Abstract
Patients awaiting surgical procedures often experience obvious anxiety due to discomfort and uncertain events, which is one of the most common clinical manifestations in perioperative patients. Numerous studies have confirmed that preoperative anxiety is closely related to the occurrence of postoperative adverse events, such as insomnia, pain, nausea and vomiting and neurocognitive dysfunction. Appropriate intervention or treatment for preoperative anxiety may contribute to reducing the incidence of postoperative adverse events. Although people have long known about the negative effects of preoperative anxiety and have taken certain measures, the underlying mechanism has yet to be fully elucidated. In this paper, we focus on several typical postoperative adverse events that are, particularly concerning to anesthesiologists, review their relationships with preoperative anxiety, describe the intervention strategies and provide a certain summary and outlook.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Preoperative anxiety is generally described as a state of discomfort or tension caused by disease, the ward environment, or worries about anesthesia and surgery before the operation; this state is often accompanied by somatic manifestations such as palpitations, dyspnea, sweating, frequent urination, abdominal pain, diarrhea or sleep disturbance [1]. The overall prevalence of preoperative anxiety varies widely from 11% to 80% in adult patients and is higher in women than in men [2, 3]. The incidence in children ranges from 41.7% to 75.44%, and the incidence in children aged 2 to 7 in China is similar to that in other countries, i.e., approximately 67.6% [4, 5]. Currently, the evaluation of preoperative anxiety still relies on multiple psychometric scales mainly including the State Trait Anxiety Inventory-State/Trait (STAI-S/T), the Amsterdam Preoperative Anxiety and Information Scale (APAIS), the Visual Analogue Scale for Anxiety (VAS-A), the Hospital Anxiety and Depression Scale-Anxiety (HADS-A), Generalized Anxiety Disorder 7 (GAD-7) and the modified Yale Preoperative Anxiety Scale (m-YAPS) [6, 7]. Nevertheless, there is no gold standard for assessing preoperative anxiety and multiple factors should be taken into consideration when choosing suitable scales such as their reliability and accuracy, the aim of the assessment, the patient’s age and clinical state and the type of surgery being planned [6].
Although postoperative adverse events are not yet well defined, their core essence includes medical practice-related events that can cause unnecessary or unpredictable hazards to patients or have the potential to produce harm, thus further increasing hospital costs, prolonging the time of hospitalization and affecting long-term prognosis [8, 9]. Excessive preoperative anxiety not only leads to sympathetic nervous excitement, causes cardiac oxygen consumption, and promotes platelet activation and aggregation, but also increases the occurrence of postoperative adverse events, such as hemodynamic instability, the usage of anesthetics, insomnia, pain, nausea and vomiting, neurocognitive dysfunction and even long-term mortality [10, 11].
Hence, in this narrative review we focus on the relationship between preoperative anxiety and postoperative adverse events, describe effective intervention strategies for preoperative anxiety and provide a summary and outlook.
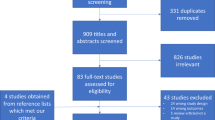
1 Methodology
We searched online for papers that examined the relationship between preoperative anxiety and postoperative adverse events. We searched the PubMed, Scopus, Web of Science and Google Scholar databases from inception to 2022 using the following terms: ‘preoperative anxiety’, ‘postoperative adverse events’, ‘postoperative insomnia’, ‘postoperative sleep disturbance’, ‘postoperative pain’, ‘postoperative nausea and vomiting’, ‘perioperative neurocognitive disorders’, ‘postoperative cognitive dysfunction’ and ‘postoperative delirium’. We focused on the most recent and most relevant clinical studies. Basic research and articles that provided no abstract were excluded.
2 Preoperative anxiety and postoperative insomnia
Insomnia is a common sleep problem that is particularly high in perioperative patients. Epidemiological data suggest that individuals with insomnia exhibit more anxiety symptoms and similarly individuals with anxiety are more likely to suffer insomnia [12, 13]. Data collected from 997 patients undergoing elective surgery from 12 hospitals in China showed that higher preoperative anxiety (STAI-S > 44) was associated to poorer postoperative sleep quality [odds ratio (OR) = 1.79, 95% confidence interval (CI) = 1.17–2.76, p = 0.008) [14]. A retrospective cohort study recruited 299 noncardiac surgery patients with a mean age of 55 years and revealed that the incidence of insomnia at 3 days postoperatively was 26.1% (78/299). Logistic regression further showed that a higher preoperative GAD-7 score was a risk factor for insomnia after surgery (95% CI = 1.041–1.218, p = 0.003) [15]. Another prospective cohort study of 107 patients undergoing primary total joint arthroplasty indicated that 31% of patients exhibited poor sleep quality at 4, 8 and even 12 weeks postoperatively. Multivariate logistic regression analysis revealed that patients with a higher Zung Self-Rating Anxiety Scale (SAS) score suffered more from sleep disturbance (OR = 1.462, 95% CI = 1.171–1.825, p = 0.001) [16]. Postoperative insomnia not only increases the use of opioid consumption, but also increases the incidence of postoperative pain and delirium, which seriously affect the recovery of patients and diminish their satisfaction [17,18,19]. Therefore, reducing preoperative anxiety may have a critical impact on improving postoperative insomnia.
