Abstract
According to the 2022 European Society of Cardiology (ESC)/European Respiratory Society (ERS) guidelines, a right heart catheterization-derived mean pulmonary arterial pressure (mPAP) > 20 mmHg at rest defines pulmonary hypertension (PH). As PH can ultimately lead to death, multidisciplinary early diagnosis, proper framework, and prompt management are crucial. ESC/ERS PH classification encompasses five groups, each sharing pathogenesis, hemodynamics, and management, i.e., group I, pulmonary arterial hypertension; II, left heart disease; III, lung disease and/or hypoxia; IV, chronic thromboembolic PH; and V, with unclear and/or multifactorial mechanisms. Chest CT is pivotal in PH grouping, comprehensively evaluating the lung, heart, pulmonary vessels, and mediastinum. In this review, we synoptically illustrate the chest CT findings of PH and provide a CT-based logical framework suggesting a PH group hypothesis. Improving knowledge of PH CT features and their combination empowers radiologists to contribute valuably to the PH multidisciplinary clinical discussion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pulmonary hypertension (PH) refers to a broad group of conditions sharing a pathologic elevation of the mean pulmonary artery pressure (mPAP) [1, 2]. In this review, we aimed to give non-dedicated radiologists basic knowledge on chest computed tomography (CT) role in PH, highlighting its inherent capability of comprehensively evaluating all the chest compartments to provide clinicians with critical diagnostic and prognostic information. Following a brief overview of key PH clinical issues and imaging modalities, we present a per-chest compartment analysis of typical CT findings in PH. We provide reference figures and synoptic tables to help the radiologist valuably contribute to the PH multidisciplinary team clinical discussion.
Definition and classifications
Current guidelines from the European Society of Cardiology (ESC)/European Respiratory Society (ERS) define PH as a right heart catheterization-defined mean mPAP value > 20 mmHg at rest [1]. PH can further be classified into pre-capillary PH, isolated postcapillary PH (IpcPH), and combined pre- and postcapillary PH (CpcPH) according to different combinations of pulmonary arterial wedge pressure (PAWP) and pulmonary vascular resistance (PVR) values (Table 1) [3, 4].
According to the leading presumed cause, physicians clinically classify PH into five groups (Table 2, Fig. 1), sharing pathogenesis, hemodynamics, and management strategies. Basically, the group I (also named pulmonary arterial hypertension, PAH) includes cases that are idiopathic, heritable, or associated with various conditions, e.g., drugs, connective tissue disease, and congenital heart disease; group II is associated with left heart disease; group III is associated with lung disease and/or hypoxia; group IV mainly includes chronic thromboembolic PH (CTEPH); and group V gather cases with unclear and/or multifactorial mechanisms, e.g., sarcoidosis. Notably, all the groups may include pre- and postcapillary components contributing to mPAP elevation. The ESC/ERS guidelines recommend a patient's multiparametric risk assessment to steer management and stratify the mortality risk [1].
Clinical pulmonary hypertension (PH) classification according to the 2022 European Society of Cardiology/European Respiratory Society guidelines. For each PH group, a visual speedometer indicates the potential CT clinical utility level according to evidence from the literature, with green being the most useful. The figure was created with BioRender.com. CTD connective tissue disease; CT computed tomography; PH pulmonary hypertension; IpcPH isolated postcapillary PH; CpcPH combined pre- and postcapillary PH
Group I. PAH is a progressive disease characterized by pulmonary artery cell proliferation, ultimately leading to luminal narrowing [5]. It can affect all age groups, with a higher prevalence among older patients with comorbidities. The current incidence approximates six cases per million adults [6]. The major causes are idiopathic, heritable, drug-induced, connective tissue disease (CTD), and congenital heart disease-associated [5]. Among CTDs, systemic sclerosis (SSc) is the leading cause of PAH in European countries [7]. Other possible causes include HIV, schistosomiasis, and portal hypertension. PAH also includes pulmonary veno-occlusive disease/pulmonary capillary hemangiomatosis (PVOD/PCH), which is a rare, potentially life-threatening, and rapidly evolving disease with overt features of venous/capillary involvement [8].
Group II. PH associated with left heart disease (LHD-PH) represents the most common cause of PH [1]. A retrograde transmission of increased left-sided pressures into the pulmonary circulation results in PH [5], pointing out endothelial dysfunction and pulmonary vascular remodeling. Hemodynamically, LHD-PH can present either an IpcPH or CpcPH component. Patients are typically elderly, often presenting with metabolic syndrome, structural left heart disease, or left atrial (LA) dilatation [6].
Group III. Chronic lung disease-related PH (CLD-PH) represents the second most common cause of PH. The primary contributors to CLD-PH include emphysema, restrictive lung diseases, hypoventilation syndromes, and lymphangioleiomyomatosis (LAM). In patients with chronic lung disease, structural modification of lung parenchyma may lead to vascular changes and, ultimately, to PH. Continuous or intermittent hypoxia is common in chronic lung disease and may result in pulmonary vessel constriction, release of growth factors, and subsequent intimal hyperplasia conditioning an increased vascular tone [9].
Group IV. This group includes PH conditions caused by obstructive pulmonary artery (PA) lesions. CTEPH is the most common cause. Non-resolved thrombi result in organization and fibrosis, thus narrowing vessels and impairing blood flow [6]. Group IV PH may rarely be due to PA sarcoma or large-vessel pulmonary vasculitis.
Group V. This group encompasses a wide range of disorders. The etiology is multifactorial, involving increased pre- and postcapillary pressure and direct effects on pulmonary vasculature [1]. Example conditions include myeloproliferative disorders, chronic renal failure, sarcoidosis, and thyroid disease [6].
Overview of imaging modalities
Even though the diagnosis of PH relies on right heart catheterization, noninvasive imaging plays a pivotal role in the PH assessment, aiming to evaluate the heart, lung parenchyma, airways, pulmonary vasculature, and mediastinum, as well as suggest critical diagnostic and prognostic information. Table 3 provides a synoptic overview of the strengths and limitations of the main imaging modalities.
