Abstract
Asthma, one of the most common chronic diseases of adults and children, is an important public health concern. The cause of asthma is thought to be a combination of genetic and environmental factors, and a growing body of research has investigated the possible geographic and contextual factors that contribute to asthma prevalence. However, few studies have incorporated geographic and environmental variables into their designs, despite evidence that geography is associated with asthma exacerbation. Additionally, studies of asthma exacerbations among adults are limited. The situation regarding asthma is particularly concerning in North Central Texas (NCT) compared to the national context. In light of this, we analyzed the geographic variation of approximately 12,000 adult patients hospitalized for asthma in the North Central Texas Region, and their association with built environmental features such as land use types, dwelling characteristics, exposure to traffic parameters at the Census Block Group (CBG) level, and pollutant concentrations in the relevant counties for the year 2014. We applied the Hierarchical Linear Model (HLM), and our analysis indicates that there are significant health disparities in the region. We found that the adult asthma hospitalization rate is significantly higher in low-income, low-education neighborhoods with a significant Black population. Furthermore, factors such as increased travel distance to work and substandard dwelling conditions have been found to trigger an increase in hospital visits for asthma patients. Conversely, the presence of greenspace in the surrounding area has been found to help reduce the frequency of asthma-related hospital visits. It is worth noting that both indoor and outdoor environmental quality contribute to adult asthma hospitalizations. Overall, our study highlights the importance of considering geographic and environmental factors in understanding the prevalence and exacerbation of asthma. Our findings suggest that targeted interventions, such as improving indoor and outdoor environmental quality and increasing access to greenspace, may help reduce the burden of asthma in high-risk communities.
Similar content being viewed by others

Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Epidemiologic, environmental science, as well as urban planning studies on geographic variation in asthma prevalence, have identified asthma as an important public health concern (Hudak 2014; Li & Newcomb 2009; Grant, Wagner, & Weiss 1999). It is one of the major chronic diseases globally and is influenced by both environmental and genetic factors (Jie et al. 2013). According to the World Health Organization (2017), about 235 million people around the world and more than 26 million people in the US are currently suffering from asthma (CDC.gov 2018; Asthma and Allergy Foundation of America 2018). Asthma is unusually prevalent in the Dallas Fort Worth (DFW) Metro area in North Texas. Nationally it ranked 77th worst place for asthma prevalence (Asthma and Allergy Foundation of America 2018).
A growing body of literature exists regarding the possible geographic and contextual factors that affect asthma prevalence. Some have found that traffic exposure and social inequalities of the neighborhoods are associated with childhood asthma hospitalization ( Newcomb and Cyr 2012; Li and Newcomb 2009). Other studies have focused on the effect of ground level ozone concentration on childhood asthma (Goodman et al. 2017; Khunsri 2015; Carls 2010). A recent study on adult asthma observed the effects of social inequalities and their association with traffic density, speed of traffic, age of housing structure and proximity to urban drilling sites (Newcomb and Li 2019). Although many other factors such as land use, outdoor air pollutants, and indoor environmental quality could affect asthma, their relationships with adult asthma hospital admission have yet to be well explored. Our research attempts to fill this gap. In particular, we investigate the association of land use, housing structure, and outdoor air pollution with adult asthma in addition to social determinants and transportation features using data from the North Central Texas (NCT) region and the Hierarchical Linear Modeling (HLM) technique. The results can be utilized by urban planners to develop plans aimed at reducing asthma exacerbations. Public health professionals can cautiously utilize the findings for asthma prevention. Policy makers can also use the information to create policies that support remedial efforts to improve public health. In the following sections, we summarize the status of this line of research, describe our research approach, and present our findings.
Studies on built environmental variables and adult asthma
Previous studies on built environmental variables and asthma prevalence largely focused on childhood asthma. A thorough and detailed review of more than 2000 published articles on asthma prevalence using Anandan et al.s’ (2010) predetermined criteria indicated that only 48 articles fulfilled the criteria. Most of these studies focused on children and teenage asthma while only a limited number of studies were available on adult asthma. A main reason behind the tendency to focus on childhood asthma is that the prevalence of asthma is higher among children than adults (Lundbäck et al. 2016; Dharmage et al. 2019) and children are more susceptible to respiratory compromise (Khreis et al. 2016). However, asthma prevalence among adults is considerable (Newcomb & Li 2019). Moreover, morbidity and mortality are higher in adult asthma patients than pediatric patients (Dharmage et al. 2019).
Evidence suggests that asthma can be affected by multiple factors, but the influence of environmental factors on asthma is complex. Although numerous studies have investigated the association between various built environmental variables and childhood asthma (Khreis et al. 2016), most studies only explored a few subsets of environmental exposures such as age of home, gas stove use (Eisner and Blanc 2003), wall dampness (Trupin et al. 2010), dust weight, presence of pet allergens (Blanc et al. 2005) and presence of vermin-related allergens (Lewis et al. 2002). The influence of many other indoor environmental factors have not been explored.
Several traffic exposure parameters have been used in the literature. Common measures of traffic exposure are distance to major roads (Balmes et al. 2009), levels of elemental carbon attributable to traffic (ECAT) (Epstein et al. 2012), traffic density (Meng et al. 2007), density of roads in the neighborhood and speed of traffic in nearby roads (Newcomb & Li 2019). Besides traffic exposure, concentration of ambient air pollutants was separately investigated by some studies to explore their influence on adult asthma. Those studies commonly investigated exposure to ozone (Alexeeff et al. 2008) and concentration of respirable particulates, specifically particulates with diameters less than 2.5 µm (PM2.5) (Young et al 2014). With the application of different statistical methods such as logistic, multivariate or land use regression models, studies found that these environmental parameters have different degrees of association with adult asthma prevalence.