3 Preoperative anxiety and postoperative pain
Postoperative pain is a common but often inadequately treated condition. Numerous studies have suggested that preoperative anxiety not only increases the consumption of intraoperative anesthetics and vasoactive drugs, but also increases the usage of postoperative analgesics and is positively correlated with postoperative acute and chronic pain [10, 20]. A prospective study of 100 patients undergoing laparoscopic hysterectomy showed that the average preoperative anxiety score (evaluated with the SAS) was 40.99 ± 55 points, which was higher than the norm (29.78 ± 46) in China. The correlation coefficients between preoperative anxiety scores and postoperative pain scores in two different groups were 0.836 and 0.870 respectively, presenting with a markedly positive correlation [21]. An institutional-based prospective cohort study demonstrated that patients with high preoperative anxiety (STAI > 44) experienced obviously increased postoperative pain at 2, 4, 6 and 12 h, with p values of 0.012, 0.01, 0.001 and 0.002 respectively. The total tramadol consumption of 24 h in patients with high anxiety levels was 156.5 ± 23.4 while in patients with low anxiety levels, it was 147.1 ± 39.0, with a p value of 0.036 [22]. In addition, a prospective study from 194 consecutive patients who underwent glaucoma surgery showed that preoperative anxiety (evaluated with the SAS) was associated with increased clinically significant postoperative pain (OR = 4.13, 95% CI = 1.29–13.2, p = 0.017) [23]. It is well known that the consequences of suboptimal postoperative pain control include persistent postsurgical pain, prolonged duration of opioid use, delayed recovery time, impaired physical function, increased length of hospital stay and health care costs [24,25,26]. Thus, it is of great significance to decrease preoperative anxiety levels to reduce postoperative pain and analgesic consumption.
4 Preoperative anxiety and postoperative nausea and vomiting
Nausea and vomiting are the most common adverse events after surgery under general anesthesia, even above pain. However, there are few relevant studies on the relationship between preoperative anxiety and postoperative nausea and vomiting (PONV), and the results are inconsistent. A prospective study enrolled 200 consecutive patients who underwent ambulatory hand surgeries under general anesthesia and illustrated that PONV during the first 24 h after surgery was associated with a high level of preoperative anxiety (assessed using APAIS) in these patients (r = 0.301, p = 0.017) [27]. A retrospective cohort study of 8665 outpatients undergoing cancer surgery revealed that patients with preoperative anxiety had higher rates of adverse outcomes including PONV (adjusted difference 1.8%, 95% CI = 0.12%–3.4%, p = 0.029) [28]. These results indicated that preventing one instance of PONV would require treating at least 30 patients for anxiety. Moreover, a cross-sectional study enrolled 51 unpremeditated children (5–16 years old) undergoing outpatient surgery and showed that children's anxiety in the preoperative holding area has no predictive value for the occurrence of PONV in the post-anesthesia care unit or 24 h postoperatively [29]. In addition, a recent study also indicated that the correlation between preoperative anxiety and PONV was not statistically significant [14]. Although the relationship is not entirely clear, several complications caused by PONV such as wound dehiscence, aspiration, elevated intracranial pressure, health care costs and patient satisfaction still need to be considered.
5 Preoperative anxiety and postoperative neurocognitive dysfunction
Decline in cognitive ability is a common complication experienced in the postoperative period by adults, especially elderly individuals. Currently, all forms of related cognitive impairment are called perioperative neurocognitive disorder (PND) rather than postoperative cognitive dysfunction (postoperative cognitive dysfunction, POCD), as previously described [30, 31]. PND includes short-term disturbances (postoperative delirium, POD) and long-term disturbances (POCD) [32, 33]. It is well known that POD or POCD is associated with an increased rate of almost any postoperative complication, prolonged hospital stays, increased care dependency, a decrease in functional state, and a long-term increase in morbidity and mortality [34, 35]. Moreover, preoperative anxiety has been shown to detrimentally affect patients cognitively [36].
POD, is a syndrome characterized by an acute change in attention, awareness and cognition after surgery, which includes alterations in consciousness and disorganized thinking [37, 38]. A growing body of research has uncovered the close association between preoperative anxiety and POD in recent years. A prospective cohort study enrolled 372 adults undergoing total hip arthroplasty demonstrated that patients with anxiety had a higher incidence of POD than patients without anxiety (25.3% vs. 14.8%, OR = 0.51, 95% CI = 0.92–0.29, p = 0.025) [39]. Another prospective observational cohort study of elderly patients (aged 65 years or older) undergoing elective orthopedic surgery illustrated that preoperative anxiety was independently associated with POD (OR = 3.119, 95% CI = 1.144–8.500, p = 0.026) [40]. There was also a retrospective study that demonstrated anxiety was an independent predictor of POD in older patients undergoing elective surgery for lumbar disc herniation (OR = 2.228, 95% CI = 1.494–3.416, p = 0.009) [41]. Studies of other types of surgery have reached similar conclusions [42,43,44]. However, a few studies have also identified no significant association between them [45, 46]. The possible reasons for explanation were the difficulties in operationalization, measurement of preoperative anxiety or patients with good premorbid cognitive and functional status.