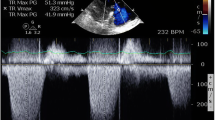
Current guidelines recommend transthoracic echocardiography (TTE) as the first-line, noninvasive imaging investigation when suspecting PH [1]. Indeed, regardless of the underlying cause, PH leads to echocardiography-detectable right ventricle (RV) pressure overload and dysfunction. Notably, echocardiography allows defining the probability of PH (low, intermediate, or high), thus prompting further investigation, including cardiac catheterization. Furthermore, TTE provides a reproducible assessment of potential left heart causes of PH, including valvular disease, left ventricle (LV) systolic or diastolic dysfunction, congenital heart disease (CHD), and intra-cardiac shunts [10]. Besides conventional TTE, speckle-tracking strain imaging and 3D echocardiography are gaining ground in monitoring right heart structure and function [11]. The assessment of RV systolic pressure is obtained with the tricuspid regurgitation jet velocity and size/collapsibility of the inferior vena cava [12]. In selected patients, transesophageal echocardiography (TEE) may further ambiguous findings, e.g., mitral valve disease, ultimately refining the patient treatment [10].
Chest radiography (CXR) is the first-line imaging modality in patients with PH, stating that presenting symptoms, such as dyspnea, are usually nonspecific. Albeit unhelpful in mild PH, CXR demonstrates high sensitivity and specificity in detecting moderate to severe PH [13]. Indeed, CXR findings can suggest PH, e.g., central PAs with or without peripheral pruning, and right heart chambers enlargement [14], while certain abnormalities can elicit the suspicion of specific PH groups, e.g., left heart chambers’ enlargement, gross valve calcification, and pulmonary venous congestion suggest group II; interstitial fibrosis, bronchiectasis changes or extensive emphysema suggest group III; the Hampton's hump, i.e., wedge-shaped, pleural-based opacification due to pulmonary infarction, and the Westermark sign, i.e., focal peripheral hyperlucency due to oligemia resulting in a collapsed appearance of vessels distal to the occlusion, suggest group IV [15].
Cardiac Magnetic Resonance Imaging (CMRI) is the gold standard in evaluating RV size and function, allowing highly reproducible tissue characterization and distinguishing ischemic perfusion from fibrotic processes [16]. Furthermore, it provides high-resolution 3D volumetric visualization of the RH, allowing identification of congenital cardiac abnormalities and quantification of blood flow, and helps recognize regurgitant valvular flow and the relationship between RV and LV [17].
Radionuclide ventilation–perfusion scanning (V/Q) is pivotal in ruling out or detecting CTEPH in patients with suspected or newly diagnosed PH, stating > 90% sensitivity and specificity [1, 18]. V/Q is performed with gas (Xe133), aerosolized droplets (Technetium 99 M, DTPA/MDP/Sulphur colloid) or carbon particles (Technegas) for the ventilation phase, and Technetium labeled macro-aggregated albumin for the perfusion phase [19]. A segmental mismatched perfusion defect with preserved ventilation to the corresponding regions at V/Q in PH patients defines CTEPH. Nevertheless, V/Q can display nonmatched perfusion defects in up to 10% of patients with PAH (including PVOD/PCH) [20]. Therefore, a high probability V/Q in patients with PH does not always correspond to CTEPH.
The role of chest CT in the noninvasive work-up
Non-contrast CT (NCT)
Non-contrast CT (NCT) can provide valuable information in patients with unexplained dyspnea and suspected PH, as well as in patients with confirmed PH to help diagnose group I, III, or V PH. Concerning group I PH, NCT can detect indirect signs of PH resulting from pulmonary microvasculopathy, such as centrilobular micronodules, peripheral neovascularization, and areas of ground-glass attenuation [21]. NCT may also suggest PVOD/PCH when distinguishing imaging features are present, i.e., centrilobular ground-glass opacities, interlobular septa thickening, and mediastinal lymphadenopathy, particularly when these findings coexist [22, 23]. Moreover, NCT can detect lung fibrosis or emphysema, thus pointing toward group III PH, as well as signs of sarcoidosis, pulmonary Langerhans cell histiocytosis, and neurofibromatosis, raising the suspicion of group V PH.
Pulmonary CT angiography (CTPA)
The key benefit of pulmonary CT angiography (CTPA) is helping diagnose CTEPH via several direct and indirect signs, including thrombus within the vascular walls, bands in the PAs, filling defects, mosaic perfusion, and hypertrophic bronchial arteries. CTPA can also depict cardiovascular abnormalities such as intra-cardiac shunts, abnormal pulmonary venous return, patent ductus arteriosus, and pulmonary arteriovenous malformation [1]. Additionally, CTPA can suggest PH when revealing PA dilatation (> 30 mm), a PA-to-aorta ratio higher than 0.9, enlarged right heart chambers, RV wall thickness ≥ 6 mm, RV/LV ratio higher than 1, and septal deviation ≥ 140° [24].
Dual-energy CT angiography (DECTA)
Dual-energy CT angiography (DECTA) enables displaying pulmonary "perfusion" maps derived from the iodine content within the pulmonary vasculature, enabling noninvasive analysis of lung microcirculation [25]. DECTA demonstrated excellent agreement with V/Q in diagnosing CTEPH [26], with higher accuracy, reduced radiation exposure, and concurrent lung and heart morphology assessment [27]. DECTA proved high sensitivity in predicting the disease level of CTEPH, distinguishing between proximal and distal disease, thereby providing valuable road-mapping for pulmonary endarterectomy aimed at improving hemodynamics [28]. Notably, DECTA-derived pulmonary perfusion patterns enable differentiating acute pulmonary embolism and CTEPH [20, 29], thus helping in CTEPH early diagnosis. Moreover, DECTA can detect perfusion changes in a small proportion of group I PH, including idiopathic PAH and PVOD/PCH [30]. The perfusion patterns of PAH considerably differ from peripheral CTEPH, being almost exclusively patchy and homogeneous in the former and patchy or pulmonary embolism type in the latter [31, 32].
Per-chest compartment analysis of CT findings in PH
We hereafter resume typical chest CT findings in PH according to the most involved chest compartment, i.e., lung, heart, pulmonary vessels, and mediastinum. Table 4 resumes some of the most frequent clinical conditions associated with PH and the corresponding CT imaging findings.
Lung
Several CLDs can cause PH, including those of group III PH (interstitial lung diseases, chronic obstructive pulmonary disease [COPD], and combined pulmonary fibrosis and emphysema [CPFE]) and group V PH (sarcoidosis, pulmonary Langerhans' cell histiocytosis, and neurofibromatosis type 1) [33]. Chest CT is paramount in detecting PH-related lung findings, including signs of emphysema and/or airway disease, interstitial lung disease and fibrosis, centrilobular nodules, interlobular septal thickening, subpleural peripheral opacities, and mosaic attenuation pattern [24, 34].
