Abstract
Background
The objective of this study was to evaluate the impact of nursing interventions on sleep quality in hospitalized patients.
Methods
A comprehensive literature search was conducted, encompassing databases such as PubMed/MEDLINE, Scopus, Web of Science, EMBASE, ProQuest, Science Direct, and Cochrane Library, with publications up until September 2022 being considered. A random-effects model was utilized to calculate standardized mean differences (SMD) and 95% confidence intervals (CIs) for continuous outcomes.
Results
A total of 77 studies involving 7771 participants were included in the systematic review. Among these, 18 studies met the inclusion criteria for the meta-analysis, involving a total of 1153 participants. The meta-analysis results indicated a positive effect of nursing interventions on sleep quality, as measured by the Pittsburgh Sleep Quality Index (PSQI) score (SMD = −4.21, 95% CI = −5.75 to −2.67, P < 0.001), and the St. Mary’s Hospital Sleep Questionnaire (SMHSQ) (SMD = −1.87, 95% CI = −2.77 to −0.98, P < 0.001). However, there was substantial heterogeneity observed among the studies (I2 = 97.8%, P < 0.001 and I2 = 93.5%, P < 0.001, respectively). While a significant number of individual studies demonstrated that nursing interventions improved both sleep quantity and quality in hospitalized patients.
Conclusions
The meta-analysis identified three specific interventions; relaxation, music therapy, and the use of earplugs/eye masks, that had a positive impact on sleep quantity and quality. It is important to acknowledge that due to variations in methodological quality and heterogeneity among the included studies, drawing definitive conclusions regarding the effectiveness of different interventions is challenging, and interpreting the results with caution is necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Sleep quality plays a crucial role in the recovery of patients within a hospital setting. Adequate sleep promotes physiological, cognitive, and emotional restoration, which are essential for the healing process [1, 2]. Conversely, inadequate sleep quality can lead to negative consequences such as immune suppression, impaired wound healing, heightened pain perception, delirium, and prolonged hospital stays [3]. In addition, hospitalized patients often experience environmental factors that can disrupt their sleep, including noise, light, frequent interruptions, and uncomfortable bedding [4, 5]. Therefore, healthcare providers should prioritize the implementation of strategies aimed at improving sleep quality for hospitalized patients.
Given the significant impact of sleep quality on patient outcomes, it is crucial for healthcare providers to integrate sleep promotion into routine care practices. Nursing interventions, including non-pharmacological approaches, aim to mitigate environmental factors that can disrupt patients’ sleep, such as noise and light exposure [6]. These interventions also involve promoting good sleep hygiene by establishing regular sleep–wake cycles and providing designated quiet time. Furthermore, physical devices like earplugs and eye masks [7, 8], as well as relaxation techniques such as massage therapy, muscle relaxation, imagery, and therapeutic touch, can be utilized to alleviate the negative effects of poor sleep in hospital settings [9, 10]. Alternative therapies like aromatherapy and acupuncture have also been suggested as potential strategies to improve sleep quality for patients [11].
Several systematic reviews have highlighted the effectiveness of nursing interventions in improving sleep among various patient populations [12,13,14]. However, previous studies have reported that clinical data available at the time were insufficient, and further Randomized Controlled Trials (RCTs) were needed to assess efficacy. Consequently, there is limited conclusive evidence regarding the effectiveness of nursing interventions in enhancing sleep quality among hospitalized patients. Therefore, conducting this study was crucial for reviewing recent research. The primary objective of this systematic review and meta-analysis was to determine whether there is substantial scientific evidence indicating that nursing interventions have a positive impact on sleep quality in hospitalized patients. Hence, the purpose of this investigation was to identify, analyze, and compare all existing research related to this inquiry. To the best of our knowledge, this is the most comprehensive and inclusive systematic review and meta-analysis conducted to examine this issue.
2 Participants and Methods
2.1 Study Design
This study followed the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) statement [15]. The study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database (CRD42020145830), and ethical approval for the study was obtained from the research ethics committee of Baqiyatallah University of Medical Sciences under the ethics code IR.BMSU.REC.1398.175.
2.2 Search Strategy
The databases PubMed/MEDLINE, Scopus, Web of Science, EMBASE, ProQuest, Science Direct, and Cochrane Library were searched for publications up to September 2022. The search strategy involved the use of MeSH terms and keywords such as “sleep disorder” OR “sleep deprivation” OR “sleep apnea” OR “insomnia” OR “sleep latency” OR “rapid eye movement” OR “non-rapid eye movement” OR “sleep stage” OR “sleep quality” OR “sleep time” OR “sleep wake disorder” AND “intensive care” OR “intensive care unit” OR “critical care” OR “ICU” OR “CCU” OR “Hospitalized patients” OR “critical patients” OR “non-critical patients” AND “nursing interventions” OR “non-pharmacological interventions” OR “alternative therapies” OR “music therapy” OR “massage therapy” OR “muscle relaxation” OR “cognitive therapy” OR “behavior therapy” OR “physical therapy” OR “aromatherapy” OR “acupuncture” OR “eye masks” OR “earplugs". To further identify potentially relevant studies, primary article references were also reviewed. All relevant articles that met predefined selection criteria were evaluated.
2.3 Eligibility Criteria
The inclusion and exclusion criteria for eligible studies were as follows: (a) studies had to fall into the following categories: randomized controlled trials (RCTs), randomized crossover studies, cluster randomized trials, or randomized or non-randomized quasi-experimental studies with control groups. These studies aimed to assess the effect of nursing interventions on adult patients; (b) participants in the studies had to be adult patients, both critical and non-critical, who were hospitalized for a minimum of 72 h and had stable hemodynamic status. There were no restrictions based on gender or ethnicity; (c) the nursing interventions or non-pharmacological therapies considered included the use of physical devices such as earplugs and eye masks, relaxation techniques like massage therapy, muscle relaxation, imagery, yoga, stretching exercises, resistance training, and therapeutic touch, and improvement of sleep hygiene or reduction of disturbing environmental factors including noise reduction, lighting control, quiet time, and synchronization of ICU activities with daylight. Equipment modification such as ventilator mode or type, and alternative therapies like aromatherapy and acupuncture were also considered; (d) Studies had to report changes in both objective and subjective sleep variables, which were measured using standardized instruments. Exclusion criteria comprised of (a) participants diagnosed with obstructive sleep apnea, dementia or any prior sleep disorder diagnosis; (b) those who were terminally ill or required palliative care; (c) conference articles, abstracts, and protocols; (d) studies that were not written in English or Persian.
2.4 Data Extraction
The process of data extraction was conducted in three stages. Initially, all seven scientific databases were examined, and duplicate studies were removed. In the second stage, two researchers independently searched for studies using the title and abstract to identify relevant articles. In the third stage, two investigators reviewed the full text of the remaining articles to determine if they met the inclusion criteria for the review. To extract the data from the selected studies, a pre-designed form was used which contained details such as author’s name, year of study, study type, study setting, sample size, type of intervention, type of assessment instrument, and sleep quality outcomes in both intervention and control groups before and after the intervention. In case of any ambiguities or disagreements between the reviewers, these were resolved through discussion and consensus.