Unlike POD, POCD refers to a persistent rather than a transient state of cognitive dysfunction that occurs subsequent to surgery and anesthesia [47, 48]. To date, no direct evidence has suggested that there is a definite relationship between preoperative anxiety and POCD. A secondary data analysis of POCD in a cohort study of patients ≥ 65 undergoing elective noncardiac surgery demonstrated that preoperative anxiety symptoms were related to physical state rather than a harbinger of early cognitive decline [49]. Moreover, a prospective cohort study enrolled 26 older participants (mean age = 70 years, standard deviation = 8 years) who were scheduled for cochlear implantation has illustrated that no significant risk factors (including preoperative anxiety) were identified besides an effect of age on POCD [50]. Although reducing preoperative anxiety may provide an effective strategy for preventing PND, more high-quality evidence is needed.
6 Preoperative anxiety and other adverse events
In addition to the above adverse events, preoperative anxiety is also a negative factor affecting postoperative recovery. On the one hand, preoperative anxiety may give rise to perioperative hypertension, sinus tachycardia, myocardial ischemia and other cardio-cerebral vascular accidents, which can cause an increase in hospitalization expense and extension of hospitalization time [51]. On the other hand, preoperative anxiety also elicits the secretion of catecholamines and glucocorticoids in patients and further increases the risk of infection as well as delays wound healing [52]. In addition, although high levels of anxiety have been presented in few patients anticipated in cardiac surgery, these confer a strong and independent heightened risk of mortality or major morbidity [53]. Moreover, preoperative anxiety in young children undergoing surgery is associated with a more painful postoperative recovery and a higher incidence of sleep disorders, delirium and other problems [54]. Thus, preoperative anxiety has many effects on perioperative prognosis and outcome, so it is necessary to conduct appropriate interventions.
7 Intervention strategies for preoperative anxiety
Currently, effective interventions to treat or prevent preoperative anxiety are being actively explored to decrease the development of postoperative adverse events. Such interventions mainly include pharmacotherapies and nonpharmacotherapies.
7.1 Pharmacotherapy
Pregabalin is a gabapentinoid that has been widely used for the treatment of seizures and pain [55]. Additionally, as an adjuvant of opioids, it can also reduce opioid consumption when used in combination [56]. Recently, a systematic review and meta-analysis illustrated that there was moderate evidence of the efficacy of gabapentinoids in anxiety states [mean difference (MD) = −0.55, 95% CI = −0.92 – −0.18) [57]. An earlier prospective, randomized and controlled study conducted in consenting patients who underwent elective craniotomy for brain tumor resection demonstrated that perioperative use of twice-daily 150 mg pregabalin could attenuate preoperative anxiety, improve perioperative sleep quality, and reduce postoperative pain scores and analgesic usage without increasing the rate of adverse effects [58]. Another prospective, randomized and controlled study revealed that pregabalin was effective in reducing preoperative anxiety and that 150 or 300 mg pregabalin was associated with reduced blood pressure fluctuations after intubation, but with no significant differences between the two dose groups [59]. A similar study also directly presented that 150 mg of pregabalin was effective in attenuating preoperative anxiety and stress responses to endotracheal intubation [60].
Perioperative benzodiazepines are administered because of their anxiolytic, sedative and amnestic effects [61]. The use of midazolam as premedication for inducing anxiolysis before surgical procedures is widely accepted. In a double-blinded randomized clinical trial, investigators enrolled 90 participants aged 2–6 years who were scheduled for elective ear-, nose-and-throat surgery. Compared to oral clonidine (4 µg/kg) or intranasal dexmedetomidine (2 µg/kg), preschool children who took midazolam orally (0.5 mg/kg) resulted in more effective anxiolysis and less sedation [62]. A prospective, randomized and placebo-controlled study enrolled 88 patients scheduled for outpatient surgery and revealed that intravenous midazolam (0.04 mg/kg) was an effective anxiolytic and fewer patients in the midazolam group experienced postoperative vomiting than placebo group patients (8% vs. 21%) [63]. Alprazolam, a new short-acting benzodiazepine, has been confirmed earlier to be an effective alternative to midazolam for anxiety reduction without causing amnesia [64, 65]. Seventy-five patients scheduled for abdominal hysterectomy under general anesthesia were included in a randomized, placebo-controlled study. Oral alprazolam (0.5 mg 2 h prior to surgery) provided significant anxiolysis and showed no opioid sparing effects postoperatively compared to placebo. However, we must pay attention to the impairment of psychomotor function in the early postoperative period [64].
Melatonin, a naturally occurring hormone, has been confirmed to offer an alternative treatment to benzodiazepines for ameliorating anxiety conditions in the perioperative period [2, 66]. Madsen et al. carried out a systematic meta-analysis including 27 randomized controlled trials and 2319 participants to assess the use of melatonin for treating perioperative anxiety. They pointed out that melatonin could effectively reduce preoperative anxiety (MD = −11.69, 95% CI = −13.80 – −9.59) and had less interference with psychomotor and cognitive function than benzodiazepines [2]. In addition, a double-blind randomized clinical trial demonstrated that melatonin (5 mg prolonged-release oral capsules) was an effective alternative to manage anxiety and could help to reduce intraoperative midazolam consumption and hospital stay in women undergoing total abdominal hysterectomy [67]. Moreover, a randomized and placebo-controlled trial also showed that compared with oral midazolam (0.3 mg/kg), a multimodal anxiolytic approach with oral melatonin (0.3 mg/kg) could markedly reduce preoperative anxiety and postoperative delirium in children 3 to 8 years who received sevoflurane anesthesia for elective ambulatory procedures [68].