Emphysema and airway disease
Permanent enlargement of airspaces beyond the terminal bronchioles and destruction of alveolar walls define lung emphysema (Fig. 2a) [22, 35]. Along with emphysema, chest CT can display signs of airway disease, including bronchial wall thickening of the central airways and distal airway changes such as tree-in-bud opacities, centrilobular micronodules, air trapping, bronchiolectasis, and oligemia. Different combinations of such findings mirror conditions that lead to functional irreversible airflow limitation in the framework of COPD [36]. PH frequently complicates COPD, with a prevalence approximating 40% of patients and much higher in end-stage disease, with the majority presenting with mild-to-moderate PH [37]. Hence, assessing CT signs of emphysema and airway disease in patients with suspected/established PH is crucial. It is essential to emphasize that, since COPD is a common condition in the general population, in patients with coexisting PH, a comprehensive clinical, imaging, and functional assessment is mandatory to ascertain if PH results from COPD or it is due to a coincident non-group III etiology [38].
Interstitial lung disease and fibrosis
Interstitial lung disease (ILD) is an umbrella term indicating a broad, heterogeneous group of lung conditions sharing restrictive physiology and impaired gas exchange, albeit with highly variable causes and pathological, clinical, and imaging features. Connective tissue disease-related interstitial lung disease (CTD-ILD), idiopathic pulmonary fibrosis (IPF), chronic hypersensitivity pneumonitis, pulmonary Langerhans cell histiocytosis, and sarcoidosis are the ILDs that most commonly complicate with PH [39]. Other conditions include combined pulmonary fibrosis and emphysema (CPFE) and LAM [1]. Notably, all the above-mentioned ILD-related PH conditions belong to group III except sarcoidosis and pulmonary Langerhans cell histiocytosis, which fall under group V due to their multifactorial nature. They all share general pathophysiology mechanisms, including alveolar hypoxia, reactive vasoconstriction, and various parenchymal and vascular remodeling processes, ultimately leading to PH (Fig. 2a) [39].
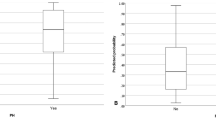
From a practical viewpoint, CT detection and quantification of ILD extent is essential, irrespective of the PH group. Indeed, mild parenchymal lung changes (i.e., fibrosis and/or emphysema) in patients with idiopathic PAH are associated with worse survival [40], probably identifying a distinct PH phenotype of idiopathic PAH closer to group II PH [41]. Moreover, among patients with SSc-related PH, those with extensive ILD (i.e., CT extent > 30%) are associated with worse survival than those with PAH and low DLCO but no or limited ILD [42, 43].
Centrilobular ground-glass nodules
Centrilobular ground-glass nodules (CGGN) represent an easily overlooked but typical pulmonary finding in patients with PH (Fig. 2b). Ill-defined CGGN are common in PAH, presumably reflecting cholesterol granulomas, hemorrhage, or plexogenic arterial lesions. CGGN can also be present in patients with long-standing left-to-right heart shunt and, most importantly, in various ILD, including subacute hypersensitivity pneumonitis and smoking-related respiratory bronchiolitis [44]. Notably, a correct interpretation of CGGN is crucial. Indeed, when CGGN presents as isolated in the framework of idiopathic PAH, it is not associated with lower DLCO nor worse survival [45]. On the contrary, the situation is much different when CGGN is part of an ILD or reflects PVOD/PCH, carrying the risk of aggravated prognosis.
Interlobular septal thickening
The morphology of interlobular septal thickening can help group PH. Indeed, smooth, irregular, and nodular thickening points toward group II PH (i.e., LHD, Fig. 2c), group III PH (lung fibrosis), or group V PH (sarcoidosis, fibrosing mediastinitis), respectively. In the absence of signs of LHD or ILD, interlobular septal thickening may mirror the postcapillary congestion typical of patients with PVOD/PHC, prompting the search for accoupling CGGN and mediastinal lymph-node enlargement.
Subpleural peripheral opacities
Nonspecific, subpleural peripheral bands or consolidation areas resembling parenchymal scars can frequently be encountered in CTEPH (Fig. 2d) [46], thus prompting careful evaluation of PAs (see further in the text).
Mosaic attenuation pattern
The mosaic attenuation pattern is present in nearly 20% of patients with PH [47]. While possible in all the PH clinical groups, its distribution tends to be heterogeneous or patchy, perivascular in idiopathic PAH, and segmental and well defined in CTEPH [48].
Heart
Technological advances in chest CT acquisition, mainly related to high temporal resolution, make first-hand heart and coronary artery imaging feasible. Indeed, various cardiac findings are detectable on non-ECG-gated CT scans, including cardiac shunts, coronary and valvular calcifications, and chamber enlargement [49, 50].
Congenital heart diseases
PH can develop in patients with CHDs due to pulmonary over-circulation (left-to-right shunt, from systemic to pulmonary circulation), falling under group I PH. Several CHD characterized by chronic and untreated pulmonary over-circulation can ultimately lead to Eisenmenger Syndrome (ES), i.e., the progressive development of pulmonary vasculopathy (increased PVR) with reversal of shunt flow (from right-to-left or bidirectional) [51]. Examples include atrial septal defects, partial anomalous pulmonary venous return, ventricular septal defects, and patent ductus arteriosus. Notably, patients with large post-tricuspid defects and complex anatomical lesions and/or those associated with trisomy 21 are at higher risk of early PH development [52]. Less frequently, PH may complicate obstructive left heart lesions, thus falling under group II PH [1]. Patients who undergo radical correction at a later age, or partially corrective intervention only, may complicate with PH even when the CHD is associated with small defects/shunts [1].
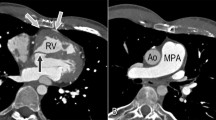
CT is crucial in investigating PAH associated with congenital heart disease, providing detailed information on cardiac chambers, great arteries, pulmonary vasculature, parenchyma, and mediastinal structures in a single acquisition with high spatial resolution (Fig. 3a). This is particularly beneficial when acoustic windows are limited (constraining echocardiography), in case of lung disease, or when patients cannot undergo MRI. Communication between chambers can be visualized, and shunt direction can be inferred from the contrast flow. CTPA is the preferred noninvasive method for evaluating proximal and distal PAs, identifying PA dilation and in-situ thrombus formation due to sluggish blood flow. CT excels in assessing extracardiac features, notably native or surgically created systemic-to-pulmonary shunts [53].