2.5 Quality Assessment
The methodological quality of the included manuscripts was assessed independently by two authors using the Jadad rating scale [16], and Joanna Briggs Institute (JBI) critical appraisal tool for randomized controlled trials (RCTs) and quasi-experimental studies, respectively. Jadad scale is a three‐item, validated, and reliable scoring tool that focuses on randomization, blinding, and withdrawals/dropouts. Studies can be given an overall score from 0 to 5, with a score of 5 being an ideal score and a score of ≥3 considered to be high quality [17] (Supplementary file, Table S1). Disagreements between researchers were resolved by discussion. Quasi-experimental studies were evaluated using nine criteria based on the JBI Critical Appraisal Tool. All questions were answered as yes, no, not clear, or not applicable and assessed individually. After evaluating all the components of the study, the overall rating was determined using the criteria set out in the tool. Based on the number of “yes” responses, a rating of good = (≥7 yes), medium = (4–6) and poor = (≤3 yes) (Supplementary file, Table S2).
2.6 Statistical Analysis
STATA version 17 (Stata Corp; College Station; TX, USA) was used to calculate pooled standard mean differences (SMDs) and 95% CIs for continuous outcomes. Studies were included for quantitative analysis if mean values and SDs of the sleep scores were reported based on two types of sleep quality tools; Pittsburgh Sleep Quality Index (PSQI) or St. Mary’s Hospital Sleep Questionnaire (SMHSQ). The primary analysis included meta-analysis for sleep quality and quantity. In addition, subgroups analysis was carried out based on the type of nursing interventions which were divided into five subgroups; (1) using eye masks and earplugs, (2) relaxation techniques, (3) music intervention, (4) aromatherapy and (5) acupressure. The standardized mean difference (SMD) was calculated as the main outcome summary statistic, using a random-effects model to account for inter-study heterogeneity and to account for the overall effect of the intervention on sleep quality and quantity. The between-study variance was estimated using the restricted maximum likelihood method. The level of heterogeneity among trials was assessed using the Cochran Q test and I-squared (I2) statistics [18]. Chi2 statistic with a P value <0.10 or an inconsistency between studies I2 > 50% was considered as significant heterogeneity. Significance results of the test and values higher than 75% for I2 indicated substantial heterogeneity.
A sensitivity analysis was performed, removing each study in turn and recomputing the pooled estimates to determine the impact of each study. Analyses were performed to identify discordant studies using techniques based on the leave-one-out method to guide model review and identify studies that most impacted the overall estimates of the meta-analysis [19]. In addition, a cumulative meta-analysis was also performed by sorting studies by year of publication. To assess publication bias, we used funnel plots. Potential publication bias was assessed using Egger’s test (linear regression method) [20], and Begg’s test (rank correlation method) [21]. To assess the sources of heterogeneity, the meta-regression analysis was performed using sample size as the independent variable and the effect size (ES) as the dependent variable in the model.
3 Results
3.1 Search Outcomes
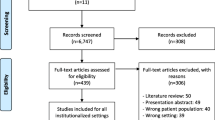
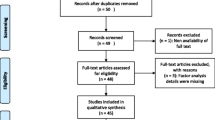
The search conducted in English and Persian languages yielded 17,754 and 1056 articles, respectively. After removing duplicates and irrelevant studies, a total of 647 articles remained for full-text evaluation. Among of these, 570 articles were excluded as they did not meet all the inclusion criteria. Finally, 77 full-text articles were included in the study. Most of the included studies were limited to qualitative synthesis due to the absence of control groups, lack of sleep quality scores before intervention, and reliance on self-reported outcomes. Therefore, only 18 studies, which utilized various sleep quality assessment tools, were suitable for quantitative synthesis. The remaining studies (n = 59) were included in the qualitative analysis. A summary of the literature search results and screening process can be found in Fig. 1.
3.2 Characteristics of Included Studies in the Quantitative Synthesis
In this study, a total of 77 studies were included, out of which 18 studies involving 1153 participants were included in the meta-analysis [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]. The characteristics of these 18 studies are presented in Table 1. Among them, 14 were randomized trials [23,24,25,26,27,28,29,30,31,32,33,34,35,36], and 4 were quasi-randomized trial studies [22, 37,38,39]. All 18 trials used subjective sleep scales to measure sleep quality; seven trials used St. Mary’s Hospital Sleep Questionnaire (SMHSQ) [23, 25, 28, 29, 33, 34, 37], while eleven studies employed the Pittsburgh Sleep Quality Index (PSQI) scale [22, 24, 26, 27, 30,31,32, 35, 36, 38, 39]. The number of participants per study ranged from a minimum of 40 to a maximum of 80. The majority of trials focused on patients admitted to coronary care units (CCUs), except for two trials conducted in intensive care units (ICUs) [24] and in a non-ICU [39]. Various interventions were studied across the included trials. We identified five trials that employed earplugs, eye masks, or a combination of both [22, 27, 31, 32, 38], three trials that investigated music interventions [26, 30, 39], three trials that examined relaxation technique [33, 35, 37], one trial that explored acupressure [23], one trial that implemented quiet time [25], and five trials that investigated the use of aromatherapy with lavender [24, 28, 29, 34, 36].
3.3 Overall and Subgroup Meta-analysis
Eleven studies with 756 participants and seven studies with 446 participants reported data on sleep outcomes using the PSQI and SMHSQ scales, respectively. The pooled SMD analysis between intervention and control groups showed a positive effect of nursing interventions on sleep quality based on PSQI scores (SMD = −4.21, 95% CI = −5.75 to −2.67, P < 0.001) and SMHSQ scores (SMD = −1.87, 95% CI = −2.77 to −0.98, P < 0.001), with substantially heterogeneity among the studies (I2 = 97.8%, P < 0.001 and I2 = 93.5%, P < 0.001), respectively (Fig. 2A, B). The results showed that the mean scores of PSQI and SMHSQ of the intervention groups were 4.21 and 1.87 points lower, respectively, compared to the control groups. In both PSQI and SMHSQ instruments, a lower score indicates better sleep quality, so the results indicate an improvement in overall sleep quality in the intervention groups.
Next, we carried out subgroup analyses by types of nursing interventions according to PSQI (Fig. 3). In the subgroup analyses separated by nursing interventions, positive effects on sleep quality were observed in studies that used earplug and eye mask device (SMD = −4.02, 95% CI = −6.02 to −1.12, I2 = 98.42%, P < 0.001), aromatherapy intervention (SMD = −3.88, 95% CI = −7.67 to −0.09, I2 = 97.45%, P < 0.001), and music therapy (SMD = −4.53, 95% CI = −7.69 to −1.36, I2 = 98.42%, P < 0.001) to improve sleep quality in hospitalized patients using the PSQI. In addition, according to pooled analysis based on SMHSQ (Fig. 4), relaxation technique had positive effects on sleep quality in hospitalized patients (SMD = −2.76, 95% CI = −3.45 to −2.07, I2 = 69.96%, P < 0.001). However, three trials showed no effects of aromatherapy on sleep quality (SMD = −1.28, 95% CI = −2.84 to 0.29, I2 = 95.17%, P = 0.065).