Dexmedetomidine is a highly selective α2-adrenergic receptor agonist that is associated with sedative and analgesic sparing effects as well as reduced delirium and anxiety. Recent research has shown that dexmedetomidine could improve the preoperative anxiety of patients undergoing carotid artery stenting and achieve a sufficient sedation effect without causing postoperative cognitive dysfunction [69]. Moreover, when compared with midazolam, dexmedetomidine was effective in decreasing preoperative anxiety upon separation from parents [risk ratio (RR) = 1.30 (1.05–1.62), p = 0.02] [70]. Unlike oral or intravenous administration, intranasal dexmedetomidine eliminates the need for venous opening, pain and other side effects such as infection and anaphylaxis in patients [71, 72]. A prospective, randomized and controlled trial indicated that intranasal dexmedetomidine could safely and effectively improve the preoperative anxiety and insomnia condition of patients with insomnia and anxiety [73]. In addtion, another prospective study also illustrated that intranasal dexmedetomidine premedication was more effective than oral midazolam to reduce preoperative anxiety in pediatric patients (2–12 years of age) [74]. Thus, intranasal dexmedetomidine may be used as a complementary therapy for preoperative anxiety.
7.2 Nonpharmacotherapy
Aromatherapy is a form of holistic healing treatment that uses essential oils or aromas to improve persons’ emotional and physical conditions. The pooled results from a systematic meta-analysis demonstrated that aromatherapy with different essential oils could alleviate anxiety significantly regardless of the reason for anxiety. The weighted MD was −5.16 for the STAI-S (95% CI = −5.78 – −4.55, p < 0.001) and −2.85 for the STAI-T (95% CI = −3.95 – −1.75, p < 0.001) [75]. Another meta-analysis indicated that aromatherapy could significantly ameliorate preoperative anxiety (standard MD = −0.57, 95% CI = −0.75 – −0.39, p < 0.00001) for adults awaiting surgical procedures, compared to placebo control, conventional care and no intervention. Short-length (≤ 20 min per session) aromatherapy inhalation seemed to be more worthy of being recommended in clinical settings [76]. In addition, a randomized trial determined that aromatherapy could reduce anxiety when administered to women (≥ 18 years) before undergoing breast surgery despite no significant changes in vital signs [77].
Music therapy is the clinical use of music to accomplish individualized goals such as reducing stress and improving mood and anxiety. It has been suggested that preoperative music exposure was effective in reducing anxiety level and self-reported pain on intra- and post-operative pain during cataract surgery [78]. A prospective, randomized and controlled trial illustrated that listening to patient-preferred favour music preoperatively can reduce anxiety, regulate hemodynamic parameters and improve postoperative patient satisfaction [79]. A recent randomized controlled study showed that music therapy might be a viable complementary modality to usual surgical care in the gynecologic setting for its ability to significantly decrease preoperative anxiety in women undergoing total laparoscopic hysterectomy for benign conditions [80].
Massage therapy is a traditional technique in China and it can prompt the release of hormones and provide a feeling of ease to relieve tension and anxiety. A recent study revealed that foot massage is effective in alleviating pain and anxiety while improving quality of life in patients undergoing anterior cervical discectomy and fusion [81]. Moreover, machine-based hand massage significantly reduces anxiety in patients awaiting ambulatory surgery while not significantly affecting their vital signs [82]. Furthermore, aromatherapy massage with lavender oil increases sleep quality and reduces the level of anxiety in patients with colorectal surgery in the preoperative period [83].
Other forms of relaxation also reveal good anxiolytic effects. Guided imagery is a free stress-relieving therapy and, with practice, can be done just about anywhere. A randomized, triple-blind clinical trial illustrated that guided imagery relaxation therapy was an effective nursing intervention for the reduction of state anxiety and blood cortisol levels in the preoperative period in patients undergoing video-laparoscopic bariatric surgery [84]. Hypnosis is a modified state of consciousness that is different from normal consciousness and sleep stages. A randomized controlled trial revealed that hypnosis intervention significantly alleviated patients’ anxiety levels before entering the operating rooms [85]. In addition to the methods mentioned above, acupuncture, virtual reality and proper exercise are also noninvasive and nondrug intervention methods that have been reported to effectively reduce preoperative anxiety [51, 86, 87]. However, further research is needed to address the effective use of nonpharmacotherapies in the management of preoperative anxiety.
8 Summary and outlook
As one of the most common clinical problems in perioperative patients, preoperative anxiety is closely related to the occurrence of postoperative adverse events. Many clinical studies have confirmed that preoperative anxiolytic interventions can effectively reduce the occurrence of postoperative adverse events. Therefore, paying more attention to patients' preoperative anxiety and taking more effective actions will help ensure the safety of patients and improve their satisfaction. Nevertheless, due to their complicated relationship, studies on the mechanisms of preoperative anxiety affecting postoperative adverse events are relatively rare. Therefore, exploring the exact mechanisms and identifying new therapeutic targets should be priorities for future work.
Availability of data and materials
Not applicable.
