Abstract
Purpose
To describe the modes of death (MOD), the elements related to the decision to forgo life-sustaining treatments (LST) as well as the medical and parental environment surrounding time of death in our pediatric intensive care unit (PICU).
Methods
This is a retrospective, single-center study from a Swiss PICU. All patients between 30 days and 18 years of age who died in our PICU from 2006 to 2019 were eligible for inclusion. Data were collected from patients’ record and from a standardized death form containing information on circumstances surrounding end-of-life. Patients’ and families’ characteristics as well as trends over time of MOD were evaluated.
Results
Of 6930 PICU admissions during the whole study period, 121 (1.7%) died in our PICU. Mortality significantly decreased from 2.9% in 2006 to 1% in 2019 (p = 0.003). More than half of patients died after a decision to transition to comfort care (68.56%). Withdrawal and limitation of LST were the prevalent MOD (56%) with a significant increase in withdrawal over time. Primary diagnosis, limitation (vs. withdrawal) of LST, type of admission and families’ religious background are associated with longer latencies between admission to decision to comfort care and from decision to death. At least one parent was present in 94% of cases when LST were limited or withdrawn.
Conclusions
Most of the deaths follow LST limitation or withdrawal with increasing rates of withdrawal over time. We also showed that time latencies between admission and decision and from decision to death varies depending on MOD, patients’ characteristics and families ‘religious background.
Similar content being viewed by others
Introduction
In developed countries, most of inpatients deaths occur in intensive care [1]. When restorative care fails, the transition from cure to comfort is frequently made in pediatric intensive care units (PICU) [2]. Nonetheless the availability of advanced resuscitation measures and sophisticated life sustaining treatments may render end-of-life (EOL) decisions difficult [3]. Actually, discontinuation of life-sustaining treatments (LST) has become the most frequent mode of death in PICU [4,5,6]. The attitude towards the limitation of LST varies according to geographical and cultural factors [7,8,9]. End-of-life care for children and neonates with complex chronic conditions in Switzerland have been recently studied [10, 11]. However updated information on how children die in PICUs is lacking in our country. Moreover some details such as family’s presence at the bedside, parents ‘attitude towards limitation of LST as well as the type of limitation/withdrawal LST warrant additional exploration [12]. We encourage the continuous presence of parents in PICU and clinical decisions are shared with professionals according to a family-centered model of care [13].
The aim of this study is to describe the modes of death (MOD) and their variability overtime as well as the elements related to the decision to forgo LST. This is a descriptive study based on a standardized death form completed by the most senior attending physician after every consecutive death in our PICU. This information might add some details of value on how to improve the care of patients during the transition to EOL and through the dying process in PICU patients.
Materials and methods
Study design and population
This is a retrospective single-center observational study, where patients were recruited from the PICU of the Geneva Children’s Hospital from January 2006 to December 2019. This is a 12-bed, multidisciplinary PICU in a teaching tertiary referral children’s hospital. As neonates represented the study population of a distinct study carried out by our group, only patients between 30 days (corrected age) and 18 years of age who died in our PICU were eligible for inclusion. The local Institutional Review Board (Commission cantonale d’éthique de la recherche 2019–02,328) approved the study and waved the need for informed consent.
Data collection
Researchers collected the following data from electronic patients’ records: age, gender, length-of-stay (LOS), underlying chronic illness, technology dependence prior to PICU admission (defined as children needing medical devices at home such as home ventilation, tracheostomy, enteral or parenteral feeding or renal replacement therapy) [14], source and type (elective vs urgent) of admission, primary diagnosis, Pediatric Index of Mortality 2 (PIM2) score, shift during which the patient died (day 7:30–17:00; night 17:00–7:30) and religious affiliation [15]. In order to avoid variations in trends due to the small sample size, the study period has been divided in two blocks (from 2006 to 2012 and 2013 to 2019).
Standardized death form
The form contains data on circumstances surrounding EOL such as MOD, time from PICU admission to decision and from decision to death, parental presence, chaplain presence, whether the child was held into parents’ arms at time of death, type of LST that have been limited/withdrawn, presence of conflict between the PICU team and the family at the time of death, need for hospital ethics representatives involvement, whether an autopsy was proposed and accepted and type and dose of sedative and analgesic drugs at time of death. Every patient is classified at time of death by the attending physician according to the following mutually exclusive MOD: death despite maximal resuscitation (RES); brain death (BD); limitation (but not withdrawal) of LST (L/LST), withdrawal of LST (W/LST) [5].