3.4 Sensitivity Analysis
In the overall analyses, when considering the sleep quality assessment tools used, substantial heterogeneities were observed among studies utilizing the PSQI (I2 = 98.45%, P < 0.001) and the SMHSQ (I2 = 95.17%, P < 0.001). To investigate the influence of each individual study on the SMD, we conducted additional meta-analyses by omitting each study one at a time. The results showed that the studies by Zolfaghari et al. [38], and Farokhnejhad Afshar [39], had the most substantial impact on the total index. These two studies overestimated the effect size in terms of improving sleep quality. When excluding these two studies, the estimate became borderline significant (SMD = −4.14, 95% CI = −5.25 to −3.03) (Supplementary file, Figure S1A). Regarding the studies assessing sleep quality based on the SMHSQ, the study by Otaghi et al. [34], had the greatest impact on the overall SMD. This particular study overestimated the magnitude of the impact on improving sleep quality (SMD = −1.87, 95% CI = −2.82 to −0.91) (Supplementary file, Figure S1B).
3.5 Cumulative Meta-analysis
A cumulative meta-analysis was performed by repeatedly conducting the meta-analysis with the addition of new studies. We conducted a cumulative meta-analysis based on the publication year of the included studies. The findings suggest that the effect of nursing interventions on patients’ sleep quality experienced a temporary decrease between 2012–2014 and 2018–2020 (Supplementary file, Figure S2A). When considering the data from the SMHSQ, there appears to be a decline in the effectiveness of nursing interventions over time, spanning from 2011 to 2021. However, this reduction in effectiveness did not reach statistical significance. Overall, the cumulative SMD of sleep quality did not exhibit a discernible trend over time, with no significant differences observed (Supplementary file, Figure S2A).
3.6 Publication Bias
In 11 studies that reported the SMD of nursing interventions on sleep quality among experimental and control groups based on PSQI, the funnel plots, Begg’s (P < 0.001) and Egger’s (P = 0.003) tests showed some publication bias (Supplementary file, Figure S3A). In 7 studies that reported the SMD of nursing interventions on sleep quality based on SMHSQ, the funnel plots showed asymmetric mood and confirmed presence of publication bias. In addition, the Begg’s (P = 0.006) and Egger’s (P < 0.001) tests showed a publication bias (Supplementary file, Figure S3B).
3.7 Explore Heterogeneity
Meta-regression analysis was performed to find the source of heterogeneity among the trials that reported the sleep quality after nursing interventions based on PSQI and SMHSQ. The year of the study, sample size, age, gender and marital status of the subjects in each group (experimental and control groups), were used for exploration the heterogeneity. The results of meta-regression analysis are presented in (Supplementary file, Table S3). While there were an association between age [age in control group (P = 0.036), and age in intervention group (P = 0.031)] and male gender [male gender in control group (P = 0.039), and male gender in intervention group (P = 0.044)] with improvement of sleep quality based on PSQI, no such association was observed between variables and outcome in studies that reported the sleep quality based on SMHSQ.
3.8 Characteristics of Included Studies in the Qualitative Synthesis
Fifty-nine studies with 6618 participants were included in the systematic review [40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98]. The characteristics of 59 studies are presented in (Supplementary file, Table S4). The sleep scales varied among these trials; but the majority of trials used subjective sleep scales to measure sleep quality. Among the subjective tools for sleep evaluation, the Richards Campbell Sleep Questionnaire (RCSQ) (n = 14) [42, 45, 54, 60, 64, 65, 68, 69, 72, 77, 90, 94, 95], and the Veran Snyder-Halpern subjective sleep quality questionnaire (VSHSS) (n = 13) [40, 44, 47, 49, 50, 67, 73, 80, 82, 85,86,87, 92], were the most frequently used. Six trials used the PSQI scale [46, 53, 59, 66, 81], and four trials used SMHSQ [33, 89, 91, 97]. On the other hand, among the objective tools for sleep evaluation polysomnography (PSG) (n = 7) [43, 51, 56, 57, 75, 78, 88], was the most frequently used. A trial used electroencephalography (EEG) [56], Actigraphy [48], and Bispectral index (BIS) [61] for sleep assessment. In addition, five studies used an author-designed sleep questionnaire [63, 70, 71, 83, 84], and ten studies used variable assessment tools such as Epworth Sleepiness Scale (ESS) [52, 58, 76], Hospital Sleep Quality Questionnaire [74, 96], Sleep Efficiency Index (SEI) [79], Glide well Rapid Sleep Screening (GRSS) [62], Groningen Sleep Quality Scale (GSQS) [93], and Psychometric properties of the Patient-Reported Outcomes Measurement Information System (PROMIS) sleep disturbance questionnaire [55].
3.9 Qualitative Reporting of Results
The 59 articles were sorted by type of nursing interventions and are presented in the following categories: sleep hygiene interventions (n = 12) [33, 42, 47, 52, 57, 58, 64, 69, 72, 79, 84, 90], earplugs or eye masks or both interventions (n = 12) [44, 51, 63, 67, 70, 71, 73, 83, 86, 87, 92], aromatherapy interventions (n = 10) [40, 45, 49, 50, 66, 74, 77, 94, 96, 97], music interventions (n = 6) [59,60,61, 68, 85, 88], acupressure intervention (n = 2) [48, 91], relaxation techniques (n = 7) [41, 75, 76, 80,81,82, 89], ventilator mode interventions (n = 2) [43, 78], protective care and behavioral interventions (n = 4) [54, 62, 65, 93], and studies that used multi-interventions compare with routine care (n = 4) [46, 55, 56, 95].
3.10 Sleep Hygiene Interventions
Sleep hygiene or reduced sleep interruption programs attempt to reduce the number of elements that can disrupt sleep, both in the environment and on a personal level. Quite time, noise reduction, lighting control, synchronization of ICU activities with daylight, regulation of room temperature for greater comfort, avoidance of daytime napping, and engaging in physical exercise throughout the day are examples of such interventions. We identified 12 studies [33, 42, 47, 52, 57, 58, 64, 69, 72, 79, 84, 90], that examined the effect of sleep hygienic interventions on patients’ sleep quality, which included noise reduction and light control [52, 79, 98], controlling night‐time noise and activities [72], night noise reduction [64, 90], quiet time [47, 58, 69, 84], and separation room of patients [57]. Out of 12 studies, 10 (83.3%) studies indicated that the sleep hygiene interventions are easy to apply and effective in improving the sleep quality. However, two trials by Diaz Alonso [52], and Van de pol et al. [90], did not find that reducing night noise was effective in improving patients’ sleep quality.
3.11 Earplugs or Eye Masks or Both Interventions
Eleven studies reported the efficacy of eye masks, earplugs or both interventions on subjective sleep quality using the PSQI [53], VSHSS [44, 67, 73, 86, 87, 92], and an author-designed sleep questionnaire [63, 70, 71, 83]. Additionally, a study showed the positive effect of eye masks or earplugs or both on objective sleep variables as measured using PSG [51]. Due to clinical heterogeneity in study design and different types of assessment tools, the results from these studies could not be statistically combined. However, all of these studies (100%) show that the use of eye masks or earplugs, or both, contributes to patients’ sleep quality.