Abbreviations
- APAIS:
-
Amsterdam preoperative anxiety and information scale
- CI:
-
Confidence interval
- GAD-7:
-
Generalized anxiety disorder 7
- HADS-A:
-
Hospital anxiety and depression scale-anxiety
- MD:
-
Mean difference
- m-YAPS:
-
Modified Yale preoperative anxiety scale
- OR:
-
Odds ratio
- POCD:
-
Postoperative cognitive dysfunction
- POD:
-
Postoperative delirium
- PONV:
-
Postoperative nausea and vomiting
- PND:
-
Perioperative neurocognitive disorders
- RR:
-
Risk ratio
- SAS:
-
Self-rating anxiety scale
- STAI-S/T:
-
State trait anxiety inventory-state/trait
- VAS-A:
-
Visual analogue scale for anxiety
References
Stamenkovic DM, Rancic NK, Latas MB, Neskovic V, Rondovic GM, Wu JD, et al. Preoperative anxiety and implications on postoperative recovery: what can we do to change our history. Minerva Anestesiol. 2018;84(11):1307–17.
Madsen BK, Zetner D, Møller AM, Rosenberg J. Melatonin for preoperative and postoperative anxiety in adults. Cochrane Database Syst Rev. 2020;12(12):CD009861.
Eberhart L, Aust H, Schuster M, Sturm T, Gehling M, Euteneuer F, et al. Preoperative anxiety in adults - a cross-sectional study on specific fears and risk factors. BMC Psychiatry. 2020;20(1):140.
Liu W, Xu R, Jia J, Shen Y, Li W, Bo L. Research progress on risk factors of preoperative anxiety in children: a scoping review. Int J Environ Res Public Health. 2022;19(16):9828.
Liang Y, Huang W, Hu X, Jiang M, Liu T, Yue H, et al. Preoperative anxiety in children aged 2–7 years old: a cross-sectional analysis of the associated risk factors. Transl Pediatr. 2021;10(8):2024–34.
Zemła AJ, Nowicka-Sauer K, Jarmoszewicz K, Wera K, Batkiewicz S, Pietrzykowska M. Measures of preoperative anxiety. Anaesthesiol Intensive Ther. 2019;51(1):64–9.
Jenkins BN, Fortier MA, Kaplan SH, Mayes LC, Kain ZN. Development of a short version of the modified yale preoperative anxiety scale. Anesth Analg. 2014;119(3):643–50.
Fecho K, Moore CG, Lunney AT, Rock P, Norfleet EA, Boysen PG. Anesthesia-related perioperative adverse events during in-patient and out-patient procedures. Int J Health Care Qual Assur. 2008;21(4):396–412.
Sangkum L, Wathanavaha C, Tantrakul V, Pothong M, Karnjanarachata C. Modified STOP-Bang for predicting perioperative adverse events in the Thai population. BMC Anesthesiol. 2021;21(1):132.
Lindberg MF, Miaskowski C, Rustøen T, Cooper BA, Aamodt A, Lerdal A. Preoperative risk factors associated with chronic pain profiles following total knee arthroplasty. Eur J Pain. 2021;25(3):680–92.
Cserép Z, Losoncz E, Balog P, Szili-Török T, Husz A, Juhász B, et al. The impact of preoperative anxiety and education level on long-term mortality after cardiac surgery. J Cardiothorac Surg. 2012;7:86.
Manzar MD, Noohu MM, Salahuddin M, Nureye D, Albougami A, Spence DW, et al. Insomnia symptoms and their association with anxiety and poor sleep hygiene practices among Ethiopian university students. Nat Sci Sleep. 2020;12:575–82.
Choueiry N, Salamoun T, Jabbour H, El Osta N, Hajj A, Rabbaa Khabbaz L. Insomnia and relationship with anxiety in university students: a cross-sectional designed study. PLoS One. 2016;11(2):e0149643.
Li XR, Zhang WH, Williams JP, Li T, Yuan JH, Du Y, et al. A multicenter survey of perioperative anxiety in China: Pre- and postoperative associations. J Psychosom Res. 2021;147:110528.
Huang X, Wu D, Wu AS, Wei CW, Gao JD. The association of insomnia with depression and anxiety symptoms in patients undergoing noncardiac surgery. Neuropsychiatr Dis Treat. 2021;17:915–24.
Wang Y, Liu Y, Li X, Lv Q, Xia Q, Wang X, et al. Prospective assessment and risk factors of sleep disturbances in total hip and knee arthroplasty based on an Enhanced Recovery After Surgery concept. Sleep Breath. 2021;25(3):1231–7.
Nowakowski S, Levy-Meeks ME, Dawson DB, Meers JM, Stout-Aguilar JS, Kilic GS, et al. Association of preoperative sleep pattern with posthysterectomy pain: a pilot study. J Clin Sleep Med. 2020;16(11):1901–8.
Rhon DI, Snodgrass SJ, Cleland JA, Cook CE. Comorbid insomnia and sleep apnea are associated with greater downstream health care utilization and chronic opioid use after arthroscopic hip surgery. Pain Physician. 2019;22(4):E351–60.
Leung JM, Sands LP, Newman S, Meckler G, Xie Y, Gay C, et al. Preoperative sleep disruption and postoperative delirium. J Clin Sleep Med. 2015;11(8):907–13.
Tan H, Wei J, Li S, Yu L, Sun H, Ji K, et al. Pain threshold, anxiety and other factors affect intensity of postoperative pain in gastric cancer patients: a prospective cohort study. Chin J Cancer Res. 2021;33(3):343–51.
Zhang L, Hao LJ, Hou XL, Wu YL, Jing LS, Sun RN. Preoperative anxiety and postoperative pain in patients with laparoscopic hysterectomy. Front Psychol. 2021;12:727250.