Statistical analysis
Categorical and continuous variables are expressed as frequencies and percentages and as median and interquartile range (25th–75th percentiles) respectively. Differences between groups were assessed by chi-square, t test/Wilcoxon test or Mann–Whitney/Kruskal–Wallis as appropriate. All statistical tests were two-sided and a value of p < 0.05 was deemed significant. All analyses were performed using R statistical software version 3.6.0 (The R Foundation for Statistical Computing).
Results
Patients ‘characteristics and modes of death
There were 6930 PICU admissions during the whole study period, 121 (1.7%) of whom died in the PICU. Mortality significantly decreased from 2.9% in 2006 to 1% in 2019 (p for trend = 0.003). Sociodemographic and clinical characteristics of patients who died are shown in Table 1. Cardiovascular diseases were the most common underlying chronic conditions (22, 19%), followed by neurologic-neuromuscular (13, 11%) and onco-hematologic diseases (9, 7%). Underlying chronic conditions were more prevalent in RES and in L/LST patients (79% and 75% respectively) compared to BD and W/LST patients (52% and 50% respectively). Cardiovascular diseases were the most common underlying chronic condition in RES patients (9 of 28, 32%), while neurologic-neuromuscular, renal, and respiratory diseases were the most prevalent chronic conditions in the L/LST group (8 of 20, 40%). Median PIM2 risk of death was 28% among decedents with no significant changes throughout the study period (p for trend = 0.12). Median PIM2 score of patients admitted in our PICU remained also stable between 4 and 5% during the whole study period. More than half of patients died after a decision to transition to comfort care (68.6%). All characteristics of patients stratified by mode of death are summarized in Table 2.
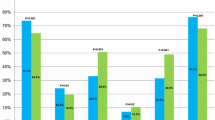
We divided the study period in two blocks (from 2006 to 2012 and 2013 to 2019). We found no significant differences between the two groups in term of age, primary diagnosis, presence of underlying chronic diseases and technology dependence. Throughout the study period, more parents decided to withdraw LST (from 30% until 2012 to 46% after 2012, p = 0.06). There was a trend toward less BD (from 24% until 2012 to 12% after 2012, p = 0.09) while L/LST (from 16% until 2012 and 22% after 2012, p = 0.40) and RES (from 31% until 2012 to 21% after 2012, p = 0.21) remained fairly stable. These trends are illustrated in Fig. 1. Underlying chronic diseases were more frequent in patients with L/LST (15, 75%) and RES (22, 79%) compared to BD (13, 52%) and W/LST (24, 50%).
Interval between admission to decision to comfort care and from decision to death
Time from admission to decision to proceed to comfort care was 4.1 (range 1.6–14.9) days for the whole cohort. A planned PICU admission (30 days vs. 15 days for urgent admissions, p = 0.004) and type of primary diagnosis (38 days for respiratory disease vs. 6 days for pre-PICU cardiorespiratory arrest, p = 0.027) were associated with longer duration between admission and comfort care decision. There was a trend towards a longer interval between admission and decision to comfort care for families with a religious background (40, 14, and 6 days for Muslim, Catholic, and families without religious preference respectively, p = 0.08).
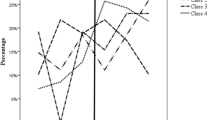
Median duration from decision to comfort care to death was 1 (range 0–8) day. In particular this time interval was 4 h in case of W/LST and 6 days for L/LST. Table 3 shows time interval difference according to limitation and withdrawal of LST. Families with a religious background experienced a significantly longer time latency between decision and death (24, 12, and 6 days for Muslim, Catholic, and families without religious preference respectively, p = 0.009).