Heart CT findings in pulmonary hypertension. a 3D volume rendering image of the heart and pulmonary vessels showing adulthood-discovered congenital malformation with inferior vena cava draining into the left atrium (LA). b LA enlargement. How to measure the LA anteroposterior diameter is reported (double-sided arrow). c Left coronary artery calcification (arrow). d. Aortic valve calcification (arrow)
Left atrium enlargement
The close correlation between LA enlargement and group II PH is well established. Previous studies found an excellent diagnostic accuracy of CTPA-derived LA diameter and area, thus distinguishing patients with group II PH from those with non-group II PH [17, 54,55,56]. The LA diameter should be the largest anterior–posterior diameter on the slice in the middle 50% of the LA craniocaudal extension (Fig. 3b) [57]. LA area can be calculated through manual or automatic segmentation [57].
Coronary artery and valvular calcification
LHD causes backpressure and increases the hydrostatic pressure in the pulmonary veins, eventually resulting in increased pressure in PAs [58].
Aortic or mitral valvular thickening and calcification can indicate valvular stenosis, the calcification degree correlating with the valvular stenosis severity [59]. Valvular calcification can be identified as high-attenuation material in the aortic valve and mitral region. Concerning the aortic valve, care should be taken to differentiate valve calcification from calcification in the aortic root, mitral annulus, or coronary (Fig. 3c) [60].
Coronary artery calcification can be identified as high-attenuation material in the path of a coronary artery (Fig. 3d). For non-gated thoracic CT in routine clinical practice, a simple visual ordinal score performed on a whole-patient basis has been recommended [60].
Pulmonary vessels
Identifying CT signs about pulmonary vessels helps recognize group IV PH, mostly CTEPH (Fig. 4). Other causes of pulmonary vascular obstruction, such as malignant tumors (sarcomas, renal carcinoma, uterine carcinoma, germ-cell tumors of the testis), arteritis without connective tissue disease, and congenital pulmonary arterial stenosis, are far less common and described elsewhere [1].
Pulmonary vessel CT findings in pulmonary hypertension. a Chronic, non-occlusive thrombi in pulmonary arteries (arrow). b Mosaic attenuation pattern reflecting oligemia. c. Pulmonary artery branch abruption, abnormal tapering, and corkscrewing. d Right hypertrophic bronchial artery (red arrow). c, d Thin-slab MIP coronal reformatted images show pulmonary artery branch abruption, abnormal tapering, and corkscrewing (c), and right hypertrophic bronchial artery (arrow in d)
Signs of chronic thromboembolic pulmonary disease
Chronic thromboembolic pulmonary disease (CTEPD) refers to symptomatic patients due to post-thromboembolic fibrotic obstructions within the PA, with or without PH [1]. CTEPD patients typically exhibit mismatched perfusion defects on V/Q and signs of chronic, organized, fibrotic clots on CTPA or angiography after at least three months of therapeutic anticoagulation, including ring-like stenoses, webs/slits, and chronic total occlusions (pouch lesions or tapered lesions) [1]. CTEPH is the preferred term for patients with CTEPD complicating with PH. In 0.6–4.4% of acute PE, abnormal, persistent residual thromboembolic occlusion, combined with a variable degree of microscopic vasculopathy, leads to CTEPH [61, 62]. If untreated, CTEPH can ultimately evolve into right heart failure [21].
Imaging modalities to assess CTEPH include echocardiography, V/Q, CTPA, and right heart catheterization with pulmonary angiography [63]. Typical CTPA findings include signs of non-occlusive and occlusive chronic thrombi [64]. Non-occlusive thrombi present as linear filling defects, forming bands across the PAs and creating webs; alternatively, they may appear as eccentric thrombi with an obtuse vessel wall margin (Fig. 4a). Occlusive chronic thrombi occlude the vessel lumen, causing vascular constriction (unlike acute thrombi, which enlarge the vessel). PA branch abruption, abnormal tapering, and corkscrewing are other frequent CTEPH findings (Fig. 4b) [64].
Mosaic attenuation CT pattern is a crucial, indirect sign of CTEPH [65]. Vessel narrowing results in hypoperfused lung areas, appearing as well-defined abnormally hypodense regions alternating with abnormally hyperdense areas, with patchy distribution, reflecting vascular perfusion differences (Fig. 4c). Indeed, patent vessels resulting in increased blood flow supply the hyperdense areas, while the hypodense areas are located distal to vascular narrowing/occlusion. Small airway disease (SAD) is another cause of mosaic attenuation CT pattern due to hypoxic vasoconstriction. While large airway wall thickening in the hypodense areas is a frequent SAD-associated finding, patients with CTEPH typically exhibit peripheral scarring resulting from previous infarctions, thus helping differentiate the two conditions [64].
Collateral circulation develops in CTEPH, likely due to increased vascular resistance and blood flow blockages. Consequently, enlarged, tortuous bronchial artery collaterals running through the mediastinum into the hila are frequent findings, particularly in areas affected by obstruction (Fig. 4d). Although these collateral vessels assist in sustaining perfusion to lung tissue beyond thrombotic blockages, the exposure of the pulmonary circulation to the elevated pressure values of the systemic circulation can induce vascular remodeling and, in turn, arteriopathy [66].
Right-ventricular hypertrophy is frequently encountered in long-standing PH. Notably, right atrial dilatation coexists and is detectable at CT in many patients with CTEPH due to a combination of elevated right heart pressures and right ventricular dilatation conditioning functional tricuspid regurgitation [64].
Mediastinum
Along with pulmonary, cardiac, and vascular signs, several mediastinal findings can help diagnose and group PH. We focus on three abnormalities we frequently encounter when dealing with PH, which are lymph-node enlargement, esophageal dilatation, and signs of portal hypertension.
Lymph-node enlargement
Conventionally, a short-axis cut-off of 10 mm defines an enlarged lymph node (LN) [67]. Enlarged mediastinal LNs are a frequent CT finding, lacking specificity. It can be encountered in many different PH-related pathologies pertaining to all five clinical groups. Indeed, mediastinal LN enlargement is common in group II PH and has been reported in 45% of patients with CTEPH, possibly due to right-sided failure and increased lymphatic flow [68]. Nevertheless, a couple of conditions worth mentioning, including sarcoidosis and PVOD/PCH.
Symmetric LN enlargement at stations 4R, 7, 11L, and 11R in sarcoidosis defines the classical Garland's triad (Fig. 5a, b). LNs typically present focal, eggshell, or icing sugar calcifications [69]. It has been supposed that enlarged LNs can determine pulmonary vascular compression or extrinsic stenoses, thus restricting blood flow and, ultimately, causing PH [70]. It must be pointed out that the pathophysiology of sarcoidosis-associated PH is multifactorial, which is why it pertains to group V PH. Indeed, several other mechanisms have been hypothesized, including advanced lung parenchyma involvement, cardiac sarcoidosis-inducing systolic/diastolic LV dysfunction, PVOD/PCH, higher risk of thromboembolic disease, and sarcoidosis-triggered vascular granulomatous inflammation [71].