Tadesse M, Ahmed S, Regassa T, Girma T, Hailu S, Mohammed A, et al. Effect of preoperative anxiety on postoperative pain on patients undergoing elective surgery: Prospective cohort study. Ann Med Surg (Lond). 2022;73:103190.
Li Z, Yao S, Ni Y, Huang W, Zheng W, Yang J, et al. Associated risk factors of postoperative pain after glaucoma surgery: a prospective study. Int Ophthalmol. 2022;42(3):829–40.
Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res. 2017;10:2287–98.
Ishida Y, Okada T, Kobayashi T, Funatsu K, Uchino H. Pain Management of Acute and Chronic Postoperative Pain. Cureus. 2022;14(4):e23999.
Gupta AK, Mena S, Jin Z, Gan TJ, Bergese S. Postoperative pain: a review of emerging therapeutic options. Expert Rev Neurother. 2021;21(10):1085–100.
Roh YH, Gong HS, Kim JH, Nam KP, Lee YH, Baek GH. Factors associated with postoperative nausea and vomiting in patients undergoing an ambulatory hand surgery. Clin Orthop Surg. 2014;6(3):273–8.
Majumdar JR, Vertosick EA, Cohen B, Assel M, Levine M, Barton-Burke M. Preoperative Anxiety in Patients Undergoing Outpatient Cancer Surgery. Asia Pac J Oncol Nurs. 2019;6(4):440–5.
Wang SM, Kain ZN. Preoperative anxiety and postoperative nausea and vomiting in children: is there an association? Anesth Analg. 2000;90(3):571–5.
Evered L, Silbert B, Knopman DS, Scott DA, DeKosky ST, Rasmussen LS, et al. Recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery-2018. Br J Anaesth. 2018;121(5):1005–12.
Eckenhoff RG, Maze M, Xie Z, Culley DJ, Goodlin SJ, Zuo Z, et al. Perioperative Neurocognitive Disorder: State of the Preclinical Science. Anesthesiology. 2020;132(1):55–68.
Monk TG, Price CC. Postoperative cognitive disorders. Curr Opin Crit Care. 2011;17(4):376–81.
Tasbihgou SR, Absalom AR. Postoperative neurocognitive disorders. Korean J Anesthesiol. 2021;74(1):15–22.
Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157–65.
Deiner S, Silverstein JH. Postoperative delirium and cognitive dysfunction. Br J Anaesth. 2009;103 Suppl 1(Suppl 1):i41-46.
Tulloch I, Rubin JS. Assessment and Management of Preoperative Anxiety. J Voice. 2019;33(5):691–6.
Rudolph JL, Marcantonio ER. Review articles: postoperative delirium: acute change with long-term implications. Anesth Analg. 2011;112(5):1202–11.
Wilson JE, Mart MF, Cunningham C, Shehabi Y, Girard TD, MacLullich AMJ, et al. Delirium. Nat Rev Dis Primers. 2020;6(1):90.
Ma J, Li C, Zhang W, Zhou L, Shu S, Wang S, et al. Preoperative anxiety predicted the incidence of postoperative delirium in patients undergoing total hip arthroplasty: a prospective cohort study. BMC Anesthesiol. 2021;21(1):48.
Ren A, Zhang N, Zhu H, Zhou K, Cao Y, Liu J. Effects of preoperative anxiety on postoperative delirium in elderly patients undergoing elective orthopedic surgery: a prospective observational cohort study. Clin Interv Aging. 2021;16:549–57.
Mou Q, Gao M, Liu X, Wei C, Lan G, Zhao X, et al. Preoperative anxiety as an independent predictor of postoperative delirium in older patients undergoing elective surgery for lumbar disc herniation. Aging Clin Exp Res. 2022;35(1):85–90.
Pakrad F, Pakrad E, Darvishi N, Poorolajal J. Preoperative anxiety and depression increases the incidence of delirium after coronary artery bypass graft surgery. J Perianesth Nurs. 2020;35(5):496–501.
Cheng HW, Liu CY, Chen YS, Shih CC, Chen WY, Chiou AF. Assessment of preoperative frailty and identification of patients at risk for postoperative delirium in cardiac intensive care units: a prospective observational study. Eur J Cardiovasc Nurs. 2021;20(8):745–51.
Wada S, Inoguchi H, Sadahiro R, Matsuoka YJ, Uchitomi Y, Sato T, et al. Preoperative Anxiety as a Predictor of Delirium in Cancer Patients: A Prospective Observational Cohort Study. World J Surg. 2019;43(1):134–42.
Fukunaga H, Sugawara H, Koyama A, Okamoto K, Fukui T, Ishikawa T, et al. Relationship between preoperative anxiety and onset of delirium after cardiovascular surgery in elderly patients: focus on personality and coping process. Psychogeriatrics. 2022;22(4):453–9.
Milisen K, Van Grootven B, Hermans W, Mouton K, Al Tmimi L, Rex S, et al. Is preoperative anxiety associated with postoperative delirium in older persons undergoing cardiac surgery? Secondary data analysis of a randomized controlled trial. BMC Geriatr. 2020;20(1):478.
Brodier EA, Cibelli M. Postoperative cognitive dysfunction in clinical practice. BJA Educ. 2021;21(2):75–82.
Evered LA, Silbert BS. Postoperative cognitive dysfunction and noncardiac surgery. Anesth Analg. 2018;127(2):496–505.