Circumstances of death during L/LST and W/LST
No conflict between the PICU team and the family regarding the decision to limit or withdraw LST was recorded at time of death. In 26% (18 of 68) of cases, the parents made the decision to L/LST or W/LST to which the PICU team agreed, considering the decision to be in the patient’s best interest. In the remaining 50 (74%) of cases, a consensual decision was reached after guidance was provided by the PICU team. For L/LST patients, the most frequent type of LST limitation was non-initiation of cardiopulmonary resuscitation (CPR) (13, 74%), followed by non-initiation of vasoactive drugs (11, 65%) and non-initiation of mechanical ventilation (MV) (7, 35%). The most frequent type of W/LST was the withdrawal of MV (37, 77%) followed by the withdrawal of vasoactive drugs (20, 42%). In 82% (56 of 68) of the patients for which information on sedation and analgesia around the time of death was available, the most frequently used were opioids in 82% (56 of 68) of patients as a continuous infusion. Among opioids, morphine was the molecule of choice in 59% (40 of 68) of cases. Benzodiazepines (midazolam) were used as a continuous infusion in 45% (31 of 68). Neuromuscular blockade drugs were never used at time of death. At least one parent was present in 94% (64 of 68) of cases when LST were limited or withdrawn, with no difference between L/LST and W/LST. Chaplains were present in 32% (22 of 68) of cases. Thirty-five percent (24 of 68) of patients in the L/LST and W/LST groups died in parent’s arms. Hospital ethics representatives were involved in 5% (6 of 121) of cases. Autopsy was demanded by medical team in 85 patients (70%) and was accepted in 40 cases (47%). Judicial review was not required in any case.
Discussion
The main findings of our single-center retrospective study of circumstances surrounding death in our PICU are as follows: (1) L/LST and W/LST are the prevalent MOD. Withdrawal of LST, in particular, significantly increased during the study period; (2) type of admission, primary diagnosis and religious background might influence intervals between admission to decision to comfort care and from decision to death.
Patients’ characteristics and modes of death
Most deaths in our PICU follow W/LST and L/LST. Several reports suggest that in recent years an increasing percentage of deaths occur after limitation or withdrawal of support [4, 16]. The proportion of patients undergoing W/LST in our cohort (40%) are comparable with reports from the USA, the UK, and Australia [2, 5, 17].
The unchanged PIM2 score among PICU admissions throughout the study period and the concomitant decrease in the unadjusted mortality rate over this period indicates that more patients with analogous severity of illness are surviving. Improved PICU management might explain this reduction in mortality. This tendency may also mirror an increasing acceptance of survival with more severe disability by parents [3]. During the study period, we also observed a stable illness severity among decedents along with a rise in W/LST. This may imply that W/LST is increasingly accepted by parents. Conversely the lack of a significant decrease in RES in the presence of stable PIM2 scores points at acute in-hospital resuscitation outcomes and the availability of extracorporeal cardiopulmonary resuscitation as areas of potential improvements. Our results show that the majority of the deaths occurred among patients with underlying chronic diseases thus confirming previous reports [10, 18]. The prevalence of cardiac disorders, where rapid deterioration is possible, as the main type of chronic disease among RES patients might explain the high percentage of pre-existing chronic conditions in this group. On the other hand, complex conditions such as neurologic-neuromuscular or respiratory diseases were more frequent in the L/LST group. The slowly progressive nature of some of those conditions may possibly allow extra time for families to come to terms with unavoidable deaths and choose transition to comfort care.
The mortality rate of our cohort throughout the study period is not significantly different from the overall mortality that has been recently described in Switzerland between 2012 and 2017 (1.7% vs. 2% respectively) [19]. The mortality rate in 2019 in our unit was particularly low. We have no clear explanation for that as the sickest children in the region come to our unit. It is possible that small variations in the number of deaths and/or in the number of patients admitted might produce larger fluctuations in mortality rates in units dealing with a relatively limited number of patients as ours.
Time of death
Interval between admission to decision to comfort care
Longer duration between admission and decision to forgo LST was associated with elective PICU admissions, which in our unit mainly concern post-operative patients. Families may indeed need extra time to come to terms with their child’s unavoidable death after an elective procedure, regardless of surgical complexity. On the contrary, decision to limit LST was taken earlier for patients who received CPR before PICU admission. It is likely that death appeared inevitable for those patients.
