatric Society. 2000;48:176–82.
Nobile L, Fabio S, et al. The impact of extra cerebral organ failure on outcome of patients after cardiac arrest: an observational study from the ICON database Critical Care. 2016;20:368.
Herlitz J, Bång A, Aune S, et al. Characteristics and outcome among patients suffering in-hospital cardiac arrest in monitored and non-monitored areas. Resuscitation. 2001;48(2):125–35.
Perers E, Abrahamsson P, et al. There is a difference in characteristics and outcome between women and men who suffer out of hospital cardiac arrest. Resuscitation. 1999;40:133–40.
Merchant RM, Berg RA, Yang L, Becker LB, Groeneveld PW, et al. Hospital variation in survival after in-hospital cardiac arrest. J Am Heart Assoc. 2014;3: e000400.
Grigoriyan A, Vazquez R, Palvinskaya T, et al. Outcomes of cardiopulmonary resuscitation for patients on vasopressors or inotropes: a pilot study. J Crit Care. 2009;24:415–8.
Skrifvars MB, Varghese B, Parr MJ. Survival and outcome prediction using the Apache III and the out-of hospital cardiac arrest (OHCA) score in patients treated in the intensive care unit (ICU) following out-of-hospital, in hospital or ICU cardiac arrest. Resuscitation. 2012;83:728–33.
Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–7.
Meaney PA, Nadkarni VM, Kern KB, Indik JH, Halperin HR, Berg RA. Rhythms and outcomes of adult in-hospital cardiac arrest. Crit Care Med. 2010;38:101–8.
Cooper S, Janghorbani M, Cooper G. A decade of in-hospital resuscitation: Outcomes and prediction of survival? Resuscitation. 2006;68:231–7.
Skogvoll E, Isern E, et al. In-hospital cardiopulmonary resuscitation, 5 years incidence and survival according to the Ustein template. Acta Anaesthesiol Scand. 1999;43:177–84.
Rankin APN. The in-hospital Ustein style: use in reporting outcome from cardiac arrest in Meddlemore hospital 1995–1996. Resusxitation. 1998;36:91–4.
Peberdy MA, Ornato JP, Larkin GL, et al. Survival from in-hospital cardiac arrestduring nights and weekends. JAMA. 2008;299:785-92.7.
Brindley PG, Markland DM, Mayers I, et al. Predictors of survival following in-hospital adult cardiopulmonary resuscitation. CMAJ. 2002;167:343–8.
Goldberger ZD, Chan PS, Berg RA, et al. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: An observational study. Lancet. 2012;380:1473–81.
Hyeong-Joong Y, Young-Soo K, Yong K, Suck-Jun O, Kwang-Myung K, et al. Factors associated with survival and neurological outcome after cardiopulmonary resuscitation of neurosurgical intensive care unit patients. Neurosurgery. 2006;59:838–46.
Rosenbaum EA, Shenkman L. Predicting outcome of in-hospital cardiopulmonary resuscitation. Crit Care Med. 1988;16:583–6.
Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007;33:237–45.
Tobi KU, Abhulimhen-Iyoha BI. Cardio Pulmonary Resuscitation in Children: Outcome in a General Intensive Care Unit in Nigeria. West Afr J Med. 2014;33(4):239–44.
Acknowledgements
NA.
Funding
NA.
Author information
Authors and Affiliations
Contributions
S.S.: Data Collection and analysis, Scientific writing. YN: Protocol design, Clinical supervision. SF: Patient enrolling, Data Collection. AG: Supervision. SM: Protocol design, Supervision, Editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval was granted from the Cairo University Critical Care Department Ethical Committee in December 2012. Consent to Participate was obtained from the attending relative or if no relative was available, the arrest witness.
Consent for publication
NA.
Competing interests
Prof Sherif Mokhtar is a co-author of this study and the Honorary Editor-in-Chief of the journal. He was not involved in handling this manuscript during the submission. The rest of the authors have no conflict of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nassar, Y., Fathy, S., Sabri, S. et al. Clinical outcomes of patients with in-hospital witnessed cardiac arrest: effect of co-morbidities. Egypt. J. Critical. Care. Med. 11, 2 (2024). https://doi.org/10.1007/s44349-024-00002-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44349-024-00002-0