The existing studies considered social environmental factors at both the individual and neighborhood level along with physical environmental parameters. However, these studies have not simultaneously investigated the combined effects of both indoor and outdoor environmental subsets in the same analysis. Moreover, some of these studies (Lewis et al. 2002; Blanc et al. 2005) have analyzed the sociodemographic condition in a manner almost entirely divorced from the physical environmental factors.
A study by Trupin et al. (2010) has considered indoor (wall dampness, air filter, wood heating system, pet, total amount of dust, metal concentration, etc.), outdoor (land use, distance of roadway from residence, concentration of ozone, NO2, PM2.5, PM10 etc.), and neighborhood socioeconomic characteristics. The authors collected the indoor environmental information through individual interview, and obtained the outdoor data that are at the neighborhood level from secondary sources. Despite the hierarchical structure of their data at individual and neighborhood level, they used multiple linear regression for data analysis. This may cause a possibility of aggregation bias and reduced the statistical strength of the data. Besides, factors such as land use were not explicitly explored by their study, in which they considered land use as a dichotomous variable to distinguish urban land uses from rural land use.
Newcomb and Li (2019) considered a wide variety of environmental variables, but they only considered urban drilling for land use. Models including other land use variables could portray a more comprehensive picture of the influence of land use on adult asthma. Moreover, they considered age of housing structures as one of the parameters of neighborhood quality. This measurement may not capture precisely the indoor environment of homes.
Our research advances previous studies by utilizing precise measurements and investigating the combined influence of outdoor, indoor, and social environmental variables on adult asthma prevalence. Besides considering neighborhood, land use, transportation, and dwelling characteristics we also considered Ozone and Particulate Matter 2.5 as pollutant concentration available at the county or regional level. Since ozone is a gas, it can easily disperse throughout the air and impact people living in different areas, even those who are not in close proximity to pollution sources. Similarly, PM2.5 can be dispersed across a region, affecting multiple neighborhoods and communities. This can be particularly problematic in urban areas with high levels of traffic and industry, where PM concentrations tend to be higher. Therefore, considering the hierarchical data structure and limitations of previous literature, we employ more advanced modeling techniques that are better suited for the data structure. Our study aims to make a valuable contribution to the literature by providing empirical results from an understudied area, utilizing more complete data and advanced analytical techniques.
Methods
Study area
The study area is the 12 counties in the NCT Region. In this research, we considered 12 out of the 16 counties in the NCT region, as ozone concentration information was available for only these 12 counties for the year 2014. The unit of analysis is Census Block Group. This study includes 11697 unduplicated records of 18 to 65 year old individual asthma patients with valid addresses in the study area. These patients were admitted into 56 hospitals within the NCT area for treatment of asthma from January 1, 2014 to December 31, 2014. Figure 1 represents the geocoded location of those adult asthma patients.
Research hypotheses and data
In order to comprehensively investigate the combined effects on adult asthma, we include variables in the dimensions of transportation, land use, socioeconomic characteristics, and housing condition. The variables and their expected relationships with the dependent variable are displayed in Table 1.
Data processing
Adult asthma hospitalization rate
We obtained data on adult asthma patients from the Dallas/Fort Worth Hospital Council Foundation (DFWHCF). The dataset included geographic locations but did not contain any other identifiable information. To ensure accuracy, we thoroughly checked individual addresses for case sensitivity and spelling issues before geocoding the location information. We were able to geocode approximately 95% of hospital records, while the remaining 5% were excluded due to unknown or incomplete addresses. The patients had unique identifier numbers and some patients were admitted to the hospitals for multiple times. In this research, the number of each unique patient was considered which means patients with multiple admissions will be counted once. Then, this unduplicated number of patients was considered with respect to the adult population of pertinent CBGs. After a rigorous data cleaning process, the location information was aggregated at the census block group level, which further protected the privacy of the patients. The dependent variable, adult asthma hospitalization rate in each census block group, was calculated with the following equation:
where, i denotes census block group (CBG), Ra stands for Adult Asthma Hospitalization Rate in particular CBG, Na is number of each unique adult asthmatic patient admitted in Hospital, Ta is Total adult population of pertinent CBG.
Travel distance to work
We used the Origin–destination (OD) data of the LEHD Origin–Destination Employment Statistics (LODES). In this dataset, jobs totals are associated with both a home Census Block and a work Census Block. We joined the OD data with census block shape file using ArcGIS. Then we determined the distance from the centroid of home census blocks to the work census blocks. Since the unit of analysis of our study is Census Block Groups, we aggregated the distances by census block group, then divided the aggregated travel distance value with the number of workers at each census block groups who worked outside of home using the following equation:
where, i indicates particular census block group, Dw is the Average Travel Distance per worker in Census Block Group (CBG), Ad is the aggregated distance between origin and work destination at census block groups, Tw is the total number of workers of 16 years and over, Hw is the number of workers 16 years and over who worked at home.
Weighted road density
In our study, we incorporated the concept of weighted road density to account for the varying levels of exposure to different road types within a particular area (Hansell et al. 2014). Weighted road density takes into consideration the cumulative impact of nearby roads, which may differ in terms of traffic lane numbers, traffic volume, speed, and purpose. We calculated the weighted road density for internal roads within the census block groups (CBGs), including major highways, arterials, and private roads. In accordance with previous research (Hansell et al. 2014), we assigned a weighting of 3 to arterial roads, 2 to distributor roads, and 1 to local roads. Following this concept by Hansell et al. (2014), we calculated the Weighted Road Density with the following equation:
In this equation, i denotes the particular census block group, l indicates length, Wr is the weighted road density, Ba is area of pertinent CBG in square mile, G is Driveway, P is Private Road, C is Connecting Road, M is Minor Arterial, E is Major Arterial, F is Access Ramp, S is Service Road and Z is major highways. All road lengths were considered in miles, and area of census block group was considered in square mile.