Interval from decision to comfort care to death
The present study also confirms other reports suggesting that L/LST and W/LST are clinically different as withdrawal of LST is actually associated with earlier mortality compared to L/LST [20, 21]. The duration between the time of decision and actual death was indeed very short (4 h) after W/LST and was significantly shorter than after L/LST (6.5 days). Others reported comparable results with a median duration going from 30 min to 3 h [10, 12, 22]. Severity of illness as measured by the PIM2 score was higher in the W/LST group than in the L/LST group. The shorter interval in the W/LST group may therefore indicate that those children were significantly sicker at the time of the decision. The association between families’ religious backgrounds with longer duration from decision to actual death merits consideration. It is possible that some extra time is given to religious families in order to implement rituals, sacred readings, prayers, or sacraments around the time of death of their child [23]. We reported longer intervals from decision to comfort care to death for Muslim families. Muslim patients may provide challenges for many non-Muslim healthcare providers [24]. The act on the decision to comfort care might therefore be delayed as a consequence of misunderstandings between families and clinicians resulting from inadequate knowledge of specific beliefs and behaviors and/or the presence of a linguistic barrier. Unaddressed spiritual needs are associated with poorer quality of life of patients and their families and the provision of spiritual care might improve EOL outcomes such as the perception of compassionate and patient-centered care [25]. Understanding the patient’s values and religious traditions may reduce conflicts with the medical and nursing staff [26]. We believe that the systematic incorporation of spiritual care into medical care of seriously ill patients should be enabled in order to allow a more individualized approach to EOL care [27]. We systematically offer spiritual support to families in the form of access to multi-faith chaplaincy services. This may explain the relatively high rate of chaplain presence at the time of the patient’s death.
Circumstances of death during L/LST and W/LST
In our PICU, communication with families occurs at formal meetings as well as at the bedside and decisions are shared with parents. Nurses and residents are encouraged to participate in formal meetings with parents. A summary of the discussion is added to the clinical record of the patient at the end of every formal meeting. Differences between parents and clinicians concerning interventions that the PICU team considered inadvisable occurred in a few cases. In these cases, several formal meetings and the implication of hospital ethics representatives aimed at clarifying the objectives of care have been necessary to reach a consensus between clinicians and families. Unfortunately, the incidence of such conflicts as well as the number of meetings was not available for analysis.
In our unit, mechanical ventilation and vasopressors are usually withdrawn sequentially in accordance with recommendations for the withdrawal of LST [28]. Paralyzing agents were not used at the time of W/LST as we believe that they serve no purpose in these circumstances [29].
In our study, at least one parent was present in almost all cases after L/LST or W/LST. The family presence at the bedside should be enabled as it may help reduce the feelings of disempowerment and threatened parental role by the PICU environment and the actions of the staff [18]. Also, the possibility for the parents to hold the child at time of death might help maintaining the parental role through the participation to the care of their child. Nonetheless, only one third of patients died into their parents’ arms during the study period. Parents’ choice not to hold the child at the time of death is respected in our PICU. Unfortunately, we are not able to analyze the reasons behind this particular parents’ decision.
This study has limitations. This is a single center retrospective study with limited generalizability and possible incomplete or missing documentation. Patients who may have been discharged home to die are anecdotal in our PICU. Nonetheless, those patients are not included in this database. No information on patients’ functional status, previous PICU admission, number of family meetings and clinicians who attended to them is recorded. Data on pediatric palliative care are not reported as this program has only recently been implemented in our center. Attending physicians share common definitions of MOD. Moreover, the standardized death remained unchanged throughout the study period. Nonetheless, misclassification of MOD cannot be ruled out. Longer intervals between admission to decision to comfort care might also be explained by clinical complications occurring during the same period of time. Our data cannot provide information on complications arising during the PICU admission. The care of the dying child is fraught with challenges for healthcare professionals. In the case of particularly complex ethical situations, clinicians may need more time to reach a shared decision and eventually discuss an end-of-life care plan with the family. This might in turn further prolong the interval between admission to decision to comfort care. Again, we are not able to provide information on that point. We systematically ask parents if they would like to eventually discuss about their experience with the attending physician in charge at the time of death of their child and we offer the possibility of visiting the unit. The choice of whether contacting the PICU staff and the timing is left to the parents. Data on parents’ follow-up are unfortunately not available. We were not able to provide the proportion of organ donation requests and acceptance as this information was not available for 84% of patients.