In PVOD/PCH, mediastinal LN enlargement is present in up to 84% of cases [72]. It probably derives from venous congestion, veno-lymphatic shunts, and angiogenetic factors typically encountered in this condition [73, 74]. Albeit such enlarged LNs have no specific station location, when associated with centrilobular ground-glass opacities and interlobular septa smooth thickening, they are highly suggestive of PVOD/PCH [75].
Esophageal dilatation
An axial diameter cut-off value > 10 mm at the carina level or a maximum diameter > 15 mm defines esophageal dilatation [76]. The dilatation of the lower two-thirds of the esophagus, particularly below the level of the aortic arch, suggests systemic sclerosis (SSc) (Fig. 5c) [77]. In patients with SSc, esophageal smooth muscle becomes atrophic, with replacing fibrous tissue leading to severe dysmotility, dilatation, and absent peristalsis [78]. Esophageal abnormalities have been implicated in SSc-related ILD development. In patients with known/suspected PH, the association of esophageal dilatation and ILD should raise the suspicion of SSc-related PH, thus prompting further tests [79].
Signs of portal hypertension
Persistent portal hypertension leads to the development of portosystemic collaterals. CT displays varices as distinct, round, tubular, or winding structures exhibiting smooth, homogeneous attenuation and enhancing to a similar degree as portal and mesenteric veins after contrast injection [80, 81]. Mediastinal varices include (i) esophageal veins, presenting with nodular thickening of the esophageal wall and enhancing nodular intraluminal protrusions with scalloped borders near the esophageal hiatus (Fig. 5d); (ii) paraoesophageal veins, manifesting as dilated collateral vessels encircling the esophagus and descending thoracic aorta; (iii) pericardiophrenic veins, which are dilated veins in the cardiophrenic angle, often associated with cirrhosis due to inferior vena cava membranous obstruction [81]. The presence of these mediastinal signs, along with other indicators such as other dilated collateral vessels, nodular and shrunken liver, ascites, and splenomegaly, supports the suspicion of portal hypertension-associated PAH, also known as portopulmonary hypertension [82].
Conclusion
PH is a complex condition encompassing a broad range of different clinical scenarios, thus requiring multidisciplinary interaction to prompt adequate diagnosis, risk stratification, and management. The crucial and constantly evolving role of chest CT in the noninvasive work-up of patients with known or suspected PH mandates adequate knowledge of typical and less frequent CT findings to adequately interpret them and valuably contribute to the PH multidisciplinary clinical discussion.
Abbreviations
- CGGN:
-
Centrilobular ground-glass nodules
- CHD:
-
Congenital heart disease
- CLD-PH:
-
Chronic lung disease-related PH
- CMRI:
-
Cardio magnetic resonance imaging
- COPD:
-
Chronic obstructive pulmonary disease
- CpcPH:
-
Combined pre- and postcapillary PH
- CT:
-
Computed tomography
- CTD:
-
Connective tissue disease
- CTEPD:
-
Chronic thromboembolic pulmonary disease
- CTEPH:
-
Chronic thrombo-embolic pulmonary hypertension
- CPFE:
-
Combined pulmonary fibrosis and emphysema
- CPTA:
-
CT pulmonary angiography
- DECTA:
-
Dual-energy CT angiography
- DTPA:
-
Diethylenetriamine pentaacetate
- ES:
-
Eisenmenger Syndrome
- ESC:
-
European Society of Cardiology
- ESR:
-
European Respiratory Society
- HIV:
-
Human immunodeficiency virus
- ILD:
-
Interstitial lung disease
- IpcPH:
-
Isolated postcapillary PH
- IPF:
-
Idiopathic pulmonary fibrosis
- LA:
-
Left atrial
- LAM:
-
Lymphangioleiomyomatosis
- LHD:
-
Left heart disease
- LV:
-
Left ventricle
- MDP:
-
Methyl diphosphonate
- mPAP:
-
Mean pulmonary arterial pressure
- MRI:
-
Magnetic resonance imaging
- NCT:
-
Non-contrast CT
- PA:
-
Pulmonary artery
- PAH:
-
Pulmonary arterial hypertension
- PAP:
-
Pulmonary arterial pressure
- PAWP:
-
Pulmonary Artery Wedge Pressure
- PH:
-
Pulmonary hypertension
- PH-LHD:
-
PH associated with left heart disease
- PVOD:
-
Pulmonary veno-occlusive disease
- PCH:
-
Pulmonary capillary hemangiomatosis
- PVR:
-
Pulmonary vascular resistance
- RV:
-
Right ventricle
- SAD:
-
Small airway disease
- SSc:
-
Systemic sclerosis
- V/Q:
-
Ventilation/perfusion
- TEE:
-
Transesophageal echocardiography
- TTE:
-
Transthoracic echocardiography
- WU:
-
Wood units
References
Humbert M, Kovacs G, Hoeper MM et al (2023) 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J 61:2200879. https://doi.org/10.1183/13993003.00879-2022
Kularatne M, Gerges C, Jevnikar M et al (2024) Updated clinical classification and hemodynamic definitions of pulmonary hypertension and its clinical implications. J Cardiovasc Dev Dis 11(3):78. https://doi.org/10.3390/jcdd11030078
Condon DF, Nickel NP, Anderson R et al (2019) The 6th World Symposium on Pulmonary Hypertension: what’s old is new. F1000Res. 8:F1000. https://doi.org/10.12688/f1000research.18811.1
Pieske B, Tschöpe C, de Boer RA et al (2019) How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur Heart J 40(40):3297–3317. https://doi.org/10.1093/eurheartj/ehz641
Anderson JJ, Lau EM (2022) Pulmonary hypertension definition, classification, and epidemiology in Asia. JACC Asia 2(5):538–546. https://doi.org/10.1016/j.jacasi.2022.04.008
Cullivan S, Gaine S, Sitbon O (2023) New trends in pulmonary hypertension. Eur Respir Rev 32(167):220211. https://doi.org/10.1183/16000617.0211-2022
Cansu DÜ, Korkmaz C (2023) Pulmonary hypertension in connective tissue diseases: epidemiology, pathogenesis, and treatment. Clin Rheumatol 42(10):2601–2610. https://doi.org/10.1007/s10067-022-06446-y