3.12 Aromatherapy Intervention
Ten studies compared aromatherapy intervention to usual care and measured perceived sleep quality using various assessment tools, including VSHSS [40, 49, 50], RCSQ [45, 77, 94], PSQI [66], SMHSQ [97], and the Sleep Hospital Quality Questionnaire [74, 96]. Two studies used hybrid aromatherapy [40, 49], six studies used lavender [45, 50, 66, 74, 77, 94], one trial used damask rose extract [97], and another used “Citrus Aurantium” aroma [96]. The majority of results (nine out of ten studies) showed that aromatherapy, as a cost-effective and uncomplicated method, can improve the sleep quality of hospitalized patients [40, 45, 49, 50, 66, 74, 77, 96, 97]. However, Borromeo et al.’s study [94] revealed that passively diffused aromatherapy using lavender did not significantly affect sleep quality in CCU patients. Thus, 91.7% of studies reported aromatherapy as an effective intervention.
3.13 Music Intervention
Six studies investigated the impact of music therapy versus usual care on patients’ sleep quality. Four of these studies assessed subjective sleep variables using tools like PSQI [59], VSHSS [85] and RCSQ [60, 68], while two studies measured objective sleep variables using BIS BIS [61] and PSG [88]. Of the six studies, five found music therapy to be effective in improving sleep quality [60, 61, 68, 85, 88]. However, Ghiasvandian et al. [59] conducted a study on 70 patients undergoing coronary artery bypass surgery (CABG) and measured objective sleep variables using BIS. The results showed no significant difference in sleep quality before and after the intervention between the experimental and control groups.
3.14 Relaxation Techniques
Seven RCTs evaluated the impact of various relaxation techniques on sleep quality in patients in critical care units (CCUs). The techniques assessed included relaxation and imagery, massage therapy, muscle relaxation, foot baths, relaxation training, and foot reflexology massage. The studies measured sleep quality using different tools, such as the EES [76], PSQI [41, 81], VSHSS [80, 82], SMSHQ [89], and one trial used the PSG [75]. Of the seven studies, two trials by Namba et al. [75] and Talebi Ghadicolaei et al. [89], found that foot baths were not effective in improving sleep quality for patients.
3.15 Acupressure Intervention
Two studies reviewed the effects of valerian acupressure intervention on sleep quality [48, 91]. Yaghoubi et al. [91] conducted an RCT with 60 ICU patients after CABG to evaluate the effectiveness of valerian acupressure compared to routine care. The experimental group received acupressure while the control group only took sedative drugs as needed. Sleep quality was measured using the SMHSQ and results showed that the experimental group had significantly lower scores than the control group [14 (13–14) vs. 23 (23–25), P = 0.001], indicating that valerian acupressure can improve sleep quality in CABG patients. Chen et al. [48] also conducted an RCT to explore the effects of valerian acupressure on the sleep of ICU patients. The experimental group received acupressure on specific points while the control group received conventional treatment. Results showed that the experimental group had increased sleep time and decreased frequency of waking up, supporting the hypothesis that valerian acupressure could improve sleeping time and quality for ICU patients.
3.16 Ventilator Mode Intervention
Two cross-over trials were conducted to investigate the effects of ventilator modes on objective sleep variables in ICU patients, using PSG [43, 78]. One trial by Parthasarathy et al. [78], which compared the objective sleep variables of participants receiving Assist Control Ventilation (ACV) versus Pressure Control Ventilation (PCV). This trial demonstrated a significant increase in Sleep Efficiency Index (SEI) (75 ± 5 vs. 63 ± 5, P < 0.05) and a significant reduction in sleep fragmentation index (54 ± 7 vs. 79 ± 7, P < 0.05) in the ACV group compared to the PSV group. Another trial by Andréjak et al. [43] showed that sleep quantity and quality were significantly improved with PCV compared to spontaneous ventilation with 6 cm H2O inspiratory pressure (low-PSV).
3.17 Care and Behavioral Interventions
Four RCTs and two quasi-experimental studies were conducted to evaluate the effects of protective care and behavioral interventions on subjective sleep variables [54, 62, 65, 93]. Of the four studies, two by Kamdar et al. [65], and Johanson et al. [62], found that physiotherapy and cognitive-behavior therapy did not effectively improve patients’ sleep quality In a quasi-experimental clinical trial involving 160 patients undergoing CABG, those who received supportive educational intervention for at least two days showed significantly better sleep quality than the control group who received routine care [93]. Sleep quality was assessed using the Groningen Sleep Quality Scale (GSQS), which ranges from 0 to 14, with higher scores indicating lower subjective sleep quality. The mean GSQS score for the experimental group was 4.6 ± 5.50, while that of the control group was 10.76 ± 1.27 (P < 0.0001).
3.18 Multi-interventions
Four studies were conducted to investigate the impact of combination interventions versus the usual care on patients’ sleep quality [46, 55, 56, 95]. The multi-interventions included oral melatonin with eye mask/earplugs [56], aromatherapy (damask rose) with eye masks [46], earplugs/eye masks with relaxing music [95], and earplugs/eye masks with white noise [55]. Although all studies indicated that both types of interventions had a significant effect on patients’ sleep quality compared to routine care, we assessed the trials using Jadad scoring and confirmed that two studies [56, 95] did not report why participants withdrew or were removed from the study. Moreover, they did not use double-blind procedures between examiners and examinees.
4 Discussion
This study aimed to examine the effect of nursing interventions on the sleep quality of hospitalized individuals. A systematic review and meta-analysis were conducted, analyzing a total of 77 studies involving 7771 participants. Among these 77 studies, 18 studies (comprising 1153 patients) shared similarities in terms of methodology, study population, sleep quality measurement tools, and inclusion/exclusion criteria. Consequently, these 18 studies were included in the meta-analysis, while the remaining studies (n = 59) underwent a systematic review. The nursing interventions investigated in this study were categorized into eight main groups, including sleep hygiene (factors such as noise reduction, lighting control, and quiet time), the use of earplugs or eye masks (or both), aromatherapy, music therapy, relaxation techniques, acupressure, protective and behavioral interventions, and ventilator modes. The evaluation of patients’ sleep quality was conducted using various tools, which could be classified into two approaches: objective sleep quality (measured by PSG, BIS, EEG, or actigraphy) and subjective sleep quality (measured by PSQI, SMHSQ, VSHSS, RCSQ, or original sleep questionnaires).
After analyzing the 18 studies included in the meta-analysis, it was observed that 11 of these studies utilized the PSQI scale, while the remaining 7 studies used the SMHSQ scale to assess patient sleep quality. The results of the meta-analysis indicated a positive effect of nursing interventions on sleep quality when examining both PSQI and SMHSQ scores in the pooled SMD analysis between the intervention and control groups. Moreover, upon conducting subgroup analysis, it was discovered that patients who received nursing interventions such as earplugs and eye masks, music therapy, or aromatherapy exhibited significantly improved sleep quality, as indicated by the PSQI scores.