Other variables
In addition to road density, we also examined other built environmental factors, such as land use and dwelling characteristics. To calculate the proportion of different land use types within each Census Block Group, we divided the area of each land use type by the total land area of the Census Block Group. Similarly, we computed the percentage of housing units that lacked complete kitchens or plumbing systems and those that were older than 40 years by dividing the number of such units by the total number of housing units in the neighborhood. This normalization technique allowed us to compare and analyze these variables more effectively.
For air pollution, we considered ozone and particulate matter 2.5. The Environmental Protection Agency (EPA) sets and updates the air quality standards for ground‐level ozone to improve public health and environmental protection. For 12 counties of the NCT region, this data was available for the year 2014 from the Texas Commission on Environmental Quality (TCEQ). The ozone concentration is recorded through continuous air monitoring stations (CAMS) and these CAMS numbers were used to get the measurements from individual sites located in NCT regions. The readings can represent concentration of ozone at the county level (Khunsri 2015). The EPA sets the standard of the primary 8-h ozone standard and the range for “Unhealthy for Sensitive Groups” begins at 71 parts per billion (ppb). We used the “maximum value” of Eight Hours Ozone high value days which was close to or met or exceeded 71 ppb in 2014. The EPA sets the 24-h PM2.5 standard to 35 μg/m3 and the level of the annual PM2.5 standard at 12 μg/m3 (The U.S. Environmental Protection Agency, n.d.-c). We considered the average daily density of fine particulate matter (PM2.5) in micrograms per cubic meter for the year 2014 that was available for all NCT counties from ‘Key Finding Reports: County Health Rankings and Road Maps’(cite source or date).
Analytical approaches
For data analysis, this study employed spatial cluster analysis and descriptive statistics. To identify hotspots or clusters of adult asthma patients, we used the Hot Spot Analysis (Getis-Ord Gi*) tool. To investigate potential multicollinearity among independent variables, we conducted a correlation analysis. Additionally, we used multiple linear regression models to identify the statistically significant sociodemographic, land use, transportation, and dwelling factors that influence asthma conditions. The built environmental parameters of our research are at different geographic levels, such as pollutants (PM2.5 and Ozone) at the county level and other built environmental variables (land use, transportation, dwelling) at the census block group level. In other words, the data are nested in different levels, with individuals nested in census block groups and census block groups nested in counties. Previous studies have shown that when research data are nested, statistical approaches must account for the multilevel nature of the data to avoid errors in interpretation (Dickinson, Miriam & Basu 2005). Therefore, our study explored the geographical distribution and severity of adult asthma patients in North Central Texas concerning the influential surrounding outdoor and indoor determinants using Hierarchical Linear Modeling. The model specification is presented in Fig. 2.
Research findings
Characteristics of adult asthma patients
The age and gender compositions of adult patients and the general population are shown in Fig. 3. It is evident that there were more female asthma patients than male in every age cohort as shown in Fig. 3(a). In comparison, the male/female ratio of the general population in every age group was almost equal as revealed in Fig. 3(b). Among the asthmatic patients, the percentage of females in the age group of 65 years was about 74% − the largest percentage among all age groups. The percentage of females in the age group of 18–19 years was about 54%, which is the lowest in all the age groups but still higher than their male counterparts.
The higher ratio of women with asthma incidence has been consistently reported by many scholars for years and for various countries (Abraham, et al. 2003; Santillan 2003; Pignataro et al. 2017). Previous studies attributed this phenomenon to female hormones that are responsible for such susceptibility towards asthma (Zein, et al. 2019; Koper et al. 2017). Though, the precise role of sex hormones remains unclear, they are known to be involved in the intricate cellular signaling pathways. Male hormones have protective effects against asthma through effects on cellular immune system (Koper et al. 2017).
Table 2 presents a comparison of the racial disparities of adult asthma in the NCT region. The data reveals that the percentage of black patients (43.20%) was approximately equal to that of white patients (48.60%). However, when examining the total black and white population across all census block groups (CBGs) in North Central Texas, it becomes clear that the black population represents only 15% of all races in the region, while the white population comprises 72%. However, despite their smaller population size, black individuals accounted for 43% of adult asthma patients in the region, highlighting a significant disparity in asthma prevalence. In this predominantly white region, the proportion of black asthma patients is similar to that of white asthma patients, indicating that black individuals in NCT region experience a greater burden of asthma severity. They also potentially face difficulty accessing health services. The data shows that a higher percentage of minority groups, such as Native American and Black patients, were uninsured compared to other race groups. Specifically, about 56% of Native American and 46% of Black adult asthma patients were uninsured, compared to approximately 40% among white patients as shown in Table 2. These disparities strongly suggest unequal access to healthcare among different race groups.
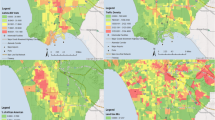
Spatial cluster of asthma prevalence
We conducted a spatial pattern analysis to identify the areas with the highest concentration of adult asthma patients in the study region. Our hotspot analysis revealed that the majority of asthma patients who visited hospitals were concentrated in the center of Dallas, Tarrant, and Hunt counties (refer to Fig. 4). These hotspots, depicted in red, indicate that with 90% confidence or higher, most of the asthma patients who visited hospitals reside in these areas. It was found that 36% of the total adult population living in census block groups with adult asthma patients were situated in these hotspots. Furthermore, 50% of adult asthma patients were living in these identified hotspot areas. In contrast, areas with few hospital visits were identified as cold spots, illustrated in blue, in Denton, Collin, Parker, Kaufmann, Rockwall, and Hood counties with a confidence level of 90% or higher.