Delhaye C, Walsdorff M, Hackx M (2020) Case 276: pulmonary veno-occlusive disease and pulmonary capillary hemangiomatosis disease. Radiology 295(1):240–244. https://doi.org/10.1148/radiol.2020180473
McGettrick M, Peacock A (2020) Group 3 pulmonary hypertension: challenges and opportunities. Glob Cardiol Sci Pract. 2020(1):202006. https://doi.org/10.21542/gcsp.2020.6
Sharma M, Burns AT, Yap K et al (2021) The role of imaging in pulmonary hypertension. Cardiovasc Diagn Ther 11(3):859–880. https://doi.org/10.21037/cdt-20-295
Farrell C, Balasubramanian A, Hays AG et al (2022) A clinical approach to multimodality imaging in pulmonary hypertension. Front Cardiovasc Med 18(8):794706. https://doi.org/10.3389/fcvm.2021.794706
Austin C, Alassas K, Burger C et al (2015) Echocardiographic assessment of estimated right atrial pressure and size predicts mortality in pulmonary arterial hypertension. Chest 147(1):198–208. https://doi.org/10.1378/chest.13-3035
Miniati M, Monti S, Airò E et al (2014) Accuracy of chest radiography in predicting pulmonary hypertension: a case-control study. Thromb Res 133(3):345–351. https://doi.org/10.1016/j.thromres.2013.12.019
McCann C, Gopalan D, Sheares K et al (2012) Imaging in pulmonary hypertension, part 1: clinical perspectives, classification, imaging techniques and imaging algorithm. Postgrad Med J 88(1039):271–279. https://doi.org/10.1136/postgradmedj-2011-130292
Shahul HA, Manu MK, Mohapatra AK (2019) Hampton’s hump, Westermark’s sign and Palla’s sign in acute pulmonary thromboembolism: a rare concurrence. BMJ Case Rep 12(9):e231693. https://doi.org/10.1136/bcr-2019-231693
von Knobelsdorff-Brenkenhoff F, Schulz-Menger J (2023) Cardiovascular magnetic resonance in the guidelines of the European Society of Cardiology: a comprehensive summary and update. J Cardiovasc Magn Reson 25(1):42. https://doi.org/10.1186/s12968-023-00950-z
van de Veerdonk MC, Roosma L, Trip P et al (2024) Clinical-imaging-pathological correlation in pulmonary hypertension associated with left heart disease. Eur Respir Rev 33(171):230144. https://doi.org/10.1183/16000617.0144-2023
Konstantinides SV, Meyer G, Becattini C et al (2019) 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur Respir J 54:1901647. https://doi.org/10.1183/13993003.01647-2019
Metter D, Tulchinsky M, Freeman LM (2017) Current status of ventilation–perfusion scintigraphy for suspected pulmonary embolism. AJR Am J Roentgenol 208:489–494. https://doi.org/10.2214/AJR.16.17195
Seferian A, Helal B, Jaïs X et al (2012) Ventilation/perfusion lung scan in pulmonary veno-occlusive disease. Eur Respir J 40(1):75–83. https://doi.org/10.1183/09031936.00097911
Remy-Jardin M, Ryerson CJ, Schiebler ML et al (2021) Imaging of pulmonary hypertension in adults: a position paper from the Fleischner Society. Eur Respir J 57(1):2004455. https://doi.org/10.1183/13993003.04455-2020
Resten A, Maitre S, Humbert M et al (2004) Pulmonary hypertension: CT of the chest in pulmonary veno-occlusive disease. AJR Am J Roentgenol 183:65–70. https://doi.org/10.2214/ajr.183.1.1830065
Ali N, Loughborough WW, Rodrigues JCL et al (2019) Computed tomographic and clinical features of pulmonary veno-occlusive disease: raising the radiologist’s awareness. Clin Radiol 74(9):655–662. https://doi.org/10.1016/j.crad.2019.04.023
Altschul E, Remy-Jardin M, Machnicki S et al (2019) Imaging of Pulmonary Hypertension: Pictorial Essay. Chest 156(2):211–227. https://doi.org/10.1016/j.chest.2019.04.003
Moore J, Remy J, Altschul E et al (2024) Thoracic applications of spectral CT scan. Chest 165(2):417–430. https://doi.org/10.1016/j.chest.2023.07.4225
Masy M, Giordano J, Petyt G et al (2018) Dual-energy CT (DECT) lung perfusion in pulmonary hypertension: concordance rate with V/Q scintigraphy in diagnosing chronic thromboembolic pulmonary hypertension (CTEPH). Eur Radiol 28(12):5100–5110. https://doi.org/10.1007/s00330-018-5467-2
Schüssler A, Lug Q, Kremer N et al (2023) Evaluation of diagnostic accuracy of dual-energy computed tomography in patients with chronic thromboembolic pulmonary hypertension compared to V/Q-SPECT and pulmonary angiogram. Front Med (Lausanne) 22(10):1194272. https://doi.org/10.3389/fmed.2023.1194272
Eberhard M, McInnis M, de Perrot M et al (2022) Dual-energy CT pulmonary angiography for the assessment of surgical accessibility in patients with chronic thromboembolic pulmonary hypertension. Diagnostics (Basel) 12(2):228. https://doi.org/10.3390/diagnostics12020228
Gertz RJ, Gerhardt F, Pienn M et al (2023) Dual-layer dual-energy CT-derived pulmonary perfusion for the differentiation of acute pulmonary embolism and chronic thromboembolic pulmonary hypertension. Eur Radiol. https://doi.org/10.1007/s00330-023-10337-4
Vlahos I, Jacobsen MC, Godoy MC et al (2022) Dual-energy CT in pulmonary vascular disease. Br J Radiol 95(1129):20210699. https://doi.org/10.1259/bjr.20210699
Lefebvre B, Kyheng M, Giordano J et al (2022) Dual-energy CT lung perfusion characteristics in pulmonary arterial hypertension (PAH) and pulmonary veno-occlusive disease and/or pulmonary capillary hemangiomatosis (PVOD/PCH): preliminary experience in 63 patients. Eur Radiol 32(7):4574–4586. https://doi.org/10.1007/s00330-022-08577-x
Giordano J, Khung S, Duhamel A et al (2017) Lung perfusion characteristics in pulmonary arterial hypertension (PAH) and peripheral forms of chronic thromboembolic pulmonary hypertension (pCTEPH): Dual-energy CT experience in 31 patients. Eur Radiol 27(4):1631–1639. https://doi.org/10.1007/s00330-016-4500-6
Valentini A, Franchi P, Cicchetti G et al (2023) Pulmonary hypertension in chronic lung diseases: what role do radiologists play? Diagnostics (Basel) 13(9):1607. https://doi.org/10.3390/diagnostics13091607