The use of earplugs/eye masks or a combination of both has consistently demonstrated a positive effect on the sleep quality of hospitalized patients. This is supported by 12 studies [44, 51, 53, 63, 67, 70, 71, 73, 83, 86, 87, 92], in the review section and five studies [22, 27, 31, 32, 38] included in the meta-analysis. These findings are consistent with our previous study [7]. Regarding relaxation techniques, such as therapeutic massage, Hatha Yoga exercise, muscle relaxation, reflexology massage, and foot bath, their impact on sleep quality among hospitalized patients was explored in 10 studies out of the total 77 reviewed. Among these 10 studies, three [33, 35, 37], were included in the meta-analysis, revealing a positive effect of implementing relaxation techniques on sleep quality. The remaining seven studies [41, 75, 76, 80,81,82, 89] underwent systematic review, and five of them [41, 76, 80,81,82] demonstrated a significant improvement in sleep quality following the use of relaxation techniques. These results are consistent with previous studies, particularly a systematic review [99], which reported positive effects of therapeutic massage on outcomes such as stress, anxiety, pain, and sleep quality among adult patients in the ICU. Overall, the evidence suggests that relaxation techniques can be an effective approach to enhance sleep quality in hospitalized patients. In addition, the review reveals that 83% of the studies analyzed in the systematic section highlight the positive impact of music interventions on patients’ sleep quality [60, 61, 68, 85, 88]. This finding is further supported by the meta-analysis, which confirms the favorable effects of music interventions [26, 30, 39].
Based on the results of individual studies, several interventions have shown a positive impact on both the quality and quantity of sleep. These interventions include implementing quiet time [47, 58, 69, 84] and reducing noise levels [42, 57, 64, 72, 79, 90, 98] as part of sleep hygiene practice, using care-behavioral methods [54, 62, 65, 93] and adjusting ventilator modes [43, 78]. However, due to variations in study design and assessment tools across different clinical settings, it was not feasible to statistically combine these results. Additionally, combining interventions such as music therapy with the use of eye masks/earplugs or oral melatonin in conjunction with eye masks/earplugs has demonstrated improved outcomes, as shown in several studies [46, 55, 56, 95]. Notably, these studies have reported statistically significant differences between the intervention and control groups. Nevertheless, the lack of rigorous methodological approaches diminishes the strength of the evidence obtained.
4.1 Strengths and limitations
In this study, we conducted an extensive literature search in Persian and English languages, without any date restrictions. Additionally, we thoroughly reviewed the reference lists in relevant articles. It is important to note that this study is the first of its kind to specifically focus on the effects of nursing interventions on the sleep quality of hospitalized patients. We ensured the adherence to rigorous PRISMA guidelines in our research methodology. Moreover, each study’s risk of bias was assessed using either the Jadad rating scale or JBI quality assessment tool. Sensitivity analysis and meta-regression analysis were also conducted to ensure the robustness of the findings. However, it is crucial to acknowledge the limitations of this study. Firstly, out of the 77 related studies, only data from 18 were included in the meta-analysis, potentially limiting the generalizability of the findings. Furthermore, the studies exhibited heterogeneity due to variations in demographic and clinical characteristics of the population, which might have influenced the outcomes. The small sample sizes of the included studies could impact the statistical power and precision of the results. Additionally, the short duration of evaluation periods in some studies might limit our understanding of the long-term effects of the interventions. The use of various subjective and objective sleep assessment techniques across studies introduces the possibility of inconsistencies and biases in the data. Lastly, the presence of methodological limitations, such as the lack of double-blinding, raises concerns about the reliability and accuracy of the obtained results. Therefore, it is necessary to interpret the results of this study with caution, considering these limitations.
5 Conclusions
Based on our findings, a substantial number of individual studies indicate that nursing interventions have the potential to enhance both the quantity and quality of sleep in hospitalized patients. However, it is important to note that most of the included studies were limited to qualitative synthesis due to variations in intervention types, control groups, populations, outcome measurements, and reliance on self-reported outcomes. To estimate the effectiveness of these interventions on sleep, we conducted a meta-analysis using two measurement tools (PSQI and SMHSQ). The analysis revealed evidence of a positive effect on both the quantity and quality of sleep in hospitalized patients for only four specific interventions: the use of earplugs and eye masks, relaxation techniques, music therapy, and aromatherapy interventions. It is crucial to exercise caution in interpreting these results due to the differing methodological quality and heterogeneity of the included studies. Drawing definitive conclusions about the efficacy of different interventions is challenging. Nevertheless, these findings offer a comprehensive dataset to explore the current evidence and suggest potential areas for future studies.
Data Availability
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
References
Tiruvoipati R, Mulder J, Haji K. Improving sleep in intensive care unit: an overview of diagnostic and therapeutic options. J Patient Exp. 2020;7(5):697–702. https://doi.org/10.1177/2374373519882234.
Delaney LJ, Van Haren F, Lopez V. Sleeping on a problem: the impact of sleep disturbance on intensive care patients—a clinical review. Ann Intensive Care. 2015;5:3. https://doi.org/10.1186/s13613-015-0043-2.
Pisani MA, Friese RS, Gehlbach BK, Schwab RJ, Weinhouse GL, Jones SF. Sleep in the intensive care unit. Am J Respir Crit Care Med. 2015;191(7):731–8. https://doi.org/10.1164/rccm.201411-2099CI.
Pulak LM, Jensen L. Sleep in the intensive care unit: a review. J Intensive Care Med. 2016;31(1):14–23. https://doi.org/10.1177/0885066614538749.
Medrzycka-Dabrowska W, Lewandowska K, Kwiecień-Jaguś K, Czyż-Szypenbajl K. Sleep deprivation in intensive care unit—systematic review. Open Med (Warsaw, Poland). 2018;13:384–93. https://doi.org/10.1515/med-2018-0057.
Brito RA, do Nascimento Rebouças Viana SM, Beltrão BA, de Araújo Magalhães CB, de Bruin VMS, de Bruin PFC. Pharmacological and non-pharmacological interventions to promote sleep in intensive care units: a critical review. Sleep Breath. 2020;24(1):25–35. https://doi.org/10.1007/s11325-019-01902-7
Karimi L, Rahimi-Bashar F, Mohammadi SM, Mollahadi M, Khosh-Fetrat M, Vahedian-azimi A, et al. The efficacy of eye masks and earplugs interventions for sleep promotion in critically ill patients: a systematic review and meta-analysis. Front Psychiatry. 2021;12: 791342. https://doi.org/10.3389/fpsyt.2021.791342.
Wallace CJ, Robins J, Alvord LS, Walker JM. The effect of earplugs on sleep measures during exposure to simulated intensive care unit noise. Am J Crit Care. 1999;8(4):210.
Babahaji M, Tayebi A, Ebadi A, Askari S, Ebrahimi S, Sharafi S. Effect of Hathayoga exercise on sleep quality of hemodialysis patients. Iran J Nurs Res. 2014;9(3):1–9.
Bahraini S, Bekhradi R, Mannani R, Naji S. the effect of massage therapy on the quality of sleep in women with multiple sclerosis being admitted by isfahan MS Association. J Urmia Nurs Midwifery Fac. 2011;8(4):197–203.