We further examined the spatial clusters by income groups and land use types. The hotspots contain very low (62%)- low (40%) household median income census block groups (Table 3). This indicates patients with hospital visits are highly concentrated in low-income areas. Adult asthma patients living in low-income areas face challenges that can impact their health outcomes. These areas are often characterized by a lack of access to healthcare, limited resources for managing asthma symptoms, and exposure to environmental factors that can exacerbate asthma symptoms. In contrast, the identified cold spots were primarily comprised of high (72%) and very high-income census block groups (87%). This suggests that patients residing in these areas were less likely to visit hospitals. A comparison of two maps, one showing the hotspots and the other showing the median household income of census block groups (Fig. 5), further highlights the relationship between income and asthma hospitalization rates.
The hotspot clusters are primarily characterized by commercial (48%), industrial (36%), and transportation (54%) land uses. These types of land uses have been linked to asthma exacerbation in previous literature, making it particularly concerning that adult asthma patients with hospital visits are concentrated in these areas. In contrast, the cold spots were characterized by a higher proportion of green spaces, accounting for approximately 38% of the land use. These areas may help reduce the influence of asthma exacerbation and provide a potential solution to mitigate the effects of asthma. Notably, the hotspots only had a 21% share of green spaces.
Hierarchical Linear Model (HLM)
In this study, the dependent variable adult asthma hospitalization rate and predictor variables such as land use, transportation, socioeconomic and dwelling conditions are at census block groups level. On the other hand, concentration of ozone and particulate matter 2.5 are at county level, which is upper-level data or level 2 data. The unit of analysis (i.e. census block group) is nested within the higher level (county) data. The aim of this study was to investigate the impact of various factors on adult asthma hospitalization rates in census block groups where asthma patients reside. Specifically, we examined how changes in land use, transportation, socioeconomic status, and dwelling conditions at the census block group level, as well as changes in air pollutant concentration in the surrounding county, affected the hospitalization rate. To account for the complexity of these factors operating at different geographic levels, we utilized a Hierarchical Linear Model (HLM) to analyze the relationships between the dependent variable and the predictors. This approach allowed us to explore the composite effects of the predictors across different geographic levels on adult asthma hospital admission condition.
But before developing the HLM model, we examined Pearson correlations to identify collinearity among all the Census Block Group level predictor variables (land use, transportation, socioeconomic and dwelling parameters). We excluded highly correlated variables from further consideration. Then, among a wide range of predictors from land use, transportation, socioeconomic and dwelling parameters, we identified the statistically significant parameters by separately developing a multiple regression model. Then we used those statistically significant built environmental and socioeconomic parameters at level 1 of the HLM model.
We used the stepwise random intercept linear mixed model of SPSS to generate the HLM model. We developed the HLM in two steps. In the first model, we added the census block group level or level 1 built environmental and socioeconomic variables. The second and final model contains both census block group and county level predictor variables. Table 4 presents goodness of fit statistics of all these models.
The -2 log likelihood of model 2 or final model indicates a better fit of the model compared to the first model. The result of the final HLM model is presented in Table 5. In level 1, race, income, commute distance and in level 2, ozone are significantly associated at 0.05 level after controlling for all other variables.
Transportation parameters
The transportation variables, specifically commute distance and travel mode, have significant effects. Controlling for other factors, the coefficient of commute distance is approximately 0.03. This indicates that for every mile increase in commute distance, there is a 0.03 increase in the adult asthma rate. Longer exposure to the traffic environment due to a longer travel distance is associated with adult asthma exacerbation. Similarly, the results demonstrate that traveling by bus has a positive correlation with the hospital admission rate (0.002). On the other hand, compared to other modes, working from home reduces the adult asthma rate by 0.001. The results suggest that buses may emit higher levels of pollutants when approaching, idling, and leaving from bus stops, and that transit riders waiting in those areas are exposed to poor air quality caused by buses (Kim 2018). On the other hand, working from home can avoid daily exposure to harmful pollution and reduce the chance of getting respiratory problems.
While other traffic exposure variables are not significant at the 0.05 level, they display the expected signs. For example, the results of our model indicate that weighted road density and distance from major highways have a positive association with the adult asthma rate. These findings are consistent with the results of previous studies. According to the previous literature, an increased amount of traffic infrastructure in a neighborhood is associated with an increased exacerbation of respiratory symptoms (Hansell et al. 2014; Rose et al. 2009).
Land use
The results of the model show significant relationships between the percentage of land used for mobile homes and greenspace and the dependent variable at the 0.05. Specifically, a percentage increase in mobile homes is associated with a 0.013 increase in adult asthma hospitalization rate. Previous studies have suggested that mobile homes are constructed with materials that may release formaldehyde, and chronic inhalation of this chemical can contribute to exacerbations of respiratory symptoms (Gan et al. 2017). The coefficient of greenspace is approximately -0.002, indicating that an increase in greenspace is associated with a reduction in the adult asthma hospitalization rate. Preserving green spaces in any area can help to reduce respiratory problems among the residents (Ebisu et al. 2011).
Moreover, the model outputs suggest that although commercial land use and railroads are not strongly associated with the asthma hospitalization rate, the signs of the relationships align with existing literature. Previous studies have found commercial land use and railroads to be linked with asthma exacerbations, especially in asthmatic children, as these land uses generate traffic-related air pollution (Maantay 2001; Juhn et al. 2010).
Dwelling condition
The study examined the indoor environment quality of housing units in relation to kitchen and plumbing facilities. According to the Department of Housing and Urban Development (HUD), a housing unit is considered to be of substandard/low quality if it lacks either complete plumbing or complete kitchen facilities (U.S. Census Bureau 2015).