Wang S, Cardieri B, Mo Lin H, Liu X, Sano M, Deiner SG. Depression and anxiety symptoms are related to pain and frailty but not cognition or delirium in older surgical patients. Brain Behav. 2021;11(6):e02164.
Claes AJ, de Backer S, Van de Heyning P, Gilles A, Van Rompaey V, Mertens G. Postoperative cognitive dysfunction after cochlear implantation. Eur Arch Otorhinolaryngol. 2018;275(6):1419–27.
Fathi M, Alavi SM, Joudi M, Joudi M, Mahdikhani H, Ferasatkish R, et al. Preoperative anxiety in candidates for heart surgery. Iran J Psychiatry Behav Sci. 2014;8(2):90–6.
Singh Solorzano C, Steptoe A, Leigh E, Kidd T, Jahangiri M, Poole L. Pre-surgical Caregiver Burden and Anxiety Are Associated with Post-Surgery Cortisol over the Day in Caregivers of Coronary Artery Bypass Graft Surgery Patients. Int J Behav Med. 2019;26(3):316–22.
Williams JB, Alexander KP, Morin JF, Langlois Y, Noiseux N, Perrault LP, et al. Preoperative anxiety as a predictor of mortality and major morbidity in patients aged >70 years undergoing cardiac surgery. Am J Cardiol. 2013;111(1):137–42.
Kain ZN, Mayes LC, Caldwell-Andrews AA, Karas DE, McClain BC. Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing surgery. Pediatrics. 2006;118(2):651–8.
Mathieson S, Lin CC, Underwood M, Eldabe S. Pregabalin and gabapentin for pain. BMJ. 2020;369:m1315.
Knezevic NN, Aijaz T, Camacho-Ortega A, Candido KD. A Retrospective Analysis of Gabapentinoid and Opioids to Opioid Monotherapy for Pain Relief in Patients with Chronic Neck and Low Back Pain. Pain Med. 2021;22(8):1760–6.
Hong JSW, Atkinson LZ, Al-Juffali N, Awad A, Geddes JR, Tunbridge EM, et al. Gabapentin and pregabalin in bipolar disorder, anxiety states, and insomnia: systematic review, meta-analysis, and rationale. Mol Psychiatry. 2022;27(3):1339–49.
Shimony N, Amit U, Minz B, Grossman R, Dany MA, Gonen L, et al. Perioperative pregabalin for reducing pain, analgesic consumption, and anxiety and enhancing sleep quality in elective neurosurgical patients: a prospective, randomized, double-blind, and controlled clinical study. J Neurosurg. 2016;125(6):1513–22.
Chen W, Huang H, Yang C, Hu X, Bao F, Jiang H. Preoperative Low-dose and High-dose Pregabalin and Cardiovascular Response to Endotracheal Intubation: A Prospective, Randomized, Single-blind, Controlled Study in China. Clin Ther. 2019;41(1):68–77.
Singh D, Yadav JS, Jamuda BK, Singh P. Oral Pregabalin as Premedication on Anxiolysis and Stress Response to Laryngoscopy and Endotracheal Intubation in Patients Undergoing Laparoscopic Cholecystectomy: A Randomized Double-Blind Study. Anesth Essays Res. 2019;13(1):97–104.
Spence J, Young J, Alhazzani W, Whitlock R, D’Aragon F, Um K, et al. Safety and efficacy of perioperative benzodiazepine administration: study protocol for a systematic review and meta-analysis. BMJ Open. 2019;9(12):e031895.
Bromfalk Å, Myrberg T, Walldén J, Engström Å, Hultin M. Preoperative anxiety in preschool children: a randomized clinical trial comparing midazolam, clonidine, and dexmedetomidine. Paediatr Anaesth. 2021;31(11):1225–33.
Bauer KP, Dom PM, Ramirez AM, O’Flaherty JE. Preoperative intravenous midazolam: benefits beyond anxiolysis. J Clin Anesth. 2004;16(3):177–83.
De Witte JL, Alegret C, Sessler DI, Cammu G. Preoperative alprazolam reduces anxiety in ambulatory surgery patients: a comparison with oral midazolam. Anesth Analg. 2002;95(6):1601–6, table of contents.
Ozkan TA, Koprulu S, Karakose A, Dillioglugil O, Cevik I. Does using alprazolam during outpatient flexible cystoscopy decrease anxiety and pain? Arch Esp Urol. 2017;70(9):800–5.
Hansen MV, Halladin NL, Rosenberg J, Gögenur I, Møller AM. Melatonin for pre- and postoperative anxiety in adults. Cochrane Database Syst Rev. 2015;2015(4):CD009861.
Rosas-Luna LE, Castelán-Martínez OD, Mora-Magaña I, Ángeles-Castellanos M, Ubaldo-Reyes LM. Midazolam reduction with pre-operative melatonin in abdominal hysterectomy: double-blind randomized clinical trial. Cir Cir. 2022;90(3):353–8.
Singla L, Mathew PJ, Jain A, Yaddanapudi S, Peters NJ. Oral melatonin as part of multimodal anxiolysis decreases emergence delirium in children whereas midazolam does not: A randomised, double-blind, placebo-controlled study. Eur J Anaesthesiol. 2021;38(11):1130–7.