Obanor OO, McBroom MM, Elia JM, Ahmed F, Sasaki JD, Murphy KM, et al. The impact of earplugs and eye masks on sleep quality in surgical icu patients at risk for frequent awakenings. Crit Care Med. 2021. https://doi.org/10.1097/ccm.0000000000005031.
Hellström A, Willman A. Promoting sleep by nursing interventions in health care settings: a systematic review. Worldviews Evid Based Nurs. 2011;8(3):128–42. https://doi.org/10.1111/j.1741-6787.2010.00203.x.
Hu RF, Jiang XY, Chen J, Zeng Z, Chen XY, Li Y, et al. Non-pharmacological interventions for sleep promotion in the intensive care unit. Cochrane Database Syst Rev. 2015;2015(10):CD008808. https://doi.org/10.1002/14651858.CD008808.pub2.
Tamrat R, Huynh-Le MP, Goyal M. Non-pharmacologic interventions to improve the sleep of hospitalized patients: a systematic review. J Gen Intern Med. 2014;29(5):788–95. https://doi.org/10.1007/s11606-013-2640-9.
Moher D, Liberati A, Tetzlaff J, Altman DG. Reprint—preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. 2009;89(9):873–80.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. https://doi.org/10.1016/0197-2456(95)00134-4.
Jadad AR. The merits of measuring the quality of clinical trials: is it becoming a Byzantine discussion? Transpl Int. 2009;22(10):1028. https://doi.org/10.1111/j.1432-2277.2009.00919.x.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. https://doi.org/10.1002/sim.1186.
Viechtbauer W, Cheung MW. Outlier and influence diagnostics for meta-analysis. Res Synth Methods. 2010;1(2):112–25. https://doi.org/10.1002/jrsm.11.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clin Res Ed). 1997;315(7109):629–34. https://doi.org/10.1136/bmj.315.7109.629.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Baghaei R, Ghaderi C, Feizi A. The effect of eye masks on nocturnal sleep in patients hospitalized in the intensive cardiac care units. J Urmia Nurs Midwifery Fac. 2014;12(9):800–6.
Bagheri NM, Heydari GMA, Rezaie S, Pouresmail Z, Yazdani CJ. The effect of acupressure on the quality of sleep in patients with acute coronary syndrome in CCU. Iran J Crit Care Nurs. 2014;7(1):7–14.
Blackburn L, Achor S, Allen B, Bauchmire N, Dunnington D, Klisovic RB, et al. The effect of aromatherapy on insomnia and other common symptoms among patients with acute leukemia. Oncol Nurs Forum. 2017;44(4):E185–93. https://doi.org/10.1188/17.Onf.E185-e193.
Borji M, Otaghi M, Salimi E, Sanei P. Investigating the effect of performing the quiet time protocol on the sleep quality of cardiac patients. Biomed Res. 2017;28(16):7076–80.
Cheraghi M-A, Akbari K, Bahramnezhad F, Haghani H. The effect of instrumental music on sleep in patients admitted to Coronary Care Unit. Iran J Cardiovasc Nurs. 2015;3(4):24–33.
Cheraghi MA, Akbari K, Bahramnezhad F, Haghani H. The effect of earplug on the sleep of patients hospitalized in the coronary care unit. Complement Med J. 2018;8(2):2293–303.
Davari H, Ebrahimian A, Rezayei S, Tourdeh M. Effect of lavender aromatherapy on sleep quality and physiological indicators in patients after CABG surgery: a clinical trial study. Indian J Crit Care Med. 2021;25(4):429–34. https://doi.org/10.5005/jp-journals-10071-23785.
Moeini M, Khadibi M, Bekhradi R, Mahmoudian SA, Nazari F. Effect of aromatherapy on the quality of sleep in ischemic heart disease patients hospitalized in intensive care units of heart hospitals of the Isfahan University of Medical Sciences. Iran J Nurs Midwifery Res. 2010;15(4):234.
Najafi GT. Investigating the effect of listening to nature sounds on sleep quality in patients hospitalized in cardiac care units. Complement Med J. 2018;8(1):2167–80.
Neyse F, Daneshmandi M, Sadeghi Sharme M, Ebadi A. The effect of earplugs on sleep quality in patients with acute coronary syndrome. Iran J Crit Care Nurs. 2011;4(3):127–34.
Neiseh F, Daneshmandi M, Sadeghi Shermeh M, Ebadi A. Effect of eye mask on sleep quality in patients with acute coronary syndrome. J Caring Sci. 2012;1(3):135.
Oshvandi K, Abdi S, Karampourian A, Moghimbaghi A, Homayounfar S. The effect of foot massage on quality of sleep in ischemic heart disease patients hospitalized in CCU. Iran J Crit Care Nurs. 2014;7(2):66–73.
Otaghi M, Qavam S, Norozi S, Borji M, Moradi M. Investigating the effect of lavender essential oil on sleep quality in patients candidates for angiography. Biomed Pharmacol J. 2017;10(1):473–8.
Saeedi Taheri Z, Asadzandi M, Ebadi A. The effect of spiritual care based on GHALBE SALIM model on spiritual experience in patients with coronary artery disease. J Nurs Educ. 2013;1(3):45–53.
Samadi Z, Jannati Y, Hamidia A, Ali Mohammadpour R, Hesamzadeh ALI. The effect of aromatherapy with lavender essential oil on sleep quality in patients with major depression. J Nurs Midwifery Sci. 2021;8(2):67–73.
Shafiee Z, Babaee S, Nazari A, Atashi V. The effect of massage therapy on sleep quality of patients after coronary artery bypass graft operation. Iran J Cardiovasc Nurs. 2013;2(2):22–9.
Zolfaghari MAP, Noghabi AAA, Khameslou MA. Modification of environmental factors on quality of sleep among patients admitted to CCU. J Hayat. 2013;18(4):61–8.
Farokhnezhad Afshar P, Zahednezhad H, Ajri Khamesloo M, Ghanei Gheshlagh R, Fathi R. Effect of white noise on the sleep of elderly patients hospitalized in coronary care units. Iran J Ageing. 2016;11(1):44–51.
Aalami H, Moghadam HM, Moghaddam MB, Bazeli J. Effect of hybrid aromatherapy on sleep quality of patients with acute coronary syndrome admitted to cardiac care unit. Middle East J Fam Med. 2018;7(10):268.
Akinci B, Yeldan I, Bayramoğlu Z, Akpınar TB. The effects of posture and relaxation training on sleep, dyspnea, pain and quality of life in the short-term after cardiac surgery: a pilot study. Turk Gogus Kalp Dama. 2016;24:258–65.
Rahimi A, Faizi F, Nir MS, Amirifar A, Mahmoudikohani F. The effect of planned team work-based cares on the sleep quality in cardio vascular surgery patients of intensive care unit. J Educ Health Promot. 2022;11:231.
Andréjak C, Monconduit J, Rose D, Toublanc B, Mayeux I, Rodenstein D, et al. Does using pressure-controlled ventilation to rest respiratory muscles improve sleep in ICU patients? Respir Med. 2013;107(4):534–41.
Arab M, Mashayekhi F, Ranjbar H, Abazari F, Dortaj E. Comparing the effects of using Earplugs and eye masks on sleep quality of patients in coronary care unit (CCU). Ann Mil Health Sci Res. 2013;11(2):e66529.