In addition to plumbing and kitchen facilities, the age of the residential structure was considered as a parameter to indicate indoor housing characteristics. Residential structures that were built at least 40 years ago were assumed to indicate dilapidation, as previous studies have found that older buildings are more likely to contain asthma triggers such as cockroaches, rodents, mold, and dust mites (Corburn et al. 2006). Housing age was used as a proxy to determine indoor environment quality in different neighborhoods.
The study found that a higher percentage of older housing units was associated with a higher rate of adult asthma hospital admissions. Additionally, the percentage of housing units with incomplete plumbing facilities was strongly and positively related to the adult asthma hospitalization rate. The lack of complete plumbing and a complete kitchen can introduce disease vectors such as insects or rats, which may exacerbate asthma symptoms (Krieger & Higgins 2002).
Air pollutant concentration
The concentration of ozone and PM2.5 is measured at different county-level sites in the NCT region. These measurements can represent the pollutants' concentrations across the counties, which can eventually affect the microclimate or neighborhood level. Thus, we considered this county-level data in addition to the neighborhood built environmental variables to observe the impact at the neighborhood level. To capture the influence of parameters at different geographic levels, we applied HLM. Our analysis indicates that the effect of PM2.5 on adult asthma is statistically insignificant, while the effect of ozone concentration is statistically significant. Ozone is known to trigger asthma attacks by irritating the lungs and airways. The Asthma and Allergy Foundation of America (2018) also states that ozone concentration is directly related to asthma attacks. The Dallas Fort Worth region is non-attainment for ozone, which means that it does not meet the national primary or secondary ambient air quality standard for ozone pollution (U.S. Environmental Protection Agency, n.d.b). Our model suggests that adult asthma hospital visits increase with increased ozone concentration during Eight Hour Ozone high-value days in this region. However, the impact of ozone on asthma is complex, and its severity can vary depending on several factors such as age, level and duration of exposure, and underlying health conditions.
Summary and discussion
In contrast to other studies on adult asthma in the USA, we considered a wide variety of physical environmental factors that includes both indoor and outdoor parameters as well as different geographical levels. This is a novel strategy since many researchers have investigated the influence of specific environmental factors on adult asthma exacerbations and in most cases they focused on single aspects such as traffic exposure, air pollutant concentration or housing condition (Trupin et al. 2010). By incorporating different sets of physical and social environmental factors together, this study uncovers which predictors have stronger explanatory power over other factors to reflect associations with asthma exacerbations. Overall, the study found that sociodemographic, indoor housing qualities, and outdoor physical environment all contribute to the asthma hospitalization rate in different neighborhoods.
Our descriptive analysis results showed that there exists a large disparity in adult asthma in the north Texas region. The majority of adult asthma patients admitted to hospital were African American and are less likely to be insured. The model results indicated that higher rates of hospital visits tended to be in black neighborhoods with low income and low education level. Historically marginalized groups generally have less access to asthma management/education due to inadequate health insurance coverage, less accessibility to health care due to transportation issues, fear of using medication due to side effects, and lack of knowledge about asthma triggers and management (Mansour et al. 2000; Bender and Bender 2005). Moreover, such groups are more likely to be exposed to harmful environments that exacerbate their asthma symptoms As studies found, low income neighborhoods are more likely to be located near industrial sites and major roadways both of which produce a lot of air pollution (Hsu et al. 2018).
Our study also reveals the important effects of transportation and land use variables on adult asthma. After controlling for road density and proximity to major highways, our analysis detected the effects of commute distance, and some commute modes have strong influence on asthma.
The variable of mobile home is not only a measure of land use but can also serve as a proxy for a measure of the indoor environmental quality because of the materials in those houses. Mobile home, older housing structure, housings without complete kitchen or plumbing system can be found in low-income, distressed neighborhoods because low-income communities might not have enough resources to maintain the quality of both indoor and outdoor environment, hence suffer from the negative health outcomes.
Air pollutants like Ozone can get dispersed far from its source, making it a regional rather than a local pollutant. This means that even if an individual is not located near a source of ozone pollution, they can still be exposed to high levels of ozone due to its regional dispersion. According to the Asthma and Allergy Foundation of America, exposure to ozone can cause asthma attacks, and people with asthma are particularly vulnerable to the effects of ozone. Our study has shown that an increase in "Bad Ozone Days" in the Dallas Fort Worth area can significantly exacerbate asthma conditions among adults, leading to hospital admissions. Thus, it is essential to take measures to reduce ozone pollution and protect public health, especially those with pre-existing respiratory conditions.
Limitations
Every research has limitations, and this study is not an exception. One of the important limitations is data availability. Several epidemiologic studies have reported genetic condition, weight, smoking habit, and daily lifestyle, etc., are important parameters associated with asthma. However, data collected from the Dallas Fort Worth Hospital Council Foundation (DFWHCF), which collects data from hospitals across the north Texas region, do not include such detailed information. The data policy prohibits the disclosure of personal information, precluding the possibility of conducting surveys or focus group discussions with adult asthma patients sourced from DFWHCF. As a result, investigating asthma conditions based on their behavioral patterns and other genetic information was not a viable option to consider in our research.
There might be workplace influence on adult asthma exacerbation (Trupin et al. 2010). However, we could not capture such influences due to data limitations. Nevertheless, our study investigated the effects of areas surrounding the living place of adult asthma patients and part of their daily commuting pattern.