Wu LP, Kang WQ. Effect of dexmedetomidine for sedation and cognitive function in patients with preoperative anxiety undergoing carotid artery stenting. J Int Med Res. 2020;48(9):300060520938959.
Pasin L, Febres D, Testa V, Frati E, Borghi G, Landoni G, et al. Dexmedetomidine vs midazolam as preanesthetic medication in children: a meta-analysis of randomized controlled trials. Paediatr Anaesth. 2015;25(5):468–76.
Wilt TJ, MacDonald R, Brasure M, Olson CM, Carlyle M, Fuchs E, et al. Pharmacologic Treatment of Insomnia Disorder: An Evidence Report for a Clinical Practice Guideline by the American College of Physicians. Ann Intern Med. 2016;165(2):103–12.
Lou BX, Oks M. Insomnia: Pharmacologic Treatment. Clin Geriatr Med. 2021;37(3):401–15.
Zeng W, Chen L, Liu X, Deng X, Huang K, Zhong M, et al. Intranasal Dexmedetomidine for the Treatment of Pre-operative Anxiety and Insomnia: A Prospective, Randomized, Controlled, and Clinical Trial. Front Psychiatry. 2022;13:816893.
Linares Segovia B, García Cuevas MA, Ramírez Casillas IL, Guerrero Romero JF, BotelloBuenrostro I, Monroy Torres R, et al. Pre-anesthetic medication with intranasal dexmedetomidine and oral midazolam as an anxiolytic. A clinical trial. An Pediatr (Barc). 2014;81(4):226–31. Spanish.
Gong M, Dong H, Tang Y, Huang W, Lu F. Effects of aromatherapy on anxiety: a meta-analysis of randomized controlled trials. J Affect Disord. 2020;274:1028–40.
Guo P, Li P, Zhang X, Liu N, Wang J, Yang S, et al. The effectiveness of aromatherapy on preoperative anxiety in adults: a systematic review and meta-analysis of randomized controlled trials. Int J Nurs Stud. 2020;111:103747.
Franco L, Blanck TJ, Dugan K, Kline R, Shanmugam G, Galotti A, et al. Both lavender fleur oil and unscented oil aromatherapy reduce preoperative anxiety in breast surgery patients: a randomized trial. J Clin Anesth. 2016;33:243–9.
Guerrier G, Bernabei F, Lehmann M, Pellegrini M, Giannaccare G, Rothschild PR. Efficacy of preoperative music intervention on pain and anxiety in patients undergoing cataract surgery. Front Pharmacol. 2021;12:748296.
Kavak Akelma F, Altınsoy S, Arslan MT, Ergil J. Effect of favorite music on postoperative anxiety and pain. Anaesthesist. 2020;69(3):198–204.
Casarin J, Cromi A, Sgobbi B, Di Siena A, Serati M, Bolis ME, et al. Music Therapy for Preoperative Anxiety Reduction in Women Undergoing Total Laparoscopic Hysterectomy: A Randomized Controlled Trial. J Minim Invasive Gynecol. 2021;28(9):1618-24.e1.
Ren N, Yang G, Ren X, Li L. Effects of foot massage on relieving pain, anxiety and improving quality of life of patients undergone a cervical spine surgery. Health Qual Life Outcomes. 2021;19(1):22.
Ni CH, Wei L, Wu CC, Lin CH, Chou PY, Chuang YH, et al. Machine-Based Hand Massage Ameliorates Preoperative Anxiety in Patients Awaiting Ambulatory Surgery. J Nurs Res. 2021;29(3):e152.
Ayik C, Özden D. The effects of preoperative aromatherapy massage on anxiety and sleep quality of colorectal surgery patients: a randomized controlled study. Complement Ther Med. 2018;36:93–9.
Felix MMDS, Ferreira MBG, Oliveira LF, Barichello E, Pires PDS, Barbosa MH. Guided imagery relaxation therapy on preoperative anxiety: a randomized clinical trial. Rev Lat Am Enfermagem. 2018;26:e3101.
Saadat H, Drummond-Lewis J, Maranets I, Kaplan D, Saadat A, Wang SM, et al. Hypnosis reduces preoperative anxiety in adult patients. Anesth Analg. 2006;102(5):1394–6.
Zanella S, Buccelletti F, Vassiliadis A, De Bortoli R, Visentini S, Pedrotti G, et al. Preoperative anxiety management: acupuncture vs. pharmacological treatment - A prospective study. Eur Rev Med Pharmacol Sci. 2022;26(3):900–5.
Jung MJ, Libaw JS, Ma K, Whitlock EL, Feiner JR, Sinskey JL. Pediatric Distraction on Induction of Anesthesia With Virtual Reality and Perioperative Anxiolysis: A Randomized Controlled Trial. Anesth Analg. 2021;132(3):798–806.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
KN and ZM contributed to the conception of the study and writing, reviewing as well as editing of the manuscript. JZ contributed to the material collection.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors of the manuscript have read and agreed to publish.
Competing interests
Prof. Zhengliang Ma is a member of the Editorial Board in Anesthesiology and Perioperative Science and recuses himself from every editorial procedure of this submission including peer-review and academic decisions. All the other authors claim that there are no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ni, K., Zhu, J. & Ma, Z. Preoperative anxiety and postoperative adverse events: a narrative overview. APS 1, 23 (2023). https://doi.org/10.1007/s44254-023-00019-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44254-023-00019-1