Ayik C, Özden D. The effects of preoperative aromatherapy massage on anxiety and sleep quality of colorectal surgery patients: A randomized controlled study. Complement Ther Med. 2018;36:93–9. https://doi.org/10.1016/j.ctim.2017.12.002.
Babaii A, Adib-Hajbaghery M, Hajibagheri A. The effect of aromatherapy with damask rose and blindfold on sleep quality of patients admitted to cardiac critical care units. Iran J Nurs. 2015;28(93):96–105.
Chamanzari H, Hesari-Moghadam M, Malekzadeh J, Shakeri MT, Hojjat SK, Hosseini SM. Effect of implementation of quiet time protocol on sleep quality of patients in intensive care unit. Med Surg Nurs J. 2016;5(1):49–56.
Chen J-H, Chao Y-H, Lu S-F, Shiung T-F, Chao Y-F. The effectiveness of valerian acupressure on the sleep of ICU patients: a randomized clinical trial. Int J Nurs Stud. 2012;49(8):913–20.
Cho M-Y, Min ES, Hur M-H, Lee MS. Effects of aromatherapy on the anxiety, vital signs, and sleep quality of percutaneous coronary intervention patients in intensive care units. Evid Based Complementary Altern Med. 2013;2013:1–6.
Cho EH, Lee MY, Hur MH. The effects of aromatherapy on intensive care unit patients’ stress and sleep quality: a nonrandomised controlled trial. Evid Based Complementary Altern Med eCAM. 2017;2017:2856592. https://doi.org/10.1155/2017/2856592.
Demoule A, Carreira S, Lavault S, Pallanca O, Morawiec E, Mayaux J, et al. Impact of earplugs and eye mask on sleep in critically ill patients: a prospective randomized study. Crit Care. 2017;21(1):284.
Diaz-Alonso J, Smith-Plaza AM, Suarez-Mier B, Lana A. Impact of a nurse intervention to improve sleep quality in intensive care units: results from a randomized controlled trial. Dimens Crit Care Nurs. 2018;37(6):310–7. https://doi.org/10.1097/dcc.0000000000000319.
Eliyasianfar S, Khazaei H, Khatoni A, Pourmirza Kalhori R, Rezaei M. The effect of blindfolds and earplugs on sleep quality of patients admitted to the cardiac intensive care unit. J Clin Res Paramed Sci. 2016;5(1): e81442.
Fakhr-Movahedi A, Mirmohammadkhani M, Ramezani H. Effect of milk-honey mixture on the sleep quality of coronary patients: a clinical trial study. Clin Nutr ESPEN. 2018;28:132–5.
Farrehi PM, Clore KR, Scott JR, Vanini G, Clauw DJ. Efficacy of sleep tool education during hospitalization: a randomized controlled trial. Am J Med. 2016;129(12):1329.e9-1329.e17.
Foreman B, Westwood AJ, Claassen J, Bazil CW. Sleep in the neurological intensive care unit: feasibility of quantifying sleep after melatonin supplementation with environmental light and noise reduction. J Clin Neurophysiol. 2015;32(1):66–74.
Gabor JY, Cooper AB, Crombach SA, Lee B, Kadikar N, Bettger HE, et al. Contribution of the intensive care unit environment to sleep disruption in mechanically ventilated patients and healthy subjects. Am J Respir Crit Care Med. 2003;167(5):708–15.
Gardner G, Collins C, Osborne S, Henderson A, Eastwood M. Creating a therapeutic environment: a non-randomised controlled trial of a quiet time intervention for patients in acute care. Int J Nurs Stud. 2009;46(6):778–86.
Ghiasvandian S, Haghverdi R, Zakerimoghadam M, Kazemnezhad A, Mousavi M, Saeid Y. The effect of preferred music on sleep quality among patients after coronary artery bypass surgery. Iran J Cardiovasc Nurs. 2014;3(3):14–21.
Hansen IP, Langhorn L, Dreyer P. Effects of music during daytime rest in the intensive care unit. Nurs Crit Care. 2018;23(4):207–13. https://doi.org/10.1111/nicc.12324.
Jaber S, Bahloul H, Guétin S, Chanques G, Sebbane M, Eledjam J. Effects of music therapy in intensive care unit without sedation in weaning patients versus non-ventilated patients. Annales francaises d’anesthesie et de reanimation. 2007;26(1):30–8.
Johanson KA, Bohlen AJ, Feliciano L. No need to count sheep: investigating an online insomnia intervention among older adults. Am J Geriatr Psychiatry. 2018;26(3):S156.
Jones C, Dawson D. Eye masks and earplugs improve patient’s perception of sleep. Nurs Crit Care. 2012;17(5):247–54.
Kamdar BB, King LM, Collop NA, Sakamuri S, Colantuoni E, Neufeld KJ, et al. The effect of a quality improvement intervention on perceived sleep quality and cognition in a medical ICU. Crit Care Med. 2013;41(3):800.
Kamdar BB, Combs MP, Colantuoni E, King LM, Niessen T, Neufeld KJ, et al. The association of sleep quality, delirium, and sedation status with daily participation in physical therapy in the ICU. Crit Care. 2016;20(1):1–9.
Karadag E, Samancioglu S, Ozden D, Bakir E. Effects of aromatherapy on sleep quality and anxiety of patients. Nurs Crit Care. 2017;22(2):105–12.
Khoddam H, Maddah SA, Rezvani Khorshidi S, Zaman Kamkar M, Modanloo M. The effects of earplugs and eye masks on sleep quality of patients admitted to coronary care units: a randomised clinical trial. J Sleep Res. 2022;31(2): e13473. https://doi.org/10.1111/jsr.13473.
Kim J, Choi D, Yeo MS, Yoo GE, Kim SJ, Na S. Effects of patient-directed interactive music therapy on sleep quality in postoperative elderly patients: a randomized-controlled trial. Nat Sci Sleep. 2020;12:791–800. https://doi.org/10.2147/nss.s286375.
Knauert MP, Redeker NS, Yaggi HK, Bennick M, Pisani MA. Creating naptime: an overnight, nonpharmacologic intensive care unit sleep promotion protocol. J Patient Exp. 2018;5(3):180–7.
Koo YJ, Koh HJ. Effects of eye protective device and ear protective device application on sleep disorder with coronary disease patients in CCU. Taehan Kanho Hakhoe Chi. 2008;38(4):582–92.
Le Guen M, Nicolas-Robin A, Lebard C, Arnulf I, Langeron O. Earplugs and eye masks vs routine care prevent sleep impairment in post-anaesthesia care unit: a randomized study. Br J Anaesth. 2014;112(1):89–95.
Li SY, Wang TJ, Vivienne Wu SF, Liang SY, Tung HH. Efficacy of controlling night-time noise and activities to improve patients’ sleep quality in a surgical intensive care unit. J Clin Nurs. 2011;20(3–4):396–407.
Mashayekhi F, Pilevarzadeh M, Amiri M, Rafiei H. The effect of eye mask on sleep quality in patients of coronary care unit o efeito da mascara de olhos na qualidade de sono em pacientes em uma unidade coronariana. Sleep Sci. 2013;6(3):108–11.