Conclusion
It is important to ensure access to health facilities for asthma patients regardless of age, gender, race, or income level. Asthma prevention and treatment measures should be more accessible to patients regardless of payor status. Integrating prevention and treatment into public health services rather than depending on private sources of care could improve access. Interventions targeting health systems that address discrimination and ensure access to care should be initiated in any asthma mitigation plan for populations. Furthermore, environmental justice policies should be incorporated in the work principles of urban planning agencies which can help the socially distressed asthma population. In collaboration with public health agencies, urban planners can help identify the spatial pattern of asthma severity and help with suggestions for creating less toxic areas.
Externalities of other land uses regarding asthma patients should also be carefully considered. As the presence of railroads, mobile homes, commercial and industrial entities were found to be positively associated with asthma hospitalization rates, planners, health care providers and policy makers should attempt to control the health impact of such land uses. Since the existence of natural green space or timberlands was found to reduce the asthma hospitalization rate in the NCT region, areas with railroads should be surrounded by natural vegetation in residential areas. Similarly, with the help of local government, transportation planners and urban planners can ensure residential locations are at safer distances from major highways. Also, for existing residential areas near highways there should be sufficient protective measures such as green boundaries. This can help to reduce railroad-related air pollution.
For other significant transportation parameters, such as travel distance to work and travel mode to work, planners should consider travel patterns selected by the travelers. Individuals with asthma can be exposed to asthma awareness programs, which include information about travelling shorter distances or living closer to workplaces. People with asthma can be encouraged to use masks to avoid inhalation of public transit emitted pollutants at transit stoppages or on board. In addition, diesel powered buses or other public transportation should be updated to use more environmentally friendly fuel that can help to reduce the risks for asthma patients.
Substandard housing with incomplete kitchen and plumbing systems or dilapidated conditions should be renovated or upgraded according to the standard housing codes. Public health agencies and housing authorities should make strong collaborations to ensure enforcement of these codes. Historically, housing and building codes are the result of public health reforms of the late 1800s and early 1900s to tackle infectious disease instigated by public housing. But today, housing and health departments are different sectors which obstructs their capabilities to undertake more comprehensive and place-based approaches (De Leon, E., & Schilling 2017). Currently, preparation and execution of most housing codes are the responsibility of the housing and construction department (Krieger and Higgins 2002). Through strong cooperation among public health, housing, and urban planning departments, ensuring healthy homes can be achieved. Local governments can promote community outreach to educate housing authorities and residents to resolve complex issues of substandard housing.
For air pollutants, urban planners should employ pollution reduction techniques in different areas to keep the concentration of PM2.5 within a manageable limit. Moreover, trees help to absorb or reduce particulate matter suspended in the air. Increased vegetation and tree plantations in different areas can help reduce such pollution. For ozone, there are multiple ozone monitoring stations in the north central Texas region, which support the ozone alert system for bad ozone days ranging from high alert levels (maroon color- indicate hazardous) to lower alert level (green color-indicate good). An ozone alert is issued every time the ozone level increases (orange level, more than 71 ppb) that is harmful for sensitive groups of people like children, elderly with respiratory health issues and workers who work outside for a long time. During an Ozone Alert Day, the sensitive groups are advised to reduce prolonged outside activities and people with asthma are advised to follow their asthma action plan and keep their relief medicine handy (City of Dallas 2018). Such a warning system could also be introduced for other pollutants. This has the potential to help individuals with asthma and other respiratory conditions to be cautious and avoid exposure to pollutants.
To improve the comprehensiveness and accuracy of our findings, future research can address the limitations of our study. For instance, our research did not account for important factors such as weight, height, lifestyle, stress levels, or genetic information of the patients. Collecting and incorporating this additional information in future studies can provide more enriched information and help to identify the authentic reasons behind certain patterns, such as why adult female asthmatic patients are more vulnerable in NCT region. Furthermore, future research could explore the impact of climate change on asthma, including how changes in temperature, precipitation, and air quality may affect asthma risk in different regions. Ultimately, these research efforts could lead to more targeted and effective interventions for reducing the burden of adult asthma.
In conclusion, adult asthma is a growing concern, and the built environment plays a significant role in exacerbating this condition. Research has shown that exposure to indoor and outdoor air pollutants, such as traffic-related pollution and surrounding land uses can trigger asthma symptoms in adults. Additionally, poor housing conditions, including inadequate ventilation, plumbing facilities/dampness, and lack of maintenance, have also been linked to asthma exacerbations. Therefore, it is crucial for policymakers to take action to improve the built environment, reduce indoor and outdoor air pollution, and promote healthy housing conditions. By doing so, we can help reduce the burden of adult asthma and improve the quality of life for individuals living with this condition.
Study specific ethical declarations
The research adhered to the guidelines of the Declaration of Helsinki and was determined by the University of Texas Southwestern Medical Center/Texas Health Resources IRB to be non-human subject research, consequently exempt from IRB oversight.
Availability of data and materials
Data of asthma hospital visits in 2014 were obtained from the Dallas/Fort Worth Hospital Council Foundation. The ACS data are publicly available and accessible through the United States Census Bureau. LEHD Origin–Destination Employment Statistics (LODES), North Central Texas Council of Government (NCTCOG) and Texas Commission of Environmental Quality (TCEQ) also provide publicly available data.