Aluja Jaramillo F, Gutierrez FR, Díaz Telli FG et al (2018) Approach to pulmonary hypertension: from CT to clinical diagnosis. Radiographics. 38(2):357–373. https://doi.org/10.1148/rg.2018170046
Bankier AA, MacMahon H, Colby T et al (2024) Fleischner Society: glossary of terms for thoracic imaging. Radiology 310(2):e232558. https://doi.org/10.1148/radiol.232558
Coste F, Benlala I, Dournes G et al (2019) Assessing pulmonary hypertension in COPD. Is there a role for computed tomography? Int J Chron Obstruct Pulmon Dis. 14:2065–2079. https://doi.org/10.2147/COPD.S207363
Zhang L, Liu Y, Zhao S et al (2022) The incidence and prevalence of pulmonary hypertension in the COPD population: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 10(17):1365–1379. https://doi.org/10.2147/COPD.S359873
Seeger W, Adir Y, Barberà JA et al (2013) Pulmonary hypertension in chronic lung diseases. J Am Coll Cardiol 62(25 Suppl):D109–D116. https://doi.org/10.1016/j.jacc.2013.10.036
Dhont S, Zwaenepoel B, Vandecasteele E et al (2022) Pulmonary hypertension in interstitial lung disease: an area of unmet clinical need. ERJ Open Res 8(4):00272–02022. https://doi.org/10.1183/23120541.00272-2022
Lewis RA, Thompson AAR, Billings CG et al (2020) Mild parenchymal lung disease and/or low diffusion capacity impacts survival and treatment response in patients diagnosed with idiopathic pulmonary arterial hypertension. Eur Respir J 55(6):2000041. https://doi.org/10.1183/13993003.00041-2020
Godinas L, Harari S, Barberà JA et al (2020) Mild parenchymal lung disease is still lung disease. Eur Respir J 56(5):2003542. https://doi.org/10.1183/13993003.03542-2020
Launay D, Montani D, Hassoun PM et al (2018) Clinical phenotypes and survival of pre-capillary pulmonary hypertension in systemic sclerosis. PLoS ONE 13(5):e0197112. https://doi.org/10.1371/journal.pone.0197112
Morrisroe K, Hansen D, Stevens W et al (2024) Predictors and prognosis of pulmonary hypertension complicating interstitial lung disease in systemic sclerosis. Rheumatology (Oxford). https://doi.org/10.1093/rheumatology/keae166
Lewis G, Hoey ET, Reynolds JH et al (2015) Multidetector CT assessment in pulmonary hypertension: techniques, systematic approach to interpretation and key findings. Quant Imaging Med Surg 5(3):423–432. https://doi.org/10.3978/j.issn.2223-4292.2015.01.05
Dwivedi K, Condliffe R, Sharkey M et al (2022) Computed tomography lung parenchymal descriptions in routine radiological reporting have diagnostic and prognostic utility in patients with idiopathic pulmonary arterial hypertension and pulmonary hypertension associated with lung disease. ERJ Open Res 8(1):00549–02021. https://doi.org/10.1183/23120541.00549-2021
Capone C, Valentini A, Spinillo SL et al (2021) Radiological differences between chronic thromboembolic pulmonary disease (CTEPD) and chronic thromboembolic pulmonary hypertension (CTEPH). Eur Radiol 31(8):6230–6238. https://doi.org/10.1007/s00330-020-07556-4
Ussavarungsi K, Lee AS, Burger CD (2015) Mosaic pattern of lung attenuation on chest CT in patients with pulmonary hypertension. Diseases 3(3):205–212. https://doi.org/10.3390/diseases3030205
Ridge CA, Bankier AA, Eisenberg RL (2011) Mosaic attenuation. AJR Am J Roentgenol 197(6):W970–W977. https://doi.org/10.2214/AJR.11.7067
Krueger M, Cronin P, Sayyouh M et al (2019) Significant incidental cardiac disease on thoracic CT: what the general radiologist needs to know. Insights Imaging 10(1):10. https://doi.org/10.1186/s13244-019-0693-y
Secchi F, Di Leo G, Zanardo M et al (2017) Detection of incidental cardiac findings in noncardiac chest computed tomography. Medicine (Baltimore) 96(29):e7531. https://doi.org/10.1097/MD.0000000000007531
Chaix MA, Gatzoulis MA, Diller GP et al (2019) eisenmenger syndrome: a multisystem disorder-do not destabilize the balanced but fragile physiology. Can J Cardiol 35(12):1664–1674. https://doi.org/10.1016/j.cjca.2019.10.002
Lammers AE, Stegger J, Koerten MA et al (2021) secundum type atrial septal defect in patients with trisomy 21-therapeutic strategies, outcome, and survival: a Nationwide Study of the German National Registry for Congenital Heart Defects. J Clin Med 10(17):3807. https://doi.org/10.3390/jcm10173807
Piggott KD, Nykanen DG, Smith S (2011) Computed tomography angiography successfully used to diagnose postoperative systemic-pulmonary artery shunt narrowing. Case Rep Cardiol 2011:802643. https://doi.org/10.1155/2011/802643
Currie BJ, Johns C, Chin M et al (2018) CT derived left atrial size identifies left heart disease in suspected pulmonary hypertension: Derivation and validation of predictive thresholds. Int J Cardiol 1(260):172–177. https://doi.org/10.1016/j.ijcard.2018.02.114
Jivraj K, Bedayat A, Sung YK et al (2017) Left atrium maximal axial cross-sectional area is a specific computed tomographic imaging biomarker of world health organization group 2 pulmonary hypertension. J Thorac Imaging 32(2):121–126. https://doi.org/10.1097/RTI.0000000000000252
Katikireddy CK, Singh M, Muhyieddeen K et al (2016) Left atrial area and right ventricle dimensions in non-gated axial chest CT can differentiate pulmonary hypertension due to left heart disease from other causes. J Cardiovasc Comput Tomogr. 10(3):246–50. https://doi.org/10.1016/j.jcct.2016.01.014
Lick AN, Danrad R, Smith DL et al (2017) Left atrium measurements via computed tomography pulmonary angiogram as a predictor of diastolic dysfunction. J Comput Assist Tomogr. 41(5):792–797. https://doi.org/10.1097/RCT.0000000000000597
Pahal P, Sharma S (2024) Secondary pulmonary hypertension. StatPearls Publishing, Treasure Island