Mirzaeian R, Rohi M, Khadibi M. Exploring the effect of aromatherapy using lavender oil on the patients with ischemic heart disease in the intensive care units (ICUS) of the hospitals of the city of Isfahan in 2009. In: 2nd national congress on medicinal plants 15, 16 May 2013, Tehran-Iran; 2013.
Namba S, Shimoyama I, Kiguchi T, Ujike Y. Effects of foot baths on sleep in ICU patients. Chiba Med J. 2012;88(6):59–64.
Nerbass FB, Feltrim MI, Souza SA, Ykeda DS, Lorenzi-Filho G. Effects of massage therapy on sleep quality after coronary artery bypass graft surgery. Clinics (Sao Paulo, Brazil). 2010;65(11):1105–10. https://doi.org/10.1590/s1807-59322010001100008.
Özlü ZK, Bilican P. Effects of aromatherapy massage on the sleep quality and physiological parameters of patients in a surgical intensive care unit. Afr J Tradit Complement Altern Med. 2017;14(3):83–8. https://doi.org/10.21010/ajtcam.v14i3.9.
Parthasarathy S, Tobin MJ. Effect of ventilator mode on sleep quality in critically ill patients. Am J Respir Crit Care Med. 2002;166(11):1423–9.
Patel J, Baldwin J, Bunting P, Laha S. The effect of a multicomponent multidisciplinary bundle of interventions on sleep and delirium in medical and surgical intensive care patients. Anaesthesia. 2014;69(6):540–9.
Rahmani A, Naseri M, Salaree MM, Nehrir B. Comparing the effect of foot reflexology massage, foot bath and their combination on quality of sleep in patients with acute coronary syndrome. J Caring Sci. 2016;5(4):299.
Ranjbaran S, Dehdari T, Sadeghniiat-Haghighi K, Majdabadi MM. Poor sleep quality in patients after coronary artery bypass graft surgery: an intervention study using the PRECEDE-PROCEED model. J Tehran Heart Center. 2015;10(1):1–8.
Richardson S. Effects of relaxation and imagery on the sleep of critically ill adults. Dimens Crit Care Nurs. 2003;22(4):182–90.
Richardson A, Allsop M, Coghill E, Turnock C. Earplugs and eye masks: do they improve critical care patients’ sleep? Nurs Crit Care. 2007;12(6):278–86.
Ruggiero C, Dziedzic L. Promoting a healing environment: quiet time in the intensive care unit. Jt Comm J Qual Saf. 2004;30(8):465–7.
Ryu MJ, Park JS, Park H. Effect of sleep-inducing music on sleep in persons with percutaneous transluminal coronary angiography in the cardiac care unit. J Clin Nurs. 2012;21(5–6):728–35.
Scotto CJ, McClusky C, Spillan S, Kimmel J. Earplugs improve patients’ subjective experience of sleep in critical care. Nurs Crit Care. 2009;14(4):180–4.
Sharafi S, Hajiabadi F, Razi M, Bahrami M. The effect of simultaneously using earplug and eye mask on quality of sleep in intensive care unit patients: a randomized clinical trial study. Crit Care Nurs. 2018;11(4):27–34.
Su CP, Lai HL, Chang ET, Yiin LM, Perng SJ, Chen PW. A randomized controlled trial of the effects of listening to non-commercial music on quality of nocturnal sleep and relaxation indices in patients in medical intensive care unit. J Adv Nurs. 2013;69(6):1377–89.
Talebi Ghadicolaei H, Heydary Gorji MA, Bagheri B, Yazdani Charati J, Hadinejad Z. The effect of warm footbath on the quality of sleep on patients with acute coronary syndrome in cardiac care unit. J Caring Sci. 2019;8(3):137–42. https://doi.org/10.15171/jcs.2019.020.
van de Pol I, van Iterson M, Maaskant J. Effect of nocturnal sound reduction on the incidence of delirium in intensive care unit patients: an interrupted time series analysis. Intensive Crit Care Nurs. 2017;41:18–25.
Yaghoubi A, Golfeshan E, Azarfarin R, Nazari A, Alizadehasl A, Ehasni A. Effects of acupressure on sleep quality after coronary artery bypass surgery. Iran Heart J. 2017;18(3):28–34.
Yazdannik AR, Zareie A, Hasanpour M, Kashefi P. The effect of earplugs and eye mask on patients’ perceived sleep quality in intensive care unit. Iran J Nurs Midwifery Res. 2014;19(6):673.
Zakerimoghadam M, Mousavi Malek N, Esmaeeli M, Kazemnejad A. The effect of supportive educational intervention on sleep before coronary artery bypass graft surgery. Iran J Cardiovasc Nurs. 2016;4(4):40–7.
Borromeo AR. The effects of aromatherapy on the patient outcomes of anxiety and sleep quality in coronary care unit patients: Texas Woman's University; 1998. http://hdl.handle.net/11274/3698.
Hu R-F, Jiang X-Y, Hegadoren KM, Zhang Y-H. Effects of earplugs and eye masks combined with relaxing music on sleep, melatonin and cortisol levels in ICU patients: a randomized controlled trial. Crit Care. 2015;19(1):1–9.
MhF ZR, Jalilolghadr SH, Alipour HM. The effect of “CitrusAurantium” aroma on sleep quality of patients hospitalized in the coronary care unit (CCU). Complement Med J. 2014;4(1):720–33.
Tazakori Z, Babaee S, Karimolahi M, Bayat F, Mohammad T-K. The effect of damask rose extract on sleep quality in patients undergo-ing angiography admitted to cardiac care unit. Cardiovas Nurs J. 2016;5(1):52–7.
Oshvandi K, Koosha MM, Cheraghi F, Fardmal TN, Falahinia G. The impact of nursing interventions on quality of sleep among patients in coronary care unit of Ekbatan Hospital in Hamadan City, Iran. Sci J Hamadan Nurs Midwifery Fac. 2014;22(1):60–9.
Jagan S, Park T, Papathanassoglou E. Effects of massage on outcomes of adult intensive care unit patients: a systematic review. Nurs Crit Care. 2019;24(6):414–29. https://doi.org/10.1111/nicc.12417.
Acknowledgements
Thanks to guidance and advice from the “Clinical Research Development Unit of Baqiyatallah Hospital”.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to this study. AVA and MS designed the study. AVA, MM and AA contributed to the concept of the review and meta-analysis, AA, ZV, MM and MS acquisition of data, analysis and interpretation of data, drafting the article. All authors edited and revised manuscript and approved final version of manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Ethical Approval
Ethical approval for this study was obtained from the research ethics committee of Baqiyatallah University of Medical Sciences with the ethics code of IR.BMSU.REC.1398.175. In addition, this study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database (CRD42020145830). This study was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) statement.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Registration number: The study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database (CRD42020145830).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ashghab, A., Vahedian-Azimi, A., Vafadar, Z. et al. Nursing Interventions to Improve the Sleep Quality of Hospitalized Patients: A Systematic Review and Meta-analysis. Intensive Care Res 4, 55–71 (2024). https://doi.org/10.1007/s44231-024-00056-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44231-024-00056-9