References
Abraham B, Anto JM, Barreiro E, Bel EHD, Bonsignore G, Bousquet J, Castellsague J (2003) The ENFUMOSA cross-sectional european multicentre study of the clinical phenotype of chronic severe asthma. Eur Respir J 22(3):470–477. https://doi.org/10.1183/09031936.03.00261903
Alexeeff SE, Litonjua AA, Wright RO, Baccarelli A, Suh H, Sparrow D, Vokonas PS, Schwartz J (2008) Ozone exposure, antioxidant genes, and lung function in an elderly cohort : VA normative aging study. Occup Environ Med 79:736–742. https://doi.org/10.1136/oem.2007.035253
Anandan C, Nurmatov U, Van Schayck OCP, Sheikh A (2010) Is the prevalence of asthma declining ? systematic review of epidemiological studies. Allergy 65:152–167. https://doi.org/10.1111/j.1398-9995.2009.02244.x
Balmes JR, Earnest G, Katz PP, Yelin EH, Eisner MD, Chen H, Trupin L, Lurmann F, Blanc PD, Francisco S (2009) Asthma and lower airway disease original articles exposure to traffic : lung function and health status in adults with asthma. J Allergy Clin Immunol 123(3):626–631. https://doi.org/10.1016/j.jaci.2008.10.062
Bender BG, Bender SE (2005) Patient-identified barriers to asthma treatment adherence : responses to interviews, focus groups, and questionnaires. Immunol Allergy Clin North Am 25:107–130. https://doi.org/10.1016/j.iac.2004.09.005
Blanc PD, Eisner MD, Katz PP, Yen IH, Archea C, Earnest G, Janson S et al (2005) Impact of the home indoor environment on adult asthma and rhinitis. J Occup Environ Med 47(4):362–372. https://doi.org/10.1097/01.jom.0000158708.32491.9d
Corburn J, Osleeb J, Porter M (2006) Urban asthma and the neighbourhood environment in New York City. Health Place 12:167–179. https://doi.org/10.1016/j.healthplace.2004.11.002
Dharmage SC, Perret JL, Custovic A (2019) Epidemiology of asthma in children and adults. Front Pediatr 7(June):1–15. https://doi.org/10.3389/fped.2019.00246
Ebisu K, Holford TR, Belanger KD, Leaderer BP, Bell ML (2011) Urban land-use and respiratory symptoms in infants. Environ Res 111(5):677–684. https://doi.org/10.1016/j.envres.2011.04.004
Epstein TG, Ryan PH, Lemasters GK, Bernstein CK, Levin LS, Bernstein JA, Villareal MS, Bernstein DI (2012) Poor asthma control and exposure to traffic pollutants and obesity in older adults. Ann Allergy Asthma Immunol 108(6):423-428.e2. https://doi.org/10.1016/j.anai.2012.04.009
Gan WQ, Sanderson WT, Browning SR, Mannino DM (2017) Different types of housing and respiratory health outcomes. Prev Med Rep 7:124–129
Goodman JE, Ke Zu, Loftus CT, Tao Ge, Liu X, Lange S (2017) Ambient ozone and asthma hospital admissions in Texas: a time-series analysis. Asthma Res Pract 3(1):6. https://doi.org/10.1186/s40733-017-0034-1
Hansell AL, Rose N, Cowie CT, Belousova EG, Bakolis I, Ng K, Toelle BG, Marks GB (2014) Weighted road density and allergic disease in children at high risk of developing asthma. PLoS ONE 9(6):1–9. https://doi.org/10.1371/journal.pone.0098978
Hudak PF (2014) Spatial pattern of ground-level ozone concentration in Dallas-Fort Worth metropolitan area. Int J Environ Res 8(4):897–902
Jie Y, Isa ZMd, Jie X, Ju ZL, Ismail NH (2013) Urban vs. rural factors that affect adult asthma. Rev Environ Contam Toxicol 226:33–63 (Springer)
Koper I, Hufnagl K, Ehmann R (2017) Gender aspects and influence of hormones on bronchial asthma – secondary publication and update. World Allergy Organ J 10:46. https://doi.org/10.1186/s40413-017-0177-9
Krieger J, Higgins DL (2002) Housing and health : time again for public health action. Am J Public Health 92(5):758–768
Lewis SA, Weiss ST, Platts-mills TAE, Burge H, Gold DR (2002) The role of indoor allergen sensitization and exposure in causing morbidity in women with asthma. Am J Respir Crit Care Med 165:961–966. https://doi.org/10.1164/rccm.2103044
Meng Y-Y, Wilhelm M, Rull RP, English P (2007) Traffic and outdoor air pollution levels near residences and poorly controlled asthma in adults. Ann Allergy Asthma Immunol 98(5):455–463. https://doi.org/10.1016/S1081-1206(10)60760-0
Newcomb P, Cyr A (2012) Conditions associated with childhood asthma in North Texas. ISRN Allergy 2012:823608. https://doi.org/10.5402/2012/823608
Newcomb J, Li P (2009) Disparities in childhood asthma hospitalizations: a spatial analysis of contextual effects. Transport Re Part D: Transport Environ 14(5):317–25. https://doi.org/10.1016/j.trd.2009.03.004
Newcomb P, Li J (2019) Predicting admissions for adult asthma exacerbations in North Texas. Public Health Nurs 36(6):779–786. https://doi.org/10.1111/phn.12654
Pignataro FS, Bonini M, Forgione A, Melandri S, Usmani OS (2017) Asthma and gender: the female lung. Pharmacol Res. https://doi.org/10.1016/j.phrs.2017.02.017
Rose N, Cowie C, Gillett R, Marks GB (2009) Weighted road density: a simple way of assigning traffic-related air pollution exposure. Atmos Environ 43(32):5009–5014. https://doi.org/10.1016/j.atmosenv.2009.06.049
Santillan AA, Camargo CA Jr (2003) Body mass index and asthma among mexican adults : the effect of using self-reported vs measured weight and height. Int J Obes 2002:1430–33. https://doi.org/10.1038/sj.ijo.0802395
Trupin L, Balmes JR, Chen H, Eisner MD, Katharine Hammond S, Katz PP, Lurmann F et al (2010) An integrated model of environmental factors in adult asthma lung function and disease severity : a cross-sectional study. Environ Health 2:1–14
Young MT, Sandler DP, DeRoo LA, Vedal S, Kaufman JD, London SJ (2014) Ambient air pollution exposure and incident adult asthma in a Nationwide cohort of U. S. Women. Am J Respir Crit Care Med 190(8):914–921. https://doi.org/10.1164/rccm.201403-0525OC
Zein JG, Denson JL, Wechsler ME (2019) Asthma over the adult life course gender and hormonal influences asthma phenotype gender differences hormones aging autophagy. Clin Chest Med 40(1):149–161. https://doi.org/10.1016/j.ccm.2018.10.009
Asthma and Allergy Foundation of America (2018) Asthma capitals: Top 100 most challenging cities to live in with asthma. https://www.aafa.org/asthma-capitals/
Carls GS (2010) Ozone Alerts and Asthma Exacerbations: A Case Study of Dallas-Fort Worth 2000–2008. A dissertation submitted in partial fulfillment of the requirements for the degree of doctor of philosophy (Health Services Organization and Policy and Economics) in The University of Michigan
CDC.gov (2018) Most recent asthma state or territory data. 2018. https://www.cdc.gov/asthma/most_recent_data_states.htm#modalIdString_CDCTable_0.