Conclusions
Most of the deaths follow treatment limitation or withdrawal in our PICU with increasing rates of W/LST. Time latencies between admission and decision and from decision to death varies depending on MOD, patients’ characteristics and families ‘religious background. Incomplete knowledge of the factors that contribute to decision-making surrounding EOL suggests the need for additional multicenter research along the lines of what has already been done in the EURYDICE II study in 2011 [30]. Research on the possible benefits of the incorporation of cultural and religious competences to adapt EOL care to families’ background merits further attention.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon request.
References
Fraser J, Sidebotham P, Frederick J, Covington T, Mitchell EA (2014) Learning from child death review in the USA, England, Australia, and New Zealand. Lancet 384(9946):894–903. https://doi.org/10.1016/S0140-6736(13)61089-2
Burns JP, Sellers DE, Meyer EC, Lewis-Newby M, Truog RD (2014) Epidemiology of Death in the PICU at Five U.S. Teaching Hospitals*. Crit Care Med 42(9):9. https://doi.org/10.1097/CCM.0000000000000498
Laussen PC (2016) Modes and causes of death in pediatric cardiac intensive care: digging deeper*. Pediatr Crit Care Med 17(5):461–462. https://doi.org/10.1097/PCC.0000000000000711
Trowbridge A, Walter JK, McConathey E, Morrison W, Feudtner C (2019) Modes of death within a children’s hospital. Pediatrics 142(4):e20174182. https://doi.org/10.1542/peds.2017-4182
Moynihan KM et al (2019) Epidemiology of childhood death in Australian and New Zealand intensive care units. Intensive Care Med 45(9):9. https://doi.org/10.1007/s00134-019-05675-1
Meert KL et al (2015) End-of-life practices among tertiary care PICUs in the United States: a multicenter study. Pediatr. Crit. Care Med 16(7):7. https://doi.org/10.1097/PCC.0000000000000520
Kipper DJ et al (2005) Evolution of the medical practices and modes of death on pediatric intensive care units in southern Brazil*. Pediatr. Crit. Care Med 6(3):3. https://doi.org/10.1097/01.PCC.0000154958.71041.37
Suzuki F, Takeuchi M, Tachibana K, Isaka K, Inata Y, Kinouchi K (2018) Life-sustaining treatment status at the time of death in a Japanese pediatric intensive care unit. Am. J. Hosp. Palliat. Care 35(5):767–71. https://doi.org/10.1177/1049909117743474
Devictor DJ, Nguyen DT (2004) Forgoing life-sustaining treatments in children: a comparison between Northern and Southern European pediatric intensive care units. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc 5(3):211–5. https://doi.org/10.1097/01.PCC.0000123553.22405.E3
Ramelet AS et al (2020) Comparison of end-of-life care practices between children with complex chronic conditions and neonates dying in an ICU versus non-ICUs: a substudy of the pediatric end-of-life care needs in Switzerland (PELICAN) Project*. Pediatr Crit Care Med 21(5):5. https://doi.org/10.1097/PCC.0000000000002259
Zimmermann K et al (2016) When parents face the death of their child: a nationwide cross-sectional survey of parental perspectives on their child’s end-of life care. BMC Palliat Care 15:30. https://doi.org/10.1186/s12904-016-0098-3
Garros D, Rosychuk RJ, Cox PN (2003) Circumstances surrounding end of life in a pediatric intensive care unit. Pediatrics 112(5):e371. https://doi.org/10.1542/peds.112.5.e371
October TW, Hinds PS, Wang J, Dizon ZB, Cheng YI, Roter DL (2016) Parent satisfaction with communication is associated with physician patient-centered communication patterns during family conferences. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc 17(6):490–497. https://doi.org/10.1097/PCC.0000000000000719
Alexander D, et al., Initiating technology dependence to sustain a child’s life: a systematic review of reasons. J Med Ethics p medethics. 2021:2020–107099 https://doi.org/10.1136/medethics-2020-107099.
Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D (2014) Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr 14(1):199. https://doi.org/10.1186/1471-2431-14-199
Narayanan A, Thorburn K, Baines P (2009) Autopsies in children continue to reveal unanticipated discrepancies between autopsy findings and antemortem clinical diagnoses. Arch Dis Child 94(8):645. https://doi.org/10.1136/adc.2008.150417
Sands R, Manning JC, Vyas H, Rashid A (2009) Characteristics of deaths in paediatric intensive care: a 10-year study. Nurs Crit Care 14(5):235–240. https://doi.org/10.1111/j.1478-5153.2009.00348.x
Butler AE, Hall H, Willetts G, Copnell B (2015) Family experience and PICU death: a meta-Synthesis. Pediatrics 136(4):e961-973. https://doi.org/10.1542/peds.2015-1068
Polito A, Giacobino C, Combescure C, Levy-Jamet Y, Rimensberger P, Swiss Society of Intensive Care Medicine (2020) Overall and subgroup specific performance of the pediatric index of mortality 2 score in Switzerland: a national multicenter study. Eur. J. Pediatr. 179(10):1515–1521. https://doi.org/10.1007/s00431-020-03639-y
Sprung CL et al (2003) End-of-life practices in European intensive care units: the Ethicus Study. JAMA 290(6):790–797. https://doi.org/10.1001/jama.290.6.790
Ferrand E, Robert R, Ingrand P, Lemaire F (2001) Withholding and withdrawal of life support in intensive-care units in France: a prospective survey. French LATAREA Group. Lancet Lond Engl 357(9249):9–14. https://doi.org/10.1016/s0140-6736(00)03564-9
Zawistowski CA, DeVita MA (2004) A descriptive study of children dying in the pediatric intensive care unit after withdrawal of life-sustaining treatment. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc 5(3):216–223. https://doi.org/10.1097/01.pcc.0000123547.28099.44
Oppenheim A, Sprung CL (1998) Cross-cultural ethical decision-making in critical care. Crit Care Med 26(3):423–424. https://doi.org/10.1097/00003246-199803000-00003
B Attum, S Hafiz, A Malik, Z Shamoon. Cultural competence in the care of Muslim patients and their families, in StatPearls, Treasure Island (FL): StatPearls Publishing, 2022. Consulté le: 22 février 2023.. Disponible sur: http://www.ncbi.nlm.nih.gov/books/NBK499933/
Puchalski CM, Vitillo R, Hull SK, Reller N (2014) Improving the spiritual dimension of whole person care: reaching national and international consensus. J Palliat Med 17(6):642–656. https://doi.org/10.1089/jpm.2014.9427
Inwald D, Jakobovits I, Petros A (2000) Brain stem death: managing care when accepted medical guidelines and religious beliefs are in conflict Consideration and compromise are possible. Bmj 320(7244):1266–1267. https://doi.org/10.1136/bmj.320.7244.1266
Balboni TA et al (2022) Spirituality in serious illness and health. JAMA 328(2):184–197. https://doi.org/10.1001/jama.2022.11086
Downar J, Delaney JW, Hawryluck L, Kenny L (2016) Guidelines for the withdrawal of life-sustaining measures. Intensive Care Med 42(6):1003–1017. https://doi.org/10.1007/s00134-016-4330-7
Truog RD et al (2008) Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American College [corrected] of Critical Care Medicine. Crit Care Med 36(3):953–963. https://doi.org/10.1097/CCM.0B013E3181659096
Devictor DJ, Latour JM (2011) Forgoing life support: how the decision is made in European pediatric intensive care units. Intensive Care Med 37(11):1881–1887. https://doi.org/10.1007/s00134-011-2357-3
Code availability
Not applicable.
Funding
We have no fundings to declare.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Cristian Ghinescu, Aurélie Wanders, and Angelo Polito. The first draft of the manuscript was written by Aurélie Wanders and Angelo Polito and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The local Institutional Review Board (Commission cantonale d’éthique de la recherche 2019–02328) approved the study and waved the need for informed consent.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wanders, A., Ghinescu, C., Levy-Jamet, Y. et al. Circumstances surrounding end of life in a Swiss pediatric intensive care unit. Intensive Care Med. Paediatr. Neonatal 1, 7 (2023). https://doi.org/10.1007/s44253-023-00005-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44253-023-00005-2