Koos R, Mahnken AH, Sinha AM et al (2004) Aortic valve calcification as a marker for aortic stenosis severity: assessment on 16-MDCT. AJR Am J Roentgenol 183:1813–1818. https://doi.org/10.2214/ajr.183.6.01831813
Williams MC, Abbas A, Tirr E et al (2021) Reporting incidental coronary, aortic valve and cardiac calcification on non-gated thoracic computed tomography, a consensus statement from the BSCI/BSCCT and BSTI. Br J Radiol 94(1117):20200894. https://doi.org/10.1259/bjr.20200894
Kim NH, Delcroix M, Jais X et al (2019) Chronic thromboembolic pulmonary hypertension. Eur Respir J 53:1801915. https://doi.org/10.1183/13993003.01915-2018
Ende-Verhaar YM, Meijboom LJ, Kroft LJM et al (2019) Usefulness of standard computed tomography pulmonary angiography performed for acute pulmonary embolism for identification of chronic thromboembolic pulmonary hypertension: results of the InShape III study. J Heart Lung Transplant 38:731–738. https://doi.org/10.1016/j.healun.2019.03.003
François CJ, Schiebler ML (2016) Imaging of pulmonary hypertension. Radiol Clin North Am. 54(6):1133–1149. https://doi.org/10.1016/j.rcl.2016.05.011
Hahn LD, Amatheakis DG, Fernandes TM et al (2023) Multidisciplinary approach to chronic thromboembolic pulmonary hypertension: role of radiologists. Radiographics. 43(2):e220078. https://doi.org/10.1148/rg.220078
Ruaro B, Baratella E, Caforio G et al (2022) Chronic thromboembolic pulmonary hypertension: an update. Diagnostics (Basel) 12(2):235. https://doi.org/10.3390/diagnostics12020235
Yang J, Madani MM, Mahmud E et al (2023) Evaluation and management of chronic thromboembolic pulmonary hypertension. Chest 164(2):490–502. https://doi.org/10.1016/j.chest.2023.03.029
Iyer H, Anand A, Sryma PB et al (2021) Mediastinal lymphadenopathy: a practical approach. Expert Rev Respir Med 15(10):1317–1334. https://doi.org/10.1080/17476348.2021.1920404
Bergin CJ, Park KJ (2008) Lymph node enlargement in pulmonary arterial hypertension due to chronic thromboembolism. J Med Imaging Radiat Oncol 52(1):18–23. https://doi.org/10.1111/j.1440-1673.2007.01905.x
Bailey GL, Wells AU, Desai SR (2024) Imaging of pulmonary sarcoidosis—a review. J Clin Med 13(3):822. https://doi.org/10.3390/jcm13030822
Aluja Jaramillo F, Gutierrez FR, Díaz Telli FG et al (2018) Approach to pulmonary hypertension: from CT to clinical diagnosis. Radiographics. 38(2):357–373. https://doi.org/10.1148/rg.2018170046
Liu A, Price LC, Sharma R et al (2024) Sarcoidosis associated pulmonary hypertension. Biomedicines 12(1):177. https://doi.org/10.3390/biomedicines12010177
Pérez Núñez M, Alonso Charterina S, Pérez-Olivares C et al (2021) Radiological Findings in Multidetector Computed Tomography (MDCT) of hereditary and sporadic pulmonary veno-occlusive disease: certainties and uncertainties. Diagnostics (Basel) 11(1):141. https://doi.org/10.3390/diagnostics11010141
Thomas de Montpréville V, Dulmet E, Fadel E et al (2008) Lymph node pathology in pulmonary veno-occlusive disease and pulmonary capillary heamangiomatosis. Virchows Arch. 453(2):171–6. https://doi.org/10.1007/s00428-008-0636-3
Montani D, Lau EM, Dorfmüller P et al (2016) Pulmonary veno-occlusive disease. Eur Respir J 47(5):1518–1534. https://doi.org/10.1183/13993003.00026-2016
Montani D, Achouh L, Dorfmüller P et al (2008) Pulmonary veno-occlusive disease: clinical, functional, radiologic, and hemodynamic characteristics and outcome of 24 cases confirmed by histology. Medicine (Baltimore) 87(4):220–233. https://doi.org/10.1097/MD.0b013e31818193bb
Takekoshi D, Arami S, Sheppard TJ et al (2015) Computed tomography of the esophagus in scleroderma and lung disease. Tohoku J Exp Med 237(4):345–352. https://doi.org/10.1620/tjem.237.345
Buchanan ME, Fishman EK, Azadi JR (2023) CT evaluation of the esophagus: the role of CT imaging and ct imaging findings in diagnosing esophageal abnormalities. Curr Probl Diagn Radiol. 52(4):289–299. https://doi.org/10.1067/j.cpradiol.2023.03.002
Figueiredo AFSD, Costa JF, Matos AP et al (2021) Esophageal dilatation as a predictor of systemic sclerosis in patients with interstitial lung disease. Turk Thorac J 22(3):231–236. https://doi.org/10.5152/TurkThoracJ.2021.19162
Saygin D, Domsic RT (2019) Pulmonary arterial hypertension in systemic sclerosis: challenges in diagnosis screening and treatment. Open Access Rheumatol 27(11):323–333. https://doi.org/10.2147/OARRR.S228234
Hayashi H, Oda S, Kidoh M et al (2023) Pulmonary arterial hypertension associated with portal hypertension: noninvasive comprehensive assessment using computed tomography. Radiol Case Rep 19(2):671–674. https://doi.org/10.1016/j.radcr.2023.11.013
Bandali MF, Mirakhur A, Lee EW et al (2017) Portal hypertension: Imaging of portosystemic collateral pathways and associated image-guided therapy. World J Gastroenterol 23(10):1735–1746. https://doi.org/10.3748/wjg.v23.i10.1735
Jasso-Baltazar EA, Peña-Arellano GA, Aguirre-Valadez J et al (2023) Porto-pulmonary hypertension: an updated review. Transplant Direct 9(8):e1517. https://doi.org/10.1097/TXD.0000000000001517
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization: Lorenzo Cereser and Luigi Nardone. Data curation: All authors. Project administration: Lorenzo Cereser. Resources: all authors. Writing—review & editing: all authors.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest,
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nardone, L., Minichetti, P., Sauro, S.L. et al. Noninvasive assessment of pulmonary hypertension: key insights to maximize chest computed tomography. J Med Imaging Intervent Radiol 11, 9 (2024). https://doi.org/10.1007/s44326-024-00010-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44326-024-00010-5