City of Dallas (2018) Dallas-Fort Worth Ozone Alert Day – May 16. http://www.dallascitynews.net/dallas-fort-worth-ozone-alert-day-saturday-april-28
De Leon E, Schilling J (2017) Urban Blight and Public Health: Addressing the Impact of Substandard Housing, Abandoned Buildings, and Vacant Lots
Dickinson M, Basu A (2005) Multilevel modeling and practice-based research. Ann Fam Med 52–60. https://doi.org/10.1370/afm.340
Eisner MD, Blanc PD (2003) Gas stove use and respiratory health among adults with asthma in NHANES III. Occup Environ Med 60(10):759–64. https://doi.org/10.1136/oem.60.10.759
Grant EN, Wagner R, Weiss KB (1999) Observations on emerging patterns of asthma in our society. J Allergy Clin Immunol 104(2):S1–S9
Hsu A, Alexandre N, Brandt J, Chakraborty T, Comess S, Feierman, Huang T, Janaskie S, Manya D, Moroney M, Moyo N, Rauber R, Sherriff G, Thomas R, Tong J, Xie Y, Weinfurter A, Yeo Z (2018) The urban environment and social inclusion index. Yale University, New Haven
Juhn YJ, Qin R, Urm S, Katusic S (2010) The influence of neighborhood environment on the incidence of childhood asthma: a propensity score approach. J Allergy Clin Immunol 125(4):838–843.e2. https://doi.org/10.1016/j.jaci.2009.12.998
Khunsri S (2015) Spatio-temporal variations in asthma hospitalizations in Texas 2005–2011 by county and possible association with ozone exposure. [PhD Dissertation, University of Texas Arlington]. https://rc.library.uta.edu/uta-ir/bitstream/handle/10106/25091/KHUNSRI_uta_2502D_13145.pdf?sequence=1&isAllowed=y
Khreis H, Kelly C, Tate J, Parslow R, Lucas R, Nieuwenhuijsen M (2016) Exposure to Traf Fi C-Related air pollution and risk of development of childhood asthma : a systematic review and meta-analysis. Environ Int 34–40https://doi.org/10.1016/j.envint.2016.11.012
Kim D (2018) Transportation contributing factors to asthma morbidity : the case of Los Angeles county case of Los Angeles County. Int J Urban Sci 0(0):1–14.https://doi.org/10.1080/12265934.2018.1500493
Lundbäck B, Backman H, Lötvall J, Rönmark E, Lundbäck B, Backman H, Lötvall J et al (2016) Is asthma prevalence still increasing ? Is asthma prevalence still increasing ?” Expert review of respiratory medicine 6348 (November 2015). https://doi.org/10.1586/17476348.2016.1114417.
Maantay J (2001) Public Health Matters Zoning, Equity, and Public Health. Am J Public Health 91(7):1033–41. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1446712/pdf/11441726.pdf
Mansour ME, Lanphear BP, DeWitt TG (2000) Mansour(2000)Barriers_to_Asthma_Care_in_Urb.PDF. Pediatrics 106(3).
Newcomb P, Li J. 2019. Predicting admissions for adult asthma exacerbations in North Texas. 1–8. https://doi.org/10.1111/phn.12654.
Rao M, George LA, Shandas V, & Rosenstiel TN (2017) Organic thin-film transistors with sub-10-micrometer channel length with printed polymer/carbon nanotube electrodes. Assessing the potential of land use modification to mitigate ambient NO2 and its consequences for respiratory health. https://doi.org/10.1016/j.orgel.2017.10.023.
U.S. Census Bureau (2015) Plumbing and kitchen facilities in housing units. https://www.census.gov/content/dam/Census/library/working-papers/2015/acs/2015_Raglin_01.pdf
World Health Organization. (2017) Asthma. 2017. http://www.who.int/news-room/fact-sheets/detail/asthma.
Acknowledgements
The authors express their gratitude to the University of Texas Arlington and Texas Health Resources for providing research facilities.
Funding
The research did not receive any funding from any source.
Author information
Authors and Affiliations
Contributions
Conceptualization, J. Jahan, J. Li, and P. Newcomb; methodology, J. Jahan; data collection, J. Jahan, and P. Newcomb; validation, J. Li, and P. Newcomb; formal analysis, J. Jahan; writing—original draft preparation, J. Jahan; writing—review and editing, J. Jahan, J. Li and P. Newcomb.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jahan, J., Li, J. & Newcomb, P. Social and built environmental factors associated with adult asthma hospital admission in the North Central Texas. City Built Enviro 2, 8 (2024). https://doi.org/10.1007/s44213-024-00026-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44213-024-00026-3